The Arthroscopic Biceps Rerouting Technique Shows Better Early Clinical Outcomes within 1 Year Than Partial Repair in Large to Massive Rotator Cuff Tears
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Baseline Characteristics
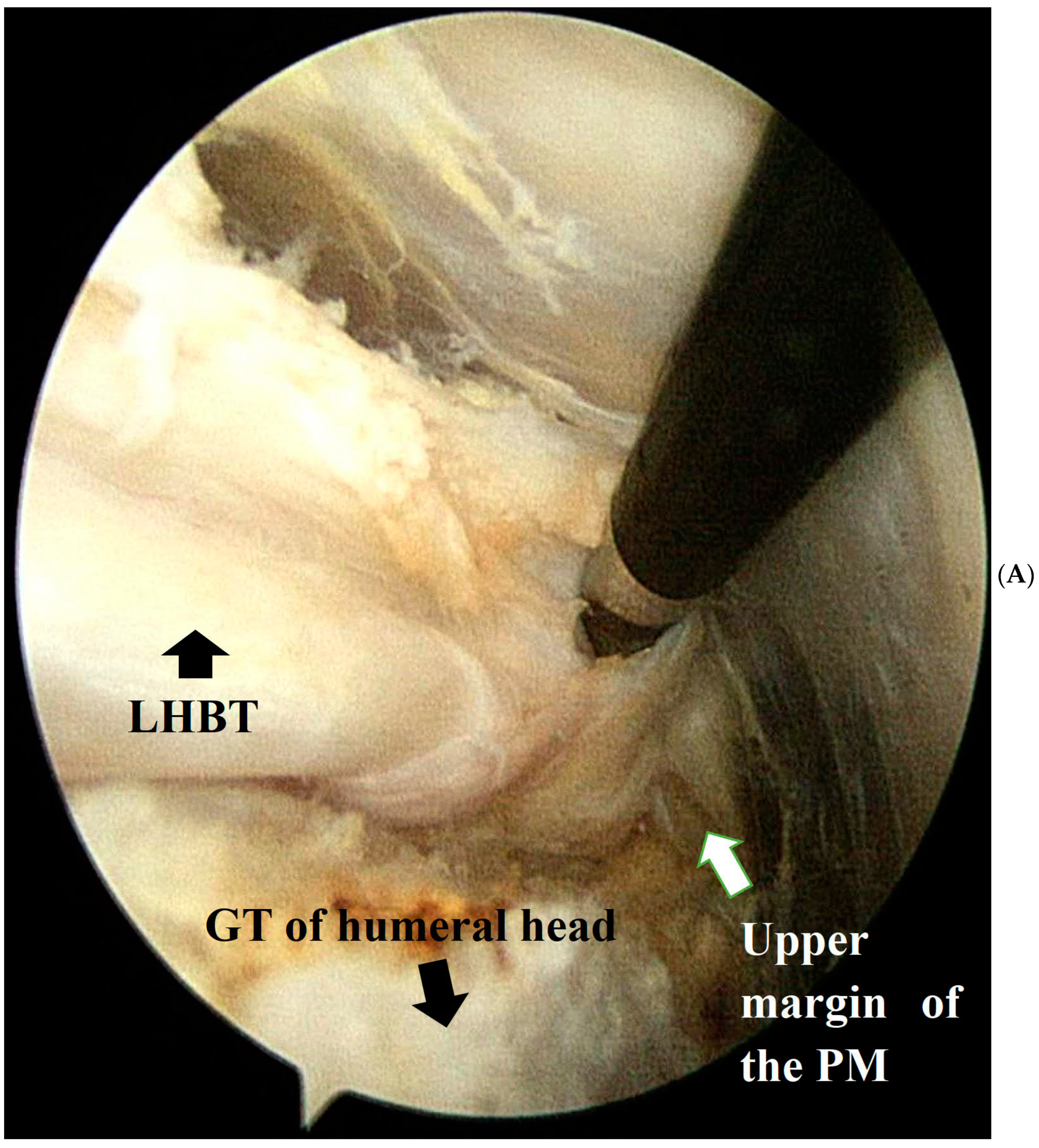
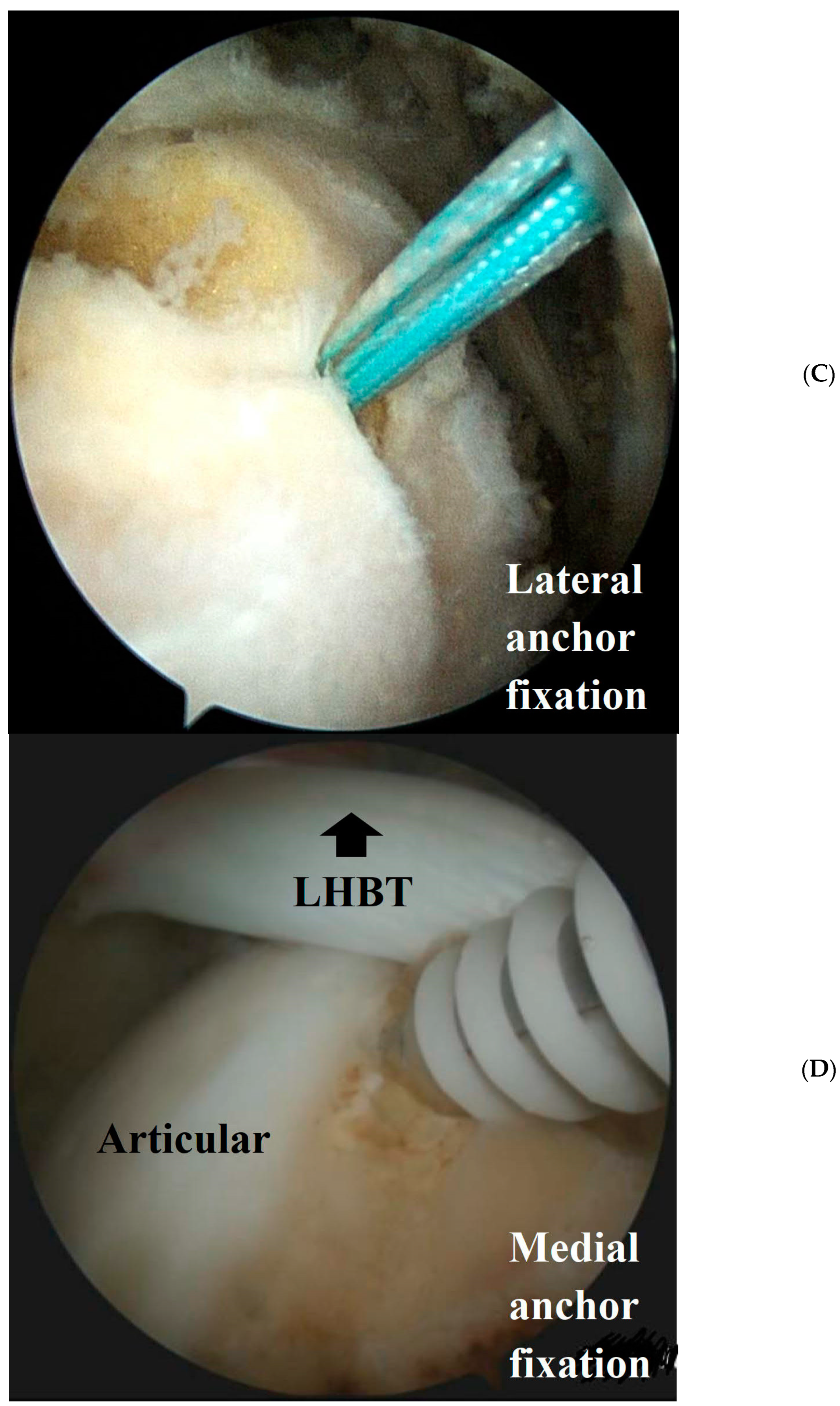
2.3. Surgical Technique
2.4. Clinical and Radiological Evaluation
2.5. Rehabilitation
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bedi, A.; Dines, J.; Warren, R.F.; Dines, D.M. Massive tears of the rotator cuff. J. Bone Jt. Surg. Am. 2010, 92, 1894–1908. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Kim, Y.H.; Chun, Y.M. Arthroscopic Partial Repair of Massive Contracted Rotator Cuff Tears. Clin. Shoulder Elb. 2014, 17, 44–47. [Google Scholar] [CrossRef]
- Rho, J.Y.; Kwon, Y.S.; Choi, S. Current Concepts and Recent Trends in Arthroscopic Treatment of Large to Massive Rotator Cuff Tears: A Review. Clin. Shoulder Elb. 2019, 22, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, S.S. Reconciling the paradox of rotator cuff repair versus debridement: A unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy 1994, 10, 4–19. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, S.S. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin. Orthop. Relat. Res. 1991, 267, 45–56. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, I.S.; Kim, S.H.; Lee, W.Y.; Chun, Y.M. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy 2012, 28, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Shon, M.S.; Koh, K.H.; Lim, T.K.; Kim, W.J.; Kim, K.C.; Yoo, J.C. Arthroscopic Partial Repair of Irreparable Rotator Cuff Tears: Preoperative Factors Associated with Outcome Deterioration over 2 Years. Am. J. Sports Med. 2015, 43, 1965–1975. [Google Scholar] [CrossRef] [PubMed]
- Han, S.Y.; Lee, T.Q.; Wright, D.J.; Park, I.J.; Mauro, M.; McGarry, M.H.; Lee, H.J.; Kim, Y.S. Effect of biceps rerouting technique to restore glenohumeral joint stability for large irreparable rotator cuff tears: A cadaveric biomechanical study. J. Shoulder Elb. Surg. 2020, 29, 1425–1434. [Google Scholar] [CrossRef]
