Abstract
Background and Objectives: Despite advancements in detection and treatment, cervical cancer remains a significant health concern, particularly among young women of reproductive age. Limited data exists in the literature regarding fertility-sparing treatment (FST) of cervical cancers with tumor sizes greater than 2 cm. The objective of this systematic review was to evaluate the reproductive outcomes of women diagnosed with cervical cancer greater than 2 cm who underwent FST. Materials and Methods: A comprehensive search of the literature was carried out on the following databases: MEDLINE, EMBASE, Global Health, The Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cochrane Methodology Register), the Health Technology Assessment Database, and Web of Science. Only original studies (retrospective or prospective) that reported reproductive outcomes of patients with cervical cancer >2 cm were considered eligible for inclusion in this systematic review (CRD42024521964). Studies describing only the oncologic outcomes, involving FST for cervical cancers less than 2 cm in size, and case reports were excluded. Results: Seventeen papers that met the abovementioned inclusion criteria were included in the present systematic review. In total, 443 patients with a cervical cancer larger than 2 cm were included in this systematic review. Eighty pregnancies occurred, with 24 miscarriages and 54 live births. Conclusions: FST appears to be a viable option for women of childbearing age diagnosed with cervical cancer larger than 2 cm. However, careful consideration is advised in interpreting these encouraging results, as they are subject to limitations, such as variability in study designs and potential biases. In addition, reproductive outcomes should be further cross-referenced with oncologic outcomes to clarify the potential risk–benefit ratio. It is critical to conduct further research using standardized approaches and larger participant groups to strengthen the validity of the conclusions drawn.
1. Introduction
Cervical cancer, despite advancements in detection and treatment, remains a significant health concern, particularly among young women of reproductive age. Uterine cervix cancer ranks as the third most frequently occurring cancer among women under the age of 40 [1], and nearly 40% of cases involving early-stage cervical cancer occur in young women who wish to maintain their fertility and may consider fertility-preserving surgery as an option [2]. Furthermore, with the increasing average age of first pregnancy in Western countries, the risk of being diagnosed with cervical neoplasm before achieving reproductive goals has progressively risen [3]. Fertility-sparing treatment (FST) has emerged as a valuable option for preserving reproductive capacity in this population, especially for those with early-stage disease [4]. However, the optimal management of young women with early-stage cervical cancer, specifically those with tumor sizes greater than 2 cm undergoing FST, remains a subject of ongoing debate and investigation.
In the 2019 guidelines of the National Comprehensive Cancer Network (NCCN), a fertility-sparing approach continues to be recommended for IB1 tumors smaller than 2 cm in size [5]. Nonetheless, the guidelines emphasize that according to some authors, a 2 cm threshold could be utilized for vaginal radical trachelectomy (VRT), while a 4 cm threshold may be preferred for abdominal radical trachelectomy (ART) [6].
In this context, in recent decades, the occurrence and mortality rates of cervical cancer in affluent nations have declined due to the introduction of structured screening programs and advancements in diagnostic and prognostic methodologies [7]. Furthermore, considering the high 5-year survival rates exceeding 90% for early-stage cervical cancer, with a significant portion of these patients being in their reproductive years (up to 40%), the need for FST is evident [8].
In addition to exposure to HPV, the primary risk factor, various other factors contribute to the development of cervical cancer, including early initiation of sexual activity (before 16 years of age), multiple sexual partners, smoking, high parity, chronic oxidative stress, and socioeconomic disadvantage [9,10,11].
Understanding the reproductive outcomes in this specific subgroup is crucial for guiding clinical decision-making and improving patient counseling. Therefore, this systematic review aimed to comprehensively evaluate the existing literature on reproductive outcomes in young women with early-stage cervical cancer (>2 cm) undergoing FST, providing insights into the effectiveness and safety of these approaches in preserving fertility while ensuring optimal oncological and reproductive outcomes.
Objectives
The aim of this systematic review was to evaluate the reproductive outcomes of women diagnosed with cervical cancer greater than 2 cm who underwent FST.
2. Materials and Methods
2.1. Eligibility Criteria
Only original studies (retrospective or prospective) that reported reproductive outcomes of patients with cervical cancer >2 <4 cm were considered eligible for inclusion in this systematic review. Studies describing only the oncologic outcomes, studies involving FST for cervical cancers less than 2 cm in size, and case report studies were excluded. Due to the limited amount of literature available on the subject, we did not exclude studies in which FST was proposed in selected cases, even for tumors larger than 4 cm.
2.2. Information Sources
This study was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12], available through the Enhancing the Quality and Transparency of Health Research (EQUATOR) network, and the Cochrane Handbook for Systematic Reviews [13]. The study was registered with the international prospective register of systematic reviews (PROSPERO) under the registration number CRD42024521964.
MEDLINE, EMBASE, Global Health, the Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cochrane Methodology Register), Health Technology Assessment Database, Web of Science, and Research Register (ClinicalTrial.gov) were searched for studies describing patients who underwent FST for cervical cancer greater than 2 cm.
