Impact of the COVID-19 Pandemic on Lifestyle Behavior and Clinical Care Pathway Management in Type 2 Diabetes: A Retrospective Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Objectives
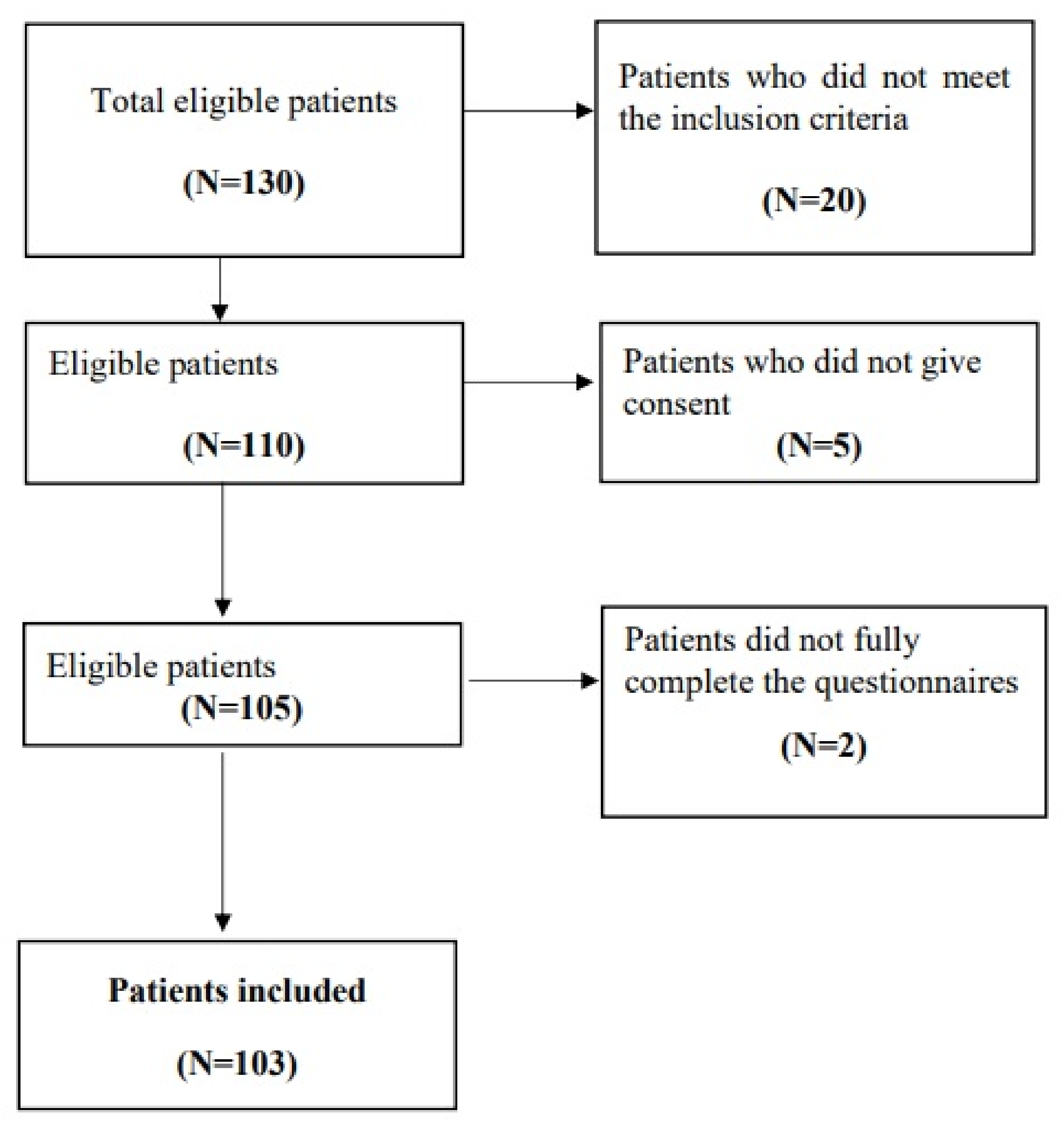
2.2. Study Design
2.3. Ethical Considerations
2.4. Study Population
2.5. Data Collection
2.6. Instrument
2.7. Statistical Analysis
3. Results
3.1. Characteristics of the Sample
3.2. PACIC Questionnaire
3.3. Medi-Lite Questionnaire
3.4. Impact of COVID-19 on the Dietary and Physical Activity Behaviors in Patients with T2D
3.4.1. Changes in Dietary Habits
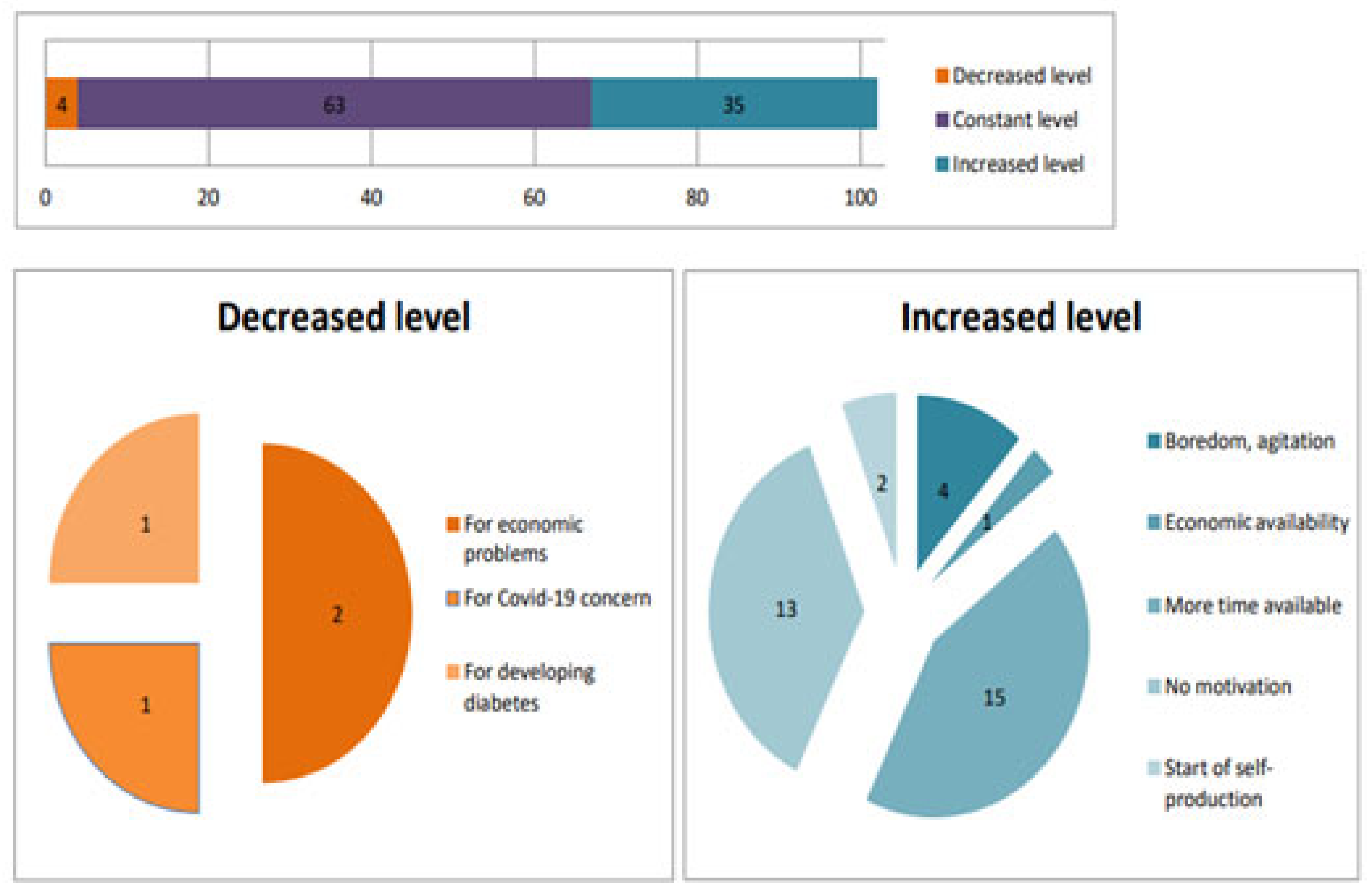
3.4.2. Changes in Physical Activity Levels
3.5. Data Correlations
3.5.1. PACIC Questionnaire
Gender
Education Level
3.5.2. Medi Lite Questionnaire
Gender
Education Level
Household Size
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (WHO). Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 1 July 2024).
- Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 1 July 2024).