- Veen, E.J.D.; Stevens, M.; Diercks, R.L. Biceps Autograft Augmentation for Rotator Cuff Repair: A Systematic Review. Arthroscopy 2018, 34, 1297–1305. [Google Scholar] [CrossRef]
- Park, S.R.; Sun, D.H.; Kim, J.; Lee, H.J.; Kim, J.B.; Kim, Y.S. Is augmentation with the long head of the biceps tendon helpful in arthroscopic treatment of irreparable rotator cuff tears? J. Shoulder Elb. Surg. 2018, 27, 1969–1977. [Google Scholar] [CrossRef]
- Lin, J.; Qi, W.; Liu, Z.; Chen, K.; Li, X.; Yan, Y.; Xu, X.; Xue, X.; Yang, Y.; Pan, X. An arthroscopic technique for full-thickness rotator cuff repair by transposition of the long head of biceps. Orthop. Traumatol. Surg. Res. 2019, 105, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Han, F.; Kong, C.H.; Hasan, M.Y.; Ramruttun, A.K.; Kumar, V.P. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop. Traumatol. Surg. Res. 2019, 105, 257–263. [Google Scholar] [CrossRef]
- El-Shaar, R.; Soin, S.; Nicandri, G.; Maloney, M.; Voloshin, I. Superior Capsular Reconstruction with a Long Head of the Biceps Tendon Autograft: A Cadaveric Study. Orthop. J. Sports Med. 2018, 6, 2325967118785365. [Google Scholar] [CrossRef]
- Kim, Y.S.; Lee, H.J.; Park, I.; Sung, G.Y.; Kim, D.J.; Kim, J.H. Arthroscopic In Situ Superior Capsular Reconstruction Using the Long Head of the Biceps Tendon. Arthrosc. Tech. 2018, 7, e97–e103. [Google Scholar] [CrossRef] [PubMed]
- Rhee, S.M.; Youn, S.M.; Park, J.H.; Rhee, Y.G. Biceps Rerouting for Semirigid Large-to-Massive Rotator Cuff Tears. Arthroscopy 2021, 37, 2769–2779. [Google Scholar] [CrossRef]
- Yoo, J.C.; Ahn, J.H.; Koh, K.H.; Lim, K.S. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy 2009, 25, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Sugaya, H.; Maeda, K.; Matsuki, K.; Moriishi, J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: Single-row versus dual-row fixation. Arthroscopy 2005, 21, 1307–1316. [Google Scholar] [CrossRef]
