Predictors of Burden for First-Ever Stroke Survivor’s Long-Term Caregivers: A Study of KOSCO
Abstract
1. Introduction
2. Materials and Methods
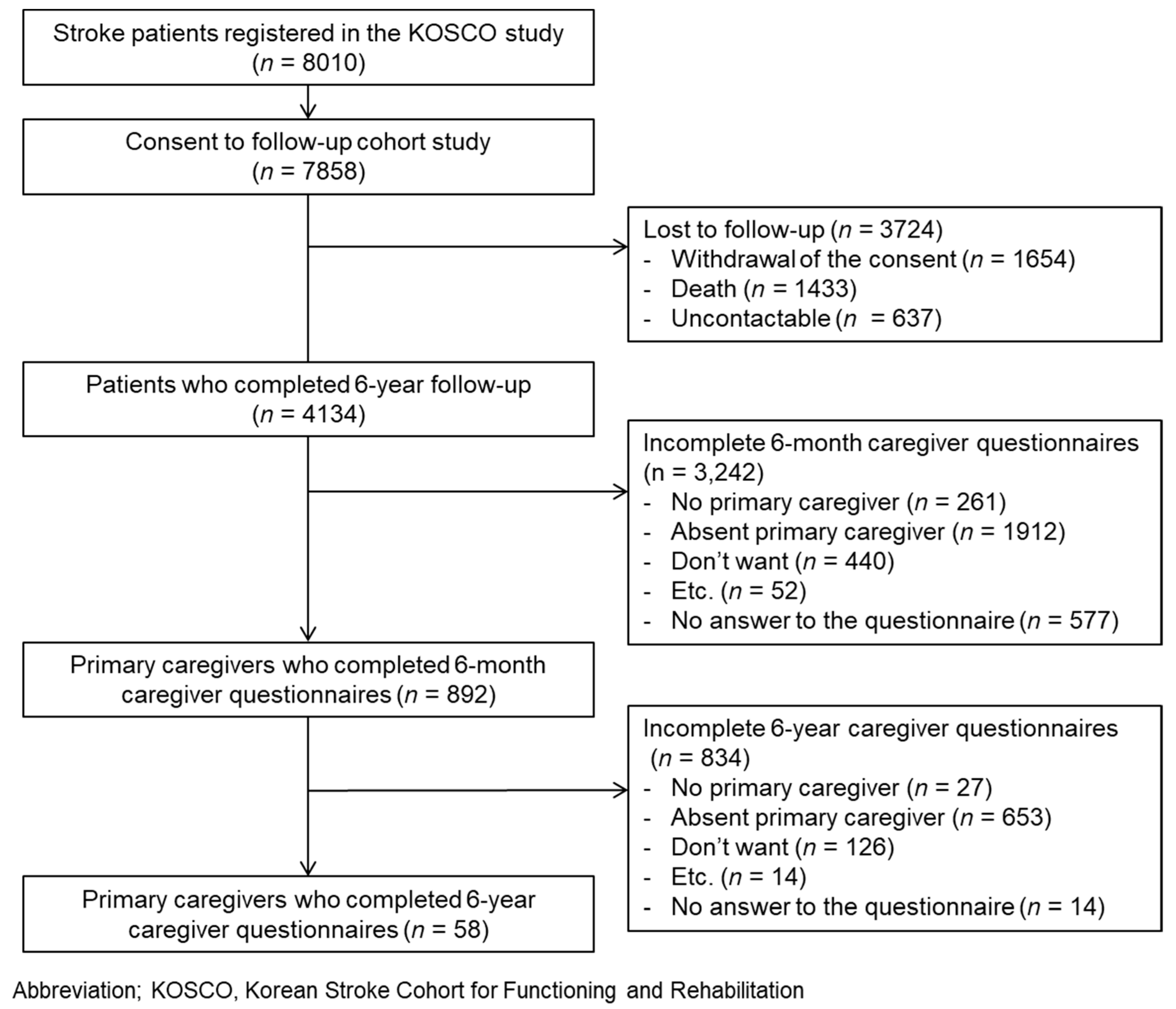
2.1. Study Design
2.2. Study Population and Procedures
2.3. Demographic Data and Measurement Tools
2.4. Factors Related to Caregiver Burden
- Dependent factors related to caregiver burden
- B.
- Independent factors related to caregiver burden
- Patient’s factors related to caregiver burden variables
- 2.
