Symptomatic Calcifications after Mastectomy: A Rare Case Report with a Review of the Literature
Abstract
1. Introduction
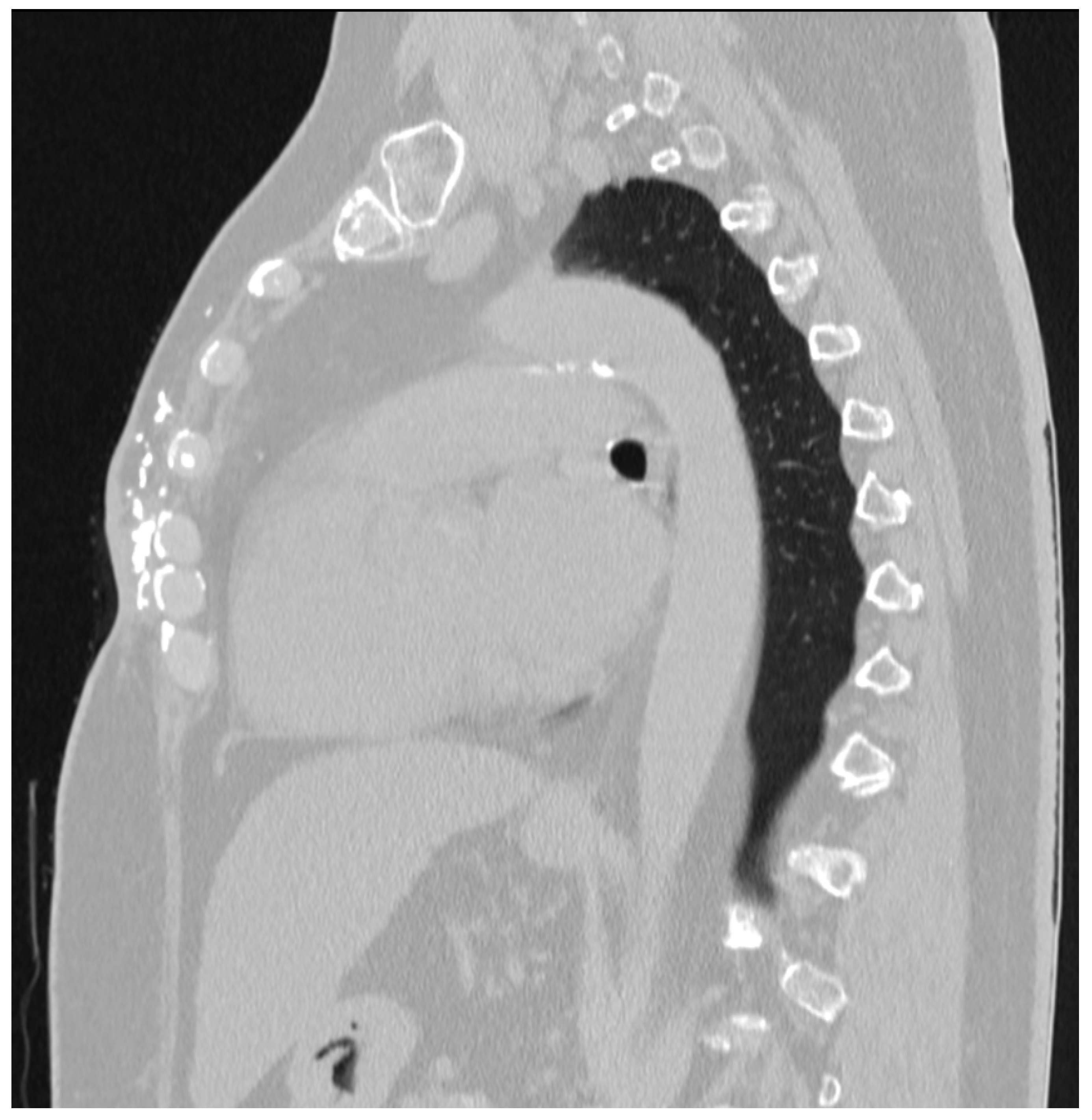
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gabani, P.; Gill, B.; de la Cruz, C.; Beriwal, S. Diffuse Chest Wall Calcifications after Post Mastectomy Radiotherapy for Breast Cancer. Appl. Radiat. Oncol. 2014, 3, 22–24. [Google Scholar] [CrossRef]
- Hermann, R.M.; Clausing, B.; Mayer, J.; Carl, U.M.; Nitsche, M. Late Radiation Sequelae as a Consequence of Breast-Conserving Therapy with Cobalt Irradiation Aggravated by Various Risk Factors. BJR Case Rep. 2015, 1, 20150026. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Ahn, S.H.; Son, B.H.; Kim, E.K. Using local flaps in a chest wall reconstruction after mastectomy for locally advanced breast cancer. Arch. Plast Surg. 2015, 42, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Pires, D.; Souza, G.; Pace, B. Use of thoracoepigastric flap in large breast resections: Phyllodes tumor case report. Mastology 2018, 23, 231–235. [Google Scholar] [CrossRef]
- Fosh, B.G.; Asokan, G.; Hainsworth, A.; Gilhotra, A.; Hoffmann, C. Radiation-Induced Necrosis and Calcinosis of the Breast: A Case Report. ANZ J. Surg. 2014, 84, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Amin, R.; Hamilton-Wood, C.; Silver, D. Subcutaneous Calcification Following Chest Wall and Breast Irradiation: A Late Complication. Br. J. Radiol. 2002, 75, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Carl, U.M.; Hartmann, K.A. Heterotopic Calcification as a Late Radiation Effect: Report of 15 Cases. Br. J. Radiol. 2002, 75, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Perna, D.; Margheim, A.; Schadt, C.R. Radiation-Induced Morphea and Dystrophic Calcinosis Cutis of the Breast. Int. J. Dermatol. 2021, 60, e373–e375. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-W.; Oh, S.-H.; Chang, S.-E.; Lee, M.-W.; Choi, J.-H.; Moon, K.-C.; Koh, J.-K. Dystrophic Calcinosis Cutis Following Chest Wall and Breast Irradiation. J. Dermatol. 2005, 32, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Lim, P.N.; Tilston, S. Right Breast Ulceration and Dystrophic Calcification as a Late Sequela Following Postmastectomy Radiotherapy. BMJ Case Rep. 2023, 16, e254086. [Google Scholar] [CrossRef] [PubMed]
- Banys-Paluchowski, M.; Brus, L.; Krawczyk, N.; Kopperschmidt, S.V.; Gasparri, M.L.; Bündgen, N.; Rody, A.; Hanker, L.; Hemptenmacher, F.; Paluchowski, P. Latissimus dorsi flap for breast reconstruction: A large single-institution evaluation of surgical outcome and complications. Arch. Gynecol. Obstet. 2024, 309, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Matros, E.; Disa, J.J. Uncommon flaps for chest wall reconstruction. Semin. Plast. Surg. 2011, 25, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Senkus-Konefka, E.; Jassem, J. Complications of Breast-Cancer Radiotherapy. Clin. Oncol. 2006, 18, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Mergancová, J.; Lierová, A.; Coufal, O.; Žatecký, J.; Melichar, B.; Zedníková, I.; Mergancová, J.; Jesenková, A.; Šťastný, K.; Gatěk, J.; et al. Radiation-Associated Angiosarcoma of the Breast: An International Multicenter Analysis. Surg. Oncol. 2022, 41, 101726. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; Kim, Y.B. Journey to Hypofractionation in Radiotherapy for Breast Cancer: Critical Reviews for Recent Updates. Radiat. Oncol. J. 2022, 40, 216–224. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Breast Cancer (Version 5.2023). Available online: https://www.nccn.org/professionals/physician_gls/pdf/breast_blocks.pdf (accessed on 12 January 2024).
