The Association of Severe Coronary Tortuosity and Non-Obstructive Coronary Artery Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Procedures
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schumann, C.L.; Mathew, R.C.; Dean, J.L.; Yang, Y.; Balfour, P.C., Jr.; Shaw, P.W.; Robinson, A.A.; Salerno, M.; Kramer, C.M.; Bourque, J.M. Functional and Economic Impact of INOCA and Influence of Coronary Microvascular Dysfunction. JACC Cardiovasc. Imaging 2021, 14, 1369–1379. [Google Scholar] [CrossRef]
- Patel, M.R.; Peterson, E.D.; Dai, D.; Brennan, J.M.; Redberg, R.F.; Anderson, H.V.; Brindis, R.G.; Douglas, P.S. Low diagnostic yield of elective coronary angiography. N. Engl. J. Med. 2010, 362, 886–895. [Google Scholar] [CrossRef]
- Kunadian, V.; Chieffo, A.; Camici, P.G.; Berry, C.; Escaned, J.; Maas, A.H.E.M.; Prescott, E.; Karam, N.; Appelman, Y.; Fraccaro, C.; et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur. Heart J. 2020, 41, 3504–3520. [Google Scholar] [CrossRef]
- Estrada, A.; Sousa, A.S.; Mesquita, C.T.; Villacorta, H. Coronary Tortuosity as a New Phenotype for Ischemia without Coronary Artery Disease. Arq. Bras. Cardiol. 2022, 119, 883–890. [Google Scholar] [CrossRef]
- Jespersen, L.; Hvelplund, A.; Abildstrøm, S.Z.; Pedersen, F.; Galatius, S.; Madsen, J.K.; Jørgensen, E.; Kelbæk, H.; Prescott, E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur. Heart J. 2012, 33, 734–744. [Google Scholar] [CrossRef]
- Chiha, J.; Mitchell, P.; Gopinath, B.; Burlutsky, G.; Kovoor, P.; Thiagalingam, A. Gender differences in the prevalence of coronary artery tortuosity and its association with coronary artery disease. Int. J. Cardiol. Heart Vasc. 2016, 14, 23–27. [Google Scholar] [CrossRef]
- Zegers, E.S.; Meursing, B.T.; Zegers, E.B.; Oude Ophuis, A.J. Coronary tortuosity: A long and winding road. Neth. Heart J. 2007, 15, 191–195. [Google Scholar] [CrossRef]
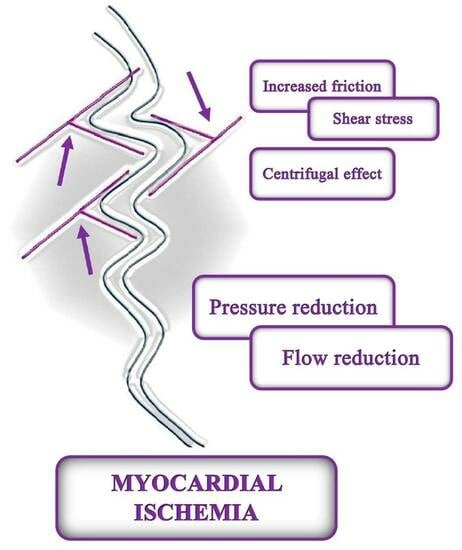
- Li, Y.; Shi, Z.; Cai, Y.; Feng, Y.; Ma, G.; Shen, C.; Li, Z.; Liu, N. Impact of coronary tortuosity on coronary pressure: Numerical simulation study. PLoS ONE 2012, 7, e42558. [Google Scholar] [CrossRef]
- Vorobtsova, N.; Chiastra, C.; Stremler, M.A.; Sane, D.C.; Migliavacca, F.; Vlachos, P. Effects of Vessel Tortuosity on Coronary Hemodynamics: An Idealized and Patient-Specific Computational Study. Ann. Biomed. Eng. 2016, 44, 2228–2239. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Zaacks, S.M.; Allen, J.E.; Calvin, J.E.; Schaer, G.L.; Palvas, B.W.; Parrillo, J.E.; Klein, L.W. Value of the American College of Cardiology/American Heart Association stenosis morphology classification for coronary interventions in the late 1990s. Am. J. Cardiol. 1998, 82, 43–49. [Google Scholar] [CrossRef]
- Muhyieddeen, A.; Wei, J.; Cui, Y.; Pepine, C.J.; Handberg, E.; Bairey Merz, N. Association of Coronary Artery Dominance With Long-term Outcomes in Female Patients With Suspected Ischemia but Nonobstructive Coronary Artery Disease. JSCAI 2023. [Google Scholar] [CrossRef]
- Ya’qoub, L.; Elgendy, I.Y.; Pepine, C.J. Syndrome of Nonobstructive Coronary Artery Diseases: A Comprehensive Overview of Open Artery Ischemia. Am. J. Med. 2021, 134, 1321–1329. [Google Scholar] [CrossRef]