- Cojocaru, D.-C.; Mitu, F.; Leon, M.-M.; Dima-Cozma, L.C.; Adam, C.A.; Cumpăt, C.M.; Negru, R.D.; Maștaleru, A.; Onofrei, V. Beyond the Acute Phase: Long-Term Impact of COVID-19 on Functional Capacity and Prothrombotic Risk—A Pilot Study. Medicina 2023, 60, 51. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.H.; Kim, G.H.J.; Park, S.-B.; Lee, S.-I.; Koh, J.S.; Brown, M.S.; Abtin, F.; McNitt-Gray, M.F.; Goldin, J.G.; Lee, J.S. Quantitative Computed Tomography Lung COVID Scores with Laboratory Markers: Utilization to Predict Rapid Progression and Monitor Longitudinal Changes in Patients with Coronavirus 2019 (COVID-19) Pneumonia. Biomedicines 2024, 12, 120. [Google Scholar] [CrossRef] [PubMed]
- Baratella, E.; Bussani, R.; Zanconati, F.; Marrocchio, C.; Fabiola, G.; Braga, L.; Maiocchi, S.; Berlot, G.; Volpe, M.C.; Moro, E.; et al. Radiological-pathological signatures of patients with COVID-19-related pneumomediastinum: Is there a role for the Sonic hedgehog and Wnt5a pathways? ERJ Open Res. 2021, 7, 00346–2021. [Google Scholar] [CrossRef] [PubMed]
- Istituto Superiore di Sanità, (ISS). Epicentro, l’Epidemiologia per la Sanità Pubblica. Available online: https://www.epicentro.iss.it/coronavirus/ (accessed on 5 July 2024).
