Does the Type of Knee Arthroplasty Affect the Patient’s Postural Stability?
Abstract
:1. Introduction
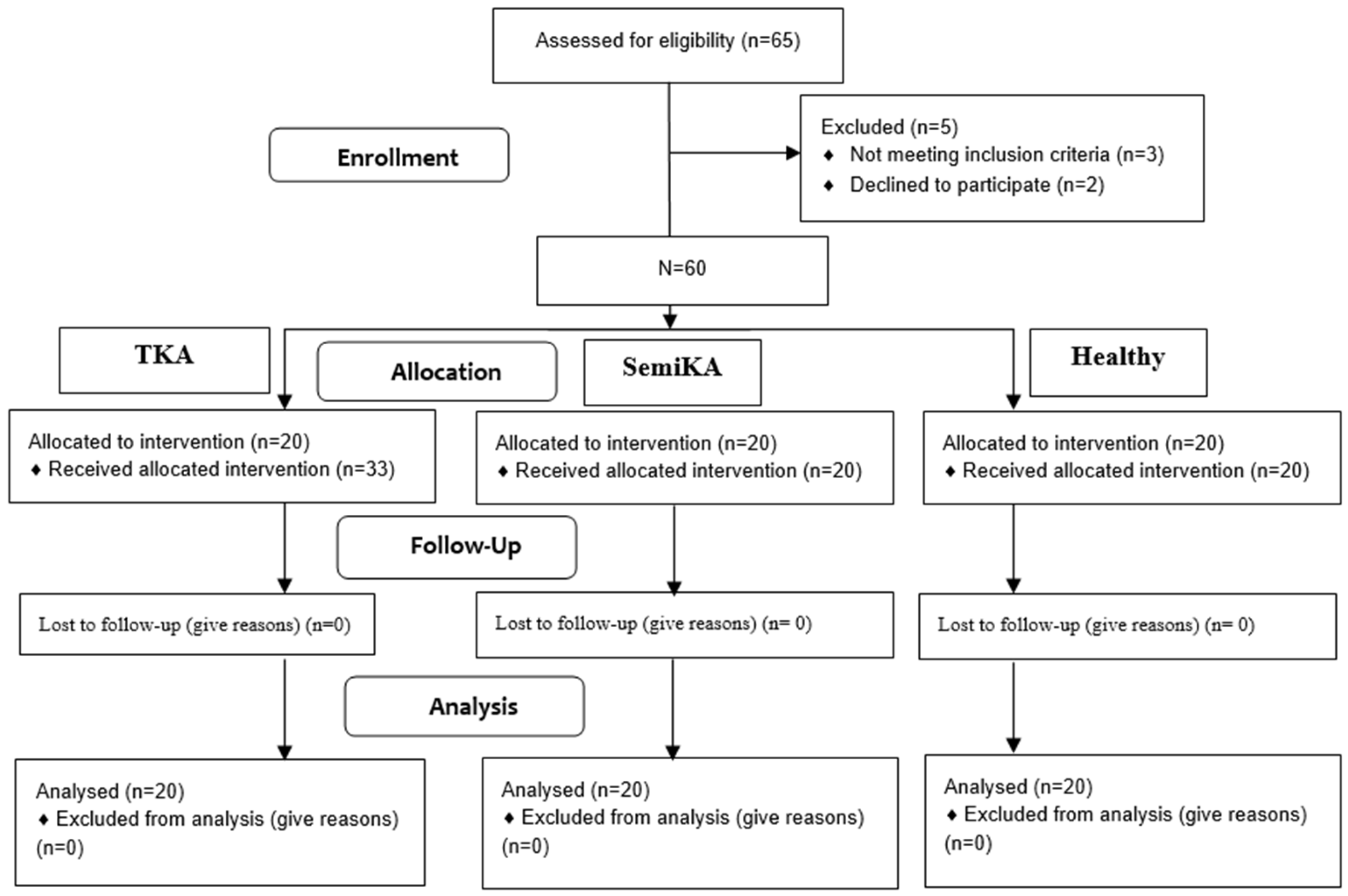
2. Materials and Methods
2.1. Study Design
2.2. Participants
- Undergoing TKA procedure or UKA implantation due to knee osteoarthritis;
- Absence of other diseases or injuries of the lower limbs;
- Absence of neurological conditions that could affect the study results;
- Ability to move independently after the surgery (without the use of orthopedic aids).