- Herrick, B.; Bishop-Jodoin, M.; Elaimy, A.; Shanmugham, L.; Glanzman, J.; Sioshansi, S.; Goff, D.; Sacher, A.; Moni, J.; Cicchetti, M.; et al. Breast Calcification Relative to Radiation Dose Distribution 21 Years after Radiation Therapy: A Case Report and an Argument Against Hypofractionation of Breast Patients. Front. Med. Case Rep. 2020, 1, 1-08. [Google Scholar] [CrossRef]




| Author | Year | Type of Article | Number of Cases | Treatment of BC | RT Scheme (Gy/Fractions) | Time from RT to Clinical Manifestation (Years) | Treatment |
|---|---|---|---|---|---|---|---|
| Fosh et al. [5] | 2013 | case report | 1 | BCS, RT | 50/25 + boost 10/5 | 13 | mastectomy |
| Amin et al. [6] | 2002 | case report | 1 | Mastectomy, RT | 45/20 | N/A | N/A |
| Carl et al. [7] | 2002 | short communication | 7 | N/A, RT | 40/- | 19 | N/A |
| N/A, RT | 77/- | 11 | N/A | ||||
| N/A, RT | 40/- | 24 | N/A | ||||
| N/A, RT | 40/- | 7 | N/A | ||||
| N/A, RT | 50/- | 6 | N/A | ||||
| N/A, RT | 50/- + boost 10/- | 2 | N/A | ||||
| N/A, RT | 30/- + boost 15/- | 16 | N/A | ||||
| Hermann et al. [2] | 2015 | case report | 1 | BCS, RT | 48.6/- + boost 10.8/- | 20 | antibiotics, debridement, VAC system, latissimus dorsi flap |
| Perna et al. [8] | 2021 | correspondence | 1 | BCS, RT | -/- | 17 | surgical excision |
| Lee et al. [9] | 2005 | case report | 1 | Mastectomy, CHT, RT | 50/20 | 26 | patient refused recommended surgery |
| Lim et al. [10] | 2023 | case report | 1 | Mastectomy, RT | 61/28 | 30 | conservative |
| Gabani et al. [1] | 2014 | case report | 1 | Mastectomy, RT | 60/30 | 13 | wide resection with reconstruction |
| 14 cases | Average dose (without boost) = 49.4 Gy | Median time of clinical manifestation = 16 years | |||||
| Average dose (with boost) = 52.9 Gy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Žatecký, J.; Coufal, O.; Sekret, D.; Peteja, M. Symptomatic Calcifications after Mastectomy: A Rare Case Report with a Review of the Literature. Medicina 2024, 60, 399. https://doi.org/10.3390/medicina60030399
Žatecký J, Coufal O, Sekret D, Peteja M. Symptomatic Calcifications after Mastectomy: A Rare Case Report with a Review of the Literature. Medicina. 2024; 60(3):399. https://doi.org/10.3390/medicina60030399
Chicago/Turabian StyleŽatecký, Jan, Oldřich Coufal, Dobroslav Sekret, and Matúš Peteja. 2024. "Symptomatic Calcifications after Mastectomy: A Rare Case Report with a Review of the Literature" Medicina 60, no. 3: 399. https://doi.org/10.3390/medicina60030399
APA StyleŽatecký, J., Coufal, O., Sekret, D., & Peteja, M. (2024). Symptomatic Calcifications after Mastectomy: A Rare Case Report with a Review of the Literature. Medicina, 60(3), 399. https://doi.org/10.3390/medicina60030399






