Biomechanical Comparison of Fixation Methods for Posterior Wall Fractures of the Acetabulum: Conventional Reconstruction Plate vs. Spring Plate vs. Variable Angle Locking Compression Plate
Abstract
1. Introduction
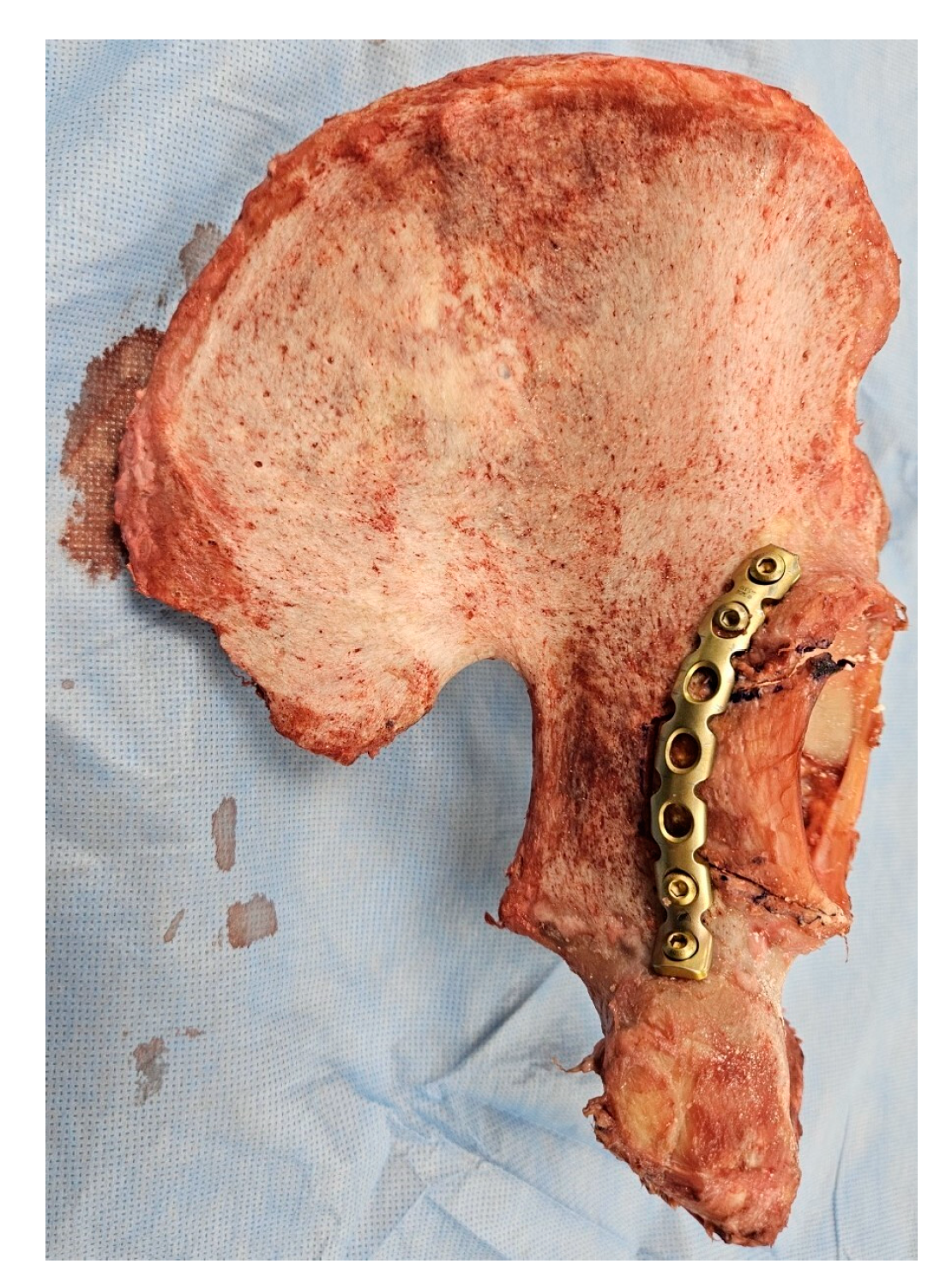
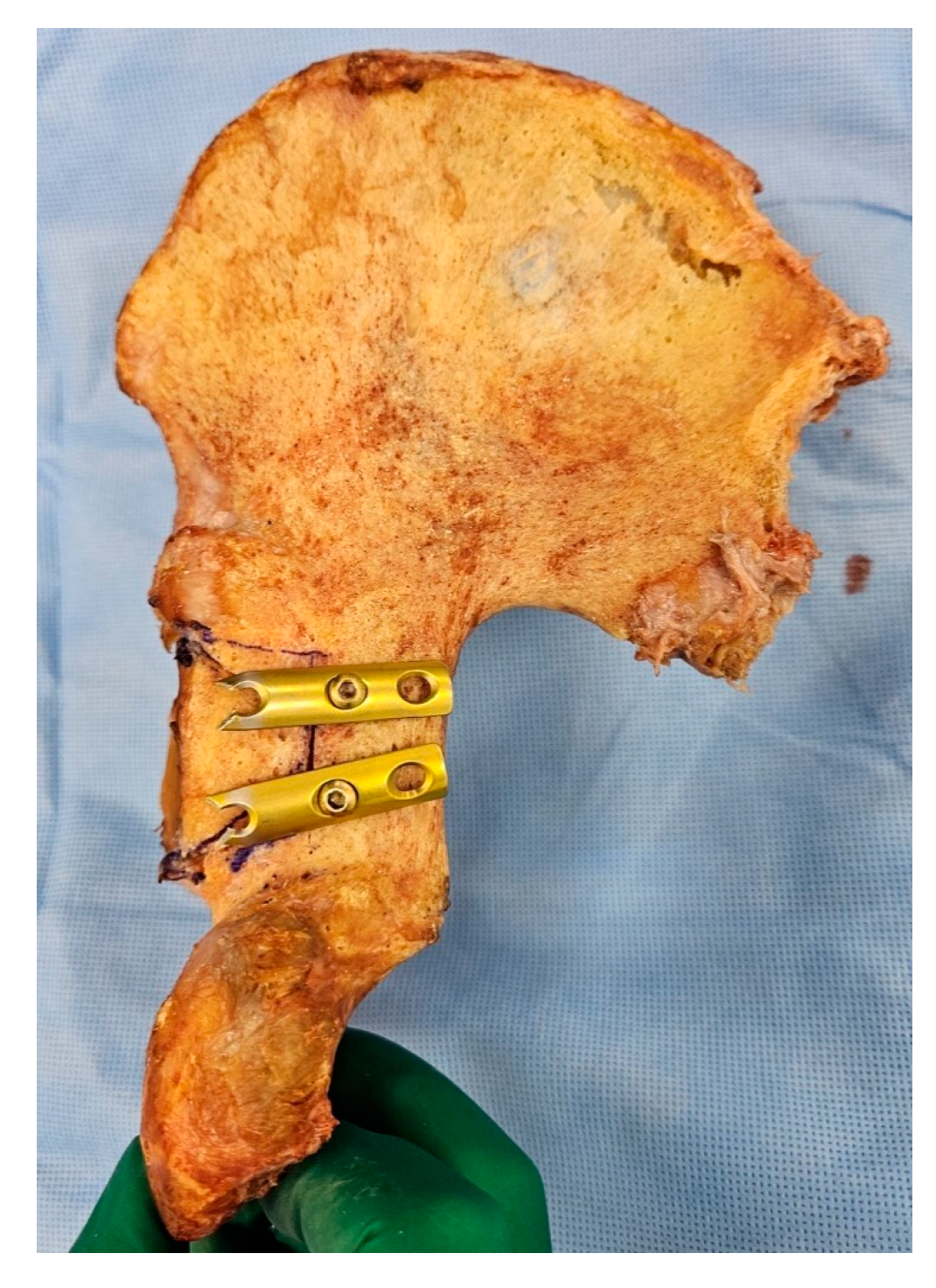
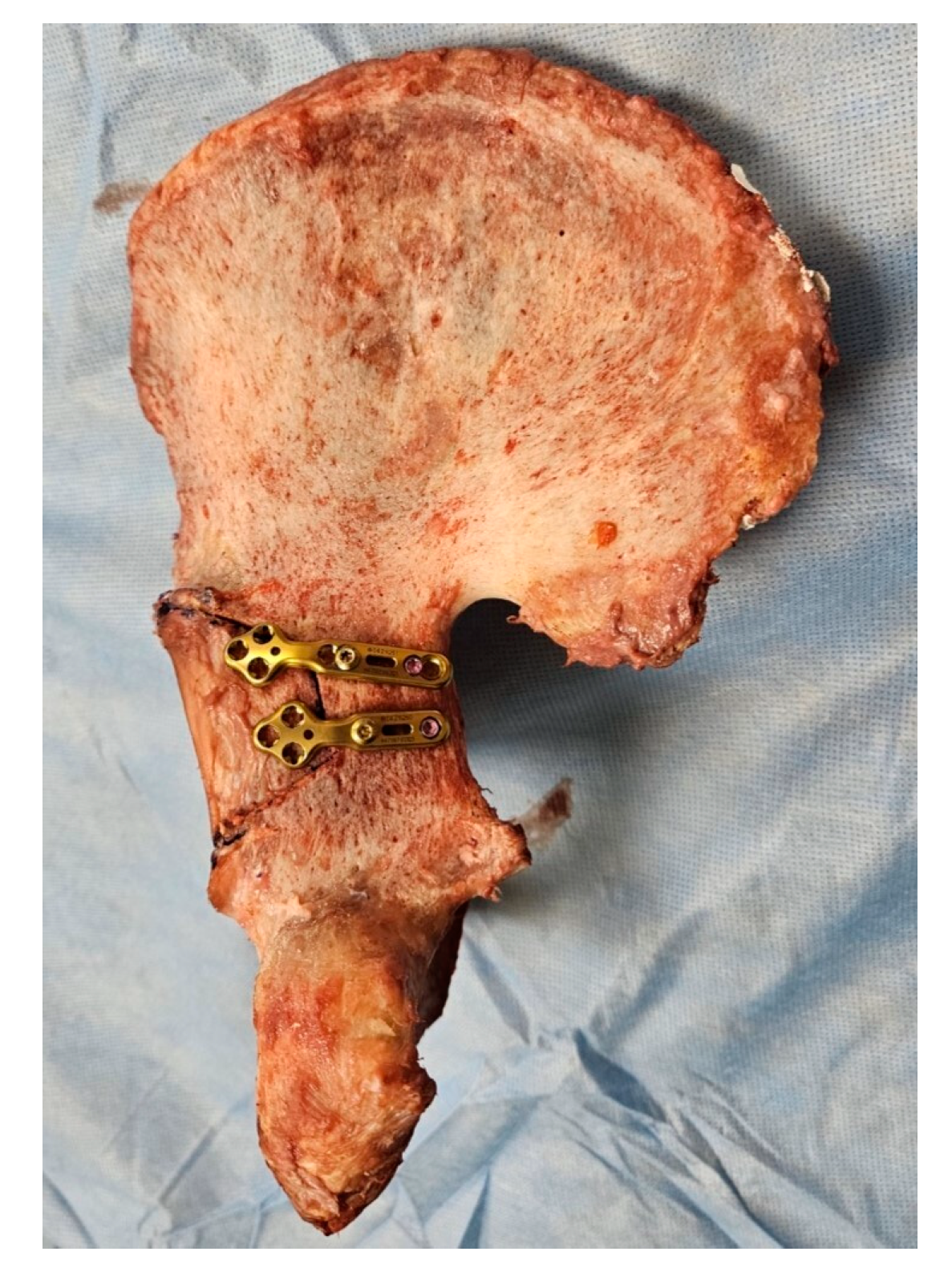
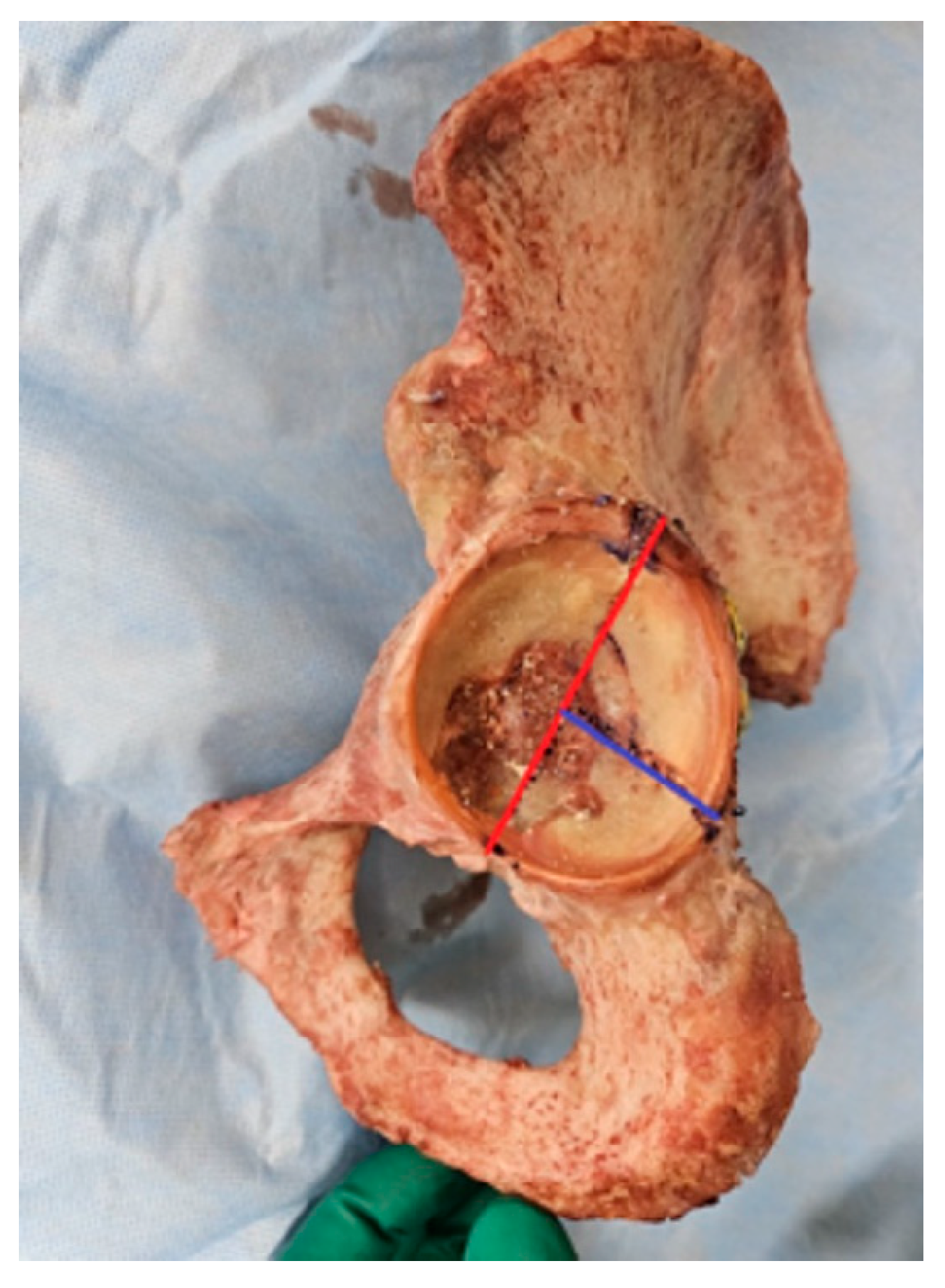
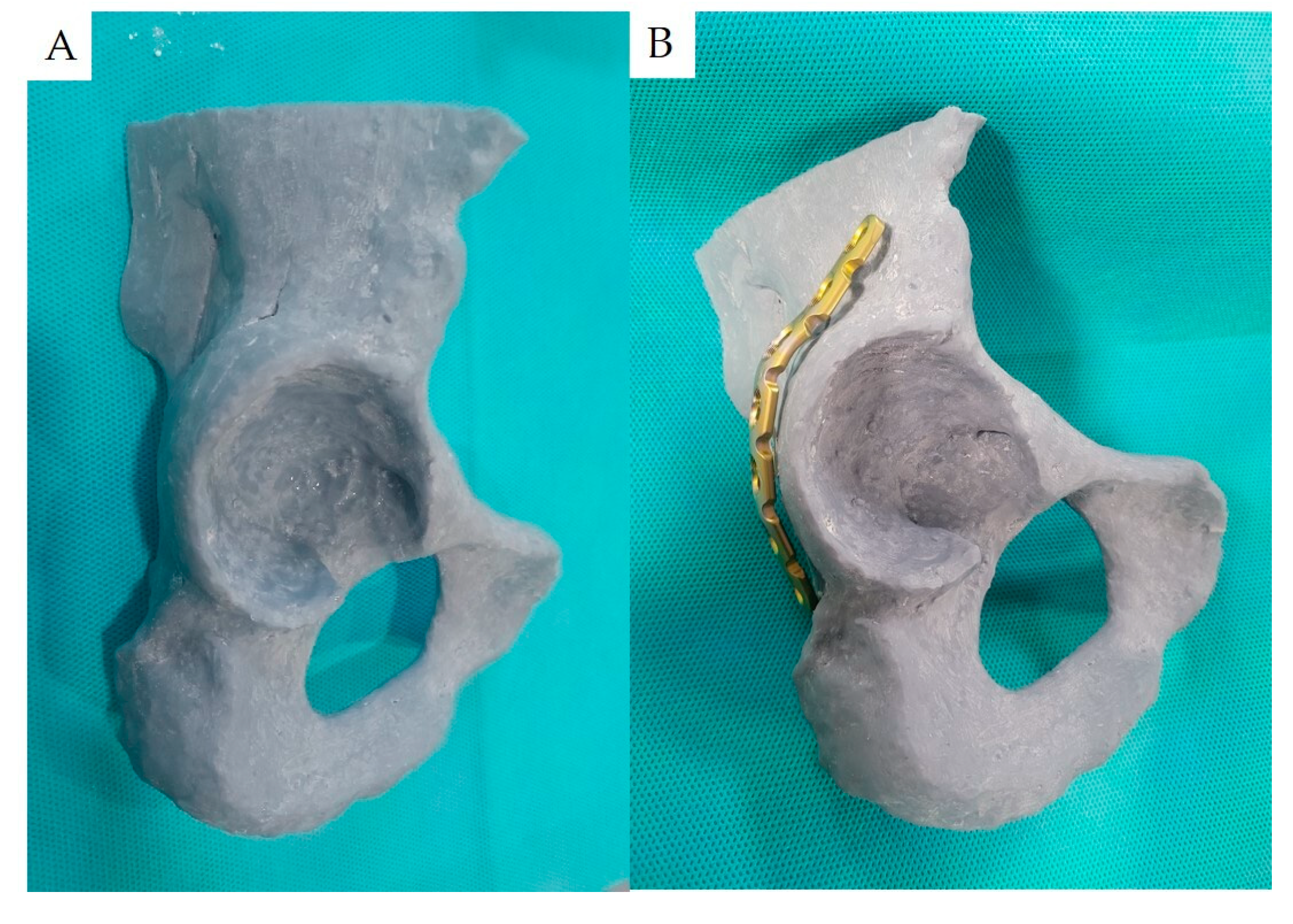
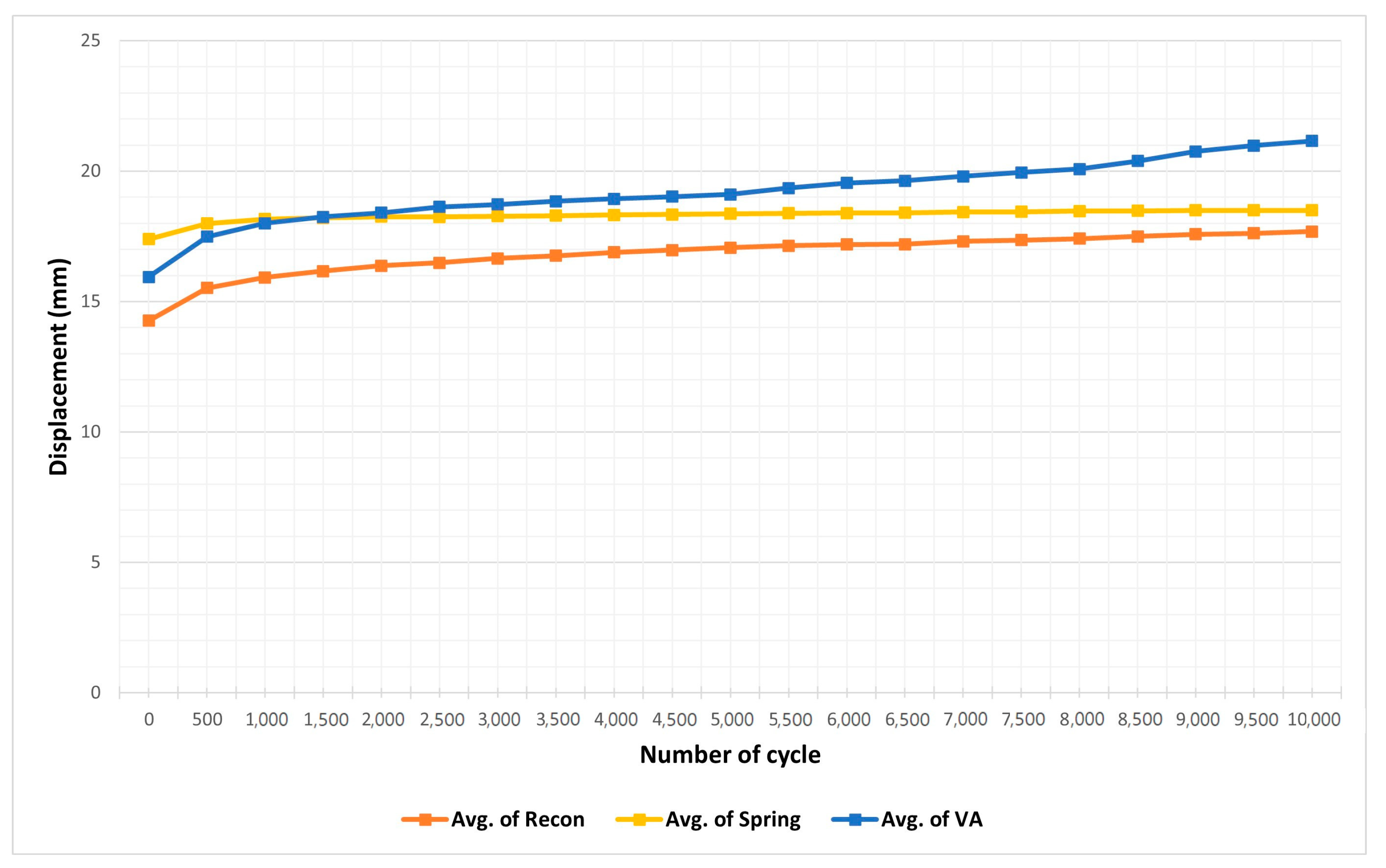
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ochs, B.G.; Marintschev, I.; Hoyer, H.; Rolauffs, B.; Culemann, U.; Pohlemann, T.; Stuby, F.M. Changes in the treatment of acetabular fractures over 15 years: Analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU). Injury 2010, 41, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Moed, B.R.; WillsonCarr, S.E.; Watson, J.T. Results of operative treatment of fractures of the posterior wall of the acetabulum. J. Bone Jt. Surg. Am. 2002, 84, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Letournel, E.; Judet, R. Fractures of the Acetabulum; Springer Science & Business Media: Berlin, Germany, 2013. [Google Scholar]
- Kumar, M.; Ahmed, M.; Hussain, G.; Saleem, M.; Sahar, K.; Bux, M. Frequency of posterior wall acetabular fracture in patients presenting with posterior hip dislocations. Rawal Med. J. 2020, 45, 347. [Google Scholar]
- Moed, B.R.; Kregor, P.J.; Reilly, M.C.; Stover, M.D.; Vrahas, M.S. Current management of posterior wall fractures of the acetabulum. Instr. Course Lect. 2015, 64, 139–159. [Google Scholar] [PubMed]