- Inflammatory conditions and acute pain in the lower limbs;
- Lack of written consent from the patient to participate in the study.
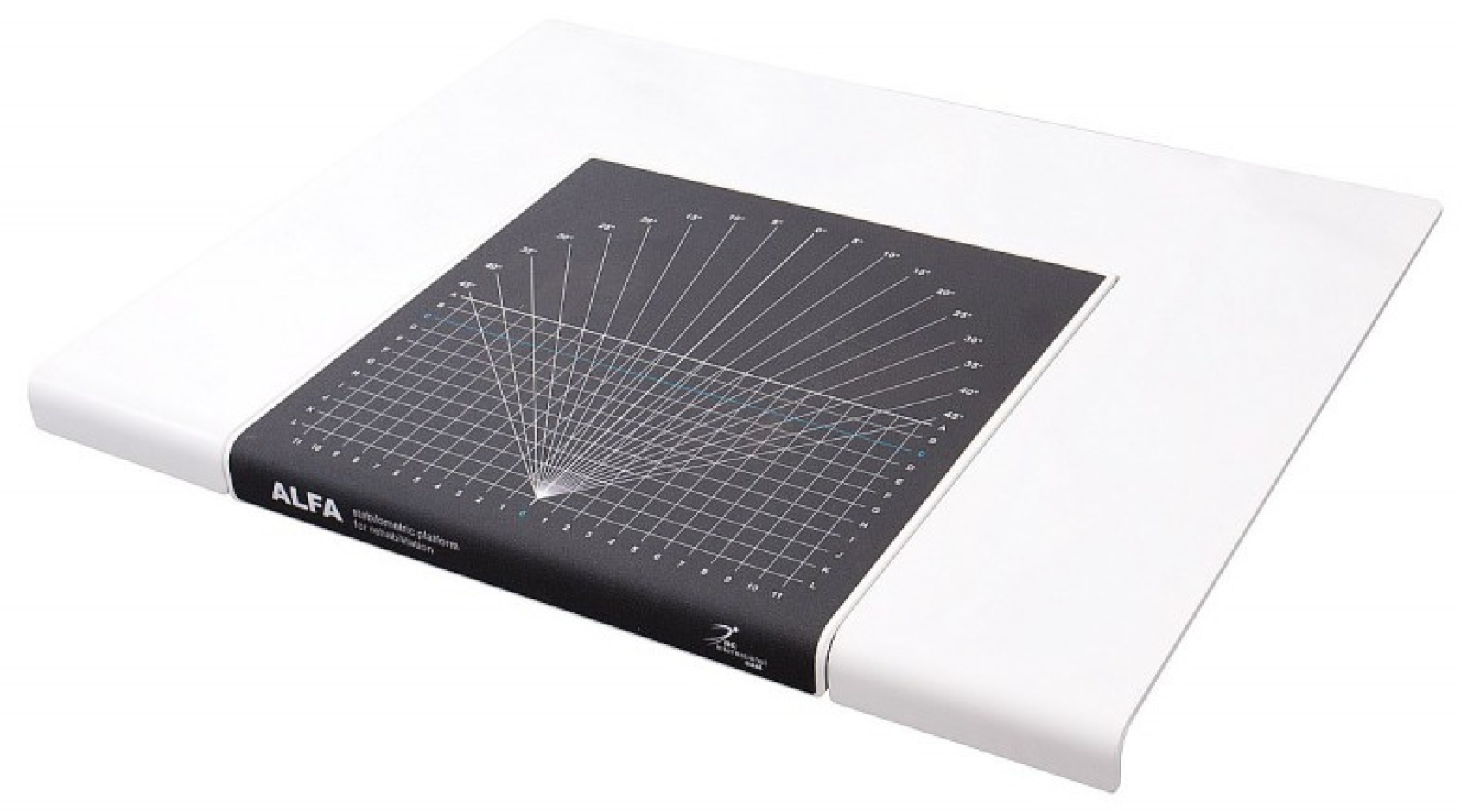
2.3. Setting
2.4. Outcome Measures
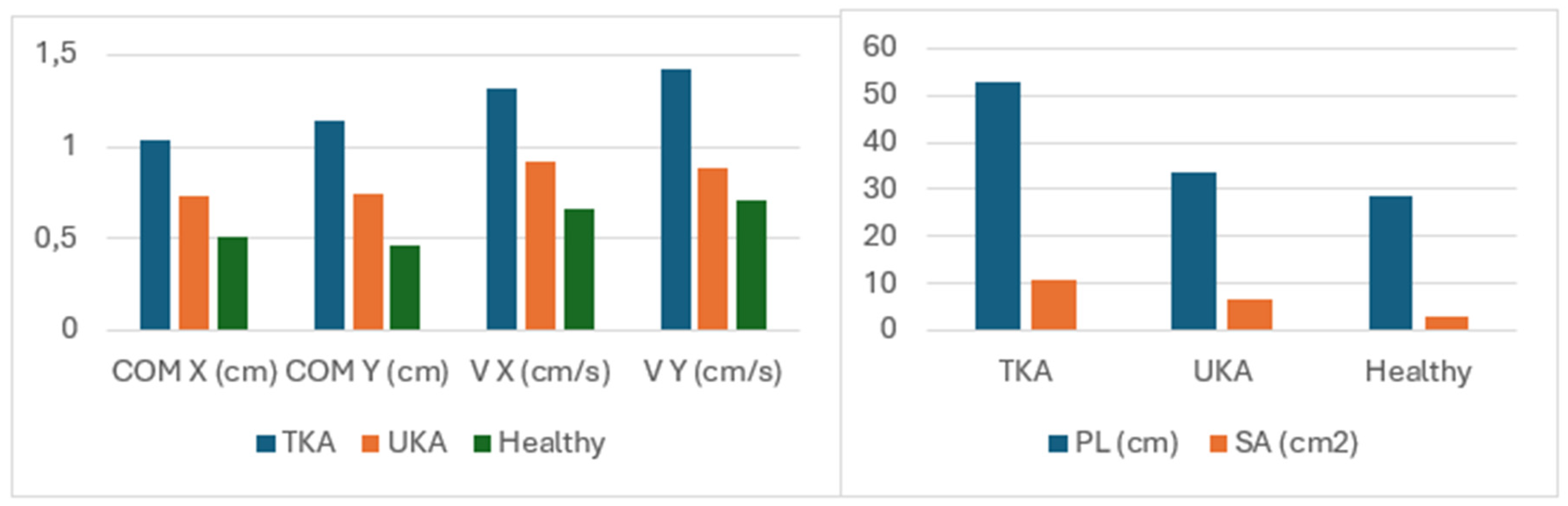
- In the Romberg’s test:
- ○