- Presidenza del Consiglio dei Ministri. Decreto del Presidente del Consiglio del 1 Marzo 2020. Misure Urgenti in Materia di Contenimento e Gestione Dell’emergenza Epidemiologica da COVID-19. Available online: https://www.gazzettaufficiale.it/eli/id/2020/03/01/20A01381/sg (accessed on 1 July 2024).
- Lai, H.; Yang, M.; Sun, M.; Pan, B.; Wang, Q.; Wang, J.; Tian, J.; Ding, G.; Yang, K.; Song, X.; et al. Risk of incident diabetes after COVID-19 infection: A systematic review and meta-analysis. Metabolism 2022, 137, 155330. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Liu, X.; Bao, K.; Huang, C. Ischemic stroke associated with COVID-19: A systematic review and meta-analysis. J. Neurol. 2022, 269, 1731–1740. [Google Scholar] [CrossRef]
- Garg, A.; Posa, M.K.; Kumar, A. Diabetes and deaths of COVID-19 patients: Systematic review of meta-analyses. Health Sci. Rev. 2023, 7, 100099. [Google Scholar] [CrossRef]
- Palaiodimos, L.; Kokkinidis, D.G.; Li, W.; Karamanis, D.; Ognibene, J.; Arora, S.; Southern, W.N.; Mantzoros, C.S. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020, 108, 154262. [Google Scholar] [CrossRef]
- Kruglikov, I.L.; Scherer, P.E. The Role of Adipocytes and Adipocyte-Like Cells in the Severity of COVID-19 Infections. Obesity 2020, 28, 1187–1190. [Google Scholar] [CrossRef]
- Zhou, Y.; Chi, J.; Lv, W.; Wang, Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (COVID-19). Diabetes/Metabolism Res. Rev. 2021, 37, e3377. [Google Scholar] [CrossRef]
- Zhou, H.; Wang, J.; Asghar, N.; Liang, B.; Song, Q.; Zhou, X. Impact of Comorbidity on the Duration from Symptom Onset to Death in Patients with Coronavirus Disease 2019: A Retrospective Study of 104,753 Cases in Pakistan. Diseases 2023, 11, 176. [Google Scholar] [CrossRef]
- Khamis, F.; Al Awaidy, S.; Al Shaaibi, M.; Al Shukeili, M.; Chhetri, S.; Al Balushi, A.; Al Sulaimi, S.; Al Balushi, A.; Wesonga, R. Epidemiological Characteristics of Hospitalized Patients with Moderate versus Severe COVID-19 Infection: A Retrospective Cohort Single Centre Study. Diseases 2021, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas Tenth Edition 2021. Available online: https://diabetesatlas.org/atlas/tenth-edition/ (accessed on 1 July 2024).
- National Institutes of Health; U.S. Department of Health and Human Services; National Institute of Diabetes and Digestive and Kidney Diseases. Available online: https://www.niddk.nih.gov/health-information/diabetes/overview/diet-eating-physical-activity#:~:text=Nutrition%20and%20physical%20activity%20are,sugar%2C%20in%20your%20target%20range (accessed on 5 July 2024).
- Petrelli, F.; Cangelosi, G.; Scuri, S.; Thu, N.C.T.; Debernardi, G.; Benni, A.; Vesprini, A.; Rocchi, R.; De Carolis, C.; Pantanetti, P.; et al. Conoscenze alimentari in pazienti afferenti ad un centro di diabetologia [Food knowledge of patients at the first access to a Diabetology center]. Acta Biomed. 2020, 91, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Cangelosi, G.; Grappasonni, I.; Nguyen, C.T.T.; Acito, M.; Pantanetti, P.; Benni, A.; Petrelli, F. Mediterranean Diet (MedDiet) and Lifestyle Medicine (LM) for support and care of patients with type II diabetes in the COVID-19 era: A cross-observational study. Acta Bio-Medica Atenei Parm. 2023, 94, e2023189. [Google Scholar] [CrossRef]
- Mulita, F.; Vailas, M.; Tchabashvili, L.; Liolis, E.; Iliopoulos, F.; Drakos, N.; Maroulis, I. The impact of the COVID-19 outbreak on emergency surgery: A Greek emergency department experience. Gastroenterol. Rev. 2021, 16, 95. [Google Scholar] [CrossRef] [PubMed]
- Khunti, K.; Valabhji, J.; Misra, S. Diabetes and the COVID-19 pandemic. Diabetologia 2023, 66, 255–266. [Google Scholar] [CrossRef]
- Gebremeskel, G.G.; Tadesse, D.B.; Haile, T.G. Mortality and morbidity in critically ill COVID-19 patients: A systematic review and meta-Analysis. J. Infect. Public Health 2024, 17, 102533. [Google Scholar] [CrossRef]
- Jahromi, A.S.; Jokar, M.; Sharifi, N.; Zahernasab, A.E.; Kariminezhad, N.; Rahmanian, V. Systematic review and meta-analysis of knowledge, attitudes, and practices regarding COVID-19 among chronic disease patients: A global perspective. Health Sci. Rep. 2024, 7, e1793. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes—2024. Diabetes Care 2024, 47 (Suppl. S1), S11–S19. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes–2024. Diabetes Care 2024, 47 (Suppl. S1), S145–S157. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 5. Facilitating positive health behaviors and well-being to improve health outcomes: Standards of care in diabetes—2024. Diabetes Care 2024, 47 (Suppl. S1), S77–S110. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 6. Glycemic Targets: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46 (Suppl. S1), S97–S110. [Google Scholar] [CrossRef] [PubMed]
- Istituto Superiore di Sanità, ISS. Giornata Mondiale Diabete: Dalla Prevalenza ALL’ACCESSO Alle Cure, i Numeri della Sorveglianza Passi. Available online: https://www.iss.it/-/giornata-mondiale-diabete-da-prevalenza-ad-accesso-cure-i-numeri-del-sistema-passi (accessed on 5 July 2024).