2.3. Search Strategy
The following medical subject heading (MeSH) and key search terms were used: “Uterine Cervical Neoplasm” (MeSH Unique ID: D002583) AND “2 cm” AND “Fertility sparing” (MeSH Unique ID: D059247) OR “Conservative treatment” (MeSH Unique ID: D000072700) AND “Trachelectomy” (MeSH Unique ID: D000069339) OR “Conization” (MeSH Unique ID: D019092) AND “Laparotomy” (MeSH Unique ID: D007813) OR “Laparoscopy” (MeSH Unique ID: D010535). We selected papers written in English from the inception of each database until 1 February 2024.
2.4. Study Selection
Titles and/or abstracts of studies retrieved using the search strategy were screened independently by 2 review authors (A.E. and A.S.L.) to identify studies that met the inclusion criteria.
The full texts of these potentially eligible articles were retrieved and independently assessed for eligibility by two other review team members (M.M. and A.D.). A manual search of the references of the included studies was also conducted to prevent the omission of pertinent research.
Any disagreements between them over the eligibility of the articles were resolved through discussion with a third (external) collaborator. All the authors approved the final selection.
2.5. Data Extraction
Two authors (V.A. and V.C.) independently extracted data from articles about study features, characteristics of the included populations, FSTs, complications, and results/outcomes using a prepiloted standard form to ensure consistency. One author (M.D.) reviewed the entire data-extraction process.
2.6. Assessment of Risk of Bias
Two reviewers (A.M.M. and R.F.) independently assessed the risk of bias of studies included in this systematic review using a modified version of the Newcastle–Ottawa Scale (NOS) [14]. The quality of the studies was evaluated in five different domains: “study design and sample representativeness”, “sampling technique”, “description of the fertility-sparing treatment”, “quality of the population description”, and “incomplete outcome data” (Table S1). Any disagreements between the reviewers were resolved by a third reviewer (A.G.).
2.7. Outcome Measures and Data Synthesis
The primary objective of this study was to evaluate the reproductive outcomes of women with early-stage cervical cancer greater than 2 cm who underwent FST. Quantitative analysis was not possible due to data heterogeneity (including differences in the type of FST). We provided a descriptive synthesis of the results in separate sections based on the type of surgical approach employed for FST (trachelectomy, conization). The body of evidence on the effectiveness of FST for IA G2EC was assessed by two authors (A.E. and G.T.) using the Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence (OCEBM) [15].
3. Results
3.1. Study Selection
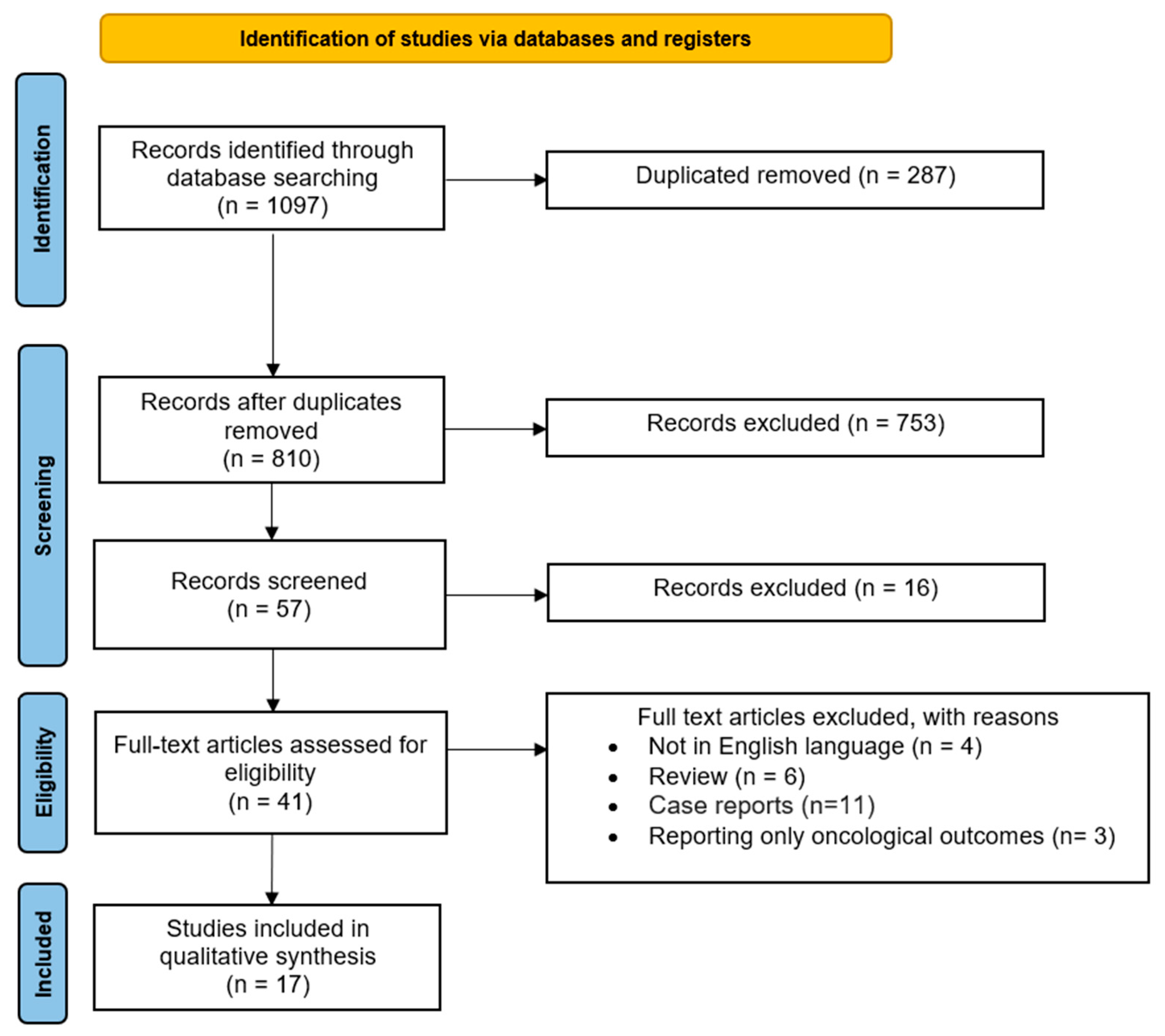
The study selection process is displayed in Figure 1. After the evaluation of the full texts, 17 papers that met the abovementioned inclusion criteria [6,8,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30] were included in the present systematic review.