- Caregiver’s factors related to caregiver burden
2.5. Statistical Analysis
2.6. Data Availability
3. Results
3.1. Comparison of the Included and Excluded Groups
3.2. Patient and Caregiver Characteristics
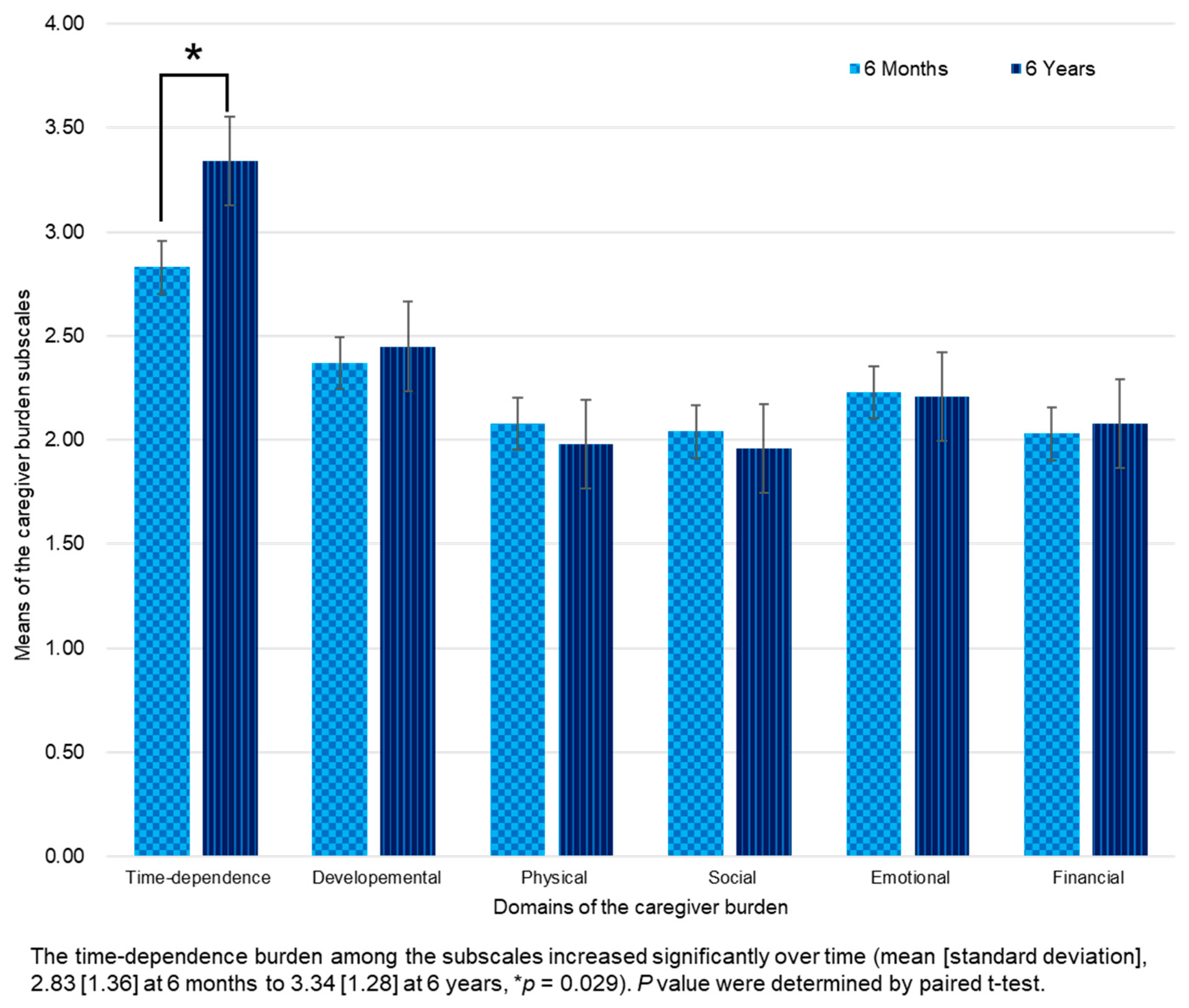
3.3. Caregiver Burden and Changes over Time
3.4. Associations and Predictors of High Caregiver Burden
4. Discussion
4.1. Predictors of Caregiver Burden
4.1.1. Patient’s Disability and Psychosocial Stress
4.1.2. Caregivers’ Burnout in Long-Term Care
4.2. Strategies to Reduce Caregiver Burden
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Stevens, E.; Emmet, E.; Wang, Y.; McKevitt, C.; Wolfe, C.D.A. The Burden of Stroke in Europe: The Challenge for Policy Makers; Stroke Alliance for Europe: London, UK, 2017; pp. 1–131. [Google Scholar]
- Statistics Korea. Annual Report on the Causes of Death Statistics, 2019; Statistics Korea: Daejeon, Republic of Korea, 2020. Available online: https://www.kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=read&aSeq=385219 (accessed on 18 March 2024).
