High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair
Abstract
:1. Introduction
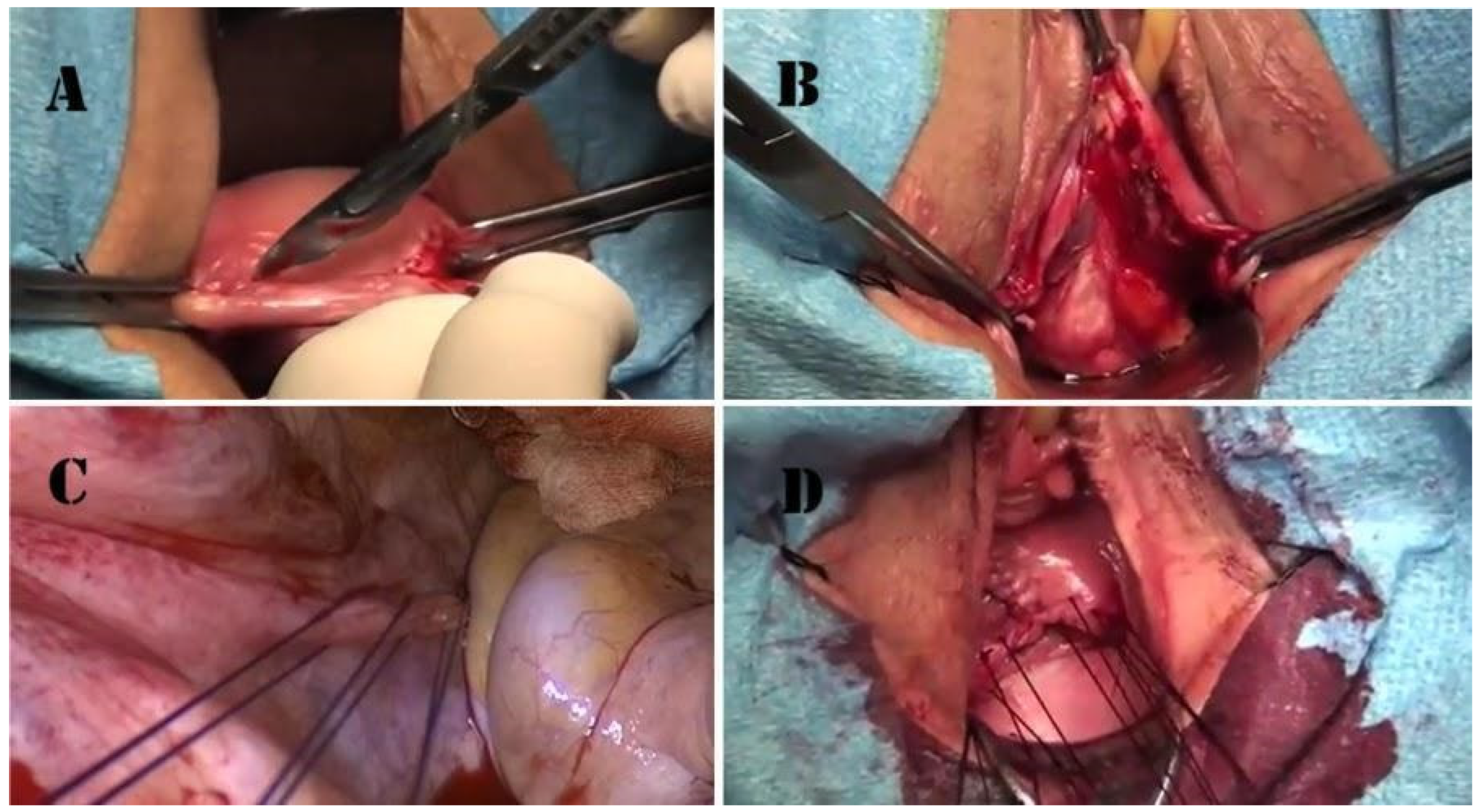
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Altman, D.; Falconer, C.; Cnattingius, S.; Granath, F. Pelvic organ prolapse surgery following hysterectomy on benign indications. Am. J. Obstet. Gynecol. 2008, 198, 572.e1–572.e6. [Google Scholar] [CrossRef]
- Slieker-ten Hove, M.C.; Pool-Goudzwaard, A.L.; Eijkemans, M.J.; Steegers-Theunissen, R.P.; Burger, C.W.; Vierhout, M.E. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2009, 20, 1037–1045. [Google Scholar] [CrossRef]
- Brunes, M.; Ek, M.; Drca, A.; Söderberg, M.; Bergman, I.; Warnqvist, A.; Johannesson, U. Vaginal vault prolapse and recurrent surgery: A nationwide observational cohort study. Acta Obstet. Gynecol. Scand. 2022, 101, 542–549. [Google Scholar] [CrossRef]
- Deo, G.; Bernasconi, D.P.; Cola, A.; Palmieri, S.; Spelzini, F.; Milani, R.; Manodoro, S.; Frigerio, M. Long-term outcomes and five-year recurrence-free survival curves after native-tissue prolapse repair. Int. J. Gynaecol. Obstet. 2019, 147, 238–245. [Google Scholar] [CrossRef]
- Manodoro, S.; Frigerio, M.; Cola, A.; Spelzini, F.; Milani, R. Risk factors for recurrence after hysterectomy plus native-tissue repair as primary treatment for genital prolapse. Int. Urogynecol. J. 2018, 29, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Manodoro, S.; Spelzini, F.; Cesana, M.C.; Frigerio, M.; Maggioni, D.; Ceresa, C.; Penati, C.; Sicuri, M.; Fruscio, R.; Nicolini, G.; et al. Histologic and metabolic assessment in a cohort of patients with genital prolapse: Preoperative stage and recurrence investigations. Minerva Ginecol. 2017, 69, 233–238. [Google Scholar] [CrossRef]
- Robinson, D.; Thiagamoorthy, G.; Cardozo, L. Post-hysterectomy vaginal vault prolapse. Maturitas 2018, 107, 39–43. [Google Scholar] [CrossRef]
- Vermeulen, C.K.M.; Veen, J.; Adang, C.; van Leijsen, S.A.L.; Coolen, A.L.W.M.; Bongers, M.Y. Pelvic organ prolapse after laparoscopic hysterectomy compared with vaginal hysterectomy: The POP-UP study. Int. Urogynecol. J. 2021, 32, 841–850. [Google Scholar] [CrossRef]
- Swift, S. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am. J. Obstet. Gynecol. 2000, 183, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Mant, J.; Painter, R.; Vessey, M. Epidemiology of genital prolapse: Observations from the Oxford family planning association study. BJOG 1997, 104, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Marchianni, M.; Bracco, G.L.; Checcucci, V.; Carabaneanu, A.; Coccia, E.M.; Mecacci, F.; Scarselli, G. True incidence of vaginal vault prolapse: Thirteen years of experience. J. Reprod. Med. 1999, 44, 678–684. [Google Scholar]
