Efficacy of Wheelchair Skills Training Program in Enhancing Sitting Balance and Pulmonary Function in Chronic Tetraplegic Patients: A Randomized Controlled Study
Abstract
1. Introduction
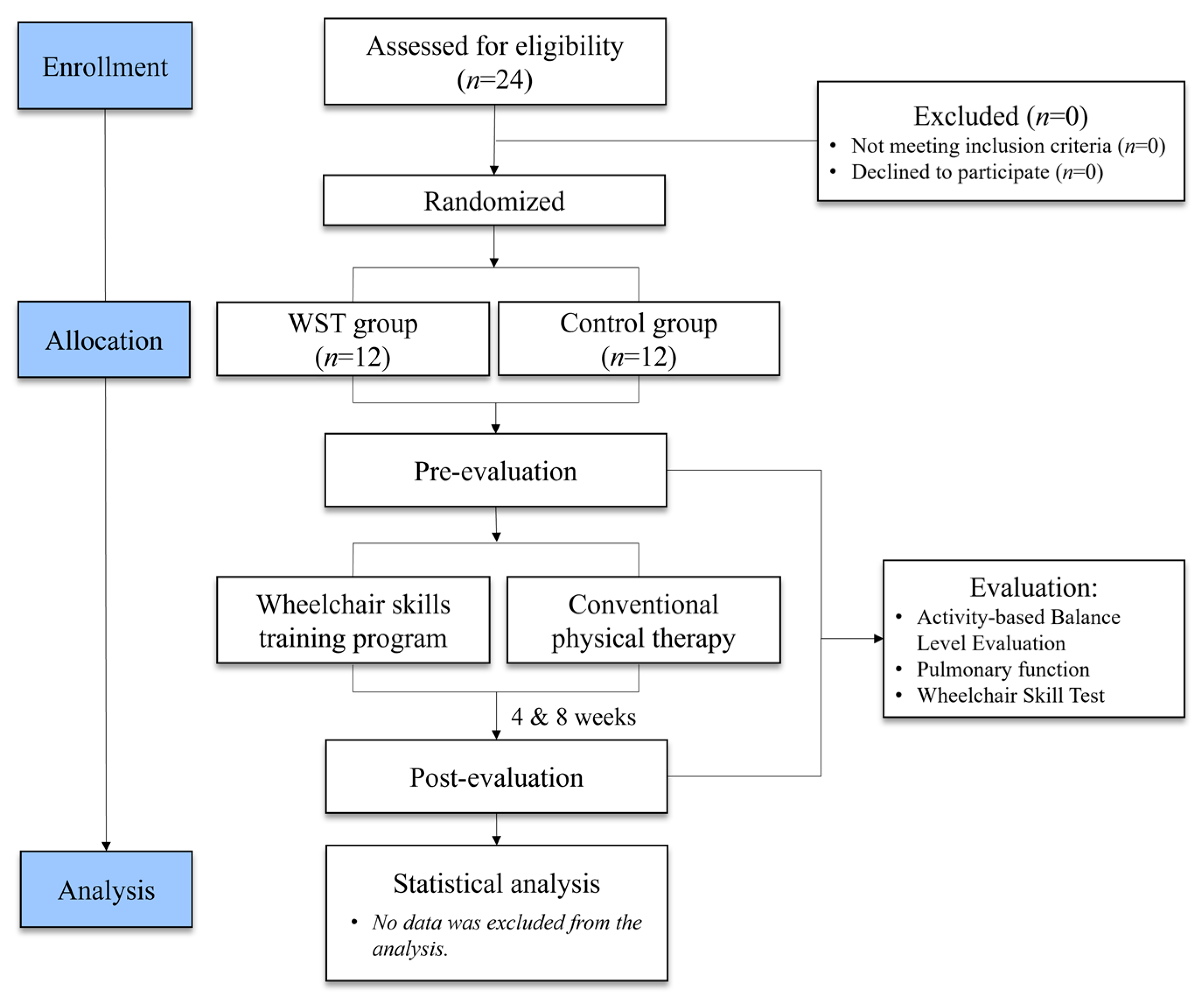
2. Materials and Methods
2.1. Subjects
2.2. Measurements
2.2.1. Activity-Based Balance Level Evaluation (ABLE)
2.2.2. Pulmonary Function
2.2.3. Wheelchair Skills Test
2.3. Interventions
Statistical Analyses
3. Results
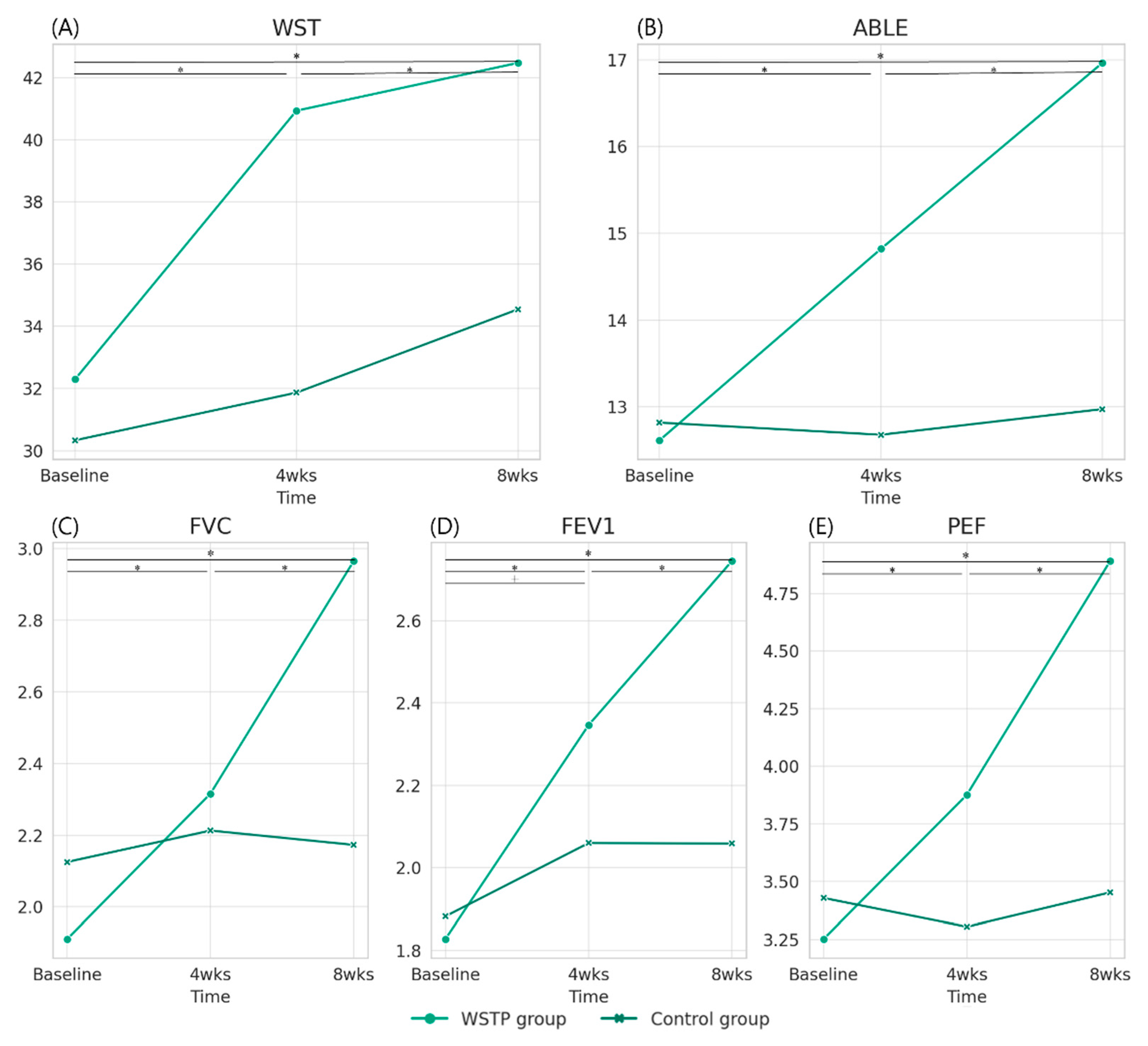
3.1. Post Hoc Pairwise Comparisons and between-Group Changes over Time
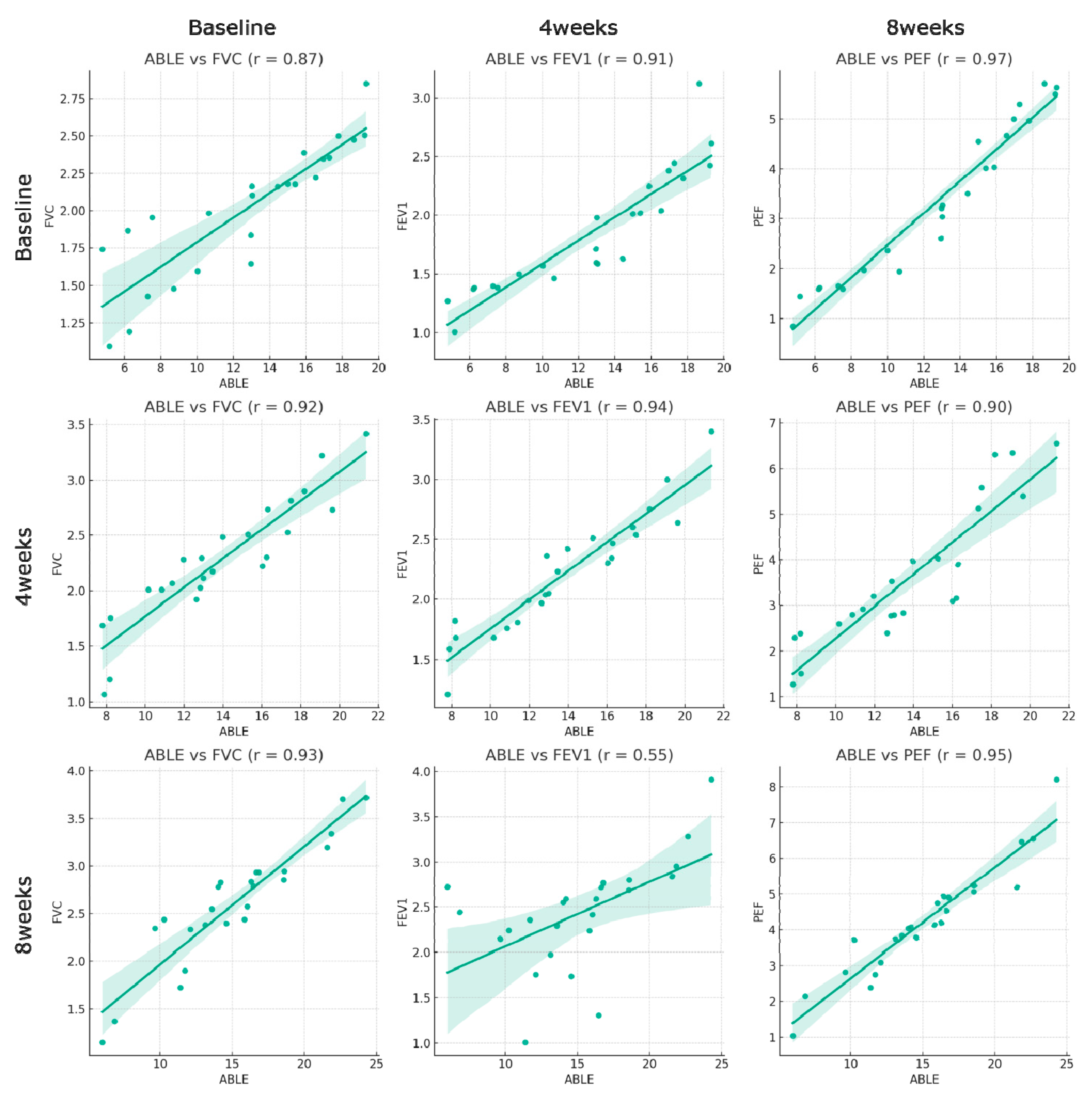
3.2. Correlation between ABLE Scores and Pulmonary Function Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sezer, N.; Akkuş, S.; Uğurlu, F.G. Chronic complications of spinal cord injury. World J. Orthop. 2015, 6, 24. [Google Scholar] [CrossRef] [PubMed]
- Dietz, V.; Fouad, K. Restoration of sensorimotor functions after spinal cord injury. Brain 2014, 137, 654–667. [Google Scholar] [CrossRef]
- Terson de Paleville, D.G.; McKay, W.B.; Folz, R.J.; Ovechkin, A.V. Respiratory motor control disrupted by spinal cord injury: Mechanisms, evaluation, and restoration. Transl. Stroke Res. 2011, 2, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.; DiMarco, A.F.; Hoit, J.D.; Garshick, E. Respiratory dysfunction and management in spinal cord injury. Respir. Care 2006, 51, 853–870. [Google Scholar] [PubMed]
- Jain, N.B.; Brown, R.; Tun, C.G.; Gagnon, D.; Garshick, E. Determinants of forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC in chronic spinal cord injury. Arch. Phys. Med. Rehabil. 2006, 87, 1327–1333. [Google Scholar] [CrossRef][Green Version]
- Schilero, G.J.; Spungen, A.M.; Bauman, W.A.; Radulovic, M.; Lesser, M. Pulmonary function and spinal cord injury. Respir. Physiol. Neurobiol. 2009, 166, 129–141. [Google Scholar] [CrossRef]
- Bluechardt, M.; Wiens, M.; Thomas, S.; Plyley, M. Repeated measurements of pulmonary function following spinal cord injury. Spinal Cord 1992, 30, 768–774. [Google Scholar] [CrossRef]