- Feigin, V.L.; Braininm, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int. J. Stroke 2022, 17, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.H. Stroke Rehabilitation Fact Sheet in Korea. Ann. Rehabil. Med. 2022, 46, 1–8. [Google Scholar] [CrossRef]
- Barker-Collo, S.; Feigin, V.L.; Parag, V.; Lawes, C.M.M.; Senior, H. Auckland Stroke Outcomes Study. Part 2: Cognition and functional outcomes 5 years poststroke. Neurology 2010, 75, 1608–1616. [Google Scholar] [CrossRef]
- Kim, W.S.; Bae, H.J.; Lee, H.H.; Shin, H.I. Status of rehabilitation after ischemic stroke: A Korean nationwide study. Ann. Rehabil. Med. 2018, 42, 528–535. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart disease and stroke statistics—2018 update. A report from the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [PubMed]
- Lee, Y.S.; Lee, H.Y.; Leigh, J.H.; Choi, Y.; Kim, H.K.; Oh, B.M. The socioeconomic burden of acquired brain injury among the Korean patients over 20 years of age in 2015–2017: A prevalence-based approach. Brain Neurorehabilit. 2021, 14, e22. [Google Scholar] [CrossRef]
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensach, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global and regional burden of stroke during 1990–2010: Findings from the Global Burden of Diseases Study 2010. Lancet 2014, 383, 245–254. [Google Scholar] [CrossRef]
- Salter, K.; Hellings, C.; Foley, N.; Teasell, R. The experience of living with stroke: A qualitative meta-synthesis. J. Rehabil. Med. 2008, 40, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Scholte op Reimer, W.J.; de Haan, R.J.; Rijnders, P.T.; Limburg, M.; van den Bos, G.A. The Burden of Caregiving in Partners of Long-Term Stroke Survivors. Stroke 1998, 29, 1605–1611. [Google Scholar] [CrossRef]
- Choi-Kwon, S.; Kim, H.; Kwon, S.U.; Kim, J.S. Factors affecting the burden on caregivers of stroke survivors in South Korea. Arch. Phys. Med. Rehabil. 2005, 86, 1043–1048. [Google Scholar] [CrossRef] [PubMed]
- McCullagh, E.; Brigstocke, G.; Donaldson, N.; Kalra, L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke 2005, 36, 2181–2186. [Google Scholar] [CrossRef]
- Vincent, C.; Desrosiers, J.; Landreville, P.; Demers, L. Burden of caregivers of people with stroke: Evolution and predictors. Cerebrovasc. Dis. 2009, 27, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Blake, H.; Lincoln, N.B.; Clarke, D.D. Caregiver strain in spouses of stroke patients. Clin. Rehabil. 2003, 17, 312–317. [Google Scholar] [CrossRef]
- Van den Heuvel, E.T.; de Witte, L.P.; Schure, L.M.; Sanderman, R.; Meyboom-de Jong, B. Risk factors for burn-out in caregivers of stroke patients, and possibilities for intervention. Clin. Rehabil. 2001, 15, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Achilike, S.; Beauchamp, J.E.S.; Cron, S.G.; Okpala, M.; Payen, S.S.; Baldridge, L.; Okpala, N.; Montiel, T.C.; Varughese, T.; Love, M.; et al. Caregiver Burden and Associated Factors Among Informal Caregivers of Stroke Survivors. J. Neurosci. Nurs. 2020, 52, 277–283. [Google Scholar] [CrossRef]
- Freytes, I.M.; Sullivan, M.; Schmitzberger, M.; LeLaurin, J.; Orozco, T.; Eliazar-Macke, N.; Uphold, C. Types of stroke-related deficits and their impact on family caregiver’s depressive symptoms, burden, and quality of life. Disabil. Health J. 2021, 14, 101019. [Google Scholar] [CrossRef]
- Zhu, W.; Jiang, Y. A Meta-analytic Study of Predictors for Informal Caregiver Burden in Patients With Stroke. J. Stroke Cerebrovasc. Dis. 2018, 27, 3636–3646. [Google Scholar] [CrossRef]