- Xu, J.; Li, Y.; Zhang, X.; Han, K.; Ye, Z.; Wu, C.; Jiang, J.; Yan, X.; Su, W.; Zhao, J. The Biomechanical and Histological Processes of Rerouting Biceps to Treat Chronic Irreparable Rotator Cuff Tears in a Rabbit Model. Am. J. Sports Med. 2022, 50, 347–361. [Google Scholar] [CrossRef]
- Zabrzyński, J.; Gagat, M.; Łapaj, Ł.; Paczesny, Ł.; Yataganbaba, A.; Szwedowski, D.; Huri, G. Relationship between long head of the biceps tendon histopathology and long-term functional results in smokers. A time to reevaluate the Bonar score? Ther. Adv. Chronic Dis. 2021, 12, 2040622321990262. [Google Scholar] [CrossRef]
- Mori, D.; Funakoshi, N.; Yamashita, F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: Patch autograft procedure versus partial repair procedure. Arthroscopy 2013, 29, 1911–1921. [Google Scholar] [CrossRef]
- Wellmann, M.; Lichtenberg, S.; da Silva, G.; Magosch, P.; Habermeyer, P. Results of arthroscopic partial repair of large retracted rotator cuff tears. Arthroscopy 2013, 29, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Koh, K.H.; Lim, T.K.; Park, Y.E.; Lee, S.W.; Park, W.H.; Yoo, J.C. Preoperative factors affecting footprint coverage in rotator cuff repair. Am. J. Sports Med. 2014, 42, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Jeong, J.Y.; Park, C.D.; Kang, S.G.; Yoo, J.C. Evaluation of the Risk Factors for a Rotator Cuff Retear after Repair Surgery. Am. J. Sports Med. 2017, 45, 1755–1761. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, H.J.; Park, T.Y.; Lee, J.U.; Kim, Y.S. Preliminary Outcomes of Arthroscopic Biceps Rerouting for the Treatment of Large to Massive Rotator Cuff Tears. J. Shoulder Elb. Surg. 2020, 36, 1384–1392. [Google Scholar] [CrossRef]
- Zabrzynski, J.; Huri, G.; Gagat, M.; Lapaj, L.; Yataganbaba, A.; Szwedowski, D.; Askin, M.; Paczesny, L. The Impact of Smoking on Clinical Results following the Rotator Cuff and Biceps Tendon Complex Arthroscopic Surgery. J. Clin. Med. 2021, 10, 599. [Google Scholar] [CrossRef]
- Zabrzynski, J.; Huri, G.; Gryckiewicz, S.; Cetik, R.M.; Szwedowski, D.; Lapaj, L.; Gagat, M.; Paczesny, L. Biceps Tenodesis versus Tenotomy with Fast Rehabilitation Protocol—A Functional Perspective in Chronic Tendinopathy. J. Clin. Med. 2020, 9, 3938. [Google Scholar] [CrossRef]