- Giannoccaro, M.P.; Moghadam, K.K.; Pizza, F.; Boriani, S.; Maraldi, N.M.; Avoni, P.; Morreale, A.; Liguori, R.; Plazzi, G. Sleep disorders in patients with spinal cord injury. Sleep Med. Rev. 2013, 17, 399–409. [Google Scholar] [CrossRef]
- Garshick, E.; Kelley, A.; Cohen, S.; Garrison, A.; Tun, C.; Gagnon, D.; Brown, R. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005, 43, 408–416. [Google Scholar] [CrossRef]
- Keeler, L.; Kirby, R.L.; Parker, K.; McLean, K.D.; Hayden, J.A. Effectiveness of the Wheelchair Skills Training Program: A systematic review and meta-analysis. Disabil. Rehabil. Assist. Technol. 2018, 14, 391–409. [Google Scholar] [CrossRef]
- Tu, C.-J.; Liu, L.; Wang, W.; Du, H.-P.; Wang, Y.-M.; Xu, Y.-B.; Li, P. Effectiveness and safety of wheelchair skills training program in improving the wheelchair skills capacity: A systematic review. Clin. Rehabil. 2017, 31, 1573–1582. [Google Scholar] [CrossRef] [PubMed]
- Lemay, V.; Routhier, F.; Noreau, L.; Phang, S.; Martin Ginis, K. Relationships between wheelchair skills, wheelchair mobility and level of injury in individuals with spinal cord injury. Spinal Cord 2012, 50, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Kirby, R.L.; Worobey, L.A.; Cowan, R.; Pedersen, J.P.; Heinemann, A.W.; Dyson-Hudson, T.A.; Shea, M.; Smith, C.; Rushton, P.W.; Boninger, M.L. Wheelchair skills capacity and performance of manual wheelchair users with spinal cord injury. Arch. Phys. Med. Rehabil. 2016, 97, 1761–1769. [Google Scholar] [CrossRef] [PubMed]
- Desroches, G.; Dumas, R.; Pradon, D.; Vaslin, P.; Lepoutre, F.-X.; Chèze, L. Upper limb joint dynamics during manual wheelchair propulsion. Clin. Biomech. 2010, 25, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.W.; Levy, C.E. Wheelchair propulsion biomechanics and wheelers’ quality of life: An exploratory review. Disabil. Rehabil. Assist. Technol. 2011, 6, 365–377. [Google Scholar] [CrossRef]
