Is the Small Ossicle of Type 1 Accessory Navicular a Cause of Foot Pain?—A Case Report
Abstract
:1. Introduction
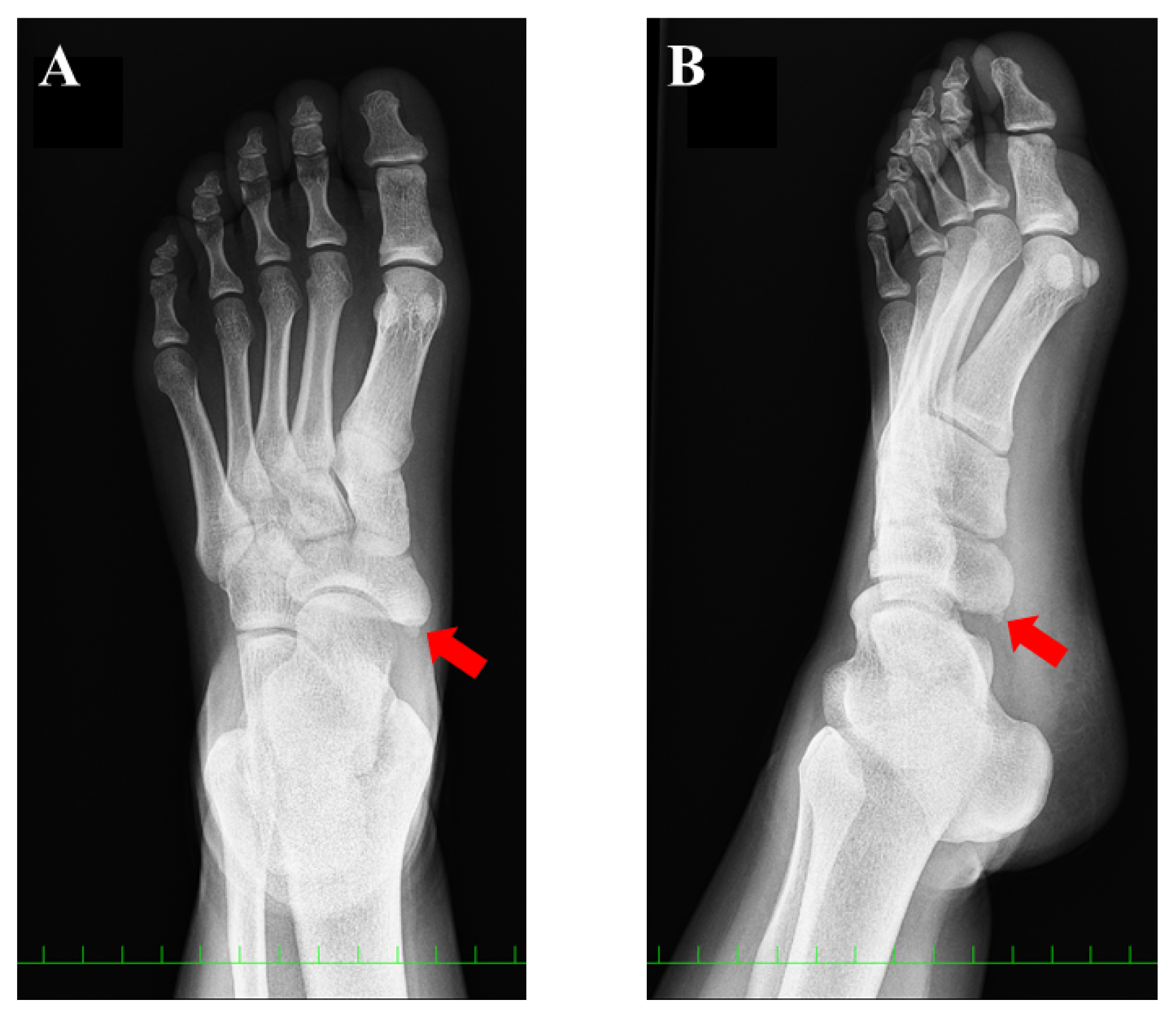
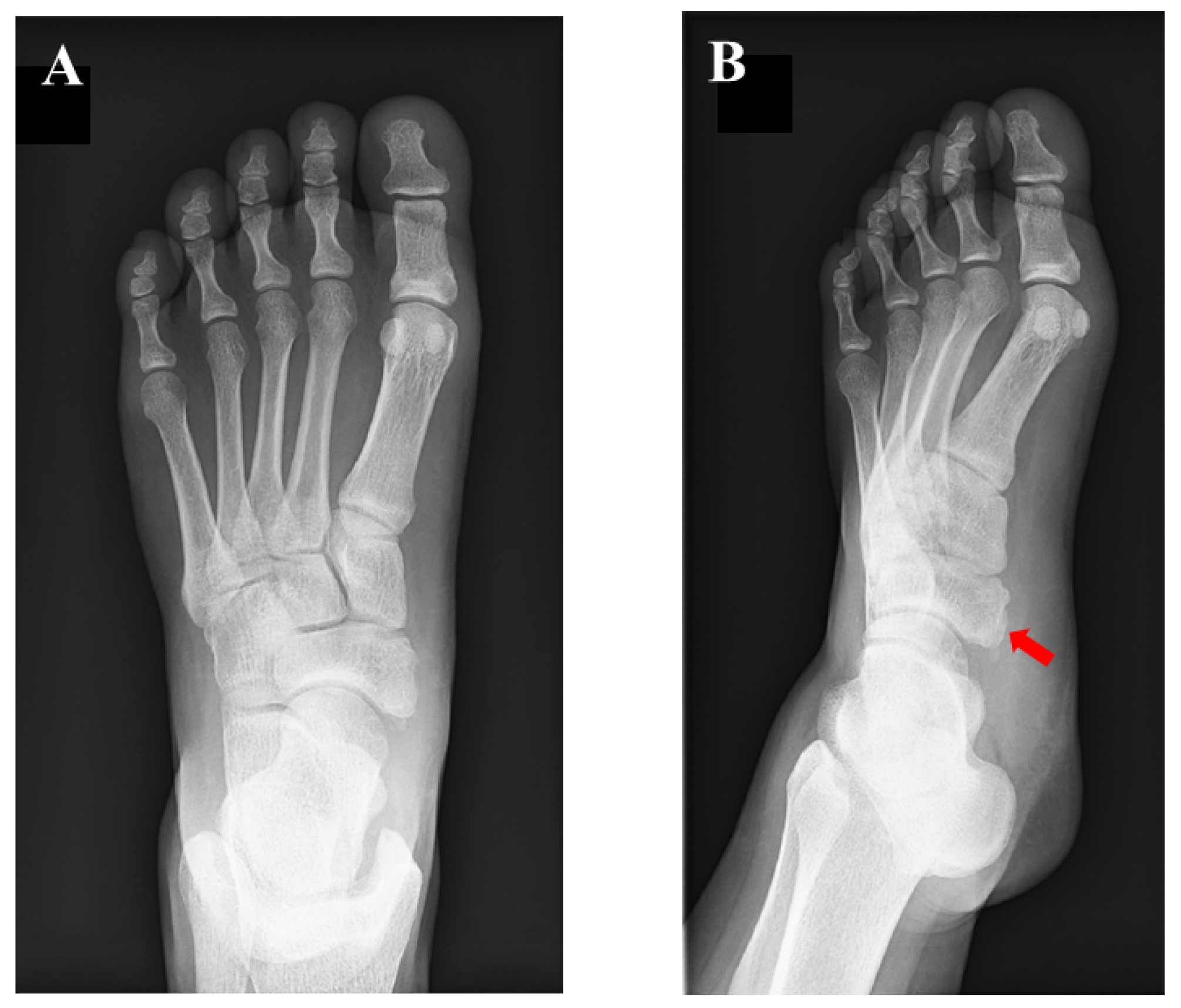
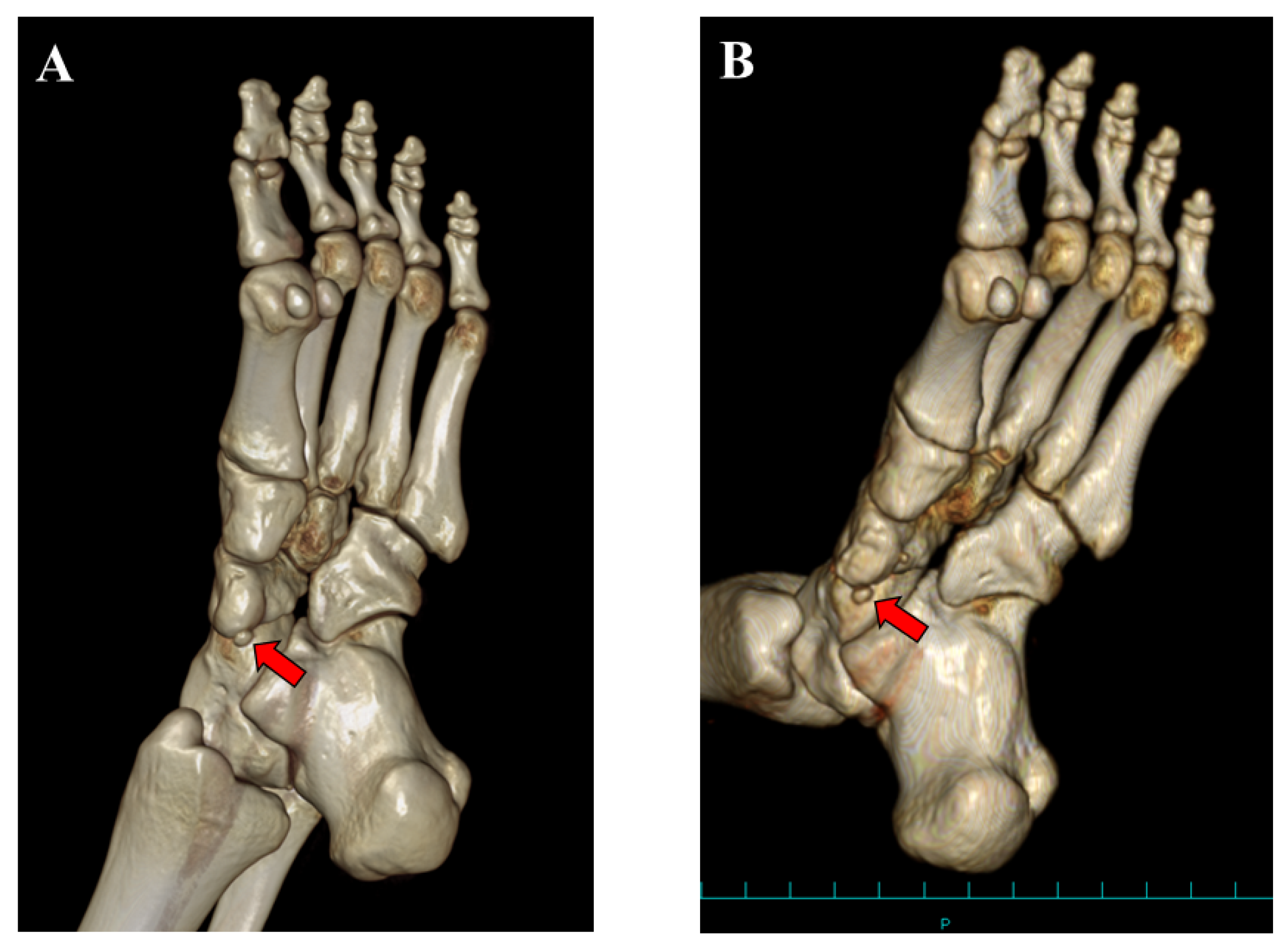
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grogan, D.P.; Gasser, S.I.; Ogden, J.A. The Painful Accessory Navicular: A Clinical and Histopathological Study. Foot Ankle 1989, 10, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Kalbouneh, H.; Alajoulin, O.; Alsalem, M.; Humoud, N.; Shawaqfeh, J.; Alkhoujah, M.; Abu-Hassan, H.; Mahafza, W.; Badran, D. Incidence and anatomical variations of accessory navicular bone in patients with foot pain: A retrospective radiographic analysis. Clin. Anat. 2017, 30, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Wariach, S.; Karim, K.; Sarraj, M.; Gaber, K.; Singh, A.; Kishta, W. Assessing the Outcomes Associated with Accessory Navicular Bone Surgery—A Systematic Review. Curr. Rev. Musculoskelet. Med. 2022, 15, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Veitch, J.M. Evaluation of the Kidner Procedure in Treatment of Symptomatic Accessory Tarsal Scaphoid. Clin. Orthop. Relat. Res. 1978, 131, 210–213. [Google Scholar] [CrossRef]