- Ojo, O.; Wang, X.-H.; Ojo, O.O.; Orjih, E.; Pavithran, N.; Adegboye, A.R.A.; Feng, Q.-Q.; McCrone, P. The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1095. [Google Scholar] [CrossRef] [PubMed]
- Wafa, I.A.; Pratama, N.R.; Sofia, N.F.; Anastasia, E.S.; Konstantin, T.; Wijaya, M.A.; Wiyono, M.R.; Djuari, L.; Novida, H. Impact of COVID-19 Lockdown on the Metabolic Control Parameters in Patients with Diabetes Mellitus: A Systematic Review and Meta-Analysis. Diabetes Metab. J. 2022, 46, 260–272. [Google Scholar] [CrossRef] [PubMed]
- Cioca, F.; Timar, R.; Ignuta, F.; Vlad, A.; Bratosin, F.; Rosca, O.; Jianu, A.M.; Rosca, D.; Septimiu-Radu, S.; Burtic, S.-R.; et al. Comparative Analysis of COVID-19 Outcomes in Type 1 and Type 2 Diabetes: A Three-Year Retrospective Study. Medicina 2024, 60, 210. [Google Scholar] [CrossRef] [PubMed]
- Tallon, E.M.; Ebekozien, O.; Sanchez, J.; Staggs, V.S.; Ferro, D.; McDonough, R.; Demeterco-Berggren, C.; Polsky, S.; Gomez, P.; Patel, N.; et al. Impact of diabetes status and related factors on COVID-19-associated hospitalization: A nationwide retrospective cohort study of 116,370 adults with SARS-CoV-2 infection. Diabetes Res. Clin. Pract. 2022, 194, 110156. [Google Scholar] [CrossRef]
- Gęca, T.; Wojtowicz, K.; Guzik, P.; Góra, T. Increased Risk of COVID-19 in Patients with Diabetes Mellitus—Current Challenges in Pathophysiology, Treatment and Prevention. Int. J. Environ. Res. Public Health 2022, 19, 6555. [Google Scholar] [CrossRef]
- Khunti, K.; Aroda, V.R.; Aschner, P.; Chan, J.C.N.; Del Prato, S.; Hambling, C.E.; Harris, S.; Lamptey, R.; McKee, M.; Tandon, N.; et al. The impact of the COVID-19 pandemic on diabetes services: Planning for a global recovery. Lancet Diabetes Endocrinol. 2022, 10, 890–900. [Google Scholar] [CrossRef]
- Matenge, S.; Sturgiss, E.; Desborough, J.; Dykgraaf, S.H.; Dut, G.; Kidd, M. Ensuring the continuation of routine primary care during the COVID-19 pandemic: A review of the international literature. Fam. Pract. 2022, 39, 747–761. [Google Scholar] [CrossRef]
- Petrelli, F.; Cangelosi, G.; Scuri, S.; Pantanetti, P.; Lavorgna, F.; Faldetta, F.; De Carolis, C.; Rocchi, R.; Debernardi, G.; Florescu, A.; et al. Diabetes and technology: A pilot study on the management of patients with insulin pumps during the COVID-19 pandemic. Diabetes Res. Clin. Pract. 2020, 169, 108481. [Google Scholar] [CrossRef]
- Amsah, N.; Isa, Z.M.; Ahmad, N.; Manaf, M.R.A. Impact of COVID-19 Pandemic on Healthcare Utilization among Patients with Type 2 Diabetes Mellitus: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 4577. [Google Scholar] [CrossRef]
- Hu, Z.; Youn, H.M.; Quan, J.; Lee, L.L.S.; Mak, I.L.; Yu, E.Y.T.; Chao, D.V.-K.; Ko, W.W.K.; Wong, I.C.K.; Lau, G.K.K.; et al. The indirect impact of the COVID-19 pandemic on people with type 2 diabetes mellitus and without COVID-19 infection: Systematic review and meta-analysis. Prim. Care Diabetes 2023, 17, 229–237. [Google Scholar] [CrossRef] [PubMed]
- McGurnaghan, S.J.; Weir, A.; Bishop, J.; Kennedy, S.; Blackbourn, L.A.K.; McAllister, D.A.; Hutchinson, S.; Caparrotta, T.M.; Mellor, J.; Jeyam, A.; et al. Risks of and risk factors for COVID-19 disease in people with diabetes: A cohort study of the total population of Scotland. Lancet Diabetes Endocrinol. 2021, 9, 82–93. [Google Scholar] [CrossRef] [PubMed]
- Paltrinieri, S.; Bressi, B.; Costi, S.; Mazzini, E.; Cavuto, S.; Ottone, M.; De Panfilis, L.; Fugazzaro, S.; Rondini, E.; Rossi, P.G. Beyond Lockdown: The Potential Side Effects of the SARS-CoV-2 Pandemic on Public Health. Nutrients 2021, 13, 1600. [Google Scholar] [CrossRef] [PubMed]
- Khamees, A.; Awadi, S.; Rawashdeh, S.; Talafha, M.; Alzoubi, M.; Almdallal, W.; Al-Eitan, S.; Saeed, A.; Al-Zoubi, R.M.; Al-Zoubi, M.S. The impact of COVID-19 pandemic lockdown on smoking habits and lifestyle: A cross-sectional study. Health Sci. Rep. 2023, 6, e1392. [Google Scholar] [CrossRef]
- Samanta, S.; Banerjee, J.; Rahaman, S.N.; Ali, K.M.; Ahmed, R.; Giri, B.; Pal, A.; Dash, S.K. Alteration of dietary habits and lifestyle pattern during COVID-19 pandemic associated lockdown: An online survey study. Clin. Nutr. ESPEN 2022, 48, 234–246. [Google Scholar] [CrossRef]
- McGinlay, M.; Straw, S.; Jagger, J.; Nouri, B.; Gierula, J.; Witte, K.K. Impact of the COVID-19 pandemic on the management of chronic heart failure. Rev. Cardiovasc. Med. 2021, 22, 271–276. [Google Scholar] [CrossRef]