- Coolen, A.W.M.; van IJsselmuiden, M.N.; van Oudheusden, A.M.J.; Veen, J.; van Eijndhoven, H.W.F.; Mol, B.W.J.; Roovers, J.P.; Bongers, M.Y. Laparoscopic sacrocolpopexy versus vaginal sacrospinous fixation for vaginal vault prolapse, a randomized controlled trial: SALTO-2 trial, study protocol. BMC Womens Health 2017, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Brubaker, L.; Maher, C.; Jacquetin, B.; Rajamaheswari, N.; von Theobald, P.; Norton, P. Surgery for pelvic organ prolapse. Female Pelvic Med. Reconstr. Surg. 2010, 16, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Nygaard, I.E.; McCreery, R.; Brubaker, L.; Connolly, A.; Cundiff, G.; Weber, A.M.; Zyczynski, H.; Pelvic Floor Disorders Network. Abdominal sacrocolpopexy: A comprehensive review. Obstet. Gynecol. 2004, 104, 805–823. [Google Scholar] [CrossRef] [PubMed]
- Hilger, W.S.; Poulson, M.; Norton, P.A. Long-term results of abdominal sacrocolpopexy. Am. J. Obstet. Gynecol. 2003, 189, 1606–1610. [Google Scholar] [CrossRef] [PubMed]
- Price, N.; Jackson, S.R. Advances in laparoscopic techniques in pelvic reconstructive surgery for prolapse and incontinence. Maturitas 2009, 62, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Paraiso, M.F.; Falcone, T.; Walters, M.D. Laparoscopic surgery for enterocele, vaginal apex prolapse and rectocele. Int. Urogynecol. J. Pelvic Floor Dysfunct 1999, 10, 223–229. [Google Scholar] [CrossRef]
- Geller, E.J.; Parnell, B.A.; Dunivan, G.C. Pelvic floor function before and after robotic sacrocolpopexy: One year outcomes. J. Minim. Gynecol. 2011, 18, 322–327. [Google Scholar] [CrossRef]
- Wattiez, A.; Mashiach, R.; Donoso, M. Laparoscopic repair of vaginal vault prolapse. Curr. Opin. Obstet. Gynecol. 2003, 15, 315–319. [Google Scholar] [CrossRef]
- Klauschie, J.L.; Cornella, J.L. Surgical treatment of vaginal vault prolapse: A historic summary and review of outcomes. Female Pelvic Med. Reconstr. Surg. 2012, 18, 10–17. [Google Scholar] [CrossRef]
- Collins, S.; Lewicky-Gaupp, C. Pelvic Organ Prolapse. Gastroenterol. Clin. N. Am. 2022, 51, 177–193. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Feiner, B.; Baessler, K.; Christmann-Schmid, C.; Haya, N.; Marjoribanks, J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst. Rev. 2016, 2, CD012079. [Google Scholar] [CrossRef] [PubMed]
- Cola, A.P.; Marino, G.; Milani, R.; Barba, M.; Volontè, S.; Spelzini, F.; Manodoro, S.; Frigerio, M. Native-tissue prolapse repair: Efficacy and adverse effects of uterosacral ligaments suspension at 10-year follow up. Int. J. Gynecol. Obstet. 2022, 159, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Schimpf, M.O.; Abed, H.; Sanses, T.; White, A.B.; Lowenstein, L.; Ward, R.M.; Sung, V.W.; Balk, E.M.; Murphy, M.; Society of Gynecologic Surgeons Systematic Review Group. Graft and Mesh Use in Transvaginal Prolapse Repair: A Systematic Review. Obstet. Gynecol. 2016, 128, 81–91. [Google Scholar] [CrossRef]
