Effect of Remimazolam- versus Propofol-Based Total Intravenous General Anesthesia on Intraoperative Hemodynamic Stability for Major Spine Surgery in the Prone Position: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
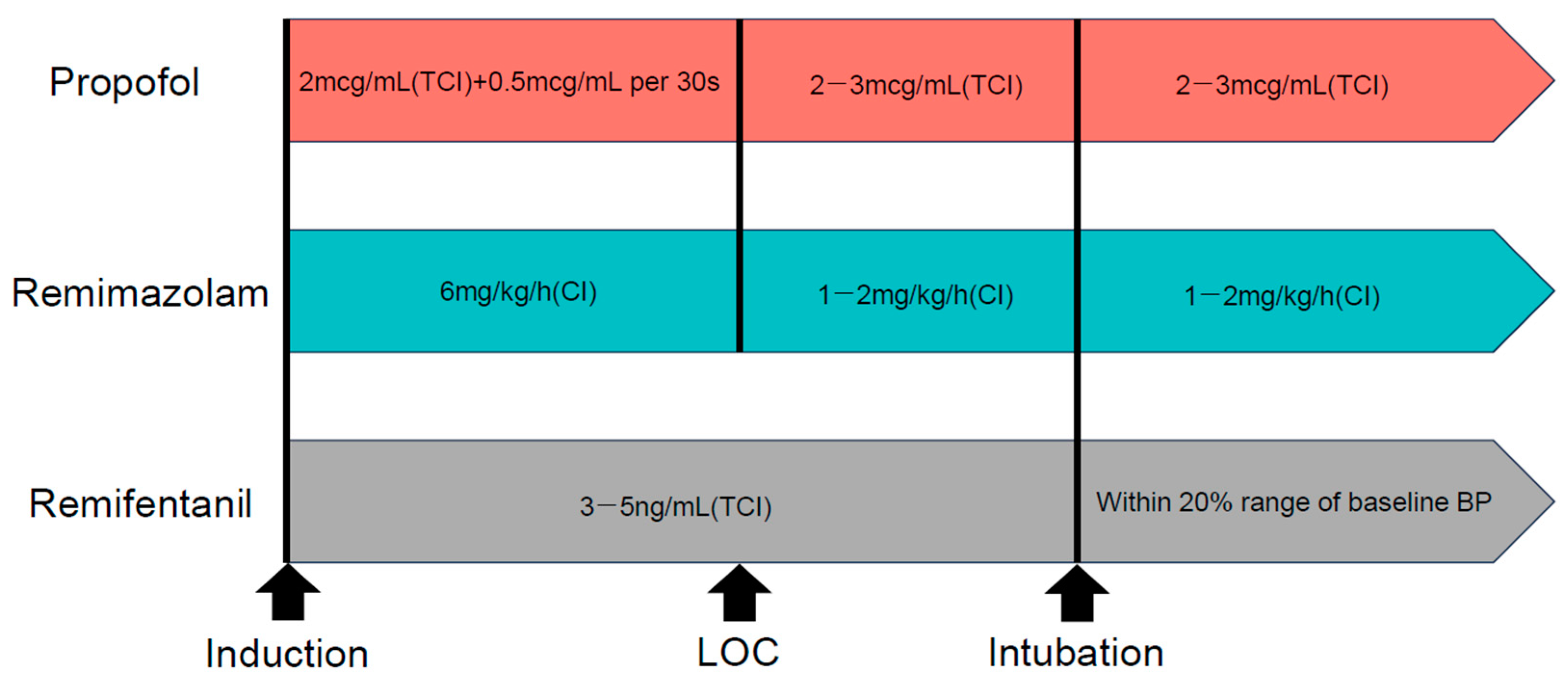
2.2. Anesthesia
2.3. Definition of Hemodynamic Events and Management
2.4. Outcome Measures
2.5. Statistical Analysis
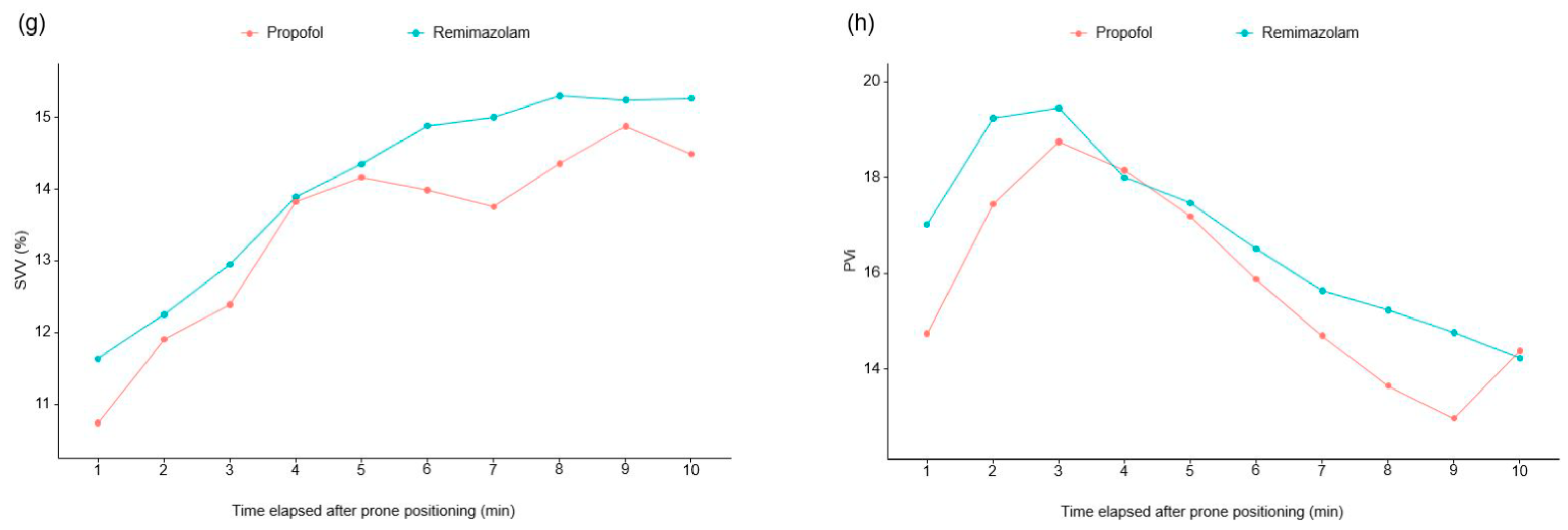
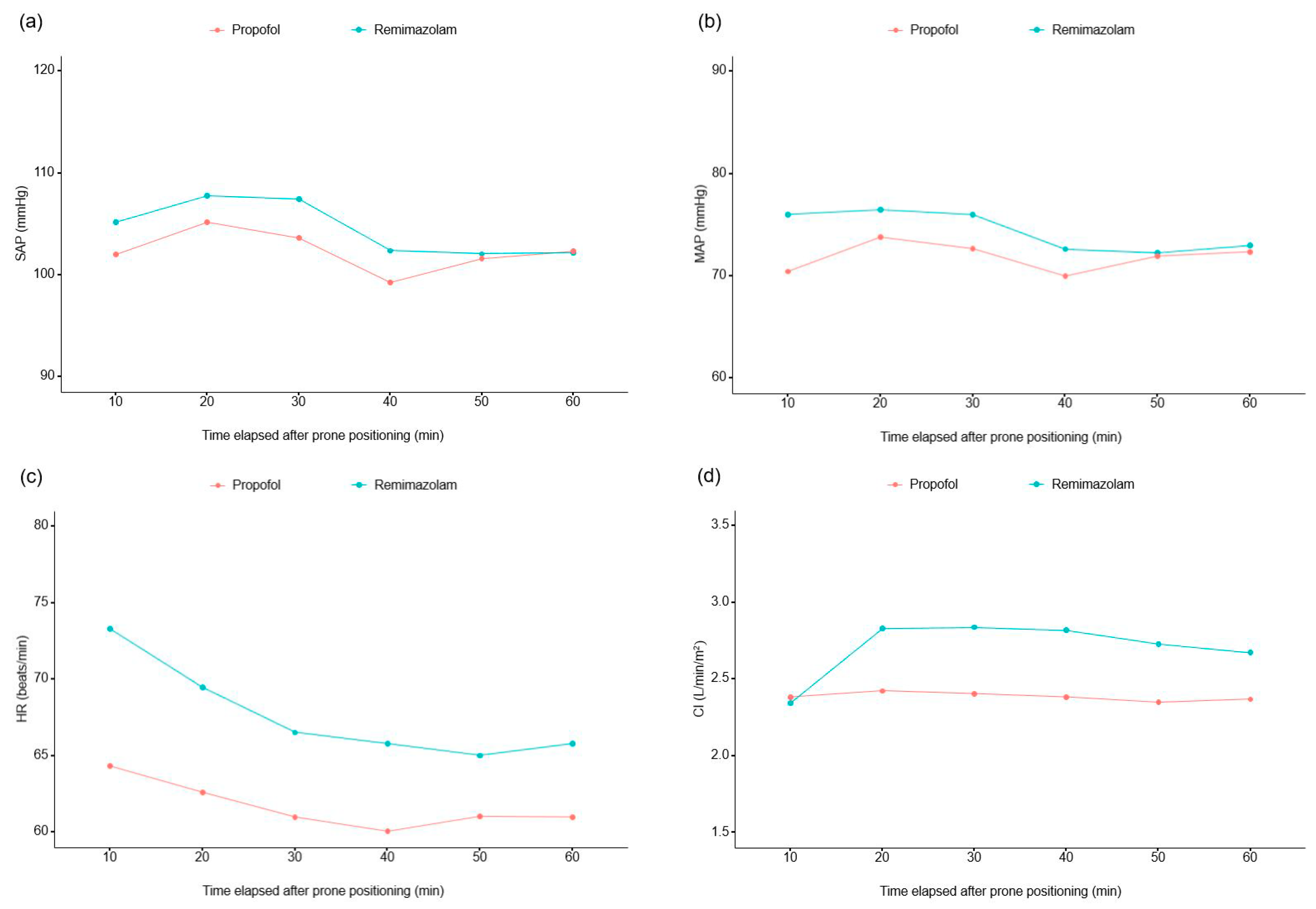
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bijker, J.B.; van Klei, W.A.; Vergouwe, Y.; Eleveld, D.J.; van Wolfswinkel, L.; Moons, K.G.; Kalkman, C.J. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology 2009, 111, 1217–1226. [Google Scholar] [CrossRef]
- Roshanov, P.S.; Sheth, T.; Duceppe, E.; Tandon, V.; Bessissow, A.; Chan, M.T.V.; Butler, C.; Chow, B.J.W.; Khan, J.S.; Devereaux, P.J. Relationship between Perioperative Hypotension and Perioperative Cardiovascular Events in Patients with Coronary Artery Disease Undergoing Major Noncardiac Surgery. Anesthesiology 2019, 130, 756–766. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Devereaux, P.J.; Garg, A.X.; Kurz, A.; Turan, A.; Rodseth, R.N.; Cywinski, J.; Thabane, L.; Sessler, D.I. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: Toward an empirical definition of hypotension. Anesthesiology 2013, 119, 507–515. [Google Scholar] [CrossRef]
- Wesselink, E.M.; Kappen, T.H.; Torn, H.M.; Slooter, A.J.C.; van Klei, W.A. Intraoperative hypotension and the risk of postoperative adverse outcomes: A systematic review. Br. J. Anaesth. 2018, 121, 706–721. [Google Scholar] [CrossRef] [PubMed]
- Edgcombe, H.; Carter, K.; Yarrow, S. Anaesthesia in the prone position. Br. J. Anaesth. 2008, 100, 165–183. [Google Scholar] [CrossRef] [PubMed]
- Wilent, W.B.; Tesdahl, E.A.; Trott, J.T.; Tassone, S.; Harrop, J.S.; Klineberg, E.O.; Sestokas, A.K. Impact of inhalational anesthetic agents on the baseline monitorability of motor evoked potentials during spine surgery: A review of 22,755 cervical and lumbar procedures. Spine J. 2021, 21, 1839–1846. [Google Scholar] [CrossRef]