- De Kreutzenberg, S.V. Telemedicine for the Clinical Management of Diabetes: Implications and Considerations After COVID-19 Experience. High Blood Press. Cardiovasc. Prev. 2022, 29, 319–326. [Google Scholar] [CrossRef]
- Scuri, S.; Tesauro, M.; Petrelli, F.; Argento, N.; Damasco, G.; Cangelosi, G.; Nguyen, C.T.T.; Savva, D.; Grappasonni, I. Use of an Online Platform to Evaluate the Impact of Social Distancing Measures on Psycho-Physical Well-Being in the COVID-19 Era. Int. J. Environ. Res. Public Health 2022, 19, 6805. [Google Scholar] [CrossRef]
- Rodríguez-Fernández, P.; González-Santos, J.; Santamaría-Peláez, M.; Soto-Cámara, R.; Sánchez-González, E.; González-Bernal, J.J. Psychological Effects of Home Confinement and Social Distancing Derived from COVID-19 in the General Population—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6528. [Google Scholar] [CrossRef]
- Segura-García, S.; Barrera-Ramírez, A.; Gutiérrez-Esparza, G.O.; Groves-Miralrio, E.; Martínez-García, M.; Hernández-Lemus, E. Effects of social confinement during the first wave of COVID-19 in Mexico City. Front. Public Health 2023, 11, 1202202. [Google Scholar] [CrossRef]
- Johansson-Pajala, R.-M.; Alam, M.; Gusdal, A.; Wågert, P.v.H.; Löwenmark, A.; Boström, A.-M.; Hammar, L.M. Anxiety and loneliness among older people living in residential care facilities or receiving home care services in Sweden during the COVID-19 pandemic: A national cross-sectional study. BMC Geriatr. 2022, 22, 927. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.G.; Fogacci, F.; Giovannini, M.; Mezzadri, M.; Grandi, E.; Borghi, C.; The Brisighella Heart Study Group. COVID-19-Related Quarantine Effect on Dietary Habits in a Northern Italian Rural Population: Data from the Brisighella Heart Study. Nutrients 2021, 13, 309. [Google Scholar] [CrossRef] [PubMed]
- Mascherini, G.; Catelan, D.; Pellegrini-Giampietro, D.E.; Petri, C.; Scaletti, C.; Gulisano, M. Changes in physical activity levels, eating habits and psychological well-being during the Italian COVID-19 pandemic lockdown: Impact of socio- demographic factors on the Florentine academic population. PLoS ONE 2021, 16, e0252395. [Google Scholar] [CrossRef]
- Hussein, Y.H.H.; Soliman, A.-Z.M. Dietary habits, lifestyle changes, and glycemic control in patients with type 2 diabetes mellitus during coronavirus disease 2019 (COVID-19): A cross-sectional study in Egypt. J. Fam. Community Med. 2023, 30, 1–11. [Google Scholar] [CrossRef]
- Felix, H.C.; Andersen, J.A.; Willis, D.E.; Malhis, J.R.; Selig, J.P.; McElfish, P.A. Control of type 2 diabetes mellitus during the COVID-19 pandemic. Prim. Care Diabetes 2021, 15, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Sankar, P.; Ahmed, W.N.; Koshy, V.M.; Jacob, R.; Sasidharan, S. Effects of COVID-19 lockdown on type 2 diabetes, lifestyle and psychosocial health: A hospital-based cross-sectional survey from South India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1815–1819. [Google Scholar] [CrossRef] [PubMed]
- Leite, N.J.C.; Raimundo, A.M.M.; Mendes, R.D.C.; Marmeleira, J.F.F. Impact of COVID-19 Pandemic on Daily Life, Physical Exercise, and General Health among Older People with Type 2 Diabetes: A Qualitative Interview Study. Int. J. Environ. Res. Public Health 2022, 19, 3986. [Google Scholar] [CrossRef]
- Leong, C.M.; Lee, T.-I.; Chien, Y.-M.; Kuo, L.-N.; Kuo, Y.-F.; Chen, H.-Y. Social Media-Delivered Patient Education to Enhance Self-management and Attitudes of Patients with Type 2 Diabetes During the COVID-19 Pandemic: Randomized Controlled Trial. J. Med. Internet Res. 2022, 24, e31449. [Google Scholar] [CrossRef]
- Hansel, B.; Potier, L.; Chalopin, S.; Larger, E.; Gautier, J.-F.; Delestre, F.; Masdoua, V.; Visseaux, B.; Lucet, J.-C.; Kerneis, S.; et al. The COVID-19 lockdown as an opportunity to change lifestyle and body weight in people with overweight/obesity and diabetes: Results from the national French COVIDIAB cohort. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2605–2611. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Strobe Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Br. Med. J. 2007, 335, 806–808. [Google Scholar] [CrossRef]
- Brambilla, A.; Stara, R.L.; Cacciapuoti, I.; The MacColl Center for Health Care Innovation, Group Health Cooperative. Italian Version of Regional Healthcare Service Authority, Emilia-Romagna Region, Italy, and in Collaboration with Federation Diabetes Emilia-Romagna (Fe.D.E.R.). Available online: https://www.act-center.org (accessed on 16 April 2024).