- Vale, J.; Diniz, S.; Leite, P.S.; Soares, D. Surgical Treatment of Acetabular Posterior Wall Fracture with Hip Arthroscopy: A Case Report. Hip Pelvis 2022, 34, 62–67. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moed, B.R.; Ajibade, D.A.; Israel, H. Computed tomography as a predictor of hip stability status in posterior wall fractures of the acetabulum. J. Orthop. Trauma 2009, 23, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Reagan, J.M.; Moed, B.R. Can computed tomography predict hip stability in posterior wall acetabular fractures? Clin. Orthop. Relat. Res. 2011, 469, 2035–2041. [Google Scholar] [CrossRef]
- Grimshaw, C.S.; Moed, B.R. Outcomes of posterior wall fractures of the acetabulum treated nonoperatively after diagnostic screening with dynamic stress examination under anesthesia. J. Bone Jt. Surg. Am. 2010, 92, 2792–2800. [Google Scholar] [CrossRef]
- Moed, B.R.; Willson Carr, S.E.; Gruson, K.I.; Watson, J.T.; Craig, J.G. Computed tomographic assessment of fractures of the posterior wall of the acetabulum after operative treatment. J. Bone Jt. Surg. Am. 2003, 85, 512–522. [Google Scholar] [CrossRef]
- Matta, J.M. Fractures of the acetabulum: Reduction accuracy and clinical results of fractures operated within three weeks of injury. J. Bone Jt. Surg. Am. 1997, 78, 1632–1645. [Google Scholar] [CrossRef]
- Olson, S.A.; Bay, B.K.; Pollak, A.N.; Sharkey, N.A.; Lee, T. The effect of variable size posterior wall acetabular fractures on contact characteristics of the hip joint. J. Orthop. Trauma 1996, 10, 395–402. [Google Scholar] [CrossRef]