- COM X—average deviation on the X-axis (cm);
- ○
- COM Y—average deviation on the Y-axis (cm);
- ○
- V X—average velocity X (cm/s);
- ○
- V Y—average velocity Y (cm/s);
- ○
- PL—path length of COM (cm);
- ○
- SA—surface area (cm2).
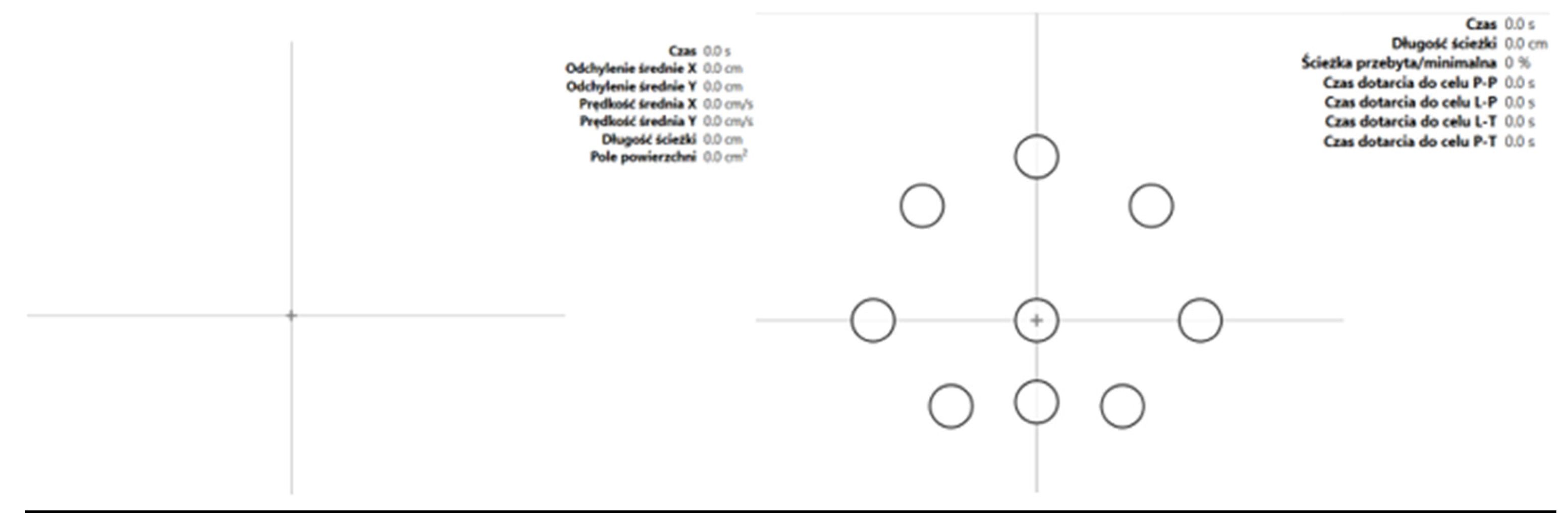