- Coleman, K.; Austin, B.T.; Brach, C.; Wagner, E.H. Evidence on the Chronic Care Model in the new millennium. Health Aff. 2009, 28, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Cangelosi, G.; Nittari, G.; Pantanetti, P.; Debernardi, G.; Scuri, S.; Sagaro, G.G.; Nguyen, C.T.T.; Grappasonni, I. Chronic Care Model in Italy: A narrative review of the literature. Prim. Health Care Res. Dev. 2022, 22, 1–7. [Google Scholar] [CrossRef]
- Sofi, F.; Dinu, M.; Pagliai, G.; Marcucci, R.; Casini, A. Validation of a literature-based adherence score to Mediterranean diet: The MEDI-LITE score. Int. J. Food Sci. Nutr. 2017, 68, 757–762. [Google Scholar] [CrossRef] [PubMed]
- Medi-Lite. Literature-Based Adherence Score to Mediterranean Diet. Available online: https://medi-lite.com/ (accessed on 21 July 2024).
- Valabhji, J.; Barron, E.; Gorton, T.; Bakhai, C.; Kar, P.; Young, B.; Khunti, K.; Holman, N.; Sattar, N.; Wareham, N.J. Associations between reductions in routine care delivery and non-COVID-19-related mortality in people with diabetes in England during the COVID-19 pandemic: A population-based parallel cohort study. Lancet Diabetes Endocrinol. 2022, 10, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Daimer, S.; Mihatsch, L.L.; Neufeld, S.A.; Murray, G.K.; Knolle, F. Investigating the relationship of COVID-19 related stress and media consumption with schizotypy, depression, and anxiety in cross-sectional surveys repeated throughout the pandemic in Germany and the UK. eLife 2022, 11, e75893. [Google Scholar] [CrossRef]
- Eren, M.A.; Gönel, A.; Karaaslan, H.; Uyar, N.; Cindoğlu, Ç.; Sabuncu, T. Effects of COVID-19 pandemic lockdown on the metabolic control of type 2 diabetes mellitus in patients. Arq. Bras. Endocrinol. Metabol. 2023, 67, e000621. [Google Scholar] [CrossRef]
- Grabowski, D.; Overgaard, M.; Meldgaard, J.; Johansen, L.B.; Willaing, I. Disrupted Self-Management and Adaption to New Diabetes Routines: A Qualitative Study of How People with Diabetes Managed Their Illness during the COVID-19 Lockdown. Diabetology 2021, 2, 1–15. [Google Scholar] [CrossRef]
- Eberle, C.; Stichling, S. Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: A systematic review. Diabetol. Metab. Syndr. 2021, 13, 95. [Google Scholar] [CrossRef]
- Derrick, S.A.; Nguyen, S.T.; Marthens, J.R.; Dambacher, L.L.; Sikalidis, A.K.; Reaves, S.K. A Mediterranean-Style Diet Improves the Parameters for the Management and Prevention of Type 2 Diabetes Mellitus. Medicina 2023, 59, 1882. [Google Scholar] [CrossRef]
- Kim, S.H.; Arora, I.; Hsia, D.S.; Knowler, W.C.; LeBlanc, E.; Mylonakis, E.; Pratley, R.; Pittas, A.G. New-Onset Diabetes After COVID-19. J. Clin. Endocrinol. Metab. 2023, 108, e1164–e1174. [Google Scholar] [CrossRef]
- Grant, F.; Scalvedi, M.L.; Scognamiglio, U.; Turrini, A.; Rossi, L. Eating Habits during the COVID-19 Lockdown in Italy: The Nutritional and Lifestyle Side Effects of the Pandemic. Nutrients 2021, 13, 2279. [Google Scholar] [CrossRef] [PubMed]
- Izzo, L.; Santonastaso, A.; Cotticelli, G.; Federico, A.; Pacifico, S.; Castaldo, L.; Colao, A.; Ritieni, A. An Italian Survey on Dietary Habits and Changes during the COVID-19 Lockdown. Nutrients 2021, 13, 1197. [Google Scholar] [CrossRef] [PubMed]
- Smith-Miller, C.A.; Berry, D.C.; Miller, C.T. Gender Differences and Their Influences on T2DM Self-Management Among Spanish-Speaking Latinx Immigrants. Hisp. Health Care Int. 2022, 20, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Zhu, H.; Liu, J.; Zhou, J.; Tang, W. Barriers to Self-Management of Type 2 Diabetes During COVID-19 Medical Isolation: A Qualitative Study. Diabetes Metab. Syndr. Obes. 2020, 13, 3713–3725. [Google Scholar] [CrossRef]