- Badaru, U.M.; Ogwumike, O.O.; Adeniyi, A.F.; Nelson, E.E. Determinants of caregiving burden and quality of life of informal caregivers of African stroke survivors: Literature review. Int. J. Disabil. Hum. Dev. 2017, 16, 249–258. [Google Scholar] [CrossRef]
- Kwon, B.M.; Lee, H.H.; Sohn, M.K.; Kim, D.Y.; Shin, Y.I.; Oh, G.J.; Lee, Y.S.; Joo, M.C.; Lee, S.Y.; Song, M.K.; et al. Contributing Factors to the Burden on Primary Family Caregivers of Stroke Survivors in South Korea. Int. J. Environ. Res. Public Health 2023, 20, 2760. [Google Scholar] [CrossRef]
- Jaracz, K.; Grabowska-Fudala, B.; Górna, K.; Jaracz, J.; Moczko, J.; Kozubski, W. Burden in caregivers of long-term stroke survivors: Prevalence and determinants at 6 months and 5 years after stroke. Patient Educ. Couns. 2015, 98, 1011–1016. [Google Scholar] [CrossRef] [PubMed]
- Visser-Meily, A.; Post, M.; van de Port, I.; Maas, C.; Forstberg-Wärleby, G.l; Lindeman, E. Psychosocial functioning of spouses of patients with stroke from initial inpatient rehabilitation to 3 years poststroke: Course and relations with coping strategies. Stroke 2009, 40, 1399–1404. [Google Scholar] [CrossRef]
- Quinn, K.; Murray, C.; Malone, C. Spousal experiences of coping with and adapting to caregiving for a partner who has a stroke: A meta-synthesis of qualitative research. Disabil. Rehabil. 2014, 36, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Kamel, A.A.; Bond, E.; Froelicher, E.S. Stroke Patients’ Caregivers: Their Experiences and Needs: A Qualitative Literature Review. Jordan Med. J. 2009, 43, 341–350. [Google Scholar]
- Tooth, L.; McKenna, K.; Barnett, A.; Prescott, C.; Murphy, S. Caregiver burden, time spent caring and health status in the first 12 months following stroke. Brain Inj. 2005, 19, 963–974. [Google Scholar] [CrossRef]
- Teel, C.S.; Duncan, P.; Lai, S.M. Caregiving experiences after stroke. Nurs. Res. 2001, 50, 53–60. [Google Scholar] [CrossRef]
- Chang, W.H.; Sohn, M.K.; Lee, J.; Kim, D.Y.; Lee, S.G.; Shin, Y.I.; Oh, G.J.; Lee, Y.S.; Joo, M.C.; Han, E.Y.; et al. Korean Stroke Cohort for functioning and rehabilitation (KOSCO): Study rationale and protocol of a multi-centre prospective cohort study. BMC Neurol. 2015, 15, 42. [Google Scholar] [CrossRef]
- Caserta, M.S.; Lund, D.A.; Wright, S.D. Exploring the Caregiver Burden Inventory (CBI): Further evidence for a multidimensional view of burden. Int. J. Aging Hum. Dev. 1996, 43, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Oh, M.S.; Yu, K.H.; Lee, J.H.; Jung, S.; Ko, I.S.; Shin, J.H.; Cho, S.J.; Choi, H.C.; Kim, H.H.; Lee, B.C. Validity and reliability of a korean version of the national institutes of health stroke scale. J. Clin. Neurol. 2012, 8, 177–183. [Google Scholar] [CrossRef]
- Bernardini, J.; Callen, S.; Fried, L.; Piraino, B. Inter-rater reliability and annual rescoring of the Charlson comorbidity index. Adv. Perit. Dial. 2004, 20, 125–127. [Google Scholar]
- Banks, J.L.; Marotta, C.A. Outcomes validity and reliability of the modified Rankin scale: Implications for stroke clinical trials: A literature review and synthesis. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.W.; Na, D.L.; Hahn, S.H. A validity study on the korean mini-mental state examination (K-MMSE) in dementia patients. J. Korean Neurol. Assoc. 1997, 15, 300–308. [Google Scholar]
- Fugl-Meyer, A.R.; Jääskö, L.; Leyman, I.; Olsson, S.; Steglind, S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand. J. Rehabil. Med. 1975, 7, 13–31. [Google Scholar] [CrossRef] [PubMed]
- Bom, P.S.; Mi, H.Y.; Wan, H.J.; Hoyoung, Y.; Woo, P.K.; Kichun, N. Standardization of Korean Version of Frenchay Aphasia Screening Test in Normal Adults. Ann. Rehabil. Med. 2009, 33, 436–440. [Google Scholar]