Figure 1.
PRISMA flow diagram of the review.
3.2. Study Characteristics
The main characteristics of the included studies are summarized in Table 1. Four studies were prospective [16,17,26,29], and twelve were retrospective studies [6,8,18,19,20,21,22,23,25,27,28,30]. One study was a case series [24].

Table 1.
Characteristics of the included studies.
Of these, five studies were from China [6,16,18,19,22], two were from Germany [20,29], two from the Netherlands [28,30], one was from Italy [17], one from Hungary [21], one from France [23], one from Colombia [25], one from Czech Republic [26], one from Belgium [27], one from United States [8], and one from Canada [24].
3.3. Risk of Bias of Included Studies
Of the seventeen studies included, nine had a low risk of bias in three or more domains [8,16,17,19,20,21,22,23,25], and eight had a high risk of bias [6,18,24,26,27,28,29,30]. A detailed description of the risk of bias in each domain among the studies is reported in Table S2.
3.4. Synthesis of the Results
Among the included studies, 14 employed trachelectomy as the FST approach for cervical cancer greater than 2 cm [6,8,16,18,19,20,21,22,23,24,26,28,29,30], while in two studies conization was evaluated [17,27]. In one study, both approaches were employed [25]. Furthermore, NACT was administered before FST in 11 studies [17,20,22,23,24,25,26,27,28,29,30]. The range of tumor size and methodology used to establish it in the included studies are shown in Table 2. As previously mentioned, we discussed the results separately based on the type of FST approach used in the various included studies.

Table 2.
Range of tumor size and methodology used for the assessment in the included studies.
3.4.1. Trachelectomy
Fifteen studies evaluated trachelectomy as an FST for patients affected by cervical tumors of a size exceeding 2 cm [6,8,16,18,19,20,21,22,23,24,25,26,28,29,30]. Of these, eight employed an abdominal approach [6,8,18,19,21,22,25,28], five used a vaginal approach [20,24,26,29,30], and one compared the effectiveness of both approaches [16]. Moreover, in one study, laparoscopic-assisted radical vaginal trachelectomy (LARVT) was utilized [23]. Additional information regarding the included studies can be found in Table 3.

Table 3.
Reproductive outcomes of studies reporting FST with trachelectomy for early-stage cervical cancer greater than 2 cm.
Cao et al. [16] compared the surgical and fertility outcomes of 150 patients treated by either VRT or ART. Forty-eight patients (32%) were affected by cervical cancer greater than 2 cm: 24 in the VRT group (50%) and 24 in the ART group (50%). Twenty-four patients tried to conceive (50%) after successfully preserving fertility, and three pregnancies occurred, resulting in three live births (100%). Patients with tumor sizes greater than 2 cm exhibited significantly higher rates of recurrence (11.6% versus 2.4%, with a p-value less than 0.05) and lower rates of pregnancy (12.5% versus 32.1%, with a p-value of 0.094) compared to patients with tumor sizes less than 2 cm.
Deng et al. [18] assessed the surgical, oncologic, and fertility outcomes in 45 patients treated with sentinel lymph node biopsy (SNLB)-guided ART. Five pregnancies occurred, with four miscarriages (80%) and one full-term delivery (20%). Similar results were obtained by Guo et al. [19], Li et al. [6], and Lintner et al. [21]. In the series by Wethington et al. [8], no pregnancies occurred.
Lanowska et al. [20] evaluated the use of NACT before VRT for the FST of 20 patients. TP or TIP for two or three cycles was administered to all patients. Seven patients achieved pregnancy; of these, one miscarriage and one ectopic pregnancy occurred (28.6%). Eventually, four live births were obtained (57.1%), with another ongoing pregnancy reported by the authors. Comparable findings were achieved by Plante et al. [24], Robova et al. [26], Vercellino et al. [29], and Zusterzeel et al. [30].
Marchiolè et al. [23] evaluated the feasibility of LARVT after NACT with TP, TIP, or TEP in 19 patients. Three live births occurred in the series.
Lu et al. [22] employed an ART approach following NACT with bleomycin + cisplatin + mitomycin in seven patients. After surgery, four patients tried to conceive (57.1), and one live birth occurred (50%). Analogous outcomes were observed by Rendòn et al. [25], and Tesfai et al. [28].
Quality of evidence: The evidence regarding the safety, effectiveness, and reliability of FST employing trachelectomy for early-stage cervical cancers of a size greater than 2 cm was classified as evidence level 3.