- Paulsamy, P.; Ashraf, R.; Alshahrani, S.H.; Periannan, K.; Qureshi, A.A.; Venkatesan, K.; Manoharan, V.; Govindasamy, N.; Prabahar, K.; Arumugam, T.; et al. Social Support, Self-Care Behaviour and Self-Efficacy in Patients with Type 2 Diabetes during the COVID-19 Pandemic: A Cross-Sectional Study. Healthcare 2021, 9, 1607. [Google Scholar] [CrossRef]
- Idris, I.B.; Hamis, A.A.; Bukhori, A.B.M.; Hoong, D.C.C.; Yusop, H.; Shaharuddin, M.A.-A.; Fauzi, N.A.F.A.; Kandayah, T. Women’s autonomy in healthcare decision making: A systematic review. BMC Women’s Health 2023, 23, 643. [Google Scholar] [CrossRef]
- Wham, C.A.; Teh, R.; Moyes, S.; Dyall, L.; Kepa, M.; Hayman, K.; Kerse, N. Health and social factors associated with nutrition risk: Results from life and living in advanced age: A cohort study in New Zealand (LiLACS NZ). J. Nutr. Health Aging 2015, 19, 637–645. [Google Scholar] [CrossRef]
- Kucukerdonmez, O.; Varli, S.N.; Koksal, E. Comparison of nutritional status in the elderly according to living situations. J. Nutr. Health Aging 2017, 21, 25–30. [Google Scholar] [CrossRef]
- Hanna, K.L.; Collins, P.F. Relationship between living alone and food and nutrient intake. Nutr. Rev. 2015, 73, 594–611. [Google Scholar] [CrossRef]
- Wu, X.; Liu, X.; Liao, W.; Kang, N.; Dong, X.; Abdulai, T.; Zhai, Z.; Wang, C.; Wang, X.; Li, Y. Prevalence and characteristics of alcohol consumption and risk of type 2 diabetes mellitus in rural China. BMC Public Health 2021, 21, 1644. [Google Scholar] [CrossRef]
- Llamosas-Falcón, L.; Rehm, J.; Bright, S.; Buckley, C.; Carr, T.; Kilian, C.; Lasserre, A.M.; Lemp, J.M.; Zhu, Y.; Probst, C. The Relationship Between Alcohol Consumption, BMI, and Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis. Diabetes Care 2023, 46, 2076–2083. [Google Scholar] [CrossRef] [PubMed]
- Knott, C.; Bell, S.; Britton, A. Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 2015, 38, 1804–1812. [Google Scholar] [CrossRef] [PubMed]
- Uusitupa, M.; Khan, T.A.; Viguiliouk, E.; Kahleova, H.; Rivellese, A.A.; Hermansen, K.; Pfeiffer, A.; Thanopoulou, A.; Salas-Salvadó, J.; Schwab, U.; et al. Prevention of Type 2 Diabetes by Lifestyle Changes: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2611. [Google Scholar] [CrossRef] [PubMed]
- Hemmingsen, B.; Gimenez-Perez, G.; Mauricio, D.; Figuls, M.R.I.; Metzendorf, M.-I.; Richter, B. Diet, physical activity or both for prevention or delay of type 2 diabetes mellitus and its associated complications in people at increased risk of developing type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2017, 12, CD003054. [Google Scholar] [CrossRef] [PubMed]
- Alshareef, R.; Al Zahrani, A.; Alzahrani, A.; Ghandoura, L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diabetes Metab. Syndr. 2020, 14, 1583–1587. [Google Scholar] [CrossRef]
- Luzi, L.; Carruba, M.; Crialesi, R.; Da Empoli, S.; Dagani, R.; Lovati, E.; Nicolucci, A.; Berra, C.C.; Cipponeri, E.; Vaccaro, K.; et al. Telemedicine and urban diabetes during COVID-19 pandemic in Milano, Italy during lock-down: Epidemiological and sociodemographic picture. Acta Diabetol. 2021, 58, 919–927. [Google Scholar] [CrossRef]
- Alessi, J.; de Oliveira, G.B.; Franco, D.W.; Becker, A.S.; Knijnik, C.P.; Kobe, G.L.; Amaral, B.B.; de Brito, A.; Schaan, B.D.; Telo, G.H. Telehealth strategy to mitigate the negative psychological impact of the COVID-19 pandemic on type 2 diabetes: A randomized controlled trial. Acta Diabetol. 2021, 58, 899–909. [Google Scholar] [CrossRef]
- Sharma, V.; Feldman, M.; Sharma, R. Telehealth Technologies in Diabetes Self-management and Education. J. Diabetes Sci. Technol. 2024, 18, 148–158. [Google Scholar] [CrossRef]
