A Lonelier World after COVID-19: Longitudinal Population-Based Study of Well-Being, Emotional and Social Loneliness, and Suicidal Behaviour in Slovenia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Procedure
2.2. Participants
2.3. Measures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Horton, R. Offline: COVID-19 is not a pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. COVID-19: Mental Health and Wellbeing Surveillance Report. Available online: https://www.gov.uk/government/publications/covid-19-mental-health-and-wellbeing-surveillance-report (accessed on 5 January 2021).
- John, A.; Pirkis, J.; Gunnell, D.; Appleby, L.; Morrissey, J. Trends in suicide during the COVID-19 pandemic. BMJ 2020, 371, m4352. [Google Scholar] [CrossRef] [PubMed]
- Lavrič, M.; Gomboc, V.; Krohne, N.; Podlogar, T.; Poštuvan, V.; Šedivy, N.Z.; de Leo, D. Concerns, Positive Changes, and Suggestions for Psychological Support during COVID-19: A Thematic Analysis. Sociol. Mind 2020, 10, 187–199. [Google Scholar] [CrossRef]
- Kavčič, T.; Avsec, A.; Zager Kocjan, G. Od začetka do konca uradne epidemije COVID-19 v Sloveniji: Stresorji, tress in blagostanje. In Psihologija Pandemije: Posamezniki in Družba v Času Koronske Kriz; Lep, Z., Hacin Beyazoglu, K., Eds.; Znanstvena založba Filozofske fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 23–35. [Google Scholar]
- Gomboc, V.; Krohn, N.; Lavrič, M.; Podlogar, T.; Poštuvan, V.; Zadravec Šedivy, N.; De Leo, D. Primerjava osamljenosti in subjektivnega blagostanja v normalnih in izrednih razmerah. In Psihologija Pandemije: Posamezniki in Družba v Času Koronske Kriz; Lep, Z., Hacin Beyazoglu, K., Eds.; Znanstvena založba Filozofske fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 79–89. [Google Scholar]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry J. Assoc. Eur. Psychiatr. 2020, 63, 32. [Google Scholar] [CrossRef] [PubMed]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Dailey, N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020, 290. [Google Scholar] [CrossRef] [PubMed]
- Luchetti, M.; Lee, J.H.; Aschwanden, D.; Sesker, A.; Strickhouser, J.E.; Terracciano, A.; Sutin, A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020, 75, 897–908. [Google Scholar] [CrossRef]
- Carollo, A.; Bizzego, A.; Gabrieli, G.; Wong, K.K.; Raine, A.; Esposito, G. I’m alone but not lonely. U-shaped pattern of self-perceived loneliness during the COVID-19 pandemic in the UK and Greece. Public Health Pract. 2021, 2, 100219. [Google Scholar] [CrossRef]
- Einav, M.; Margalit, M. Loneliness before and after COVID-19: Sense of Coherence and Hope as Coping Mechanisms. Int. J. Environ. Res. Public Health 2023, 20, 5840. [Google Scholar] [CrossRef]
- Farooq, S.; Tunmore, J.; Wajid Ali, M.; Ayub, M. Suicide, self-harm and suicidal ideation during COVID-19: A systematic review. Psychiatry Res. 2021, 306, 114228. [Google Scholar] [CrossRef]
- Ayuso-Mateos, J.L.; Morillo, D.; Haro, J.M.; Olaya, B.; Lara, E.; Miret, M. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: A longitudinal study in the general population. Epidemiol. Psychiatr. Sci. 2021, 30, e49. [Google Scholar] [CrossRef]
- Papadopoulou, A.; Efstathiou, V.; Yotsidi, V.; Pomini, V.; Michopoulos, I.; Markopoulou, E.; Papadopoulou, M.; Tsigkaropoulou, E.; Kalemi, G.; Tournikioti, K.; et al. Suicidal ideation during COVID-19 lockdown in Greece: Prevalence in the community, risk and protective factors. Psychiatry Res. 2021, 297, 113713. [Google Scholar] [CrossRef] [PubMed]
- Pirkis, J.; John, A.; Shin, S.; DelPozo-Banos, M.; Arya, V.; Analuisa-Aguilar, P.; Appleby, L.; Arensman, E.; Bantjes, J.; Baran, A.; et al. Suicide trends in the early months of the COVID-19 pandemic: An interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 2021, 8, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Farahi, S.M.M.M.; Dalexis, R.D.; Darius, W.P.; Bekarkhanechi, F.M.; Poisson, H.; Broussard, C.; Ukwu, G.; Auguste, E.; Nguyen, D.D.; et al. The global evolution of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2022, 315, 70–95. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022, 296, 567–576. [Google Scholar] [CrossRef]