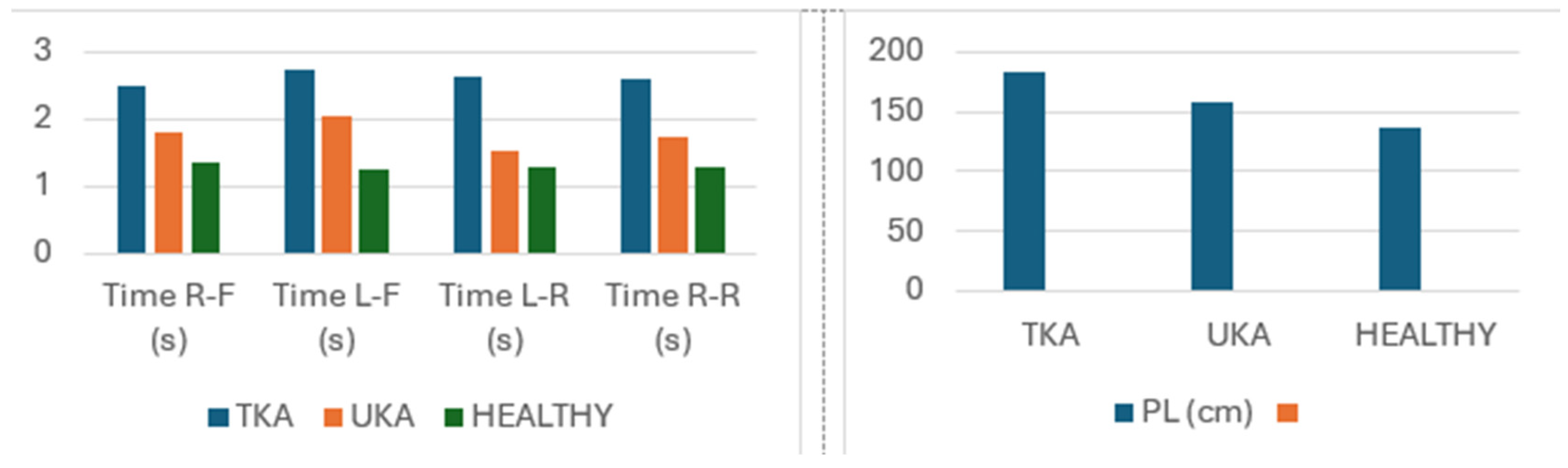
- In the dynamic test:
- ○
- Time R-F—time to reach target right front (s);
- ○
- Time L-F—time to reach target left front (s);
- ○
- Time L-R—time to reach target left rear (s);
- ○
- Time R-R—time to reach target right rear (s);
- ○
- PL—path length (cm).