- Pepine, C.J.; Anderson, R.D.; Sharaf, B.L.; Reis, S.E.; Smith, K.M.; Handberg, E.M.; Johnson, B.D.; Sopko, G.; Bairey Merz, C.N. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J. Am. Coll. Cardiol. 2010, 55, 2825–2832. [Google Scholar] [CrossRef]
- Chiha, J.; Mitchell, P.; Gopinath, B.; Plant, A.J.H.; Kovoor, P.; Thiagalingam, A. Gender differences in the severity and extent of coronary artery disease. Int. J. Cardiol. Heart Vasc. 2015, 8, 161–166. [Google Scholar] [CrossRef]
- Sharaf, B.; Wood, T.; Shaw, L.; Johnson, B.D.; Kelsey, S.; Anderson, R.D.; Pepine, C.J.; Bairey Merz, C.N. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: Findings from the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation (WISE) angiographic core laboratory. Am. Heart J. 2013, 166, 134–141. [Google Scholar] [CrossRef]
- Ganguly, P.; Alam, S.F. Role of homocysteine in the development of cardiovascular disease. Nutr. J. 2015, 14, 6. [Google Scholar] [CrossRef]
- Wu, H.Y.; Gao, T.J.; Cao, Y.W.; Diao, J.Y.; You, P.H.; Yao, X.W. Analysis of the association and predictive value of hyperhomocysteinaemia for obstructive coronary artery disease. J. Int. Med. Res. 2021, 49, 3000605211033495. [Google Scholar] [CrossRef]
- Gaibazzi, N.; Rigo, F.; Reverberi, C. Severe coronary tortuosity or myocardial bridging in patients with chest pain, normal coronary arteries, and reversible myocardial perfusion defects. Am. J. Cardiol. 2011, 108, 973–978. [Google Scholar] [CrossRef]
- Mihai, D.E.; Lupasteanu, I.; Dan, G.A. Impact of coronary artery tortuosity in ischemic and non-ischemic cardiovascular pathology. Rom. J. Intern. Med. 2021, 59, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Shen, C.; Ji, Y.; Feng, Y.; Ma, G.; Liu, N. Clinical implication of coronary tortuosity in patients with coronary artery disease. PLoS ONE 2011, 6, e24232. [Google Scholar] [CrossRef] [PubMed]
- Eleid, M.F.; Guddeti, R.R.; Tweet, M.S.; Lerman, A.; Singh, M.; Best, P.J.; Vrtiska, T.J.; Prasad, M.; Rihal, C.S.; Hayes, S.N.; et al. Coronary artery tortuosity in spontaneous coronary artery dissection: Angiographic characteristics and clinical implications. Circ. Cardiovasc. Interv. 2014, 7, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Hassanin Hanboly, N.; Ghany Abdel, M.M.; El-Kaffas Helmy, S.M.; Ahmed Udden, T. Prevalence, risk factors, and coronary angiographic profile in patients with tortuous coronary artery. Cor Vasa 2021, 63, 547–554. [Google Scholar] [CrossRef]
- Turgut, O.; Yilmaz, A.; Yalta, K.; Yilmaz, B.M.; Ozyol, A.; Kendirlioglu, O.; Karadas, F.; Tandogan, I. Tortuosity of coronary arteries: An indicator for impaired left ventricular relaxation? Int. J. Cardiovasc. Imaging 2007, 23, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Makarovic, Z.; Makarovic, S.; Bilic-Curcic, I. Sex-dependent association between coronary vessel dominance and cardiac syndrome X: A case-control study. BMC Cardiovasc. Disord. 2014, 14, 142. [Google Scholar] [CrossRef] [PubMed]
- Esfahani, M.; Farzamnia, H.; Nezarat, N. Chronic Stable Angina Patients with Tortuous Coronary Arteries: Clinical Symptoms and Risk Factors. ARYA Atheroscler. J. 2012, 7, 115–118. [Google Scholar]