- Clapcich, A.J.; Emerson, R.G.; Roye, D.P.; Xie, H., Jr.; Gallo, E.J.; Dowling, K.C.; Ramnath, B.; Heyer, E.J. The effects of propofol, small-dose isoflurane, and nitrous oxide on cortical somatosensory evoked potential and bispectral index monitoring in adolescents undergoing spinal fusion. Anesth. Analg. 2004, 99, 1334–1340. [Google Scholar] [CrossRef]
- Monk, C.R.; Coates, D.P.; Prys-Roberts, C.; Turtle, M.J.; Spelina, K. Haemodynamic effects of a prolonged infusion of propofol as a supplement to nitrous oxide anaesthesia: Studies in association with peripheral arterial surgery. Br. J. Anaesth. 1987, 59, 954–960. [Google Scholar] [CrossRef]
- Kilpatrick, G.J.; McIntyre, M.S.; Cox, R.F.; Stafford, J.A.; Pacofsky, G.J.; Lovell, G.G.; Wiard, R.P.; Feldman, P.L.; Collins, H.; Waszczak, B.L.; et al. CNS 7056: A novel ultra-short-acting Benzodiazepine. Anesthesiology 2007, 107, 60–66. [Google Scholar] [CrossRef]
- Kim, K.M. Remimazolam: Pharmacological characteristics and clinical applications in anesthesiology. Anesth. Pain Med. 2022, 17, 1–11. [Google Scholar] [CrossRef]
- Yamada, S.; Akiyama, Y.; Tachibana, S.; Hayamizu, K.; Kimura, Y.; Hashimoto, S.; Yamakage, M.; Mikuni, N. The intraoperative motor-evoked potential when propofol was changed to remimazolam during general anesthesia: A case series. J. Anesth. 2023, 37, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Takasusuki, T.; Yamaguchi, S. Remimazolam Compared to Propofol for Total Intravenous Anesthesia with Remifentanil on the Recovery of Psychomotor Function: A Randomized Controlled Trial. Adv. Ther. 2023, 40, 4395–4404. [Google Scholar] [CrossRef] [PubMed]
- Fechner, J.; El-Boghdadly, K.; Spahn, D.R.; Motsch, J.; Struys, M.; Duranteau, O.; Ganter, M.T.; Richter, T.; Hollmann, M.W.; Rossaint, R.; et al. Anaesthetic efficacy and postinduction hypotension with remimazolam compared with propofol: A multicentre randomised controlled trial. Anaesthesia 2024. [Google Scholar] [CrossRef]