- Moed, B.R.; Carr, S.E.W.; Watson, J.T. Open reduction and internal fixation of posterior wall fractures of the acetabulum. Clin. Orthop. Relat. Res. 2000, 377, 57–67. [Google Scholar] [CrossRef]
- Goulet, J.A.; Rouleau, J.P.; Mason, D.J.; Goldstein, S.A. Comminuted fractures of the posterior wall of the acetabulum. A biomechanical evaluation of fixation methods. J. Bone Jt. Surg. Am. 1994, 76, 1457–1463. [Google Scholar] [CrossRef]
- Zhang, Y.; Tang, Y.; Wang, P.; Zhao, X.; Xu, S.; Zhang, C. Biomechanical comparison of different stabilization constructs for unstable posterior wall fractures of acetabulum. A cadaveric study. PLoS ONE 2014, 8, e82993. [Google Scholar] [CrossRef]
- Zoys, G.N.; McGanity, P.L.; Lanctot, D.R.; Athanasiou, K.A.; Heckman, J.D. Biomechanical evaluation of fixation of posterior acetabular wall fractures. J. South. Orthop. Assoc. 1999, 8, 254–260. [Google Scholar]
- Ferguson, T.A.; Patel, R.; Bhandari, M.; Matta, J.M. Fractures of the acetabulum in patients aged 60 years and older. J. Bone Jt. Surg. Br. 2010, 92, 250–257. [Google Scholar] [CrossRef]
- Schutz, M.; Sudkamp, N.P. Revolution in plate osteosynthesis: New internal fixator systems. J. Orthop. Sci. 2003, 8, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Sommer, C.; Gautier, E.; Muller, M.; Helfet, D.L.; Wagner, M. First clinical results of the Locking Compression Plate (LCP). Injury 2003, 34 (Suppl. S2), B43–B54. [Google Scholar] [CrossRef]
- Fulkerson, E.; Egol, K.A.; Kubiak, E.N.; Liporace, F.; Kummer, F.J.; Koval, K.J. Fixation of diaphyseal fractures with a segmental defect: A biomechanical comparison of locked and conventional plating techniques. J. Trauma 2006, 60, 830–835. [Google Scholar] [CrossRef]