3.4.2. Conization
In three studies, conization was applied as the FST for cervical cancers of a size exceeding 2 cm [17,25,27]. Additional information regarding the included studies can be found in Table 4.

Table 4.
Reproductive outcomes of studies reporting FST with conization for early-stage cervical cancer greater than 2 cm.
As previously mentioned, Rendòn et al. [25] employed both conization and trachelectomy for FST. In all the three included studies, NACT was administered before performing surgery.
De Vincenzo et al. [17] evaluated the use of NACT before cold-knife conization in 13 patients. The NACT regimen involved TP for three cycles in all patients. After surgery, three patients attempted to conceive (33.3%), and two pregnancies occurred, resulting in 2 live births (66.7%). Similar results were obtained by Rendòn et al. [25] and by Salihi et al. [27].
Quality of evidence: The evidence regarding the safety, effectiveness, and reliability of FST employing conization for early-stage cervical cancers of a size greater than 2 cm was classified as evidence level 3.
4. Discussion
The present qualitative analysis on reproductive outcomes in young women with early-stage cervical cancer (>2 cm) undergoing FST illuminates several critical points. Firstly, our findings underscore the importance of fertility preservation in this patient population, given the substantial proportion of women of reproductive age affected by cervical cancer. FST can offer promising reproductive outcomes, providing hope for future parenthood for these women.
Since its inception by Prof Daniel Dargent in the late 1980s, VRT has undergone significant evolution. Dargent’s groundbreaking work revolutionized the management of early-stage cervical cancer by demonstrating the safe preservation of the uterine body and fertility potential in well-selected cases. Over time, this original procedure has evolved into various techniques, including ART, and more recently, laparoscopic and robotic radical trachelectomy (RRT) [3,20,31,32,33]. Furthermore, FST currently represents a feasible and well-established treatment option for other types of gynecological tumors [34,35,36]. With the implementation of new technologies in surgery [37] and the development and advancements in endoscopic surgery [38,39], minimally invasive treatment is increasingly evolving, becoming a reality.
An analysis of surveillance, epidemiology, and end results (SEER) data revealed that procedures preserving the uterus, such as cold-knife conization or trachelectomy, do not carry a significant risk of mortality when compared to hysterectomy [40]. In the same study, a tumor size greater than 2 cm represented a factor independently associated with worsened survival. In this context, the use of NACT for cervical cancers measuring 2–4 cm before FST is gaining significance, with the purpose of reducing tumor size, facilitating surgical removal, and mitigating adverse prognostic factors linked to suboptimal treatment response [41].
NACT, followed by surgery, enhances both overall survival and progression-free survival compared to surgery alone, resulting in a significant decrease in the risk of mortality [42]. Moreover, numerous studies have confirmed that NACT decreases the necessity for adjuvant radiotherapy while also reducing tumor size, lymph node involvement, and distant metastasis [26,43].
The status of lymph nodes plays a critical role as well, as a prognostic indicator, influencing the risk of recurrence and mortality [44]. However, there is currently no standardized approach for the timing of lymph node assessment compared to NACT, leaving this aspect uncertain [45,46]. Assessment of lymph nodes prior to neo-adjuvant chemotherapy seems the proper approach to better define patients with positive nodes, and, thus, poor prognosis, thereby excluding those most likely to require adjuvant treatment [20,27]. Furthermore, NACT administration before lymph node assessment may increase the pool of patients suitable for FST [47].
In total, the reproductive outcomes of 443 patients with a cervical cancer larger than 2 cm were evaluated in this systematic review. Among the included patients, 80 pregnancies occurred, with 24 miscarriages and 54 live births. The final pregnancy rate was 18.1%, with a miscarriage rate of 30% and a live birth rate of 67.5%.
Regarding trachelectomy, it represents a feasible option for FST of early-stage cervical cancers, offering favorable oncological and reproductive outcomes, even though it represents a technique that needs to be tailored to each patient [48,49]. In the present systematic review, 77 pregnancies occurred in 430 patients after trachelectomy (17.9%), resulting in 50 live births (64.9%).
On the other hand, with regard to conization, one study did not report disaggregated data about reproductive outcomes with conization or trachelectomy [25]; hence, it was possible to evaluate only the data pertaining to two studies [17,27]. Three pregnancies occurred among 23 patients (13%), all three resulting three live births (100%). Overall, the data currently available in the literature are too limited to make statements regarding the feasibility and reproductive outcomes of conization as an FST for cervical tumors larger than 2 cm [50].
However, we must also acknowledge the challenges and limitations associated with fertility-sparing approaches, including the risk of disease recurrence, the need for long-term follow-up to assess oncologic safety, and the rate of obstetric complications associated with surgical procedures. As evidence of this, the rate of infertility, premature rupture of the membranes, and premature delivery are significantly higher in patients who underwent trachelectomy [51,52]. In this systematic review, the rate of preterm delivery found after trachelectomy was up to 30%.