Clinical Examination
2.5. Statistical Analysis
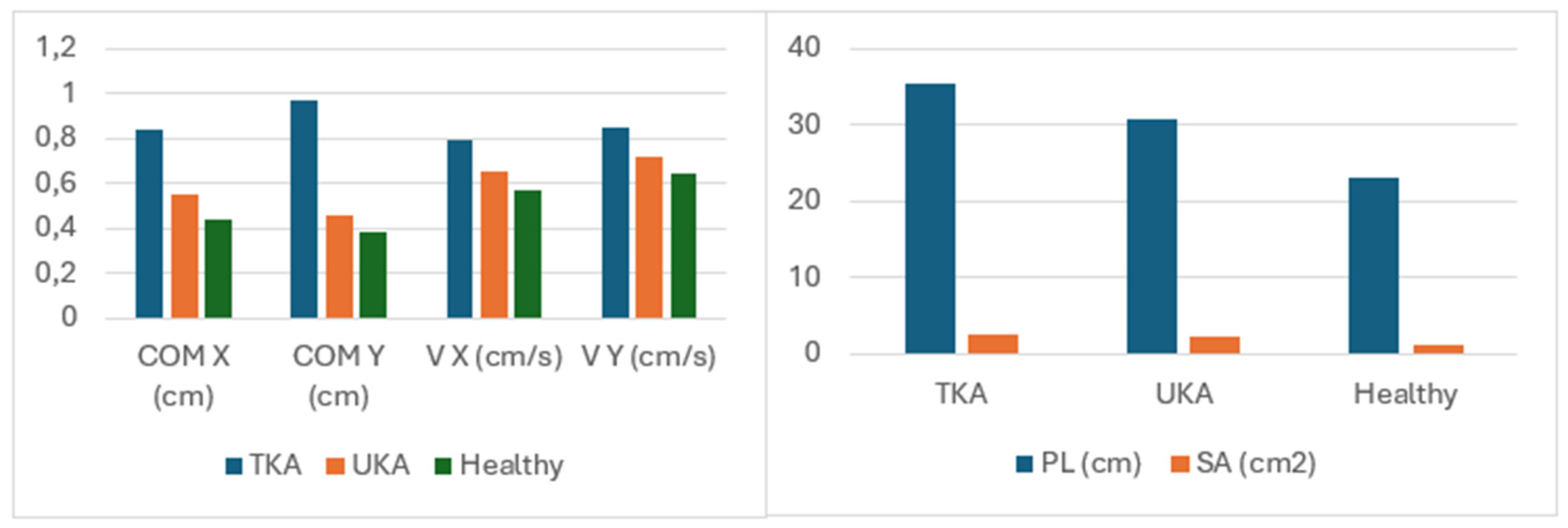
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anand, V.J.; Buckley, G.; Scally, A.; Elliott, D.B. Postural stability in the elderly during sensory perturbations and dual tasking: The influence of refractive blur. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2885–2891. [Google Scholar] [CrossRef] [PubMed]
- Kuczyński, M.; Podbielska, M.L.; Bieć, D.; Paluszak, A.; Kręcisz, K. The basics of postural control assessment: What, how and why do we need to measure? Acta Bio-Opt. Inform. Medica 2012, 4, 243–249. [Google Scholar]
- Błaszczyk, J.W.; Orawiec, R. Assessment of postural control in patients with Parkinson’s disease: Sway ratio analysis. Hum. Mov. Sci. 2011, 30, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Bove, M.; Nardone, A.; Schieppati, M. Effects of leg muscle tendon vibration on group Ia and group II reflex responses to stance perturbation in humans. J. Physiol. 2003, 550, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Goliwąs, M.; Kamińska, E.; Flis-Masłowska, M.; Wiernicka, M.; Lewandowski, J. Balance Versus Postural Stability and Its Disorders in Patients after Ischemic Stroke–Theoretical Study. Pol. J. Physiother. 2017, 17, 38–44. [Google Scholar]
- Błaszczyk, J. Control of body posture stability. Kosmos 1993, 42, 473–486. [Google Scholar]
- Roberts, B.C.; Solomon, L.B.; Mercer, G.; Reynolds, K.; Thewlis, D.; Perilli, E. Relationships between in vivo dynamic knee joint loading, static alignment and tibial subchondral bone microarchitecture in end-stage knee osteoarthritis. Osteoarthr. Cartil. 2018, 26, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Gilat, R.; Haunschild, E.D.; Patel, S.; Yang, J.; DeBenedetti, A.; Yanke, A.B.; Della Valle, C.J.; Cole, B.J. Understanding the difference between symptoms of focal cartilage defects and osteoarthritis of the knee: A matched cohort analysis. Int. Orthop. 2021, 45, 1761–1766. [Google Scholar] [CrossRef]
- Wang, W.L.; Rondon, A.J.; Tan, T.L.; Wilsman, J.; Purtill, J.J. Self-directed home exercises vs outpatient physical therapy after total knee arthroplasty: Value and outcomes following a protocol change. J. Arthroplast. 2019, 34, 2388–2391. [Google Scholar] [CrossRef]
- Palazzuolo, M.; Antoniadis, A.; Mahlouly, J.; Wegrzyn, J. Total knee arthroplasty improves the quality-adjusted life years in patients who exceeded their estimated life expectancy. Int. Orthop. 2021, 45, 635–641. [Google Scholar] [CrossRef]
- Chan, A.C.; Jehu, D.A.; Pang, M.Y. Falls after total knee arthroplasty: Frequency, circumstances, and associated factors—A prospective cohort study. Phys. Ther. 2018, 98, 767–778. [Google Scholar] [CrossRef] [PubMed]
- Canovas, F.; Dagneaux, L. Quality of life after total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2018, 104, S41–S46. [Google Scholar] [CrossRef]