- Frigg, R. Locking Compression Plate (LCP). An osteosynthesis plate based on the Dynamic Compression Plate and the Point Contact Fixator (PC-Fix). Injury 2001, 32 (Suppl. S2), 63–66. [Google Scholar]
- Tadros, A.M.A.; O’Brien, P.; Guy, P. Fixation of Marginal Posterior Acetabular Wall Fractures Using Locking Reconstruction Plates and Monocortical Screws. J. Trauma Inj. Infect. Crit. Care 2010, 68, 478–480. [Google Scholar] [CrossRef] [PubMed]
- Ebraheim, N.A.; Savolaine, E.R.; Hoeflinger, M.J.; Jackson, W.T. Radiological diagnosis of screw penetration of the hip joint in acetabular fracture reconstruction. J. Orthop. Trauma 1989, 3, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Richter, H.; Hutson, J.J.; Zych, G. The Use of Spring Plates in the Internal Fixation of Acetabular Fractures. J. Orthop. Trauma 2004, 18, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Johnson, E.E. Use of Spring Plates in Fixation of Comminuted Posterior Wall Acetabular Fractures. J. Orthop. Trauma 2018, 32, S55–S59. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.W.; Chung, H.J.; Kim, B.S.; Yeo, D.-H.; Song, J.-H.; Oh, C.-W.; Mauffrey, C.; Cho, W.-T.; Oh, J.-K. Fragment specific fixation technique using 2.7 mm VA LCP for comminuted posterior wall acetabular fractures: A novel surgical technique. Arch. Orthop. Trauma Surg. 2019, 139, 1587–1597. [Google Scholar] [CrossRef] [PubMed]