- Jang, H.-S.; Park, K.-H.; Park, H.-W. Comparison of outcomes of osteosynthesis in type II accessory navicular by variable fixation methods. Foot Ankle Surg. 2017, 23, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Kakihana, M.; Tochigi, Y.; Yamazaki, T.; Ohashi, M.; Ozeki, S. Suture anchor stabilization of symptomatic accessory navicular in adolescents: Clinical and radiographic outcomes. J. Orthop. Surg. 2020, 28, 2309499020918949. [Google Scholar] [CrossRef] [PubMed]
- Jasiewicz, B.; Potaczek, T.; Kącki, W.; Tęsiorowski, M.; Lipik, E. Results of simple excision technique in the surgical treatment of symptomatic accessory navicular bones. Foot Ankle Surg. 2008, 14, 57–61. [Google Scholar] [CrossRef]
- Wynn, M.; Brady, C.; Cola, K.; Rice-Denning, J. Effectiveness of Nonoperative Treatment of the Symptomatic Accessory Navicular in Pediatric Patients. Iowa Orthop. J. 2019, 39, 45–49. [Google Scholar]
- Cha, S.-M.; Shin, H.-D.; Kim, K.-C.; Lee, J.-K. Simple Excision vs the Kidner Procedure for Type 2 Accessory Navicular Associated with Flatfoot in Pediatric Population. Foot Ankle Int. 2013, 34, 167–172. [Google Scholar] [CrossRef]
- Coughlin, M. Sesamoid and accessory bones of the foot. In Mann’s Surgery of the Foot and Ankle, 9th ed.; Coughlin, M., Saltzman, C., Anderson, R., Eds.; Elsevier: Amsterdam, The Netherlands, 2013; pp. 544–554. [Google Scholar]