Regarding the pros and cons of the two procedures, trachelectomy offers the advantage of a more complete excision of the neoplasm but with the great downside of the impairment of fertility, mainly due to the excision of the parametrium and of the healthy cervical stroma extending beyond the tumor [53], the high miscarriage rate and preterm birth rate (approximately 30%, as found in this systematic review) [53,54], and adverse surgical outcomes in terms of urologic and neurologic morbidities [55]. On the other hand, conization is less invasive and associated with fewer complications but may not provide as high a chance of achieving a complete resection of the lesion, especially in cases of larger or more advanced tumors, such as cervical cancers greater than 2 cm. Ultimately, the choice between the two should depend also on individual patient factors and preferences. Moreover, the socioeconomic status of the patient is important both for cervical cancer prevention, access to fertility-sparing treatments, and for follow-up, as women with higher socioeconomic status will undergo more frequent check-ups, while females from disadvantaged socioeconomic backgrounds exhibit higher rates of incidence and mortality associated with cervical neoplasm [56]. In this regard, a recent population-based cohort study including 7736 young women with early-stage cervical, endometrial, or ovarian cancer undergoing FST demonstrated disparities in both clinical and sociodemographic factors affecting the utilization of FST among patients across different socioeconomic statuses [57].
Limitations
Despite the valuable insights provided by this systematic review, several limitations should be acknowledged. Firstly, the lack of high-quality studies and the heterogeneity among the included studies may have introduced biases and limited the generalizability of our findings. Additionally, variations in study designs, patient populations, and treatment modalities across the included studies may have affected the reliability of the results.
5. Conclusions
In conclusion, our systematic review highlights the significance of FST for young women diagnosed with early-stage cervical cancer, particularly those with tumors larger than 2 cm. Despite the limited number of studies available, our analysis suggests that fertility-sparing approaches hold promise for preserving reproductive function in this population.
However, the variability in treatment protocols and the lack of standardized guidelines underscore the need for further research to optimize patient selection criteria, refine therapeutic strategies, and enhance reproductive outcomes. Additionally, long-term follow-up studies are warranted to assess the oncologic safety and fertility preservation efficacy of these approaches.
Overall, our findings emphasize the importance of personalized and multidisciplinary care in managing young women with early-stage cervical cancer, ensuring both oncologic control and preservation of fertility.
Supplementary Materials
The following supporting information can be downloaded from https://www.mdpi.com/article/10.3390/medicina60040608/s1, Table S1: Modified Newcastle–Ottawa scale items, Table S2: Risk of bias assessment.
Author Contributions
Conceptualization, V.C. and G.R.; methodology, A.G.; software, V.A.; validation, A.M. and R.F.; formal analysis, M.M.; investigation, A.S.L.; resources, M.D.; data curation, A.D.; writing—original draft preparation, A.D. and A.E.; writing—review and editing, G.T. and A.S.L.; supervision, V.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Sonoda, Y.; Abu-Rustum, N.R.; Gemignani, M.L.; Chi, D.S.; Brown, C.L.; Poynor, E.A.; Barakat, R.R. A Fertility-Sparing Alternative to Radical Hysterectomy: How Many Patients May Be Eligible? Gynecol. Oncol. 2004, 95, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Plante, M. Evolution in Fertility-Preserving Options for Early-Stage Cervical Cancer: Radical Trachelectomy, Simple Trachelectomy, Neoadjuvant Chemotherapy. Int. J. Gynecol. Cancer 2013, 23, 982–989. [Google Scholar] [CrossRef]
- Theofanakis, C.; Koulakmanidis, A.-M.; Prodromidou, A.; Haidopoulos, D.; Rodolakis, A.; Thomakos, N. Fertility-Sparing Treatment for Young Patients with Early-Stage Cervical Cancer: A Dawn of a New Era. Front. Surg. 2022, 9, 867993. [Google Scholar] [CrossRef]
- Koh, W.-J.; Abu-Rustum, N.R.; Bean, S.; Bradley, K.; Campos, S.M.; Cho, K.R.; Chon, H.S.; Chu, C.; Clark, R.; Cohn, D.; et al. Cervical Cancer, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2019, 17, 64–84. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wu, X.; Li, X.; Ju, X. Abdominal Radical Trachelectomy: Is It Safe for IB1 Cervical Cancer with Tumors ≥ 2 Cm? Gynecol. Oncol. 2013, 131, 87–92. [Google Scholar] [CrossRef] [PubMed]
- SEER Cancer Statistics Review, 1975–2018 [Internet]. 2021. Available online: https://seer.cancer.gov/csr/1975_2018/index.html (accessed on 19 March 2024).
- Wethington, S.L.; Sonoda, Y.; Park, K.J.; Alektiar, K.M.; Tew, W.P.; Chi, D.S.; Leitao, M.M.; Jewell, E.; Barakat, R.R.; Abu-Rustum, N.R. Expanding the Indications for Radical Trachelectomy: A Report on 29 Patients with Stage IB1 Tumors Measuring 2–4 Centimeters. Int. J. Gynecol. Cancer 2013, 23, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Xu, H.; Zhang, L.; Qiao, Y. Cervical Cancer: Epidemiology, Risk Factors and Screening. Chin. J. Cancer Res. 2020, 32, 720–728. [Google Scholar] [CrossRef] [PubMed]
- Ghebre, R.G.; Grover, S.; Xu, M.J.; Chuang, L.T.; Simonds, H. Cervical Cancer Control in HIV-Infected Women: Past, Present and Future. Gynecol. Oncol. Rep. 2017, 21, 101–108. [Google Scholar] [CrossRef]
- Despot, A.; Fureš, R.; Despot, A.-M.; Mikuš, M.; Zlopaša, G.; D’Amato, A.; Chiantera, V.; Serra, P.; Etrusco, A.; Laganà, A.S. Reactive Oxygen Species within the Vaginal Space: An Additional Promoter of Cervical Intraepithelial Neoplasia and Uterine Cervical Cancer Development? Open Med. 2023, 18, 20230826. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Home—2020. The Centre for Evidence-Based Medicine. Available online: https://www.cebm.net/ (accessed on 20 January 2024).