- Al-Mukhtar, A.M.; Konke, C. Fracture Mechanics and Micro Crack Detection in Bone: A Short Communication. In Proceedings of the Medical Device Materials VI: Proceedings from the Materials and Processes for Medical Devices Conference, Minneapolis, MN, USA, 8–10 August 2011; p. 27776. [Google Scholar]
- Pease, F.; Ward, A.; Stevenson, A.; Cunningham, J.; Sabri, O.; Acharya, M.; Chesser, T. Posterior wall acetabular fracture fixation: A mechanical analysis of fixation methods. J. Orthop. Surg. 2019, 27, 2309499019859838. [Google Scholar] [CrossRef]
- Wu, X. A biomechanical comparison of different fixation techniques for fractures of the acetabular posterior wall. Int. Orthop. (SICOT) 2018, 42, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Altun, G.; Saka, G.; Demir, T.; Elibol, F.K.E.; Polat, M.O. Precontoured buttress plate vs reconstruction plate for acetabulum posterior wall fractures: A biomechanical study. World J. Orthop. 2019, 10, 219–227. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mast, J.; Jakob, R.; Ganz, R. Planning and Reduction Technique in Fracture Surgery; Springer: New York, NY, USA, 1989. [Google Scholar]
- Fracture and Dislocation Compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J. Orthop. Trauma 1996, 10 (Suppl. S1), 1–154. [Google Scholar]
- Cho, J.W.; Cho, W.T.; Sakong, S.; Lim, E.J.; Choi, W.; Kang, S.; Kim, B.-S.; Kim, J.-K.; Oh, C.-W.; Oh, J.-K. Mapping of acetabular posterior wall fractures using a three-dimensional virtual reconstruction software. Injury 2021, 52, 1403–1409. [Google Scholar] [CrossRef]
- Moed, B.R.; McMichael, J.C. Outcomes of posterior wall fractures of the acetabulum. Surgical technique. J. Bone Jt. Surg. Am. 2008, 90 Pt 1 (Suppl. S2), 87–107. [Google Scholar] [CrossRef]