- Perdikakis, E.; Grigoraki, E.; Karantanas, A. Os naviculare: The multi-ossicle configuration of a normal variant. Skelet. Radiol. 2011, 40, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Kurashige, T.; Tsunoda, Y. Adult Flat Foot with Multiple Accessory Navicular Bones Treated Surgically: A Case Report and Review of the Literature. J. Foot Ankle Surg. 2019, 58, 1019–1024. [Google Scholar] [CrossRef]
- Ibrahim, T.; Beiri, A.; Azzabi, M.; Best, A.J.; Taylor, G.J.; Menon, D.K. Reliability and Validity of the Subjective Component of the American Orthopaedic Foot and Ankle Society Clinical Rating Scales. J. Foot Ankle Surg. 2007, 46, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Sierevelt, I.N.; Zwiers, R.; Schats, W.; Haverkamp, D.; Terwee, C.B.; Nolte, P.A.; Kerkhoffs, G.M.M.J. Measurement properties of the most commonly used Foot- and Ankle-Specific Questionnaires: The FFI, FAOS and FAAM. A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2059–2073. [Google Scholar] [CrossRef] [PubMed]
- Jegal, H.; Park, Y.U.; Kim, J.S.; Choo, H.S.; Seo, Y.U.; Lee, K.T. Accessory Navicular Syndrome in Athlete vs General Population. Foot Ankle Int. 2016, 37, 862–867. [Google Scholar] [CrossRef] [PubMed]