- Cao, D.Y.; Yang, J.X.; Wu, X.H.; Chen, Y.L.; Li, L.; Liu, K.J.; Cui, M.H.; Xie, X.; Wu, Y.M.; Kong, B.H.; et al. Comparisons of Vaginal and Abdominal Radical Trachelectomy for Early-Stage Cervical Cancer: Preliminary Results of a Multi-Center Research in China. Br. J. Cancer 2013, 109, 2778–2782. [Google Scholar] [CrossRef] [PubMed][Green Version]
- de Vincenzo, R.; Ricci, C.; Fanfani, F.; Gui, B.; Gallotta, V.; Fagotti, A.; Ferrandina, G.; Scambia, G. Neoadjuvant Chemotherapy Followed by Conization in Stage IB2-IIA1 Cervical Cancer Larger than 2 Cm: A Pilot Study. Fertil. Steril. 2021, 115, 148–156. [Google Scholar] [CrossRef]
- Deng, X.; Zhang, Y.; Li, D.; Zhang, X.; Guo, H.; Wang, F.; Sheng, X. Abdominal Radical Trachelectomy Guided by Sentinel Lymph Node Biopsy for Stage IB1 Cervical Cancer with Tumors >2 cm. Oncotarget 2017, 8, 3422–3429. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Zhang, Y.; Chen, X.; Sun, L.; Chen, K.; Sheng, X. Surgical and Oncologic Outcomes of Radical Abdominal Trachelectomy Versus Hysterectomy for Stage IA2-IB1 Cervical Cancer. J. Minim. Invasive Gynecol. 2019, 26, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Lanowska, M.; Mangler, M.; Speiser, D.; Bockholdt, C.; Schneider, A.; Köhler, C.; Vasiljeva, J.; Al-Hakeem, M.; Vercellino, G.F. Radical Vaginal Trachelectomy after Laparoscopic Staging and Neoadjuvant Chemotherapy in Women with Early-Stage Cervical Cancer over 2 Cm: Oncologic, Fertility, and Neonatal Outcome in a Series of 20 Patients. Int. J. Gynecol. Cancer 2014, 24, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Lintner, B.; Saso, S.; Tarnai, L.; Novak, Z.; Palfalvi, L.; Del Priore, G.; Smith, J.R.; Ungar, L. Use of Abdominal Radical Trachelectomy to Treat Cervical Cancer Greater than 2 Cm in Diameter. Int. J. Gynecol. Cancer 2013, 23, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Zhang, Y.; Wang, S.; Guo, S.; Guo, H.; Zhang, Z.; Liu, C. Neoadjuvant Intra-Arterial Chemotherapy Followed by Total Laparoscopic Radical Trachelectomy in Stage IB1 Cervical Cancer. Fertil. Steril. 2014, 101, 812–817. [Google Scholar] [CrossRef] [PubMed]
- Marchiolè, P.; Ferraioli, D.; Moran, E.; Mammoliti, S.; Tigaud, J.-D.; Beurrier, F.; Chopin, N.; Mathevet, P. NACT and Laparoscopic-Assisted Radical Vaginal Trachelectomy in Young Patients with Large (2–5 cm) High Risk Cervical Cancers: Safety and Obstetrical Outcome. Surg. Oncol. 2018, 27, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Plante, M.; Lau, S.; Brydon, L.; Swenerton, K.; LeBlanc, R.; Roy, M. Neoadjuvant Chemotherapy Followed by Vaginal Radical Trachelectomy in Bulky Stage IB1 Cervical Cancer: Case Report. Gynecol. Oncol. 2006, 101, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Rendón, G.J.; Lopez Blanco, A.; Aragona, A.; Saadi, J.M.; Di Guilmi, J.; Arab Eblen, C.; Heredia Muñoz, F.; Pareja, R. Oncological and Obstetrical Outcomes after Neo-Adjuvant Chemotherapy Followed by Fertility-Sparing Surgery in Patients with Cervical Cancer ≥2 Cm. Int. J. Gynecol. Cancer 2021, 31, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Robova, H.; Halaska, M.J.; Pluta, M.; Skapa, P.; Matecha, J.; Lisy, J.; Rob, L. Oncological and Pregnancy Outcomes after High-Dose Density Neoadjuvant Chemotherapy and Fertility-Sparing Surgery in Cervical Cancer. Gynecol. Oncol. 2014, 135, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Salihi, R.; Leunen, K.; Van Limbergen, E.; Moerman, P.; Neven, P.; Vergote, I. Neoadjuvant Chemotherapy Followed by Large Cone Resection as Fertility-Sparing Therapy in Stage IB Cervical Cancer. Gynecol. Oncol. 2015, 139, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Tesfai, F.M.; Kroep, J.R.; Gaarenstroom, K.; De Kroon, C.; Van Loenhout, R.; Smit, V.; Trimbos, B.; Nout, R.A.; van Poelgeest, M.I.E.; Beltman, J.J. Fertility-Sparing Surgery of Cervical Cancer >2 cm (International Federation of Gynecology and Obstetrics 2009 Stage IB1-IIA) after Neoadjuvant Chemotherapy. Int. J. Gynecol. Cancer 2020, 30, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Vercellino, G.F.; Piek, J.M.J.; Schneider, A.; Köhler, C.; Mangler, M.; Speiser, D.; Chiantera, V. Laparoscopic Lymph Node Dissection Should Be Performed before Fertility Preserving Treatment of Patients with Cervical Cancer. Gynecol. Oncol. 