- Holden, M.K.; Gill, K.M.; Magliozzi, M.R.; Nathan, J.; Piehl-Baker, L. Clinical gait assessment in the neurologically impaired: Reliability and meaningfulness. Phys. Ther. 1984, 64, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Wesling, M.; Brady, S.; Jensen, M.; Nickell, M.; Statkus, D.; Escobar, N. Dysphagia outcomes in patients with brain tumors undergoing inpatient rehabilitation. Dysphagia 2003, 18, 203–210. [Google Scholar] [PubMed]
- Jung, H.Y.; Park, B.K.; Shin, H.S.; Kang, Y.K.; Pyun, S.B.; Paik, N.J.; Kim, S.H.; Kim, T.H.; Han, T.R. Development of the Korean Version of Modified Barthel Index (K-MBI): Multi-center study for subjects with stroke. J. Korean Acad. Rehabil. Med. 2007, 31, 283–297. [Google Scholar]
- Lesher, E.L.; Berryhill, J.S. Validation of the Geriatric Depression Scale--Short Form among inpatients. J. Clin. Psychol. 1994, 50, 256–260. [Google Scholar] [CrossRef]
- Greiner, W.; Claes, C.; Busschbach, J.J.; von der Schulenburg, J.M. Validating the EQ-5D with time trade off for the German population. Eur. J. Health Econ. 2005, 6, 124–130. [Google Scholar] [CrossRef]
- Kang, Y.S.; Choi, S.Y.; Ryu, E. The effectiveness of a stress coping program based on mindfulness meditation on the stress, anxiety, and depression experienced by nursing students in Korea. Nurse Educ. Today 2009, 29, 538–543. [Google Scholar]
- Uhm, K.E.; Jung, H.; Oh-Park, M.; Lee, B.R.; Kim, E.J.; Kim, J.H.; Lee, S.A.; Shin, J.; Kim, Y.S.; Hyun, C.; et al. Reliability and validity of the Korean version of the Caregiver Burden Inventory. Int. J. Rehabil. Res. 2021, 44, 209–214. [Google Scholar] [CrossRef]
- Lee, Y.K.; Nam, H.S.; Chuang, L.H.; Kim, K.Y.; Yang, H.K.; Kwon, I.S.; Kind, P.; Kweon, S.S.; Kim, Y.T. South Korean time trade-off values for EQ-5D health states: Modeling with observed values for 101 health states. Value Health 2009, 12, 1187–1193. [Google Scholar] [CrossRef]
- Schulz, R.; Tompkins, C.A.; Rau, M.T. A longitudinal study of the psychosocial impact of stroke on primary support persons. Psychol. Aging 1988, 3, 131–141. [Google Scholar] [CrossRef]
- Khanapur, U.M.; Jacob, J.; Arun, M.M.; Sanjith, A. Predictors of Caregiver Burden of Moderate and Severe Stroke Survivors: A Cross-Sectional Study from South India. J. Stroke Med. 2021, 4, 34–43. [Google Scholar] [CrossRef]
- Kumar, A.; Yadav, A.K.; Singh, V.K.; Pathak, A.; Chaurasia, R.N.; Mishra, V.N.; Joshi, D. Caregiver Burden in Caregivers of Stroke Survivors: A Hospital-Based Study. Ann. Indian Acad. Neurol. 2022, 25, 1092–1098. [Google Scholar]
- Ziaka, E.; Tsiakiri, A.; Vlotinou, P.; Christidi, F.; Tsiptsios, D.; Aggelousis, N.; Vadikolias, K.; Serdari, A. A Holistic Approach to Expressing the Burden of Caregivers for Stroke Survivors: A Systematic Review. Healthcare 2024, 12, 565. [Google Scholar] [CrossRef]
- Elmståhl, S.; Malmberg, B.; Annerstedt, L. Caregiver’s burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch. Phys. Med. Rehabil. 1996, 77, 177–182. [Google Scholar] [CrossRef]
- Robinson, B.C. Validation of a Caregiver Strain Index. J. Gerontol. B Psychol. Sci. Soc. Sci. 1983, 38, 344–348. [Google Scholar] [CrossRef]
- Hall, J.F.; Crocker, T.F.; Clarke, D.J.; Forster, A. Supporting carers of stroke survivors to reduce carer burden: Development of the Preparing is Caring intervention using Intervention Mapping. BMC Public Health 2019, 19, 1408. [Google Scholar] [CrossRef]
- Bugge, C.; Alexander, H.; Hagen, S. Stroke patients’ informal caregivers. Patient, caregiver, and service factors that affect caregiver strain. Stroke 1999, 30, 1517–1523. [Google Scholar] [CrossRef]
- Koh, Y.S.; Koh, G.C.; Matchar, D.B.; Hong, S.I.; Tai, B.C. Examining the Influence of Social Interactions and Community Resources on Caregivers’ Burden in Stroke Settings: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 12310. [Google Scholar] [CrossRef]