- Belk, J.W.; Kraeutler, M.J.; Houck, D.A.; Chrisman, A.N.; Scillia, A.J.; McCarty, E.C. Biceps tenodesis versus tenotomy: A systematic review and meta-analysis of level I randomized controlled trials. J. Shoulder Elb. Surg. 2021, 30, 951–960. [Google Scholar] [CrossRef]



| Group I (n = 31) | Group II (n = 41) | p Value | |
|---|---|---|---|
| Age, years | 67.10 | 65.49 | 0.87 |
| Sex, male/female, n | 10/21 | 15/26 | 0.69 |
| Follow-up period (range), months | 23.25 (12–36) | 21.24 (12–34) | 0.93 |
| Tear size, mm | |||
| medial to lateral | 31.9 | 31.3 | 0.14 |
| anterior to posterior | 26.1 | 27.4 | 0.71 |
| Acromiohumeral interval | 7.89 | 7.91 | 0.83 |
| Fatty infiltration (Goutallier classification), n (%) | 0.13 | ||
| Grade 1 | 0 (0) | 0 (0) | |
| Grade 2 | 4 (14.8) | 10 (11.1) | |
| Grade 3 | 19 (59.2) | 25 (66.6) | |
| Grade 4 | 8 (25.9) | 6 (22.2) | |
| Initial ROM | |||
| Forward flexion, ° | 140.38 ± 9.89 | 140.19 ± 18.35 | 0.97 |
| External rotation at side, ° | 80.38 ± 10.76 | 82.69 ± 14.02 | 0.52 |
| External rotation at 90° of abduction, ° | 83.85 ± 7.52 | 84.23 ± 13.01 | 0.90 |
| Internal rotation, vertebral level | 9.88 ± 2.79 | 9.92 ± 2.81 | 0.96 |
| Initial clinical score | |||
| VAS score for pain | 3.57 ± 1.87 | 2.96 ± 2.05 | 0.06 |
| ASES score | 55.86 ± 13.38 | 54.67 ± 22.33 | 0.80 |
| Constant score | 62.50 ± 16.38 | 60.08 ± 19.18 | 0.49 |
| Korean Shoulder Score | 60.73 ± 14.51 | 53.38 ± 19.71 | 0.24 |
| Preoperative | Last Follow-Up | p Value | |
|---|---|---|---|
| Range of motion | |||
| Forward flexion, ° | 140.38 ± 9.89 | 145.18 ± 6.57 | 0.48 |
| External rotation at side, ° | 80.38 ± 10.76 | 82.92 ± 9.99 | 0.56 |
| External rotation at 90° of abduction | 83.85 ± 7.52 | 86.54 ± 6.29 | 0.21 |
| Internal rotation, vertebral level | 9.88 ± 2.79 | 10.95 ± 1.39 | 0.08 |
| Clinical outcome | |||
| VAS | 3.57 ± 1.87 | 1.57 ± 0.98 | <0.001 |
| ASES score | 55.86 ± 13.38 | 79.94 ± 11.17 | <0.001 |
| CS | 62.50 ± 16.38 | 81.56 ± 11.25 | <0.001 |