2012, 126, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Zusterzeel, P.L.M.; Aarts, J.W.M.; Pol, F.J.M.; Ottevanger, P.B.; van Ham, M.A.P.C. Neoadjuvant Chemotherapy Followed by Vaginal Radical Trachelectomy as Fertility-Preserving Treatment for Patients with FIGO 2018 Stage 1B2 Cervical Cancer. Oncologist 2020, 25, e1051–e1059. [Google Scholar] [CrossRef] [PubMed]
- Saito, T.; Matsuura, M.; Tamate, M.; Iwasaki, M.; Mariya, T. Radical Vaginal Trachelectomy. Surg. J. 2021, 7, S103–S107. [Google Scholar] [CrossRef] [PubMed]
- Tsafrir, Z.; Aoun, J.; Hanna, R.; Papalekas, E.; Schiff, L.; Theoharis, E.; Eisenstein, D. Robotic Trachelectomy After Supracervical Hysterectomy for Benign Gynecologic Disease. JSLS 2016, 20, e2016.00027. [Google Scholar] [CrossRef] [PubMed]
- Salvo, G.; Pareja, R.; Ramirez, P.T. Minimally Invasive Radical Trachelectomy: Considerations on Surgical Approach. Best. Pract. Res. Clin. Obstet. Gynaecol. 2021, 75, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Pecorino, B.; Laganà, A.S.; Mereu, L.; Ferrara, M.; Carrara, G.; Etrusco, A.; Di Donna, M.C.; Chiantera, V.; Cucinella, G.; Barra, F.; et al. Evaluation of Borderline Ovarian Tumor Recurrence Rate after Surgery with or without Fertility-Sparing Approach: Results of a Retrospective Analysis. Healthcare 2023, 11, 1922. [Google Scholar] [CrossRef] [PubMed]
- Etrusco, A.; Laganà, A.S.; Chiantera, V.; Mikuš, M.; Arsalan, H.M.; d’Amati, A.; Vitagliano, A.; Cicinelli, E.; Favilli, A.; D’Amato, A. Reproductive and Oncologic Outcomes in Young Women with Stage IA and Grade 2 Endometrial Carcinoma Undergoing Fertility-Sparing Treatment: A Systematic Review. Biomolecules 2024, 14, 306. [Google Scholar] [CrossRef] [PubMed]
- Gullo, G.; Etrusco, A.; Cucinella, G.; Perino, A.; Chiantera, V.; Laganà, A.S.; Tomaiuolo, R.; Vitagliano, A.; Giampaolino, P.; Noventa, M.; et al. Fertility-Sparing Approach in Women Affected by Stage I and Low-Grade Endometrial Carcinoma: An Updated Overview. Int. J. Mol. Sci. 2021, 22, 11825. [Google Scholar] [CrossRef] [PubMed]
- Etrusco, A.; Buzzaccarini, G.; Laganà, A.S.; Chiantera, V.; Vitale, S.G.; Angioni, S.; D’Alterio, M.N.; Nappi, L.; Sorrentino, F.; Vitagliano, A.; et al. Use of Diode Laser in Hysteroscopy for the Management of Intrauterine Pathology: A Systematic Review. Diagnostics 2024, 14, 327. [Google Scholar] [CrossRef] [PubMed]
- Etrusco, A.; Laganà, A.S.; Chiantera, V.; Gerli, S.; Carugno, J.; Sorrentino, F.; Riemma, G.; Vitagliano, A.; Favilli, A. Efficacy, Safety, and Feasibility of the Treatment of Intrauterine Pathologies with the Mini-Resectoscope: A Systematic Review. Int. J. Gynaecol. Obstet. 2024. [Google Scholar] [CrossRef] [PubMed]
- Mazzon, I.; Etrusco, A.; Laganà, A.S.; Chiantera, V.; Di Angelo Antonio, S.; Tosto, V.; Gerli, S.; Favilli, A. Training in Diagnostic Hysteroscopy: The “Arbor Vitae” Method. Medicina 2023, 59, 1019. [Google Scholar] [CrossRef] [PubMed]
- Tseng, J.H.; Aloisi, A.; Sonoda, Y.; Gardner, G.J.; Zivanovic, O.; Abu-Rustum, N.R.; Leitao, M.M. Long-Term Oncologic Outcomes of Uterine-Preserving Surgery in Young Women With Stage Ib1 Cervical Cancer. Int. J. Gynecol. Cancer 2018, 28, 1350–1359. [Google Scholar] [CrossRef] [PubMed]
- Gwacham, N.I.; McKenzie, N.D.; Fitzgerald, E.R.; Ahmad, S.; Holloway, R.W. Neoadjuvant Chemotherapy Followed by Fertility Sparing Surgery in Cervical Cancers Size 2–4 Cm; Emerging Data and Future Perspectives. Gynecol. Oncol. 2021, 162, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Rydzewska, L.; Tierney, J.; Vale, C.L.; Symonds, P.R. Neoadjuvant Chemotherapy plus Surgery versus Surgery for Cervical Cancer. Cochrane Database Syst. Rev. 2012, 12, CD007406. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Shi, Y.; Wang, S.; Lu, Q. Meta-Analysis Showing That Early Response to Neoadjuvant Chemotherapy Predicts Better Survival among Cervical Cancer Patients. Oncotarget 2017, 8, 59609–59617. [Google Scholar] [CrossRef] [PubMed]