- Cangelosi, G.; Grappasonni, I.; Pantanetti, P.; Scuri, S.; Garda, G.; Thu, N.C.T.; Petrelli, F. Nurse Case Manager Lifestyle Medicine (NCMLM) in the Type Two Diabetes patient concerning post COVID-19 Pandemic management: Integrated-Scoping literature review. Ann. Ig. Med. Prev. Comunità 2022, 34, 585–602. [Google Scholar] [CrossRef]
- Cangelosi, G.; Mancin, S.; Pantanetti, P.; Nguyen, C.C.T.; Morales Palomares, S.; Biondini, F.; Sguanci, M.; Petrelli, F. Lifestyle Medicine Case Manager Nurses for Type Two Diabetes Patients: An Overview of a Job Description Frame-work—A Narrative Review. Diabetology 2024, 5, 375–388. [Google Scholar] [CrossRef]
- Rosta, L.; Menyhart, A.; Mahmeed, W.A.; Al-Rasadi, K.; Al-Alawi, K.; Banach, M.; Banerjee, Y.; Ceriello, A.; Cesur, M.; Cosentino, F.; et al. Telemedicine for diabetes management during COVID-19: What we have learnt, what and how to implement. Front. Endocrinol. 2023, 14, 1129793. [Google Scholar] [CrossRef] [PubMed]

| Gender | Participants (n) | Percentage (%) | Average Age | Average Number of Family Members | Employment Status % (n) |
|---|---|---|---|---|---|
| Male | 73 | 70.87% | 68 | 2.69 | Employed: 50.7% (n = 37) Retired: 43.8% (n = 32) Unemployed: 5.5% (n = 4) |
| Female | 30 | 29.13% | 67 | 2.69 | Employed: 43.3% (n = 13) Retired: 50.0% (n = 15) Unemployed: 6.7% (n = 2) |
| Item | Sample (n) | Mean | SD |
|---|---|---|---|
| 1 | 103 | 1.84 | 1.45 |
| 2 | 103 | 2.58 | 1.69 |
| 3 | 103 | 4.03 | 1.40 |
| 4 | 103 | 4.20 | 1.19 |
| 5 | 103 | 3.62 | 1.62 |
| 6 | 103 | 2.34 | 1.61 |
| 7 | 103 | 4.19 | 1.42 |
| 8 | 103 | 4.16 | 1.53 |
| 9 | 103 | 1.45 | 1.12 |
| 10 | 103 | 2.63 | 1.73 |
| 11 | 103 | 3.83 | 1.50 |
| 12 | 103 | 3.93 | 1.52 |
| 13 | 103 | 2.96 | 1.69 |
| 14 | 103 | 2.55 | 1.72 |
| 15 | 103 | 2.19 | 1.70 |
| 16 | 103 | 1.73 | 1.42 |
| 17 | 103 | 2.76 | 1.80 |
| 18 | 103 | 1.97 | 1.56 |
| 19 | 103 | 1.59 | 1.26 |
| 20 | 103 | 1.73 | 1.34 |
| 21 | 103 | 2.17 | 1.62 |
| 22 | 103 | 2.27 | 1.66 |
| 23 | 103 | 4.37 | 1.31 |
| 24 | 103 | 2.71 | 1.70 |
| 25 | 103 | 1.99 | 1.50 |
| 26 | 103 | 2.31 | 1.34 |
| Items | Sample (n) | Mean | SD |
|---|---|---|---|
| Fruit | 103 | 2.58 | 1.18 |
| Vegetables | 103 | 0.88 | 0.45 |
| Legumes | 103 | 1.04 | 0.64 |
| Cereals | 103 | 1.97 | 0.17 |
| Fish | 103 | 1.07 | 0.51 |
| Meat and meat products | 103 | 1.19 | 0.60 |
| Dairy products | 103 | 1.14 | 0.71 |
| Alcohol | 103 | 1.34 | 0.59 |
| Olive oil | 103 | 1.89 | 0.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cangelosi, G.; Mancin, S.; Pantanetti, P.; Sguanci, M.; Morales Palomares, S.; De Luca, A.; Biondini, F.; Tartaglia, F.; Ferrara, G.; Petrelli, F. Impact of the COVID-19 Pandemic on Lifestyle Behavior and Clinical Care Pathway Management in Type 2 Diabetes: A Retrospective Cross-Sectional Study. Medicina 2024, 60, 1624. https://doi.org/10.3390/medicina60101624
Cangelosi G, Mancin S, Pantanetti P, Sguanci M, Morales Palomares S, De Luca A, Biondini F, Tartaglia F, Ferrara G, Petrelli F. Impact of the COVID-19 Pandemic on Lifestyle Behavior and Clinical Care Pathway Management in Type 2 Diabetes: A Retrospective Cross-Sectional Study. Medicina. 2024; 60(10):1624. https://doi.org/10.3390/medicina60101624
Chicago/Turabian StyleCangelosi, Giovanni, Stefano Mancin, Paola Pantanetti, Marco Sguanci, Sara Morales Palomares, Alessia De Luca, Federico Biondini, Francesco Tartaglia, Gaetano Ferrara, and Fabio Petrelli. 2024. "Impact of the COVID-19 Pandemic on Lifestyle Behavior and Clinical Care Pathway Management in Type 2 Diabetes: A Retrospective Cross-Sectional Study" Medicina 60, no. 10: 1624. https://doi.org/10.3390/medicina60101624