- Huang, Y.; Yan, T.; Lu, G.; Luo, H.; Lai, Z.; Zhang, L. Efficacy and safety of remimazolam compared with propofol in hypertensive patients undergoing breast cancer surgery: A single-center, randomized, controlled study. BMC Anesthesiol. 2023, 23, 409. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Gong, C.; Chen, Y.; Chen, R.; Qian, Y. Effect of remimazolam vs. propofol on hemodynamics during general anesthesia induction in elderly patients: Single-center, randomized controlled trial. J. Biomed. Res. 2024, 38, 66–75. [Google Scholar] [CrossRef]
- Doi, M.; Morita, K.; Takeda, J.; Sakamoto, A.; Yamakage, M.; Suzuki, T. Efficacy and safety of remimazolam versus propofol for general anesthesia: A multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J. Anesth. 2020, 34, 543–553. [Google Scholar] [CrossRef]
- Qiu, Y.; Gu, W.; Zhao, M.; Zhang, Y.; Wu, J. The hemodynamic stability of remimazolam compared with propofol in patients undergoing endoscopic submucosal dissection: A randomized trial. Front. Med. 2022, 9, 938940. [Google Scholar] [CrossRef]
- Hasegawa, G.; Hirata, N.; Yoshikawa, Y.; Yamakage, M. Differential effects of remimazolam and propofol on heart rate variability during anesthesia induction. J. Anesth. 2022, 36, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Win, N.N.; Fukayama, H.; Kohase, H.; Umino, M. The different effects of intravenous propofol and midazolam sedation on hemodynamic and heart rate variability. Anesth. Analg. 2005, 101, 97–102. [Google Scholar] [CrossRef]
- de Wit, F.; van Vliet, A.L.; de Wilde, R.B.; Jansen, J.R.; Vuyk, J.; Aarts, L.P.; de Jonge, E.; Veelo, D.P.; Geerts, B.F. The effect of propofol on haemodynamics: Cardiac output, venous return, mean systemic filling pressure, and vascular resistances. Br. J. Anaesth. 2016, 116, 784–789. [Google Scholar] [CrossRef]
- Sekiguchi, R.; Kinoshita, M.; Kawanishi, R.; Kakuta, N.; Sakai, Y.; Tanaka, K. Comparison of hemodynamics during induction of general anesthesia with remimazolam and target-controlled propofol in middle-aged and elderly patients: A single-center, randomized, controlled trial. BMC Anesthesiol. 2023, 23, 14. [Google Scholar] [CrossRef]