- Taniguchi, M.; Sawano, S.; Maegawa, S.; Ikezoe, T.; Ichihashi, N. Physical activity mediates the relationship between gait function and fall incidence after total knee arthroplasty. J. Knee Surg. 2021, 34, 1205–1211. [Google Scholar] [CrossRef]
- Nagymáté, G.; Orlovits, Z.; Kiss, R.M. Reliability analysis of a sensitive and independent stabilometry parameter set. PLoS ONE 2018, 13, e0195995. [Google Scholar] [CrossRef] [PubMed]
- Khalaj, N.; Abu Osman, N.A.; Mokhtar, A.H.; Mehdikhani, M.; Wan Abas, W.A. Balance and risk of fall in individuals with bilateral mild and moderate knee osteoarthritis. PLoS ONE 2014, 9, e92270. [Google Scholar] [CrossRef]
- Dunsky, A. The effect of balance and coordination exercises on quality of life in older adults: A mini-review. Front. Aging Neurosci. 2019, 11, 318. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, I.; Kandel, L.; Sajina, A.; Litinezki, D.; Herman, A.; Mattan, Y. Balance is an important predictive factor for quality of life and function after primary total knee replacement. J. Bone Jt. Surg. Br. 2012, 94, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Vahtrik, D.; Ereline, J.; Gapeyeva, H.; Pääsuke, M. Postural stability in relation to anthropometric and functional characteristics in women with knee osteoarthritis following total knee arthroplasty. Arch. Orthop. Trauma Surg. 2014, 134, 685–692. [Google Scholar] [CrossRef]
- Hernefalk, B.; Brüggemann, A.; Mohammed, J.; Mukka, S.; Wolf, O. Lower mortality in distal femoral fractures in the presence of a knee arthroplasty: An observational study on 2,725 fractures from the Swedish Fracture Register. Acta Orthop. 2022, 93, 684–688. [Google Scholar] [CrossRef]
- Swanik, C.B.; Lephart, S.M.; Rubash, H.E. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J. Bone Jt. Surg. Am. 2004, 86, 328–334. [Google Scholar] [CrossRef]
- Gage, W.H.; Frank, J.S.; Prentice, S.D.; Stevenson, P. Postural responses following a rotational support surface perturbation, following knee joint replacement: Frontal plane rotations. Gait Posture 2008, 27, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Moutzouri, M.; Gleeson, N.; Billis, E.; Tsepis, E.; Panoutsopoulou, I.; Gliatis, J. The effect of total knee arthroplasty on patients balance and incidence of falls a systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3439–3451. [Google Scholar] [CrossRef] [PubMed]
- Akbaba, Y.A.; Yeldan, I.; Guney, N.; Ozdincler, A.R. Intensive supervision of rehabilitation programme improves balance and functionality in the short term after bilateral total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Woodhull-McNeal, A.P. Changes in posture and balance with age. Aging 1992, 4, 219–225. [Google Scholar] [CrossRef]
- Gong, H.; Sun, L.; Yang, R.; Pang, J.; Chen, B.; Qi, R.; Gu, X.; Zhang, Y.; Zhang, T.-M. Changes of upright body posture in the sagittal plane of men and women occurring with aging—A cross sectional study. BMC Geriatr. 2019, 19, 71. [Google Scholar] [CrossRef]