- Knapik, D.M.; Archibald, H.D.; Xie, K.K.; Liu, R.W. A retrospective study on factors predictive of operative intervention in symptomatic accessory navicular. J. Child. Orthop. 2019, 13, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Chen, J.; Chen, Z.; Zeng, C.; Guo, H. Clinical Outcomes of Fusion in Type II Accessory Naviculars with or without Asymptomatic Flatfeet. Foot Ankle Int. 2023, 44, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.-J.; Liu, X.; Li, Y.-X.; Chen, Y.; Li, J.; Zhang, H. Is Kidner procedure necessary during subtalar arthroereisis for pediatric flexible flatfoot that combined with symptomatic type 2 accessory navicular? A retrospective comparative study. Foot Ankle Surg. 2023, 29, 393–400. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yokoe, T.; Uemichi, K.; Tajima, T.; Chosa, E. Is the Small Ossicle of Type 1 Accessory Navicular a Cause of Foot Pain?—A Case Report. Medicina 2023, 59, 1562. https://doi.org/10.3390/medicina59091562
Yokoe T, Uemichi K, Tajima T, Chosa E. Is the Small Ossicle of Type 1 Accessory Navicular a Cause of Foot Pain?—A Case Report. Medicina. 2023; 59(9):1562. https://doi.org/10.3390/medicina59091562
Chicago/Turabian StyleYokoe, Takuji, Kazushi Uemichi, Takuya Tajima, and Etsuo Chosa. 2023. "Is the Small Ossicle of Type 1 Accessory Navicular a Cause of Foot Pain?—A Case Report" Medicina 59, no. 9: 1562. https://doi.org/10.3390/medicina59091562