- Hutchins, G.M.; Bulkley, B.H.; Miner, M.M.; Boitnott, J.K. Correlation of age and heart weight with tortuosity and caliber of normal human coronary arteries. Am. Heart J. 1977, 94, 196–202. [Google Scholar] [CrossRef]
- Jakob, M.; Spasojevic, D.; Krogmann, O.N.; Wiher, H.; Hug, R.; Hess, O.M. Tortuosity of coronary arteries in chronic pressure and volume overload. Catheter. Cardiovasc. Interv. 1996, 38, 25–31. [Google Scholar] [CrossRef]
- Groves, S.S.; Jain, A.C.; Warden, B.E.; Gharib, W.; Beto, R.J., 2nd. Severe coronary tortuosity and the relationship to significant coronary artery disease. West Va. Med. J. 2009, 105, 14–17. [Google Scholar]
- El Tahlawi, M.; Sakrana, A.; Elmurr, A.; Gouda, M.; Tharwat, M. The Relation between coronary tortuosity and Calcium Score in Patients with Chronic Stable Angina and Normal Coronaries by CT angiography. Atherosclerosis 2016, 246, 334–337. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wingert, A.; Wang, J.; Zhang, J.; Wang, X.; Sun, J.; Chen, F.; Khalid, S.G.; Jiang, J.; Zheng, D. Extraction of Coronary Atherosclerotic Plaques From Computed Tomography Imaging: A Review of Recent Methods. Front. Cardiovasc. Med. 2021, 8, 597568. [Google Scholar] [CrossRef]
- Li, Y.; Feng, Y.; Ma, G.; Shen, C.; Liu, N. Coronary tortuosity is negatively correlated with coronary atherosclerosis. J. Int. Med. Res. 2018, 46, 5205–5209. [Google Scholar] [CrossRef] [PubMed]
- Khosravani-Rudpishi, M.; Joharimoghadam, A.; Rayzan, E. The significant coronary tortuosity and atherosclerotic coronary artery disease; What is the relation? J. Cardiovasc. Thorac. Res. 2018, 10, 209–213. [Google Scholar] [CrossRef]
- Geng, Y.; Liu, H.; Wang, X.; Zhang, J.; Gong, Y.; Zheng, D.; Jiang, J.; Xia, L. Effect of microcirculatory dysfunction on coronary hemodynamics: A pilot study based on computational fluid dynamics simulation. Comput. Biol. Med. 2022, 146, 105583. [Google Scholar] [CrossRef]
- Geng, Y.; Wu, X.; Liu, H.; Zheng, D.; Xia, L. Index of microcirculatory resistance: State-of-the-art and potential applications in computational simulation of coronary artery disease. J. Zhejiang Univ. Sci. B 2022, 23, 123–140. [Google Scholar] [CrossRef]
- Madias, J.E. A proposal of a new index of coronary microvascular resistance based on the duration of the transient ECG repolarization changes during coronary angiography. Int. J. Cardiovasc. Imaging 2023, 39, 1075–1077. [Google Scholar] [CrossRef]
- Zhang, J.; Ma, M.; Li, H.; Pu, Z.; Liu, H.; Huang, T.; Cheng, H.; Gong, Y.; Chu, Y.; Wang, Z.; et al. Early diagnosis of coronary microvascular dysfunction by myocardial contrast stress echocardiography. Math. Biosci. Eng. 2023, 20, 7845–7858. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, J.; Gong, Y.; Xu, L.; Liu, H.; Wei, S.; Wu, Y.; Cha, G.; Wei, H.; Mao, J.; et al. Reliable Detection of Myocardial Ischemia Using Machine Learning Based on Temporal-Spatial Characteristics of Electrocardiogram and Vectorcardiogram. Front. Physiol. 2022, 13, 854191. [Google Scholar] [CrossRef]


| Variable | Group | Statistics | |
|---|---|---|---|
| Non-Obstructive CAD (N = 77) | Obstructive CAD (N = 54) | ||