| KSS | 60.73 ± 14.51 | 81.31 ± 16.87 | <0.001 |
| Preoperative | Last Follow-Up | p Value | |
|---|---|---|---|
| Range of motion | |||
| Forward flexion, ° | 140.19 ± 18.35 | 146.48 ± 6.32 | 0.15 |
| External rotation at side, ° | 82.69 ± 14.02 | 86.67 ± 6.37 | 0.16 |
| External rotation at 90° of abduction | 84.23 ± 13.01 | 87.69 ± 5.14 | 0.63 |
| Internal rotation, vertebral level | 9.92 ± 2.81 | 10.95 ± 2.01 | 0.09 |
| Clinical outcome | |||
| VAS | 2.96 ± 2.05 | 1.33 ± 1.34 | <0.001 |
| ASES score | 54.67 ± 22.33 | 82.83 ± 11.94 | <0.001 |
| CS | 60.08 ± 19.18 | 82.94 ± 7.17 | <0.001 |
| KSS | 53.38 ± 19.71 | 85.69 ± 10.21 | <0.001 |
| Preoperative | 3 Months | 6 Months | 12 Months | Last Follow-Up | |
|---|---|---|---|---|---|
| Forward flexion, ° | |||||
| Group I | 140.38 ± 9.89 | 99.82 ± 22.21 | 126.72 ± 15.59 | 137.24 ± 9.87 | 145.18 ± 6.57 |
| Group II | 140.19 ± 18.35 | 92.07 ± 29.20 | 128.44 ± 19.04 | 143.79 ± 8.09 | 146.48 ± 6.32 |
| p value | 0.97 | 0.25 | 0.69 | 0.02 | 0.47 |
| External rotation at side, ° | |||||
| Group I | 80.38 ± 10.76 | 35.20 ± 21.63 | 66.00 ± 17.93 | 75.71 ± 12.60 | 82.92 ± 9.99 |
| Group II | 82.69 ± 14.02 | 35.60 ± 23.11 | 72.00 ± 12.43 | 82.14 ± 6.86 | 86.67 ± 6.37 |
| p value | 0.52 | 0.95 | 0.13 | 0.04 | 0.19 |
| External rotation at 90° of abduction | |||||
| Group I | 83.85 ± 7.52 | 42.40 ± 23.50 | 74.84 ± 14.35 | 81.79 ± 8.63 | 86.54 ± 6.29 |
| Group II | 84.23 ± 13.01 | 35.20 ± 22.94 | 74.52 ± 12.34 | 83.57 ± 9.89 | 87.69 ± 5.14 |
| p value | 0.90 | 0.30 | 0.92 | 0.50 | 0.50 |
| Internal rotation, vertebral level | |||||
| Group I | 9.88 ± 2.79 | 2.74 ± 2.99 | 7.16 ± 3.33 | 10.43 ± 1.86 | 10.95 ± 1.39 |
| Group II | 9.92 ± 2.81 | 6.26 ± 3.37 | 9.48 ± 2.26 | 10.90 ± 1.61 | 10.95 ± 2.01 |
| p value | 0.96 | 0.00 | 0.01 | 0.45 | 1.00 |
| Preoperative | 3 Months | 6 Months | 12 Months | Last Follow-up | |
|---|---|---|---|---|---|
| VAS score for pain | |||||
| Group I | 3.57 ± 1.87 | 2.81 ± 1.71 | 2.02 ± 1.20 | 2.49 ± 2.45 | 1.57 ± 0.98 |
| Group II | 2.96 ± 2.05 | 2.58 ± 1.74 | 2.58 ± 1.67 | 1.24 ± 1.32 | 1.33 ± 1.34 |