- Abd El-Kader, S.M. Impact of respiratory muscle training on blood gases and pulmonary function among patients with cervical spinal cord injury. Electron. J. Gen. Med. 2018, 15, 15–20. [Google Scholar] [CrossRef]
- Harriss, D.; MacSween, A.; Atkinson, G. Standards for ethics in sport and exercise science research: 2018 update. Int. J. Sports Med. 2017, 38, 1126–1131. [Google Scholar] [CrossRef]
- Ardolino, E.M.; Hutchinson, K.J.; Pinto Zipp, G.; Clark, M.; Harkema, S.J. The ABLE Scale: The Development and Psychometric Properties of an Outcome Measure for the Spinal Cord Injury Population. Phys. Ther. 2012, 92, 1046–1054. [Google Scholar] [CrossRef]
- Ranu, H.; Wilde, M.; Madden, B. Pulmonary function tests. Ulst. Med. J. 2011, 80, 84–90. [Google Scholar]
- Öztürk, A.; Ucsular, F.D. Effectiveness of a wheelchair skills training programme for community-living users of manual wheelchairs in Turkey: A randomized controlled trial. Clin. Rehabil. 2011, 25, 416–424. [Google Scholar] [CrossRef]
- Kirby, R.L.; Dupuis, D.J.; MacPhee, A.H.; Coolen, A.L.; Smith, C.; Best, K.L.; Newton, A.M.; Mountain, A.D.; MacLeod, D.A.; Bonaparte, J.P. The wheelchair skills test (version 2.4): Measurement properties. Arch. Phys. Med. Rehabil. 2004, 85, 794–804. [Google Scholar] [CrossRef] [PubMed]
- Wheelchair Skills Program. The Wheelchair Skills Program (WSP) Is a Set of Free Online Low-Tech, High-Impact, Evidence-Based Resources for the Assessment and Training of the Wheelchair Skills of Users (with or without the Assistance of Caregivers) of Manual Wheelchairs, Powered Wheelchairs and Motorized Mobility Scooters. Available online: https://wheelchairskillsprogram.ca (accessed on 24 August 2023).
- Lindquist, N.J.; Loudon, P.E.; Magis, T.F.; Rispin, J.E.; Kirby, R.L.; Manns, P.J. Reliability of the performance and safety scores of the wheelchair skills test version 4.1 for manual wheelchair users. Arch. Phys. Med. Rehabil. 2010, 91, 1752–1757. [Google Scholar] [CrossRef] [PubMed]