- Sederl, J. Zur Operation des Prolapses der blind endigenden Schiede [Surgery in prolapse of a blind-end vagina]. Geburtshilfe Frauenheilkd. 1958, 18, 824–828. (In German) [Google Scholar]
- Yazdany, T.; Wong, K.; Bhatia, N.N. Sacrospinous ligament fixation for pelvic organ prolapse in the era of vaginal mesh kits. Curr. Opin. Obstet. Gynecol. 2011, 23, 391–395. [Google Scholar] [CrossRef]
- Milani, R.; Frigerio, M.; Manodoro, S. Transvaginal sacrospinous ligament fixation for posthysterectomy vaginal vault prolapse repair. Int. Urogynecol. J. 2017, 28, 1103–1105. [Google Scholar] [CrossRef]
- Leron, E.; Erez, O.; Shwarzmam, P.; Baessler, K. Sacrospinous ligament fixation (SSLF): An old method with new horizons. Arch. Gynecol. Obstet. 2022, 305, 1379–1382. [Google Scholar] [CrossRef]
- Smilen, S.W.; Saini, J.; Wallach, S.J.; Porges, R.F. The risk of cystocele after sacrospinous ligament fixation. Am. J. Obstet. Gynecol. 1998, 179 Pt 1, 1465–1472. [Google Scholar] [CrossRef]
- Holley, R.L.; Varner, R.E.; Gleason, B.P.; Apffel, L.A.; Scott, S. Recurrent pelvic support defects after sacrospinous ligament fixation for vaginal vault prolapse. J. Am. Coll. Surg. 1995, 180, 444–448. [Google Scholar]
- Inmon, W.B. Pelvic relaxation and repair including prolapse of vagina following hysterectomy. South Med. J. 1963, 56, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Shull, B.L.; Capen, C.V.; Riggs, M.W.; Kuehl, T.J. Bilateral attachment of the vaginal cuff to iliococcygeus fascia: An effective method of cuff suspension. Am. J. Obstet. Gynecol. 1993, 168 Pt 1, 1669–1677. [Google Scholar] [CrossRef] [PubMed]
- Milani, R.; Frigerio, M.; Spelzini, F.; Manodoro, S. Transvaginal iliococcygeus fixation for posthysterectomy vaginal vault prolapse repair. Int. Urogynecol. J. 2017, 28, 1599–1601. [Google Scholar] [CrossRef] [PubMed]
- Milani, R.; Frigerio, M.; Vellucci, F.L.; Palmieri, S.; Spelzini, F.; Manodoro, S. Transvaginal native-tissue repair of vaginal vault prolapse. Minerva Ginecol. 2018, 70, 371–377. [Google Scholar] [CrossRef]
- Webb, M.J.; Aronson, M.P.; Ferguson, L.K.; Lee, R.A. Posthysterectomy vaginal vault prolapse: Primary repair in 693 patients. Obstet. Gynecol. 1998, 92, 281–285. [Google Scholar] [CrossRef]
- Sze, E.H.; Karram, M.M. Transvaginal repair of vault prolapse: A review. Obstet. Gynecol. 1997, 89, 466–475. [Google Scholar] [CrossRef]
- Francis, W.J.; Jeffcoate, T.N. Dyspareunia following vaginal operations. J. Obstet. Gynaecol. Br. Commonw. 1961, 68, 1–10. [Google Scholar] [CrossRef]