| p value | 0.06 | 0.59 | 0.15 | 0.11 | 0.65 |
| ASES score | |||||
| Group I | 55.86 ± 13.38 | 64.63 ± 19.18 | 71.90 ± 12.07 | 71.25 ± 21.72 | 79.94 ± 11.17 |
| Group II | 54.67 ± 22.33 | 65.80 ± 16.61 | 73.71 ± 15.51 | 83.13 ± 12.89 | 82.83 ± 11.94 |
| p value | 0.80 | 0.83 | 0.70 | 0.047 | 0.45 |
| CS | |||||
| Group I | 62.50 ± 16.38 | 63.38 ± 15.15 | 75.63 ± 9.15 | 74.13 ± 13.62 | 81.56 ± 11.25 |
| Group II | 60.08 ± 19.18 | 66.00 ± 16.20 | 77.42 ± 12.14 | 80.97 ± 14.42 | 82.94 ± 7.17 |
| p value | 0.49 | 0.98 | 0.54 | 0.25 | 0.72 |
| KSS | |||||
| Group I | 60.73 ± 14.51 | 62.43 ± 12.94 | 73.52 ± 12.45 | 70.60 ± 15.72 | 81.31 ± 16.87 |
| Group II | 53.38 ± 19.71 | 63.48 ± 15.85 | 78.43 ± 12.47 | 80.67 ± 14.30 | 85.69 ± 10.21 |
| p value | 0.24 | 0.93 | 0.12 | 0.048 | 0.33 |
| Group I (n = 31) | Group II (n = 41) | |
|---|---|---|
| Type I | 2 | 6 |
| Type II | 7 | 10 |
| Type III | 13 | 17 |
| Type IV | 2 | 5 |
| Type V | 7 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.-S.; Ham, K.-H.; Kim, Y.-S. The Arthroscopic Biceps Rerouting Technique Shows Better Early Clinical Outcomes within 1 Year Than Partial Repair in Large to Massive Rotator Cuff Tears. Medicina 2024, 60, 240. https://doi.org/10.3390/medicina60020240
Park H-S, Ham K-H, Kim Y-S. The Arthroscopic Biceps Rerouting Technique Shows Better Early Clinical Outcomes within 1 Year Than Partial Repair in Large to Massive Rotator Cuff Tears. Medicina. 2024; 60(2):240. https://doi.org/10.3390/medicina60020240
Chicago/Turabian StylePark, Hyung-Seok, Kwon-Hyoung Ham, and Yang-Soo Kim. 2024. "The Arthroscopic Biceps Rerouting Technique Shows Better Early Clinical Outcomes within 1 Year Than Partial Repair in Large to Massive Rotator Cuff Tears" Medicina 60, no. 2: 240. https://doi.org/10.3390/medicina60020240
APA StylePark, H.-S., Ham, K.-H., & Kim, Y.-S. (2024). The Arthroscopic Biceps Rerouting Technique Shows Better Early Clinical Outcomes within 1 Year Than Partial Repair in Large to Massive Rotator Cuff Tears. Medicina, 60(2), 240. https://doi.org/10.3390/medicina60020240