- Yeung, E.H.; Szeto, A.; Richardson, D.; Lai, S.H.; Lim, E.; Cameron, J.I. The experiences and needs of Chinese-Canadian stroke survivors and family caregivers as they re-integrate into the community. Health Soc. Care Community 2015, 23, 523–531. [Google Scholar] [CrossRef]
- Qiu, X.; Sit, J.W.H.; Koo, F.K. The influence of Chinese culture on family caregivers of stroke survivors: A qualitative study. J. Clin. Nurs. 2018, 27, e309–e319. [Google Scholar] [CrossRef] [PubMed]

| Responders (n = 58) | Non-Responders (n = 834) | p Value a | |
|---|---|---|---|
| Patient characteristics b | |||
| Age, mean (SD), decades | 7.45 (1.14) | 6.93 (1.21) | 0.001 |
| Male gender, n (%) | 30 (51.7) | 482 (57.8) | 0.366 |
| Ischemic stroke, n (%) | 48 (82.8) | 652 (78.2) | 0.412 |
| Premorbid mRS, median (IQR) | 0.00 (0.00–0.00) | 0.00 (0.00–1.00) | 0.014 |
| Comorbidity, CCAS, mean (SD) | 5.07 (1.68) | 5.24 (1.53) | 0.418 |
| Comorbidity, WIC, mean (SD) | 2.52 (0.76) | 2.70 (0.85) | 0.106 |
| Initial NIHSS, mean (SD) | 7.34 (9.10) | 4.72 (6.45) | 0.035 |
| K-MMSE, mean (SD) c | 17.40 (10.02) | 24.16 (7.01) | <0.001 |
| FMA, mean (SD) c | 78.84 (30.26) | 87.15 (25.16) | 0.045 |
| FAC, median (IQR) c | 4.00 (3.00–5.00) | 5.00 (4.00–5.00) | 0.002 |
| ASHA-NOMS, median (IQR) c | 7.00 (7.00–7.00) | 7.00 (7.00–7.00) | 0.382 |
| K-FAST, mean (SD) d | 16.45 (9.39) | 21.56 (8.73) | <0.001 |
| mRS, median (IQR) c | 2.00 (1.00–3.00) | 1.00 (1.00–2.00) | <0.001 |
| K-MBI, mean (SD) c | 80.52 (28.28) | 88.76 (21.54) | 0.033 |
| GDS-SF, mean (SD) e | 6.97 (3.93) | 5.53 (4.03) | 0.029 |
| EQ-5D, mean (SD) | 52.81 (39.87) | 72.20 (30.83) | <0.001 |
| Caregiver characteristics | |||
| Age, mean (SD), decades | 6.02 (1.17) | 5.97 (1.36) | 0.786 |
| Male gender, n (%) | 20 (34.5) | 290 (34.8) | 0.964 |
| Employment, n (%) | 23 (39.7) | 347 (41.6) | 0.771 |
| Education, n (%) f | |||
| Primary school and below | 7 (12.1) | 141 (16.9) | 0.937 |
| Middle school | 9 (15.5) | 113 (13.5) | |
| High school | 23 (39.7) | 279 (33.5) | |
| College and above | 15 (25.9 | 267 (32.0) | |
| Relationship with patient, n (%) | |||
| Spouse | 28 (48.3) | 486 (58.3) | 0.577 |
| Children | 25 (43.1) | 261 (31.3) | |
| Daughter-in-law | 4 (6.9) | 27 (3.2) | |
| Paid caregiver | 0 | 6 (0.7) | |
| Grandchildren | 0 | 4 (0.5) | |
| Parent | 1 (1.7) | 16 (1.9) | |
| Other | 0 | 34 (4.1) | |
| Level of relationship, n (%) | |||
| Very good | 14 (24.1) | 293 (35.1) | 0.058 |
| Good | 30 (51.7) | 394 (47.2) | |
| Average | 12 (20.7) | 134 (16.1) | |
| Bad | 2 (3.4) | 12 (1.4) | |
| Very bad | 0 | 1 (0.1) | |
| Cohabitation with patient, n (%) | 40 (69.0) | 635 (76.1) | 0.218 |
| Care at home, n (%) | 44 (75.9) | 697 (83.6) | 0.130 |
| Consignment to long-term care institution, n (%) | 4 (6.9) | 42 (5.0) | 0.536 |
| Care in hospital, n (%) | 7 (12.1) | 75 (9.0) | 0.433 |
| Use of social services, n (%) | 0 | 10 (1.2) | 0.402 |
| Presence of alternative caregiver, n (%) | 26 (44.8) | 280 (33.6) | 0.081 |
| Self-rated health, n (%) | |||
| Very good | 5 (8.6) | 65 (7.8) | 0.257 |
| Good | 15 (25.9) | 284 (34.1) | |
| Average | 22 (37.9) | 332 (39.8) | |
| Bad | 16 (27.6) | 137 (16.4) | |
| Very bad | 0 | 16 (1.9) | |
| Self-rated stress, n (%) | |||
| Extremely | 11 (19.0) | 67 (8.0) | 0.080 |
| Very | 13 (22.4) | 182 (21.8) | |
| Moderately | 16 (27.6) | 278 (33.3) | |
| Slightly | 8 (13.8) | 161 (19.3) | |
| Not at all | 10 (17.2) | 146 (17.5) | |
| Knowledge of stroke, n (%) | |||
| Motor symptoms | 50 (86.2) | 652 (78.2) | 0.149 |