- Kim, K.M.; Bang, J.Y.; Lee, J.M.; Yang, H.S.; Choi, B.M.; Noh, G.J. Effect-site concentration of remimazolam at loss and recovery of responsiveness during general anesthesia: A simulation study. Anesth. Pain Med. 2022, 17, 262–270. [Google Scholar] [CrossRef]
- Stasiowski, M.J.; Pluta, A.; Lyssek-Boroń, A.; Kawka, M.; Krawczyk, L.; Niewiadomska, E.; Dobrowolski, D.; Rejdak, R.; Król, S.; Żak, J.; et al. Preventive Analgesia, Hemodynamic Stability, and Pain in Vitreoretinal Surgery. Medicina 2021, 57, 262. [Google Scholar] [CrossRef]
- Stasiowski, M.J.; Zmarzły, N.; Grabarek, B.O.; Gąsiorek, J. Postoperative Nausea and Vomiting following Endoscopic Sinus Surgery under the Guidance of Adequacy of Anesthesia or Pupillometry with Intravenous Propofol/Remifentanil. Pharmaceuticals 2024, 17, 2. [Google Scholar] [CrossRef]
- Saugel, B.; Sessler, D.I. Perioperative Blood Pressure Management. Anesthesiology 2021, 134, 250–261. [Google Scholar] [CrossRef]
- Cohen, B.; Rivas, E.; Yang, D.; Mascha, E.J.; Ahuja, S.; Turan, A.; Sessler, D.I. Intraoperative Hypotension and Myocardial Injury After Noncardiac Surgery in Adults With or Without Chronic Hypertension: A Retrospective Cohort Analysis. Anesth. Analg. 2022, 135, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Futier, E.; Lefrant, J.Y.; Guinot, P.G.; Godet, T.; Lorne, E.; Cuvillon, P.; Bertran, S.; Leone, M.; Pastene, B.; Piriou, V.; et al. Effect of Individualized vs Standard Blood Pressure Management Strategies on Postoperative Organ Dysfunction Among High-Risk Patients Undergoing Major Surgery: A Randomized Clinical Trial. JAMA 2017, 318, 1346–1357. [Google Scholar] [CrossRef] [PubMed]
- Salmasi, V.; Maheshwari, K.; Yang, D.; Mascha, E.J.; Singh, A.; Sessler, D.I.; Kurz, A. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology 2017, 126, 47–65. [Google Scholar] [CrossRef]