- Abou, L.; Rice, L.A. The associations of functional independence and quality of life with sitting balance and wheelchair skills among wheelchair users with spinal cord injury. J. Spinal Cord Med. 2022. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Behrman, A.L.; Ardolino, E.M.; Harkema, S.J. Activity-based therapy: From basic science to clinical application for recovery after spinal cord injury. J. Neurol. Phys. Ther. 2017, 41, S39. [Google Scholar] [CrossRef]
- Harkema, S.J.; Schmidt-Read, M.; Lorenz, D.J.; Edgerton, V.R.; Behrman, A.L. Balance and ambulation improvements in individuals with chronic incomplete spinal cord injury using locomotor training–based rehabilitation. Arch. Phys. Med. Rehabil. 2012, 93, 1508–1517. [Google Scholar] [CrossRef]
- Harness, E.; Yozbatiran, N.; Cramer, S. Effects of intense exercise in chronic spinal cord injury. Spinal Cord 2008, 46, 733–737. [Google Scholar] [CrossRef]
- Hicks, A.; Martin, K.; Ditor, D.; Latimer, A.; Craven, C.; Bugaresti, J.; McCartney, N. Long-term exercise training in persons with spinal cord injury: Effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003, 41, 34–43. [Google Scholar] [CrossRef]
- Treat-Jacobson, D.; Bronas, U.G.; Leon, A.S. Efficacy of arm-ergometry versus treadmill exercise training to improve walking distance in patients with claudication. Vasc. Med. 2009, 14, 203–213. [Google Scholar] [CrossRef]
- Jeffries, O.; Waldron, M.; Patterson, S.D.; Galna, B. An analysis of variability in power output during indoor and outdoor cycling time trials. Int. J. Sports Physiol. Perform. 2019, 14, 1273–1279. [Google Scholar] [CrossRef]
- Pi, Y.-L.; Wu, X.-H.; Wang, F.-J.; Liu, K.; Wu, Y.; Zhu, H.; Zhang, J. Motor skill learning induces brain network plasticity: A diffusion-tensor imaging study. PLoS ONE 2019, 14, e0210015. [Google Scholar] [CrossRef]