- Davut, S.; Huzmeli, I.; Hallaceli, H.; Kalacı, A. Does Total Knee Arthroplasty Positively Affect Body Static-Dynamic Balance and Fall Risk Parameters in Patients With Satisfactory Functional Scores? Cureus 2022, 14, e30207. [Google Scholar] [CrossRef] [PubMed]
- Gauchard, G.C.; Vancon, G.; Meyer, P.; Mainard, D.; Perrin, P.P. On the role of knee joint in balance control and postural strategies: Effects of total knee replacement in elderly subjects with knee osteoarthritis. Gait Posture 2010, 32, 155–160. [Google Scholar] [CrossRef]
- Bjerke, J. Gait and Postural Control after Total Knee Arthroplasty. Doctoral Dissertation, Department of Community Medicine and Rehabilitation, Physiotherapy Umeå University, Umeå, Sweden, 2014. [Google Scholar]
- Goetz, J.; Baeurle, M.; Dullien, S.; Grifka, J.; Koeck, F.; Baier, C. Postural Stability after Unicondylar Knee Arthroplasty and Patient-Specific Interpositional Knee Spacer. BioMed Res. Int. 2017, 2017, 5836025. [Google Scholar] [CrossRef]
- Karasavvidis, T.; Pagan Moldenhauer, C.A.; Haddad, F.S.; Hirschmann, M.T.; Pagnano, M.W.; Vigdorchik, J.M. Current Concepts in Alignment in Total Knee Arthroplasty. J. Arthroplast. 2023, 38 (Suppl. S2), S29–S37. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Howell, S.M.; Won, Y.Y.; Lee, O.S.; Lee, S.H.; Vahedi, H.; Teo, S.H. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3467–3479. [Google Scholar] [CrossRef] [PubMed]
- Neculăeș, M.; Hernandez-Lucas, P.; Lucaci, P. Implications of Stabilometric Assessment in Determining Functional Deficits in Patients with Severe Knee Osteoarthritis: Observational Study. J. Clin. Med. 2024, 13, 3181. [Google Scholar] [CrossRef] [PubMed]
| Variable | TKA X ± SD; (Min/Max) | UKA X ± SD; (Min/Max) | Healthy X ± SD; (Min/Max) |
|---|---|---|---|
| Age [years] | 63.47 ± 2.17 (59/69) | 64.65 ± 1.93 60/70 | 64.45 ± 3.12 (60/69) |
| Height [cm] | 164.81 ± 5.71 (158/179) | 164.63 ± 4.61 (159/177) | 165.45 ± 4.37 (159/181) |
| Body weight [kg] | 77.11 ± 11.62 (59/108) | 76.34 ± 8.32 (58/99) | 74.20 ± 9.76 (61/101) |
| Eyes Open | Group Comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Indicators | TKA | UKA | Healthy | t | p | ||||
| X ± SD | X ± SD | X ± SD | TKA–UKA | TKA–Healthy | UKA–Healthy | TKA–UKA | TKA–Healthy | UKA–Healthy | |
| COM X (cm) | 0.84 ± 0.33 | 0.55 ± 0.05 | 0.44 ± 0.02 | 3.87 | 5.32 | 8.80 | <0.001 | <0.001 | <0.001 |
| COM Y (cm) | 0.97 ± 0.40 | 0.46 ± 0.05 | 0.38 ± 0.05 | 5.68 | 6.56 | 5.17 | <0.001 | <0.001 | <0.001 |
| V X (cm/s) | 0.79 ± 0.14 | 0.65 ± 0.04 | 0.57 ± 0.04 | 4.50 | 6.98 | 6.79 | <0.001 | <0.001 | <0.001 |
| V Y (cm/s) | 0.85 ± 0.11 | 0.72 ± 0.02 | 0.64 ± 0.03 | 5.10 | 7.89 | 9.07 | <0.001 | <0.001 | <0.001 |
| PL (cm) | 35.37 ± 3.10 | 30.81 ± 0.82 | 23.06 ± 1.33 | 6.34 | 16.29 | 22.25 | <0.001 | <0.001 | <0.001 |
| SA (cm2) | 2.51 ± 0.35 | 2.32 ± 0.31 | 1.24 ± 0.14 | 1.88 | 14.93 | 14.16 | 0.15 | <0.001 | <0.001 |