| Speech symptoms | 47 (81.0) | 661 (79.3) | 0.746 |
| Visual symptoms | 38 (65.5) | 481 (57.7) | 0.242 |
| Ataxic symptoms | 48 (82.8) | 644 (77.2) | 0.328 |
| Acute stage treatment | 44 (75.9) | 579 (69.4) | 0.302 |
| Caregiver burden, mean (SD) | 33.62 (15.10) | 30.99 (13.93) | 0.167 |
| Psychosocial stress, PWI-SF, mean (SD) | 17.57 (10.14) | 18.03 (10.97) | 0.756 |
| Quality of life, EQ-5D, mean (SD) g | 89.86 (7.96) | 90.96 (7.64) | 0.292 |
| Score Range (Bad to Good) | 6 Months | 6 Years | p Value b | |
|---|---|---|---|---|
| Age, mean (SD), decades | 7.45 (1.14) | |||
| Male gender, n (%) | 30 (51.7) | |||
| Ischemic stroke, n (%) | 48 (82.8) | |||
| Premorbid mRS, median (IQR) | 6–0 | 0.00 (0.00–0.00) | ||
| Comorbidity, CCAS, mean (SD) | 16–1 | 5.07 (1.68) | ||
| Comorbidity, WIC, mean (SD) | 13–1 | 2.52 (0.76) | ||
| Initial NIHSS, mean (SD) | 42–0 | 7.34 (9.10) | ||
| K-MMSE, mean (SD) | 0–30 | 17.40 (10.02) | 13.62 (11.91) | 0.002 |
| FMA, mean (SD) | 0–100 | 78.84 (30.26) | 77.78 (29.73) | 0.731 |
| FAC, median (IQR) | 0–5 | 4.00 (3.00–5.00) | 4.00 (2.00–5.00) | 0.208 |
| ASHA-NOMS, median (IQR) | 1–7 | 7.00 (7.00–7.00) | 7.00 (6.00–7.00) | 0.083 |
| K-FAST, mean (SD) a | 0–30 | 16.45 (9.39) | 15.70 (10.84) | 0.909 |
| mRS, median (IQR) | 6–0 | 2.00 (1.00–3.00) | 2.50 (1.00–4.00) | 0.183 |
| K-MBI, mean (SD) | 0–100 | 80.52 (28.28) | 72.00 (30.94) | 0.007 |
| GDS-SF, mean (SD) a | 15–0 | 6.97 (3.93) | 2.36 (3.71) | <0.001 |
| EQ-5D, mean (SD) c | −1.7–100 | 52.81 (39.87) | 38.24 (43.43) | 0.023 |
| 6 Months | 6 Years | p Value b | |
|---|---|---|---|
| Age, mean (SD), decades | 6.02 (1.17) | 6.64 (1.21) | <0.001 |
| Male gender, n (%) | 20 (34.5) | 17 (29.3) | 0.549 |
| Employment, n (%) | 23 (39.7) | 23 (39.7) | 1.000 |
| Education a, n (%) | |||
| Primary school and below | 7 (12.1) | 8 (13.8) | 0.211 |
| Middle school | 9 (15.5) | 12 (20.7) | |
| High school | 23 (39.7) | 21 (36.2) | |
| College and above | 15 (25.9) | 14 (24.1) | |
| Relationship with patient, n (%) | |||
| Spouse | 28 (48.3) | 27 (46.6) | 0.417 |
| Children | 25 (43.1) | 26 (44.8) | |
| Daughter-in-law | 4 (6.9) | 2 (3.4) | |
| Paid caregiver | 0 | 2 (3.4) | |
| Grandchildren | 0 | 0 | |
| Parent | 1 (1.7) | 1 (1.7) | |
| Other | 0 | 0 | |
| Level of relationship, n (%) | |||
| Very good | 14 (24.1) | 24 (41.4) | 0.048 |
| Good | 30 (51.7) | 22 (37.9) | |
| Average | 12 (20.7) | 12 (20.7) | |
| Bad | 2 (3.4) | 0 | |
| Very bad | 0 | 0 | |
| Cohabitation with patient, n (%) | 40 (69.0) | 37 (63.8) | 0.508 |
| Care at home, n (%) | 44 (75.9) | 44 (75.9) | 1.000 |
| Consignment to long-term care institution, n (%) | 4 (6.9) | 8 (13.8) | 0.289 |
| Care in hospital, n (%) | 7 (12.1) | 2 (3.4) | 0.125 |
| Use of social services, n (%) | 0 | 3 (5.2) | 0.250 |
| Presence of alternative caregiver, n (%) | 26 (44.8) | 22 (37.9) | 0.481 |
| Self-rated health, n (%) | |||
| Very good | 5 (8.6) | 4 (6.9) | 0.537 |
| Good | 15 (25.9) | 15 (25.9) | |
| Average | 22 (37.9) | 31 (53.4) | |
| Bad | 16 (27.6) | 8 (13.8) | |
| Very bad | 0 | 0 | |
| Self-rated stress, n (%) | |||
| Extremely | 11 (19.0) | 5 (8.6) | 0.418 |
| Very | 13 (22.4) | 19 (32.8) | |
| Moderately | 16 (27.6) | 23 (39.7) | |
| Slightly | 8 (13.8) | 6 (10.3) | |
| Not at all | 10 (17.2) | 5 (8.6) | |
| Knowledge of stroke, n (%) | |||
| Motor symptoms | 50 (86.2) | 44 (75.9) | 0.263 |
| Speech symptoms | 47 (81.0) | 45 (77.6) | 0.824 |
| Visual symptoms | 38 (65.5) | 34 (58.6) | 0.541 |
| Ataxic symptoms | 48 (82.8) | 46 (79.3) | 0.832 |
| Acute stage treatment | 44 (75.9) | 38 (65.5) | 0.286 |
| Psychosocial stress, PWI-SF, mean (SD) | 17.57 (10.14) | 16.52 (11.47) | 0.516 |