- Milani, R.; Manodoro, S.; Cola, A.; Palmieri, S.; Frigerio, M. Transvaginal levator myorrhaphy for posthysterectomy vaginal vault prolapse repair. Int. Urogynecol. J. 2018, 29, 913–915. [Google Scholar] [CrossRef]
- Natale, F.; La Penna, C.; Padoa, A.; Panei, M.; Cervigni, M. High levator myorrhaphy for transvaginal suspension of the vaginal apex: Long-term results. J. Urol. 2008, 180, 2047–2052, discussion 2052. [Google Scholar] [CrossRef]
- Milani, R.; Manodoro, S.; Cola, A.; Bellante, N.; Palmieri, S.; Frigerio, M. Transvaginal uterosacral ligament hysteropexy versus hysterectomy plus uterosacral ligament suspension: A matched cohort study. Int. Urogynecol. J. 2020, 31, 1867–1872. [Google Scholar] [CrossRef]
- Milani, R.; Frigerio, M.; Spelzini, F.; Manodoro, S. Transvaginal uterosacral ligament hysteropexy: A video tutorial. Int. Urogynecol. J. 2017, 28, 789–791. [Google Scholar] [CrossRef]
- Milani, R.; Manodoro, S.; Cola, A.; Palmieri, S.; Reato, C.; Frigerio, M. Transvaginal native-tissue repair of enterocele. Int. Urogynecol. J. 2018, 29, 1705–1707. [Google Scholar] [CrossRef]
- Spelzini, F.; Frigerio, M.; Manodoro, S.; Interdonato, M.L.; Cesana, M.C.; Verri, D.; Fumagalli, C.; Sicuri, M.; Nicoli, E.; Polizzi, S.; et al. Modified McCall culdoplasty versus Shull suspension in pelvic prolapse primary repair: A retrospective study. Int. Urogynecol. J. 2017, 28, 65–71. [Google Scholar] [CrossRef]
- Bump, R.C.; Mattiasson, A.; Bø KBrubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef]
- Shull, B.L.; Bachofen, C.; Coates, K.W.; Kuehl, T.J. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am. J. Obstet. Gynecol. 2000, 183, 1365–1373; discussion 1373–1374. [Google Scholar] [CrossRef]
- Cola, A.; Barba, M.; Frigerio, M. Intraoperative ultrasound assessment of ureteral patency during pelvic surgery. Int. Urogynecol. J. 2021, 32, 3313–3315. [Google Scholar] [CrossRef]
- Frigerio, M.; Barba, M.; Marino, G.; Volontè, S.; Cola, A. Intraoperative ultrasound assessment of ureteral patency after uterosacral ligaments apical suspension for prolapse surgical repair: A feasibility study. Int. J. Gynaecol. Obstet. 2023, 163, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Yalcin, I.; Bump, R.C. Validation of two global impression questionnaires for incontinence. Am. J. Obstet. Gynecol. 2003, 189, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Srikrishna, S.; Robinson, D.; Cardozo, L. Validation of the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse. Int. Urogynecol. J. 2010, 21, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Campbell, P.; Cloney, L.; Jha, S. Abdominal Versus Laparoscopic Sacrocolpopexy. Obstet. Gynecol. Surv. 2016, 71, 435–442. [Google Scholar] [CrossRef]