| Eyes Closed | Group Comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Indicators | TKA | UKA | Healthy | t | p | ||||
| X ± SD | X ± SD | X ± SD | TKA–UKA | TKA–Healthy | UKA–Healthy | TKA–UKA | TKA–Healthy | UKA–Healthy | |
| COM X (cm) | 1.03 ± 0.34 | 0.73 ± 0.04 | 0.51 ± 0.02 | 3.83 | 6.66 | 21.86 | <0.001 | <0.001 | <0.001 |
| COM Y (cm) | 1.14 ± 0.38 | 0.74 ± 0.04 | 0.46 ± 0.02 | 4.66 | 8.09 | 29.63 | <0.001 | <0.001 | <0.001 |
| V X (cm/s) | 1.32 ± 0.21 | 0.92 ± 0.05 | 0.66 ± 0.03 | 8.45 | 14.26 | 19.28 | <0.001 | <0.001 | <0.001 |
| V Y (cm/s) | 1.42 ± 0.18 | 0.88 ± 0.05 | 0.71 ± 0.03 | 12.92 | 17.30 | 13.66 | <0.001 | <0.001 | <0.001 |
| PL (cm) | 52.72 ± 2.43 | 33.57 ± 1.54 | 28.72 ± 0.85 | 29.73 | 41.66 | 12.29 | <0.001 | <0.001 | <0.001 |
| SA (cm2) | 10.55 ± 0.69 | 6.49 ± 0.63 | 2.87 ± 0.45 | 19.51 | 41.57 | 20.92 | <0.001 | <0.001 | <0.001 |
| Dynamic Test | Group Comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Indicators | TKA | UKA | Healthy | t | p | ||||
| X ± SD | X ± SD | X ± SD | TKA–UKA | TKA–Healthy | UKA–Healthy | TKA–UKA | TKA–Healthy | UKA–Healthy | |
| Time R-F (s) | 2.49 ± 0.43 | 1.79 ± 0.10 | 1.34 ± 0.07 | 7.17 | 11.94 | 16.78 | <0.001 | <0.001 | <0.001 |
| Time L-F (s) | 2.75 ± 0.37 | 2.03 ± 0.19 | 1.24 ± 0.06 | 7.79 | 17.98 | 17.87 | <0.001 | <0.001 | <0.001 |
| Time L-R (s) | 2.63 ± 0.42 | 1.54 ± 0.05 | 1.29 ± 0.07 | 11.57 | 14.08 | 13.39 | <0.001 | <0.001 | <0.001 |
| Time R-R (s) | 2.58 ± 0.39 | 1.72 ± 0.05 | 1.29 ± 0.06 | 9.73 | 14.54 | 22.77 | <0.001 | <0.001 | <0.001 |
| PL (cm) | 182.59 ± 2.02 | 157.22 ± 2.76 | 135.96 ± 1.21 | 32.11 | 82.97 | 31.54 | <0.001 | <0.001 | <0.001 |
| WOMAC | ||||||||
|---|---|---|---|---|---|---|---|---|
| Group | Measurement | X ± SD | Me | Min–Max | p | Group Comparison | p before | p after |
| TKA | before | 85.45 ± 4.19 | 84.50 | 79.00–92.00 | 0.001 | TKA vs. UKA | 0.03 | 0.75 |
| after | 59.15 ± 10.77 | 59.00 | 42.00–80.00 | |||||
| UKA | before | 81.20 ± 7.57 | 82.50 | 65.00–92.00 | 0.001 | |||
| after | 58.05 ± 11.14 | 58.00 | 34.00–73.00 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sorysz, T.; Adamik, A.; Ogrodzka-Ciechanowicz, K. Does the Type of Knee Arthroplasty Affect the Patient’s Postural Stability? Medicina 2024, 60, 1582. https://doi.org/10.3390/medicina60101582
Sorysz T, Adamik A, Ogrodzka-Ciechanowicz K. Does the Type of Knee Arthroplasty Affect the Patient’s Postural Stability? Medicina. 2024; 60(10):1582. https://doi.org/10.3390/medicina60101582
Chicago/Turabian StyleSorysz, Tomasz, Aleksandra Adamik, and Katarzyna Ogrodzka-Ciechanowicz. 2024. "Does the Type of Knee Arthroplasty Affect the Patient’s Postural Stability?" Medicina 60, no. 10: 1582. https://doi.org/10.3390/medicina60101582
APA StyleSorysz, T., Adamik, A., & Ogrodzka-Ciechanowicz, K. (2024). Does the Type of Knee Arthroplasty Affect the Patient’s Postural Stability? Medicina, 60(10), 1582. https://doi.org/10.3390/medicina60101582