| Quality of life, EQ-5D, mean (SD) c | 89.86 (7.96) | 92.16 (5.92) | 0.050 |
| 6 Months | 6 Years | p Value b | |
|---|---|---|---|
| Caregiver burden total score, mean (SD) | 33.62 (15.10) | 34.38 (13.62) | 0.718 |
| Time-dependence domain, mean (SD) | 2.83 (1.36) | 3.34 (1.28) | 0.029 |
| Developmental domain, mean (SD) | 2.37 (1.28) | 2.45 (1.17) | 0.640 |
| Physical domain, mean (SD) | 2.08 (1.16) | 1.98 (1.07) | 0.595 |
| Social domain, mean (SD) | 2.04 (0.91) | 1.96 (0.90) | 0.542 |
| Emotional domain, mean (SD) | 2.23 (1.16) | 2.21 (1.07) | 0.891 |
| Financial domain, mean (SD) | 2.03 (0.98) | 2.08 (0.90) | 0.753 |
| High caregiver burden, n (%) c | 22 (37.9) | 30 (51.7) | 0.077 |
| 6 Months | 6 Years | |||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Patient characteristics a | ||||
| Initial NIHSS | 1.19 (1.06–1.33) | 0.002 | ||
| Cognitive function (K-MMSE) | 0.91 (0.86–0.97) | 0.002 | ||
| Motor function (FMA) | 0.96 (0.94–0.98) | 0.001 | 0.95 (0.92–0.98) | 0.003 |
| Mobility function (FAC) | 0.38 (0.23–0.63) | <0.001 | 0.44 (0.28–0.70) | <0.001 |
| Swallowing function (ASHA-NOMS) | 0.41 (0.17–0.99) | 0.048 | ||
| Disability (mRS) | 3.41 (1.83–6.35) | <0.001 | 2.93 (1.70–5.04) | <0.001 |
| Activities of daily living (K-MBI) | 0.94 (0.91–0.98) | 0.002 | 0.96 (0.93–0.98) | <0.001 |
| Quality of life (EQ-5D) | 0.97 (0.95–0.98) | <0.001 | 0.98 (0.97–0.99) | 0.004 |
| Caregiver characteristics a | ||||
| Education | 0.37 (0.18–0.73) | 0.004 | ||
| Patients’ children (reference = spouse) b | 0.16 (0.05–0.56) | 0.004 | ||
| Level of relationship | 2.29 (1.06–4.93) | 0.035 | ||
| Presence of alternative caregiver | 0.21 (0.06–0.70) | 0.011 | ||
| Self-rated health | 2.54 (1.26–5.13) | 0.009 | 2.32 (1.09–4.96) | 0.029 |
| Self-rated stress | 0.19 (0.08–0.44) | <0.001 | 0.30 (0.14–0.63) | 0.002 |
| Psychosocial stress (PWI-SF) | 1.19 (1.09–1.31) | <0.001 | 1.13 (1.05–1.21) | <0.001 |
| Quality of life (EQ-5D) | 0.88 (0.81–0.96) | 0.005 | ||
| 6 Months | 6 Years | |||
|---|---|---|---|---|
| OR (95% CI) a | p Value | OR (95% CI) a | p Value | |
| Patient characteristics | ||||
| Disability (mRS) | 11.60 (1.58–85.08) | 0.016 | 5.88 (2.19–15.82) | <0.001 |
| Caregiver characteristics | ||||
| Self-rated stress | 0.03 (0.00–0.47) | 0.016 | ||
| Psychosocial stress (PWI-SF) | 1.26 (1.10–1.44) | 0.001 | ||
| Quality of life (EQ-5D) | 0.76 (0.59–0.99) | 0.042 | ||
| R2adj b | 0.855 | 0.733 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-W.; Sohn, M.K.; Lee, J.; Kim, D.Y.; Shin, Y.-I.; Oh, G.-J.; Lee, Y.-S.; Joo, M.C.; Lee, S.Y.; Han, J.; et al. Predictors of Burden for First-Ever Stroke Survivor’s Long-Term Caregivers: A Study of KOSCO. Medicina 2024, 60, 559. https://doi.org/10.3390/medicina60040559
Lee J-W, Sohn MK, Lee J, Kim DY, Shin Y-I, Oh G-J, Lee Y-S, Joo MC, Lee SY, Han J, et al. Predictors of Burden for First-Ever Stroke Survivor’s Long-Term Caregivers: A Study of KOSCO. Medicina. 2024; 60(4):559. https://doi.org/10.3390/medicina60040559
Chicago/Turabian StyleLee, Jin-Won, Min Kyun Sohn, Jongmin Lee, Deog Young Kim, Yong-Il Shin, Gyung-Jae Oh, Yang-Soo Lee, Min Cheol Joo, So Young Lee, Junhee Han, and et al. 2024. "Predictors of Burden for First-Ever Stroke Survivor’s Long-Term Caregivers: A Study of KOSCO" Medicina 60, no. 4: 559. https://doi.org/10.3390/medicina60040559
APA StyleLee, J.-W., Sohn, M. K., Lee, J., Kim, D. Y., Shin, Y.-I., Oh, G.-J., Lee, Y.-S., Joo, M. C., Lee, S. Y., Han, J., Ahn, J., Kim, Y.-H., Song, M.-K., & Chang, W. H. (2024). Predictors of Burden for First-Ever Stroke Survivor’s Long-Term Caregivers: A Study of KOSCO. Medicina, 60(4), 559. https://doi.org/10.3390/medicina60040559