- Cibula, D.; McCluggage, W.G. Sentinel Lymph Node (SLN) Concept in Cervical Cancer: Current Limitations and Unanswered Questions. Gynecol. Oncol. 2019, 152, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Ai, C.; Zhang, L.; Ding, W.; Zhong, S.; Li, Z.; Li, M.; Zhang, H.; Zhang, L.; Zhang, L.; Hu, H. A Nomogram-Based Optimized Radscore for Preoperative Prediction of Lymph Node Metastasis in Patients with Cervical Cancer after Neoadjuvant Chemotherapy. Front. Oncol. 2023, 13, 1117339. [Google Scholar] [CrossRef] [PubMed]
- Plaikner, A.; Siegler, K.; Hertel, H.; Jacob, A.; Petzel, A.; Schubert, M.; Blohmer, J.-U.; Böhmer, G.; Marnitz, S.; Ragosch, V.; et al. Fertility Sparing Therapy in Women with Lymph Node Negative Cervical Cancer >2cm—Oncologic and Fertility Outcomes of Neoadjuvant Chemotherapy Followed by Radical Vaginal Trachelectomy. Int. J. Gynecol. Cancer 2023, 33, 1542–1547. [Google Scholar] [CrossRef] [PubMed]
- Maneo, A.; Chiari, S.; Bonazzi, C.; Mangioni, C. Neoadjuvant Chemotherapy and Conservative Surgery for Stage IB1 Cervical Cancer. Gynecol. Oncol. 2008, 111, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Pareja, R.; Rendón, G.J.; Sanz-Lomana, C.M.; Monzón, O.; Ramirez, P.T. Surgical, Oncological, and Obstetrical Outcomes after Abdominal Radical Trachelectomy—A Systematic Literature Review. Gynecol. Oncol. 2013, 131, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Malmsten, C.; Hellberg, P.; Bergmark, K.; Dahm-Kähler, P. Long-Term Fertility, Oncological, and Quality-of-Life Outcomes after Trachelectomy in Early Stage Cervical Cancer. Arch. Gynecol. Obstet. 2019, 299, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Batman, S.H.; Schmeler, K.M. Fertility-Sparing and Less Radical Surgery for Cervical Cancer. Curr. Oncol. Rep. 2022, 24, 1541–1548. [Google Scholar] [CrossRef] [PubMed]
- Okugawa, K.; Kobayashi, H.; Sonoda, K.; Kaneki, E.; Kawano, Y.; Hidaka, N.; Egashira, K.; Fujita, Y.; Yahata, H.; Kato, K. Oncologic and Obstetric Outcomes and Complications during Pregnancy after Fertility-Sparing Abdominal Trachelectomy for Cervical Cancer: A Retrospective Review. Int. J. Clin. Oncol. 2017, 22, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Kasuga, Y.; Ikenoue, S.; Tanaka, M.; Ochiai, D. Management of Pregnancy after Radical Trachelectomy. Gynecol. Oncol. 2021, 162, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Rob, L.; Skapa, P.; Robova, H. Fertility-Sparing Surgery in Patients with Cervical Cancer. Lancet Oncol. 2011, 12, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Bentivegna, E.; Gouy, S.; Maulard, A.; Chargari, C.; Leary, A.; Morice, P. Oncological Outcomes after Fertility-Sparing Surgery for Cervical Cancer: A Systematic Review. Lancet Oncol. 2016, 17, e240–e253. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, P.T.; Pareja, R.; Rendón, G.J.; Millan, C.; Frumovitz, M.; Schmeler, K.M. Management of Low-Risk Early-Stage Cervical Cancer: Should Conization, Simple Trachelectomy, or Simple Hysterectomy Replace Radical Surgery as the New Standard of Care? Gynecol. Oncol. 2014, 132, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.E.; Hannibal, C.G.; Nielsen, A.; Jensen, A.; Nøhr, B.; Munk, C.; Kjaer, S.K. Social Inequality and Incidence of and Survival from Cancer of the Female Genital Organs in a Population-Based Study in Denmark, 1994–2003. Eur. J. Cancer 2008, 44, 2003–2017. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, K.; Meernik, C.; Wu, C.-F.; Murphy, C.C.; Baker, V.L.; Jarmon, P.; Brady, P.C.; Nitecki, R.; Nichols, H.B.; Rauh-Hain, J.A. Disparities in Fertility-Sparing Treatment and Use of Assisted Reproductive Technology After a Diagnosis of Cervical, Ovarian, or Endometrial Cancer. Obstet. Gynecol. 2023, 141, 341–353. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).