- Salanti, G.; Peter, N.; Tonia, T.; Holloway, A.; White, I.R.; Darwish, L.; Low, N.; Egger, M.; Haas, A.D.; Fazel, S.; et al. The Impact of the COVID-19 Pandemic and Associated Control Measures on the Mental Health of the General Population: A Systematic Review and Dose-Response Meta-analysis. Ann. Intern. Med. 2022, 175, 1560–1571. [Google Scholar] [CrossRef]
- Shevlin, M.; Butter, S.; McBride, O.; Murphy, J.; Gibson-Miller, J.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.P.; McKay, R.; et al. Refuting the myth of a ‘tsunami’ of mental ill-health in populations affected by COVID-19: Evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol. Med. 2023, 53, 429–437. [Google Scholar] [CrossRef]
- Batterham, P.J.; Calear, A.L.; McCallum, S.M.; Morse, A.R.; Banfield, M.; Farrer, L.M.; Gulliver, A.; Cherbuin, N.; Rodney Harris, R.M.; Shou, Y.; et al. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Med. J. Aust. 2021, 214, 462–468. [Google Scholar] [CrossRef]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Miller, M.A.; Dailey, N.S. Three months of loneliness during the COVID-19 lockdown. Psychiatry Res. 2020, 293, 113392. [Google Scholar] [CrossRef]
- Paykel, E.S.; Myers, J.K.; Lindenthal, J.J.; Tanner, J. Suicidal feelings in the general population: A prevalence study. Br. J. Psychiatry 1974, 124, 460–469. [Google Scholar] [CrossRef]
- De Jong Gierveld, J.; Van Tilburg, T. A 6-Item Scale for Overall, Emotional, and Social Loneliness: Confirmatory Tests on Survey Data. Res. Aging 2006, 28, 582–598. [Google Scholar] [CrossRef]
- The World Health Organisation—Five Well-Being Index (WHO-5). Available online: https://www.corc.uk.net/outcome-experience-measures/the-world-health-organisation-five-well-being-index-who-5/ (accessed on 27 December 2023).
- Field, A. Discovering Statistics, Repeated Measures ANOVA. 2016. Available online: https://www.discoveringstatistics.com/docs/repeatedmeasures.pdf (accessed on 27 December 2023).
- De Leo, D.; Draper, B.; Snowdon, J.; Kolves, K. Suicides in Older Adults: A Case-Control Psychological Autopsy Study in Australia. J. Psychiatr. Res. 2013, 47, 980–988. [Google Scholar] [CrossRef]
- Matthews, T.; Danese, A.; Caspi, A.; Fisher, H.L.; Goldman-Mellor, S.; Kepa, A.; Moffitt, T.E.; Odgers, C.L.; Arseneault, L. Lonely Young Adults in Modern Britain: Findings from an Epidemiological Cohort Study. Psychol. Med. 2019, 49, 268–277. [Google Scholar] [CrossRef]
- Statistical Office of the Republic of Slovenia. Available online: https://www.stat.si/StatWeb/en/Field/Index/10/ (accessed on 27 December 2023).
- Stanley, S.M.; Markman, H.J. Helping Couples in the Shadow of COVID-19. Fam. Process 2020, 59, 937–955. [Google Scholar] [CrossRef]
- Moreira, D.N.; Pinto da Costa, M. The impact of the COVID-19 pandemic in the precipitation of intimate partner violence. Int. J. Law Psychiatry 2020, 71, 101606. [Google Scholar] [CrossRef]
- Ahmed, N.; Barnett, P.; Greenburgh, A.; Pemovska, T.; Stefanidou, T.; Lyons, N.; Ikhtabi, S.; Talwar, S.; Francis, E.R.; Harris, S.M.; et al. Mental health in Europe during the COVID-19 pandemic: A systematic review. Lancet Psychiatry 2023, 10, 537–556. [Google Scholar] [CrossRef] [PubMed]
- Hawton, K.; Lascelles, K.; Pitman, A.; Gilbert, S.; Silverman, M. Assessment of suicide risk in mental health practice: Shifting from prediction to therapeutic assessment, formulation, and risk management. Lancet Psychiatry 2022, 9, 922–928. [Google Scholar] [CrossRef] [PubMed]
- Kirič, B.; Leben Novak, L.; Lušicky, P.; Drobnič Radobuljac, M. Suicidal Behavior in Emergency Child and Adolescent Psychiatric Service Users Before and During the 16 Months of the COVID-19 Pandemic. Front. Psychiatry 2022, 13, 893040. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Majeed, A.; Gill, H.; Tamura, J.; Ho, C.R.; Mansur, R.B.; Nasri, F.; Lee, Y.; Rosenblat, J.D.; Wong, E.; et al. The Effect of Loneliness on Distinct Health Outcomes: A Comprehensive Review and Meta-Analysis. Psychiatry Res. 2020, 294, 113514. [Google Scholar] [CrossRef] [PubMed]
- Mlakar, T. Statistical Office of the Republic of Slovenia. Available online: https://www.stat.si/StatWeb/en/News/Index/10572 (accessed on 19 January 2024).