- Nieuwenhuys, A.; Oudejans, R.R. Anxiety and perceptual-motor performance: Toward an integrated model of concepts, mechanisms, and processes. Psychol. Res. 2012, 76, 747–759. [Google Scholar] [CrossRef] [PubMed]
- Covey, M.K.; McAuley, E.; Kapella, M.C.; Collins, E.G.; Alex, C.G.; Berbaum, M.L.; Larson, J.L. Upper-body resistance training and self-efficacy enhancement in COPD. J. Pulm. Respir. Med. 2012, 9, 001. [Google Scholar]
- De Troyer, A.; Moxham, J. Chest Wall and Respiratory Muscles. In Cotes’ Lung Function; Wiley: Hoboken, NJ, USA, 2020; pp. 149–176. [Google Scholar]
- Singh, V.; Jani, H.; John, V.; Singh, P.; Joseley, T. Effects of upper body resistance training on pulmonary functions in sedentary male smokers. Lung India Off. Organ Indian Chest Soc. 2011, 28, 169. [Google Scholar] [CrossRef]
- Park, S.J. Effects of inspiratory muscles training plus rib cage mobilization on chest expansion, inspiratory accessory muscles activity and pulmonary function in stroke patients. Appl. Sci. 2020, 10, 5178. [Google Scholar] [CrossRef]
- Raab, A.M.; Krebs, J.; Pfister, M.; Perret, C.; Hopman, M.; Mueller, G. Respiratory muscle training in individuals with spinal cord injury: Effect of training intensity and-volume on improvements in respiratory muscle strength. Spinal Cord 2019, 57, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Tarigan, A.P.; Ananda, F.R.; Pandia, P.; Sinaga, B.Y.; Maryaningsih, M.; Anggriani, A. The impact of upper limb training with breathing maneuver in lung function, functional capacity, dyspnea scale, and quality of life in patient with stable chronic obstructive of lung disease. Open Access Maced. J. Med. Sci. 2019, 7, 567. [Google Scholar] [CrossRef]
- Clark, C.; Cochrane, L.; Mackay, E.; Paton, B. Skeletal muscle strength and endurance in patients with mild COPD and the effects of weight training. Eur. Respir. J. 2000, 15, 92–97. [Google Scholar] [CrossRef]