- Maheshwari, K.; Turan, A.; Mao, G.; Yang, D.; Niazi, A.K.; Agarwal, D.; Sessler, D.I.; Kurz, A. The association of hypotension during non-cardiac surgery, before and after skin incision, with postoperative acute kidney injury: A retrospective cohort analysis. Anaesthesia 2018, 73, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Kwee, M.M.; Ho, Y.-H.; Rozen, W.M. The prone position during surgery and its complications: A systematic review and evidence-based guidelines. Int. Surg. 2015, 100, 292–303. [Google Scholar] [CrossRef]
- Chiang, T.Y.; Wang, Y.K.; Huang, W.C.; Huang, S.S.; Chu, Y.C. Intraoperative hypotension in non-emergency decompression surgery for cervical spondylosis: The role of chronic arterial hypertension. Front. Med. 2022, 9, 943596. [Google Scholar] [CrossRef] [PubMed]



| Propofol Group (n = 47) | Remimazolam Group (n = 47) | p-Value | |
|---|---|---|---|
| Demographic data | |||
| Sex (male) | 20 (42.6%) | 15 (31.9%) | 0.286 |
| ASA PS | |||
| 2 | 42 (89.4%) | 43 (91.5%) | |
| 3 | 5 (10.6%) | 4 (8.5%) | |
| Age (years) | 67.2 ± 7.5 | 67.4 ± 8.0 | 0.873 |
| Height (m) | 1.6 ± 0.1 | 1.6 ± 0.1 | 0.927 |
| Weight (kg) | 64.9 ± 9.2 | 61.1 ± 9.0 | 0.048 |
| Medical history | |||
| Diabetes mellitus | 7 (14.9%) | 16 (34.0%) | 0.031 |
| Hypertension | 27 (57.4%) | 23 (48.9%) | 0.408 |
| Ischemic heart disease | 4 (8.5%) | 2 (4.3%) | 0.677 |
| Cerebrovascular accident | 2 (4.3%) | 0 (0.0%) | 0.495 |
| Pulmonary disease | 4 (8.5%) | 4 (8.5%) | 1.000 |
| Renal disease | 1 (2.1%) | 4 (8.5%) | 0.361 |
| Preoperative laboratory data | |||
| Hemoglobin (g/dL) | 13.0 ± 1.4 | 12.7 ± 1.6 | 0.374 |
| White blood cell (103/µL) | 6.4 ± 1.5 | 6.3 ± 2.1 | 0.681 |
| Platelet (109/µL) | 235.6 ± 49.8 | 235.8 ± 53.8 | 0.986 |
| Albumin (g/dL) | 3.8 ± 0.3 | 4.5 ± 4.7 | 0.803 |
| Creatinine (mg/dL) | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.714 |
| Aspartate transaminase (IU/L) | 23.1 ± 7.1 | 23.1 ± 6.3 | 0.976 |
| Alanine transaminase (IU/L) | 21.8 ± 11.5 | 20.3 ± 8.0 | 0.462 |
| C-reactive protein (mg/dL) | 0.2 ± 0.6 | 0.3 ± 0.8 | 0.506 |