| Wave 0 | Wave 1 | Wave 2 | Wave 3 | ||
|---|---|---|---|---|---|
| Age | 18–24 [N (%)] | 19 (4.31) | 8 (1.82) | 6 (1.36) | 2 (0.45) |
| 25–64 [N (%)] | 335 (76.14) | 316 (71.82) | 310 (70.46) | 310 (70.46) | |
| 65–79 [N (%)] | 86 (19.55) | 110 (25) | 112 (25.45) | 115 (26.14) | |
| >80 [N (%)] | / | 6 (1.36) | 12 (2.73) | 13 (2.95) |
| Measures | Wave 0 | Wave 1 | Wave 2 | Wave 3 | |
|---|---|---|---|---|---|
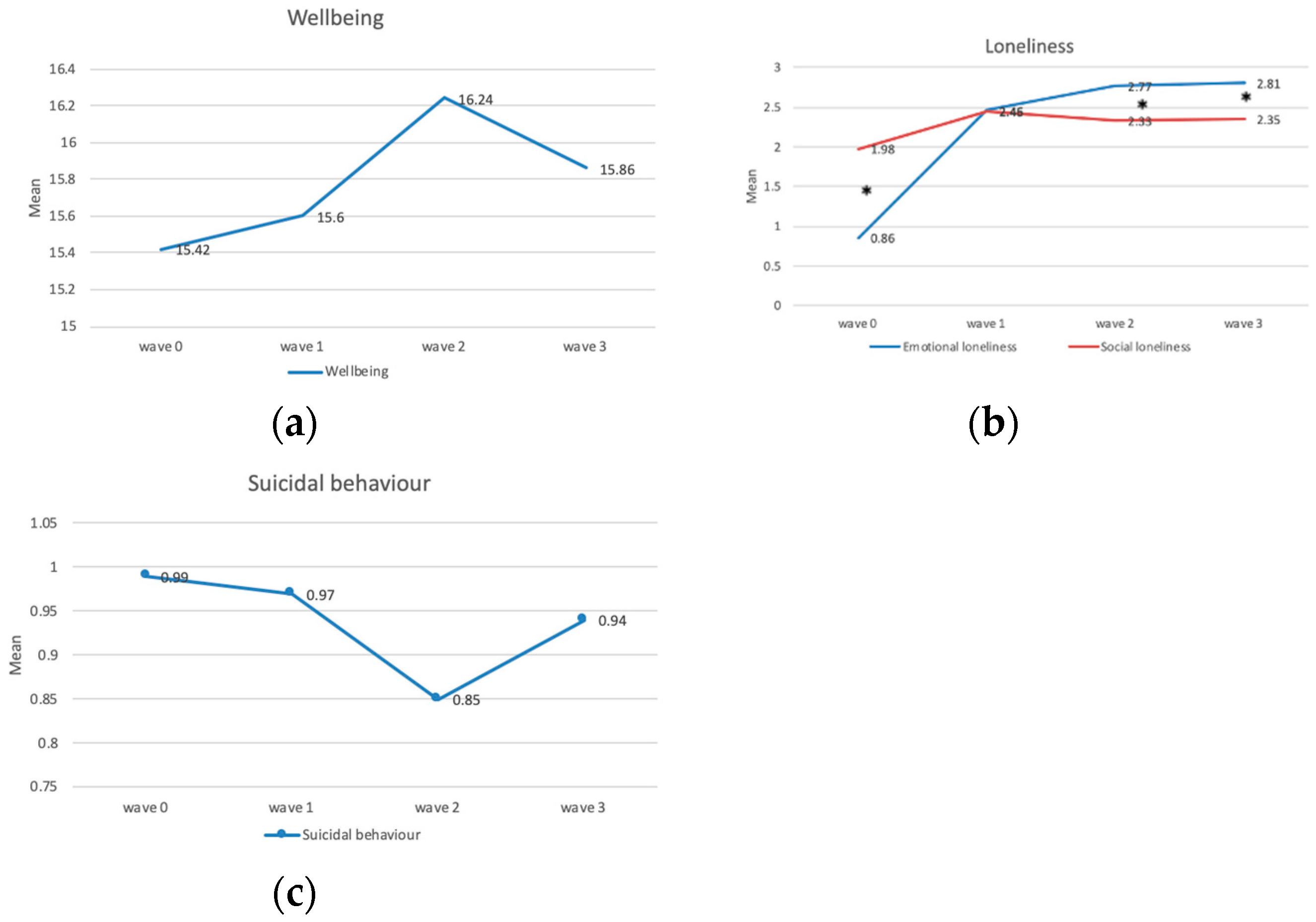
| Well-being | All [M ± SD] | 15.42 ± 4.67 | 15.60 ± 5.30 | 16.24 ± 4.92 | 15.86 ± 5.11 |
| Female [M ± SD] | 14.80 ± 4.80 | 14.73 ± 5.39 | 15.25 ± 5.16 | 14.94 ± 5.43 | |
| Male [M ± SD] | 15.98 ± 4.48 | 16.41 ± 5.11 | 17.16 ± 4.52 | 16.72 ± 4.65 | |
| Social Loneliness | All [M ± SD] | 1.98 ± 1.18 | 2.45 ± 0.97 | 2.33 ± 1.04 | 2.35 ± 1.02 |
| Female [M ± SD] | 1.82 ± 1.25 | 2.49 ± 0.93 | 2.32 ± 1.05 | 2.37 ± 1.00 | |
| Male [M ± SD] | 2.13 ± 1.08 | 2.42 ± 1.00 | 2.34 ± 1.03 | 2.33 ± 1.04 | |
| Emotional Loneliness | All [M ± SD] | 0.86 ± 1.06 | 2.46 ± 0.74 | 2.77 ± 0.57 | 2.81 ± 0.55 |
| Female [M ± SD] | 0.82 ± 1.05 | 2.39 ± 0.77 | 2.71 ± 0.61 | 2.75 ± 0.64 | |
| Male [M ± SD] | 0.90 ± 1.06 | 2.53 ± 0.70 | 2.83 ± 0.51 | 2.86 ± 0.44 | |
| Suicidal Behaviour | All [M ± SD] | 0.99 ± 2.25 | 0.97 ± 2.47 | 0.85 ± 2.19 | 0.94 ± 2.31 |
| Female [M ± SD] | 1.13 ± 2.52 | 1.18 ± 2.70 | 0.94 ± 2.30 | 0.99 ± 2.26 | |
| Male [M ± SD] | 0.86 ± 1.97 | 0.79 ± 2.21 | 0.76 ± 2.09 | 0.90 ± 2.35 |
| Measures | Wave 0 | Wave 1 | Wave 2 | Wave 3 | |
|---|---|---|---|---|---|
| Well-being | All [M ± SD] | 15.42 ± 4.67 | 15.60 ± 5.30 | 16.24 ± 4.92 | 15.86 ± 5.11 |
| 18–24 [M ± SD] | 14.95 ± 4.39 | 12.88 ± 4.85 | 14.83 ± 3.19 | 16.0 ± 1.41 | |
| 25–64 [M ± SD] | 15.03 ± 4.81 | 15.34 ± 5.26 | 15.95 ± 4.96 | 15.42 ± 5.24 | |