- Shin, J.C.; Han, E.Y.; Cho, K.H.; Im, S.H. Improvement in pulmonary function with short-term rehabilitation treatment in spinal cord injury patients. Sci. Rep. 2019, 9, 17091. [Google Scholar] [CrossRef]
- Nooijen, C.F.; de Groot, S.; Postma, K.; Bergen, M.P.; Stam, H.J.; Bussmann, J.; Van den Berg-Emons, R. A more active lifestyle in persons with a recent spinal cord injury benefits physical fitness and health. Spinal Cord 2012, 50, 320–323. [Google Scholar] [CrossRef]
- Crawford, A.; Hollingsworth, H.H.; Morgan, K.; Gray, D.B. People with mobility impairments: Physical activity and quality of participation. Disabil. Health J. 2008, 1, 7–13. [Google Scholar] [CrossRef]
- Kilkens, O.J.; Dallmeijer, A.J.; Nene, A.V.; Post, M.W.; van der Woude, L.H. The longitudinal relation between physical capacity and wheelchair skill performance during inpatient rehabilitation of people with spinal cord injury. Arch. Phys. Med. Rehabil. 2005, 86, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Durán, F.S.; Lugo, L.; Ramírez, L.; Lic, E.E. Effects of an exercise program on the rehabilitation of patients with spinal cord injury. Arch. Phys. Med. Rehabil. 2001, 82, 1349–1354. [Google Scholar] [CrossRef] [PubMed]
| WSTP Group | Control Group | |
|---|---|---|
| Age (years) | 36.02 (7.16) | 35.81 (4.51) |
| Gender (male/female) | 9/3 | 8/4 |
| Height (cm) | 167.20 (8.93) | 166.50 (7.07) |
| Weight (kg) | 64.52 (7.94) | 64.27 (4.69) |
| SCI level (C5-C6/C7-T1) | 7/5 | 6/6 |
| ASIA scale (B/C) | 6/6 | 5/7 |
| Post-injury period (months) | 34.92 (8.35) | 36.41 (9.19) |
| Wheelchair-dependent period (months) | 34.22 (8.56) | 35.66 (6.58) |
| Variables | Group | Baseline | 4 Weeks | 8 Weeks | F(p) | Post Hoc Analysis (Mean Difference) | |||
|---|---|---|---|---|---|---|---|---|---|
| Group | Time | Interaction (Group × Time) | Baseline to 4 Weeks | Baseline to 8 Weeks | |||||
| WST (score) | WSTP | 32.30 (6.84) | 40.93 (8.07) | 42.47 (7.73) | 5.41 * (0.03) | 12.56 * (<0.01) | 3.51 * (0.04) | W > C | W > C |