| Anesthesia and surgery-related data | |||
| Anesthetic time (min) * | −189 (170–210) | 186 (170–210) | 0.623 |
| Operative time (min) * | 137 (117–157) | 135 (115–159) | 0.877 |
| Total amount of remifentanil (mcg) * | 1600 (1300–1987) | 1562.5 (1226–2150) | 0.715 |
| Propofol Group (n = 47) | Remimazolam Group (n = 47) | p-Value | |
|---|---|---|---|
| Intraoperative adverse events | |||
| Patients with hypotensive event(s) | 45 (95.7%) | 39 (83.0%) | 0.091 |
| Hypotensive event per individual | 4.7 (2.4%) | 4.1 (2.7%) | 0.366 |
| Patients with severe hypotensive event(s) | 36 (76.6%) | 31 (66.0%) | 0.254 |
| Severe hypotensive event(s) per individual | 2.8 (2.3%) | 2.1 (2.1%) | 0.128 |
| Amount of administered inotropics or vasopressors | |||
| Total amount of ephedrine (mg) | 5 (0–10) | 0 (0–5) | 0.020 |
| Total amount of phenylephrine (mcg) | 1200 (0–2950) | 325 (0–1700) | 0.239 |
| Total amount of norepinephrine (mcg) | 0 (0–0) | 0 (0–0) | 0.164 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-J.; Kim, J.-Y.; Park, H.-S.; Kim, H.; Ro, Y.-J.; Koh, W.U. Effect of Remimazolam- versus Propofol-Based Total Intravenous General Anesthesia on Intraoperative Hemodynamic Stability for Major Spine Surgery in the Prone Position: A Randomized Controlled Trial. Medicina 2024, 60, 432. https://doi.org/10.3390/medicina60030432
Kim H-J, Kim J-Y, Park H-S, Kim H, Ro Y-J, Koh WU. Effect of Remimazolam- versus Propofol-Based Total Intravenous General Anesthesia on Intraoperative Hemodynamic Stability for Major Spine Surgery in the Prone Position: A Randomized Controlled Trial. Medicina. 2024; 60(3):432. https://doi.org/10.3390/medicina60030432
Chicago/Turabian StyleKim, Ha-Jung, Ji-Young Kim, Hyeok-Seong Park, Hyungtae Kim, Young-Jin Ro, and Won Uk Koh. 2024. "Effect of Remimazolam- versus Propofol-Based Total Intravenous General Anesthesia on Intraoperative Hemodynamic Stability for Major Spine Surgery in the Prone Position: A Randomized Controlled Trial" Medicina 60, no. 3: 432. https://doi.org/10.3390/medicina60030432