- Woo, S.H.; Sung, M.J.; Park, K.S.; Yoon, T.R. Three-dimensional-printing technology in hip and pelvic surgery: Current landscape. Hip Pelvis 2020, 32, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Dessouki, O.; Samiezadeh, S.; Bougherara, H.; Zdero, R.; Schemitsch, E. Biomechanics of Acute Total Hip Arthroplasty after Acetabular Fracture: Plate vs Cable Fixation; Orthopaedic Research Society (ORS): Las Vegas, NV, USA, 2015. [Google Scholar]
- Scannell, B.P.; Loeffler, B.J.; Hoenig, M.; Peindl, R.D.; D’Alessandro, D.F.; Connor, P.M.; Fleischli, J.E. Biomechanical comparison of hamstring tendon fixation devices for anterior cruciate ligament reconstruction: Part 1. Five femoral devices. Am. J. Orthop. 2015, 44, 32–36. [Google Scholar]
- Whittle, M.W. Gait Analysis and Introduction, 4th ed.; Butterworth-Heinemann: Oxford, UK, 2007. [Google Scholar]
- Feng, X.; Zhang, S.; Luo, Q.; Fang, J.; Lin, C.; Leung, F.; Chen, B. Definition of a safe zone for antegrade lag screw fixation of fracture of posterior column of the acetabulum by 3D technology. Injury 2016, 47, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Barnett, V.; Lewis, T. Outliers in Statistical Data; Wiley: New York, NY, USA, 1994; Volume 3, No. 1. [Google Scholar]
- Kim, H.T.; Ahn, J.M.; Hur, J.O.; Lee, J.S.; Cheon, S.J. Reconstruction of acetabular posterior wall fractures. Clin. Orthop. Surg. 2011, 3, 114–120. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tannast, M.; Najibi, S.; Matta, J.M. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J. Bone Jt. Surg. Am. 2012, 94, 1559–1567. [Google Scholar] [CrossRef] [PubMed]