| Control | 30.34 (6.33) | 31.87 (6.41) | 34.56 (9.04) | ||||||
| ABLE (score) | WSTP | 12.62 (1.34) | 14.82 (1.07) | 16.96 (1.21) | 1.27 (0.27) | 52.57 * (<0.01) | 41.78 * (<0.01) | W > C | W > C |
| Control | 12.82 (1.46) | 12.68 (1.16) | 12.98 (1.31) | ||||||
| FVC (L) | WSTP | 1.91 (0.12) | 2.32 (0.16) | 2.97 (0.14) | 1.34 (0.26) | 52.21 * (<0.01) | 38.71 * (<0.01) | W > C | W > C |
| Control | 2.13 (0.13) | 2.21 (0.17) | 2.17 (0.15) | ||||||
| FEV1 (L) | WSTP | 1.83 (0.15) | 2.35 (0.13) | 2.75 (0.14) | 2.90 (0.10) | 41.02 * (<0.01) | 11.79 * (<0.01) | W > C | W > C |
| Control | 1.88 (0.16) | 2.06 (0.15) | 2.06 (0.15) | ||||||
| PEF (L) | WSTP | 3.25 (0.44) | 3.88 (0.42) | 4.89 (0.38) | 1.03 (0.32) | 33.87 * (<0.01) | 29.71 * (<0.01) | W > C | W > C |
| Control | 3.43 (0.48) | 3.31 (0.46) | 3.45 (0.42) | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, S.-M.; Koo, D.-K.; Kwon, J.-W. Efficacy of Wheelchair Skills Training Program in Enhancing Sitting Balance and Pulmonary Function in Chronic Tetraplegic Patients: A Randomized Controlled Study. Medicina 2023, 59, 1610. https://doi.org/10.3390/medicina59091610
Nam S-M, Koo D-K, Kwon J-W. Efficacy of Wheelchair Skills Training Program in Enhancing Sitting Balance and Pulmonary Function in Chronic Tetraplegic Patients: A Randomized Controlled Study. Medicina. 2023; 59(9):1610. https://doi.org/10.3390/medicina59091610
Chicago/Turabian StyleNam, Seung-Min, Dong-Kyun Koo, and Jung-Won Kwon. 2023. "Efficacy of Wheelchair Skills Training Program in Enhancing Sitting Balance and Pulmonary Function in Chronic Tetraplegic Patients: A Randomized Controlled Study" Medicina 59, no. 9: 1610. https://doi.org/10.3390/medicina59091610
APA StyleNam, S.-M., Koo, D.-K., & Kwon, J.-W. (2023). Efficacy of Wheelchair Skills Training Program in Enhancing Sitting Balance and Pulmonary Function in Chronic Tetraplegic Patients: A Randomized Controlled Study. Medicina, 59(9), 1610. https://doi.org/10.3390/medicina59091610