| 65–79 [M ± SD] | 17.03 ± 3.79 | 16.65 ± 5.24 | 17.00 ± 4.74 | 16.97 ± 4.62 | |
| >80 [M ± SD] | / | 14.17 ± 7.41 | 17.58 ± 5.87 | 16.62 ± 5.16 | |
| Social Loneliness | All [M ± SD] | 1.98 ± 1.18 | 2.45 ± 0.97 | 2.33 ± 1.04 | 2.35 ± 1.02 |
| 18–24 [M ± SD] | 1.95 ± 1.31 | 2.50 ± 0.76 | 1.33 ± 1.37 | 3.00 ± 0.00 | |
| 25–64 [M ± SD] | 2.03 ± 1.14 | 2.41 ± 1.00 | 2.28 ± 1.09 | 2.27 ± 1.06 | |
| 65–79 [M ± SD] | 1.80 ± 1.27 | 2.60 ± 0.87 | 2.51 ± 0.84 | 2.57 ± 0.85 | |
| >80 [M ± SD] | / | 2.33 ± 1.21 | 2.58 ± 0.79 | 2.31 ± 1.11 | |
| Emotional Loneliness | All [M ± SD] | 0.86 ± 1.06 | 2.46 ± 0.74 | 2.77 ± 0.57 | 2.81 ± 0.55 |
| 18–24 [M ± SD] | 1.32 ± 1.20 | 1.62 ± 1.06 | 2.50 ± 0.84 | 3.00 ± 0.00 | |
| 25–64 [M ± SD] | 0.86 ± 1.06 | 2.52 ± 0.70 | 2.76 ± 0.58 | 2.76 ± 0.61 | |
| 65–79 [M ± SD] | 0.76 ± 0.99 | 2.38 ± 0.78 | 2.82 ± 0.51 | 2.92 ± 0.27 | |
| >80 [M ± SD] | / | 2.17 ± 0.75 | 2.67 ± 0.65 | 2.85 ± 0.55 | |
| Suicidal Behaviour | All [M ± SD] | 0.99 ± 2.25 | 0.97 ± 2.47 | 0.85 ± 2.19 | 0.94 ± 2.31 |
| 18–24 [M ± SD] | 1.68 ± 3.53 | 0.75 ± 0.89 | 1.33 ± 2.34 | 0.00 ± 0.00 | |
| 25–64 [M ± SD] | 0.98 ± 2.25 | 1.05 ± 2.64 | 0.90 ± 2.19 | 1.02 ± 2.43 | |
| 65–79 [M ± SD] | 0.87 ± 1.88 | 0.65 ± 1.54 | 0.55 ± 1.37 | 0.63 ± 1.44 | |
| >80 [M ± SD] | / | 3.00 ± 5.93 | 2.00 ± 5.78 | 2.08 ± 4.50 |
| Measures | F | df | p |
|---|---|---|---|
| Well-being | 5.82 | 2.85 | <0.01 |
| Social loneliness | 17.93 | 1.91 | <0.01 |
| Emotional loneliness | 625.45 | 1.815 | <0.01 |
| Suicidal behaviour | 0.62 | 2.737 | 0.59 |
| Measures | Comparisons | F | df | p |
|---|---|---|---|---|
| Well-being | Wave 0 vs. Wave 1 | 0.65 | 1 | 0.42 |
| Wave 1 vs. Wave 2 | 9.77 | 1 | <0.01 | |