- Zhang, W.; Cheon, W.C.; Zhang, L.; Wang, X.; Wei, Y.; Lyu, C. Comparison of the effectiveness of sacrospinous ligament fixation and sacrocolpopexy: A meta-analysis. Int. Urogynecol. J. 2022, 33, 3–13. [Google Scholar] [CrossRef]

| Age (Years) | 64.8 ± 9.6 |
|---|---|
| Parity (n) | 2.0 ± 0.8 |
| Menopausal status | 45 (95.7%) |
| BMI (Kg/m2) | 27.0 ± 6.1 |
| ASA status 1 | 4 (8.5%) |
| ASA status 2 | 35 (74.5%) |
| ASA status 3 | 8 (17.0%) |
| Indication for previous hysterectomy | 27 (57.4%) Uterovaginal prolapse |
| 20 (42.6%) Other benign indications |
| High Uterosacral Ligaments Suspension | 47 (100%) |
|---|---|
| Anterior repair | 33 (70.2%) |
| Posterior repair | 28 (59.6%) |
| Blood loss (mL) | 184 ± 126 |
| Operative time (min) | 82 ± 26 |
| Intraoperative complications | 0 |
| Postoperative complications | 1 (2.1%) * |
| Anatomic Recurrence | 8 (24.2%) |
|---|---|
| 7 (21.2%) |
| 2 (6.0%) |
| 1 (3.0%) |
| Reoperation | 0 (0%) |
| Postoperative bulging symptoms | 4 (12.1%) |
| PGI-I | 1.6 ± 0.8 |
| Preoperative | Postoperative | p-Value | |
|---|---|---|---|
| Aa | 1.1 ± 1.7 | −1.8 ± 1.2 | <0.001 |
| Ba | 1.3 ± 1.9 | −1.8 ± 1.2 | <0.001 |
| C | 1.2 ± 2.7 | −5.3 ± 2.7 | <0.001 |
| gh | 4.1 ± 0.7 | 3.6 ± 0.6 | <0.001 |
| pb | 2.8 ± 0.5 | 3.1 ± 0.5 | 0.01 |
| tvl | 8.6 ± 1.0 | 8.1 ± 1.2 | 0.004 |
| Ap | −1.7 ± 1.4 | −2.7 ± 0.6 | <0.001 |
| Bp | −1.5 ± 1.6 | −2.7 ± 0.6 | <0.001 |
| Preoperative | Postoperative | p-Value | |
|---|---|---|---|
| Stress urinary incontinence | 16 (34.0%) | 6 (18.2%) | 0.135 |
| Voiding symptoms | 29 (61.7%) | 6 (18.2%) | <0.001 |
| Overactive bladder syndrome | 18 (38.3%) | 10 (30.3%) | 0.486 |
| Constipation | 13 (27.7%) | 11 (33.3%) | 0.626 |
| Bulging symptoms | 47 (100%) | 4 (12.1%) | <0.001 |
| Sexual activity | 15 (31.9%) | 10 (30.3%) | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barba, M.; Cola, A.; Melocchi, T.; De Vicari, D.; Costa, C.; Volontè, S.; Sandullo, L.; Frigerio, M. High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair. Medicina 2024, 60, 320. https://doi.org/10.3390/medicina60020320
Barba M, Cola A, Melocchi T, De Vicari D, Costa C, Volontè S, Sandullo L, Frigerio M. High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair. Medicina. 2024; 60(2):320. https://doi.org/10.3390/medicina60020320
Chicago/Turabian StyleBarba, Marta, Alice Cola, Tomaso Melocchi, Desirèe De Vicari, Clarissa Costa, Silvia Volontè, Lucia Sandullo, and Matteo Frigerio. 2024. "High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair" Medicina 60, no. 2: 320. https://doi.org/10.3390/medicina60020320
APA StyleBarba, M., Cola, A., Melocchi, T., De Vicari, D., Costa, C., Volontè, S., Sandullo, L., & Frigerio, M. (2024). High Uterosacral Ligaments Suspension for Post-Hysterectomy Vaginal Vault Prolapse Repair. Medicina, 60(2), 320. https://doi.org/10.3390/medicina60020320