| Female sex; N (%) | 47 (61) | 13 (24) | χ2 = 17.3, p < 0.001 |
| Age, years; M (IQR) | 63 (55–69) | 62 (57–68) | 0.929 * |
| Height, m; M (IQR) | 1.67 (1.62–1.77) | 1.71 (1.65–1.78) | 0.184 * |
| Weight, kg; M (IQR) | 80 (68–93.25) | 85 (76–95) | 0.169 * |
| BMI, kgm−2; M (IQR) | 27.77 (25.95–31.53) | 29.31 (26.51–31.77) | 0.285 * |
| Smoking; N (%) Non-smokers Smokers | 59 (76.6) 18 (23.4) | 32 (59.3) 22 (40.7) | χ2 = 4.5, p = 0.034 |
| History; N (%) Alcohol DM HTA HLP FH | 4 (5.2) 17 (22.1) 61 (79.2) 32 (41.6) 38 (49.4) | 3 (5.6) 20 (37.0) 41 (75.9) 29 (53.7) 21 (38.9) | χ2 = 0.01, p = 0.928 χ2 = 3.5, p = 0.062 χ2 = 0.2, p = 0.656 χ2 = 1.9, p = 0.172 χ2 = 1.4, p = 0.238 |
| Dg of referral; N (%) CCS ACS | 55 (71.4) 22 (28.6) | 14 (25.9) 40 (74.1) | χ2 = 26.2, p < 0.001 |
| Variable | Group | Statistics | |
|---|---|---|---|
| Non-Obstructive CAD (N = 77) | Obstructive CAD (N = 54) | ||
| Cholesterol level, mmol/L; M (IQR) Increased; N (%) | 4.65 (3.63–5.43) 27 (35.1) | 4.66 (3.92–5.75) 22 (40.7) | p = 0.310 * χ2 = 0.43, p = 0.510 |
| HDL level, mmol/L; M (IQR) Low; N (%) | 1.26 (1.02–1.49) 17 (22.1) | 1.08 (0.96–1.34) 20 (37.0) | p = 0.019 * χ2 = 3.48, p = 0.062 |
| HDL/C, %; M (IQR) Low; N (%) | 27 (23–34.25) 6 (7.8) | 23 (20–27) 18 (33.3) | p < 0.001 * χ2 = 13.73, p < 0.001 |
| LDL level, mmol/L; M (IQR) Increased; N (%) | 2.88 (2.08–3.64) 75 (97.4) | 3.19 (2.57–3.83) 53 (98.1) | p = 0.057 * χ2 = 0.08, p = 0.780 |
| Triglycerides level, mmol/L; M (IQR) Increased; N (%) | 1.04 (0.67–1.42) 15 (19.5) | 1.54 (1.29–1.98) 21 (38.9) | p < 0.001 * χ2 = 5.95, p = 0.015 |
| Homocysteine level; M (IQR) Increased; N (%) | 10 (8.75–12.0) 10 (13.0) | 11 (10.0–14.0) 10 (18.5) | p = 0.014 * χ2 = 0.75, p = 0.388 |
| Group | Statistics | ||
|---|---|---|---|
| Variable | Non-Obstructive CAD (N = 77) | Obstructive CAD (N = 54) | |
| Tortuous coronary artery; N (%) LCX LAD RCA | 39 (50.6) 27 (35.1) 21 (27.3) 9 (11.7) | 8 (14.8) 5 (9.3) 6 (11.1) 0 (0.0) | χ2 = 17.6, p < 0.001 χ2 = 11.4, p < 0.001 χ2 = 5.03, p = 0.025 χ2 = 6.73, p = 0.010 |
| Type of coronary artery blood supply; N (%) Left Right Mixed | 29 (37.7) 46 (59.7) 2 (2.6) | 9 (16.7) 38 (70.4) 7 (13.0) | χ2 = 10.3, p = 0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zebic Mihic, P.; Saric, S.; Bilic Curcic, I.; Mihaljevic, I.; Juric, I. The Association of Severe Coronary Tortuosity and Non-Obstructive Coronary Artery Disease. Medicina 2023, 59, 1619. https://doi.org/10.3390/medicina59091619
Zebic Mihic P, Saric S, Bilic Curcic I, Mihaljevic I, Juric I. The Association of Severe Coronary Tortuosity and Non-Obstructive Coronary Artery Disease. Medicina. 2023; 59(9):1619. https://doi.org/10.3390/medicina59091619
Chicago/Turabian StyleZebic Mihic, Petra, Sandra Saric, Ines Bilic Curcic, Ivan Mihaljevic, and Iva Juric. 2023. "The Association of Severe Coronary Tortuosity and Non-Obstructive Coronary Artery Disease" Medicina 59, no. 9: 1619. https://doi.org/10.3390/medicina59091619
APA StyleZebic Mihic, P., Saric, S., Bilic Curcic, I., Mihaljevic, I., & Juric, I. (2023). The Association of Severe Coronary Tortuosity and Non-Obstructive Coronary Artery Disease. Medicina, 59(9), 1619. https://doi.org/10.3390/medicina59091619