- Clarke-Jenssen, J.; Røise, O.; Storeggen, S.; Madsen, J.E. Long-term survival and risk factors for failure of the native hip joint after operatively treated displaced acetabular fractures. Bone Jt. J. 2017, 99, 834–840. [Google Scholar] [CrossRef] [PubMed]
- Moed, B.R.; McMahon, M.J.; Armbrecht, E.S. The acetabular fracture prognostic nomogram: Does it work for fractures of the posterior wall? J. Orthop. Trauma 2016, 30, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertner, M.R. Fractures of the posterior wall of the acetabulum. J. Am. Acad. Orthop. Surg. 1999, 7, 54–65. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Kanakaris, N.K.; Sante, E.D.; Morell, D.J.; Stengel, D.; Prevezas, N. Acetabular fractures with marginal impaction. Bone Jt. J. 2013, 95, 230–238. [Google Scholar] [CrossRef]
- Abo-Elsoud, M.; Kassem, E. Fragment-specific fixation of posterior wall acetabular fractures. Int. Orthop. (SICOT) 2021, 45, 3193–3199. [Google Scholar] [CrossRef]
- Kang, J.H.; Lee, S.H.; Lee, H.J. Usefulness of Spring Plate for Acetabular Posterior Wall Fracture Including Small Fragment. J. Korean Fract. Soc. 2016, 29, 19–25. [Google Scholar] [CrossRef]

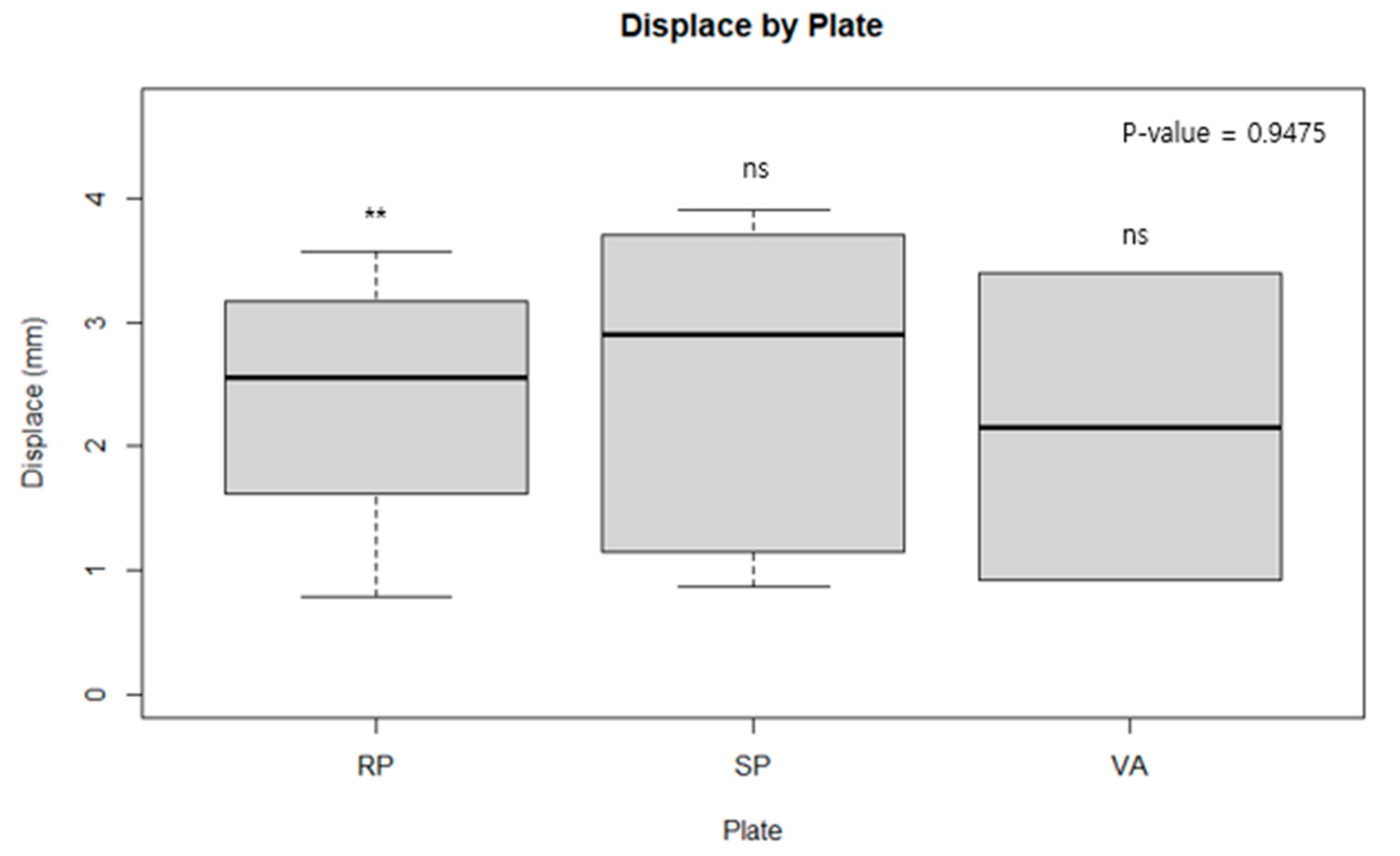

| Group | Mean (mm) | SD * | SEM † |
| RP ‡ | 2.37 | 1.04 | 0.42 |
| SP § | 2.51 | 1.42 | 0.63 |
| VA ∥ | 2.16 | 1.75 | 1.24 |
| Group vs. Group | p-value | 95% CI ¶ | |
| RP:SP | 0.87 | −1.93–1.67 | |
| RP:VA | 0.89 | −10.34–10.78 | |
| SP:VA | 0.83 | −7.47–8.18 | |
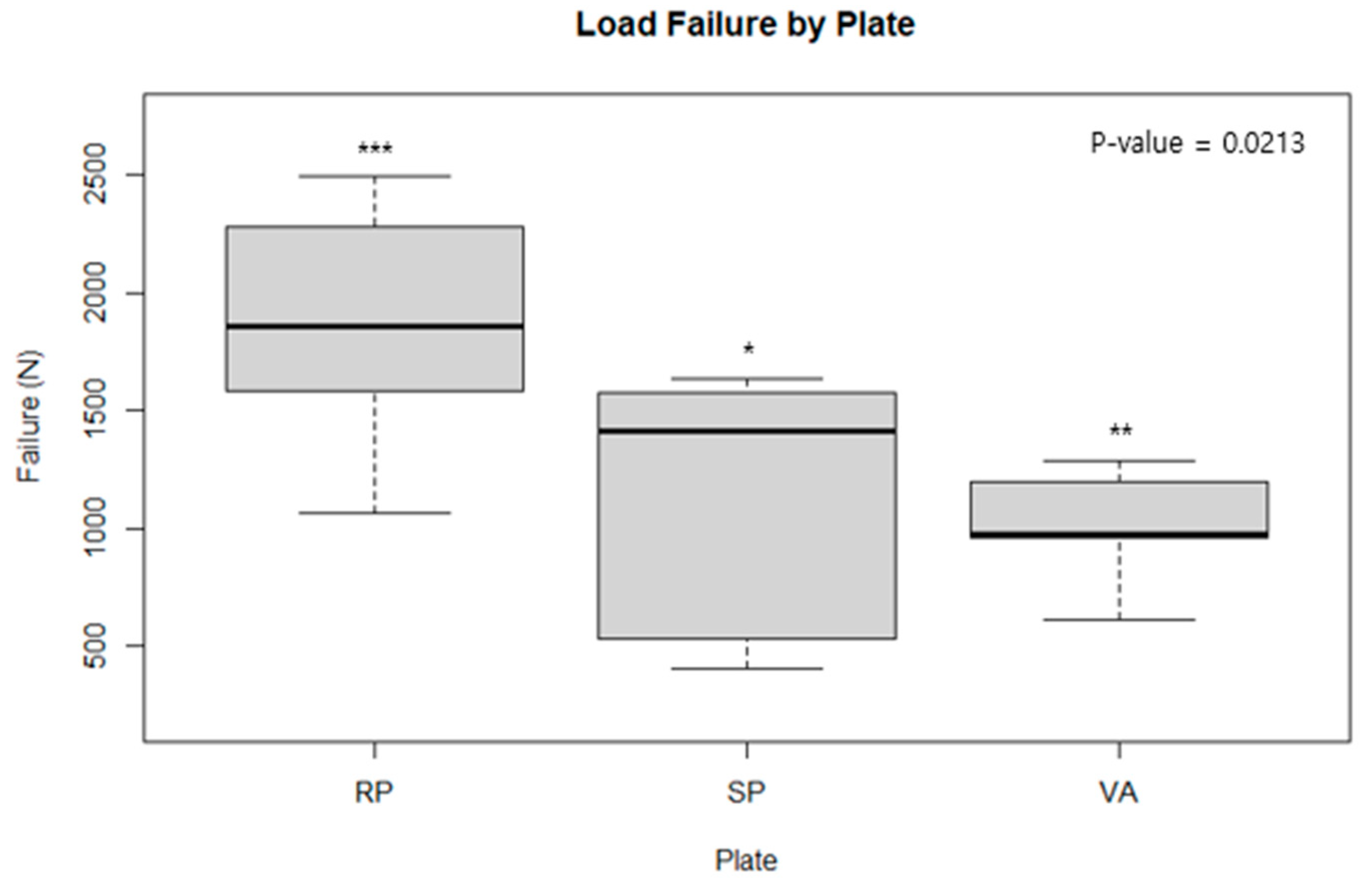
| Group | Mean (N) | SD * | SEM † |