| Wave 2 vs. Wave 3 | 4.55 | 1 | 0.03 | |
| Social loneliness | Wave 0 vs. Wave 1 | 32.74 | 1 | <0.01 |
| Wave 1 vs. Wave 2 | 7.71 | 1 | 0.01 | |
| Wave 2 vs. Wave 3 | 0.14 | 1 | 0.71 | |
| Emotional loneliness | Wave 0 vs. Wave 1 | 68.87 | 1 | <0.01 |
| Wave 1 vs. Wave 2 | 544.58 | 1 | <0.01 | |
| Wave 2 vs. Wave 3 | 1.47 | 1 | 0.23 | |
| Suicidal behaviour | Wave 0 vs. Wave 1 | 0.01 | 1 | 0.91 |
| Wave 1 vs. Wave 2 | 1.55 | 1 | 0.22 | |
| Wave 2 vs. Wave 3 | 1.10 | 1 | 0.29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poštuvan, V.; Krohne, N.; Lavrič, M.; Gomboc, V.; De Leo, D.; Rojs, L. A Lonelier World after COVID-19: Longitudinal Population-Based Study of Well-Being, Emotional and Social Loneliness, and Suicidal Behaviour in Slovenia. Medicina 2024, 60, 312. https://doi.org/10.3390/medicina60020312
Poštuvan V, Krohne N, Lavrič M, Gomboc V, De Leo D, Rojs L. A Lonelier World after COVID-19: Longitudinal Population-Based Study of Well-Being, Emotional and Social Loneliness, and Suicidal Behaviour in Slovenia. Medicina. 2024; 60(2):312. https://doi.org/10.3390/medicina60020312
Chicago/Turabian StylePoštuvan, Vita, Nina Krohne, Meta Lavrič, Vanja Gomboc, Diego De Leo, and Lucia Rojs. 2024. "A Lonelier World after COVID-19: Longitudinal Population-Based Study of Well-Being, Emotional and Social Loneliness, and Suicidal Behaviour in Slovenia" Medicina 60, no. 2: 312. https://doi.org/10.3390/medicina60020312
APA StylePoštuvan, V., Krohne, N., Lavrič, M., Gomboc, V., De Leo, D., & Rojs, L. (2024). A Lonelier World after COVID-19: Longitudinal Population-Based Study of Well-Being, Emotional and Social Loneliness, and Suicidal Behaviour in Slovenia. Medicina, 60(2), 312. https://doi.org/10.3390/medicina60020312