| RP ‡ | 1855.47 | 509.43 | 207.93 |
| SP § | 1111.79 | 592.6 | 264.55 |
| VA ∥ | 1007.72 | 260.85 | 116.45 |
| Group vs. Group | p-value | 95% CI ¶ | |
| RP:SP | 0.05 | −32.96–1520.31 | |
| RP:VA | 0.01 | 293.98–1401.51 | |
| SP:VA | 0.73 | −620.57–828.72 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chung, H.; Sohn, H.-S.; Oh, J.-K.; Lee, S.; Kim, D. Biomechanical Comparison of Fixation Methods for Posterior Wall Fractures of the Acetabulum: Conventional Reconstruction Plate vs. Spring Plate vs. Variable Angle Locking Compression Plate. Medicina 2024, 60, 882. https://doi.org/10.3390/medicina60060882
Chung H, Sohn H-S, Oh J-K, Lee S, Kim D. Biomechanical Comparison of Fixation Methods for Posterior Wall Fractures of the Acetabulum: Conventional Reconstruction Plate vs. Spring Plate vs. Variable Angle Locking Compression Plate. Medicina. 2024; 60(6):882. https://doi.org/10.3390/medicina60060882
Chicago/Turabian StyleChung, HoeJeong, Hoon-Sang Sohn, Jong-Keon Oh, Sangho Lee, and DooSup Kim. 2024. "Biomechanical Comparison of Fixation Methods for Posterior Wall Fractures of the Acetabulum: Conventional Reconstruction Plate vs. Spring Plate vs. Variable Angle Locking Compression Plate" Medicina 60, no. 6: 882. https://doi.org/10.3390/medicina60060882
APA StyleChung, H., Sohn, H.-S., Oh, J.-K., Lee, S., & Kim, D. (2024). Biomechanical Comparison of Fixation Methods for Posterior Wall Fractures of the Acetabulum: Conventional Reconstruction Plate vs. Spring Plate vs. Variable Angle Locking Compression Plate. Medicina, 60(6), 882. https://doi.org/10.3390/medicina60060882






