The Modified Harrington Procedure for Metastatic Peri-Acetabular Bone Lesion Using a Novel Highly Porous Titanium Revision Shell with Long Lever Arm Screw
Abstract
1. Introduction
2. Materials and Methods
2.1. Implant Features
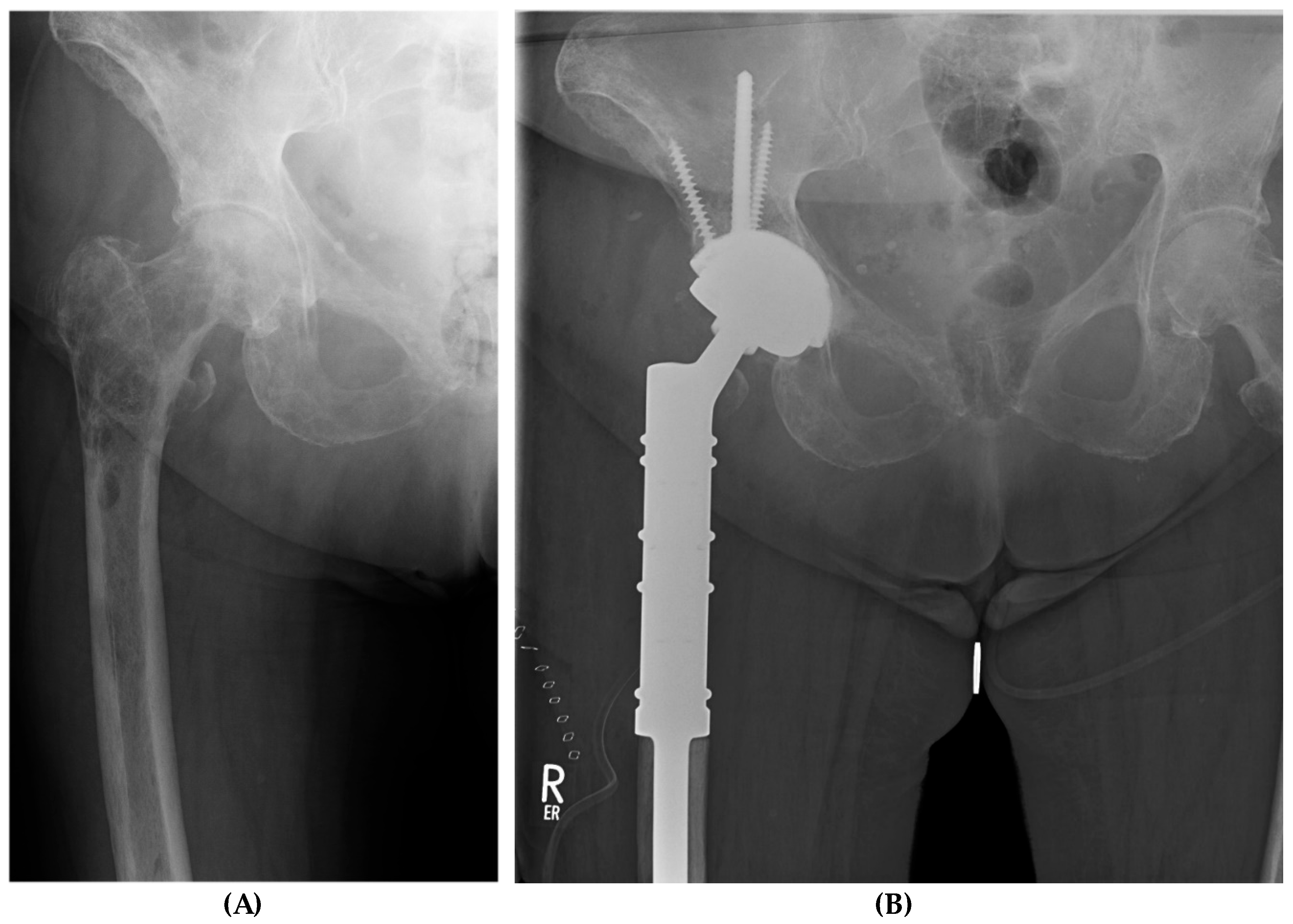
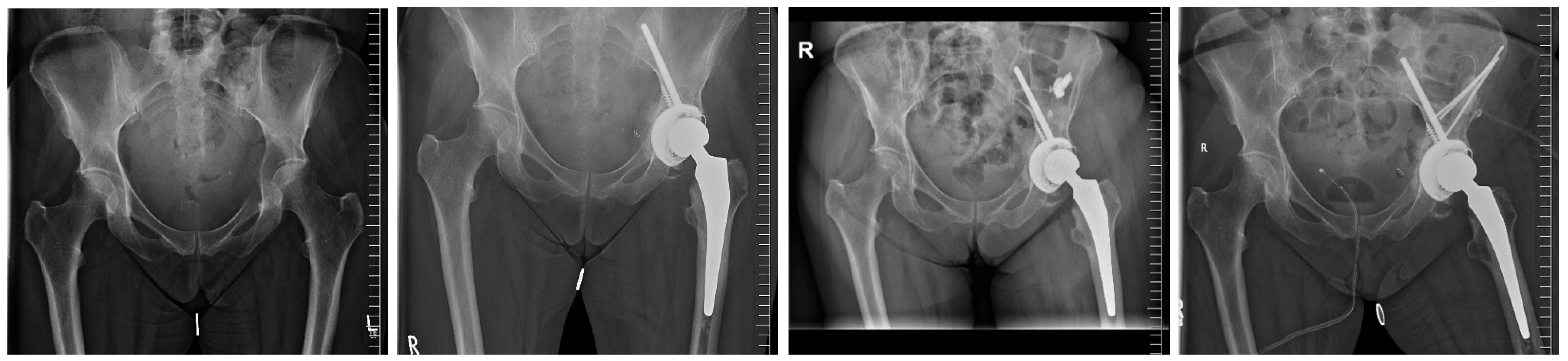
2.2. Surgical Procedure
2.3. Clinical and Radiographic Assessments
2.4. Complications
2.5. Statistical Analysis
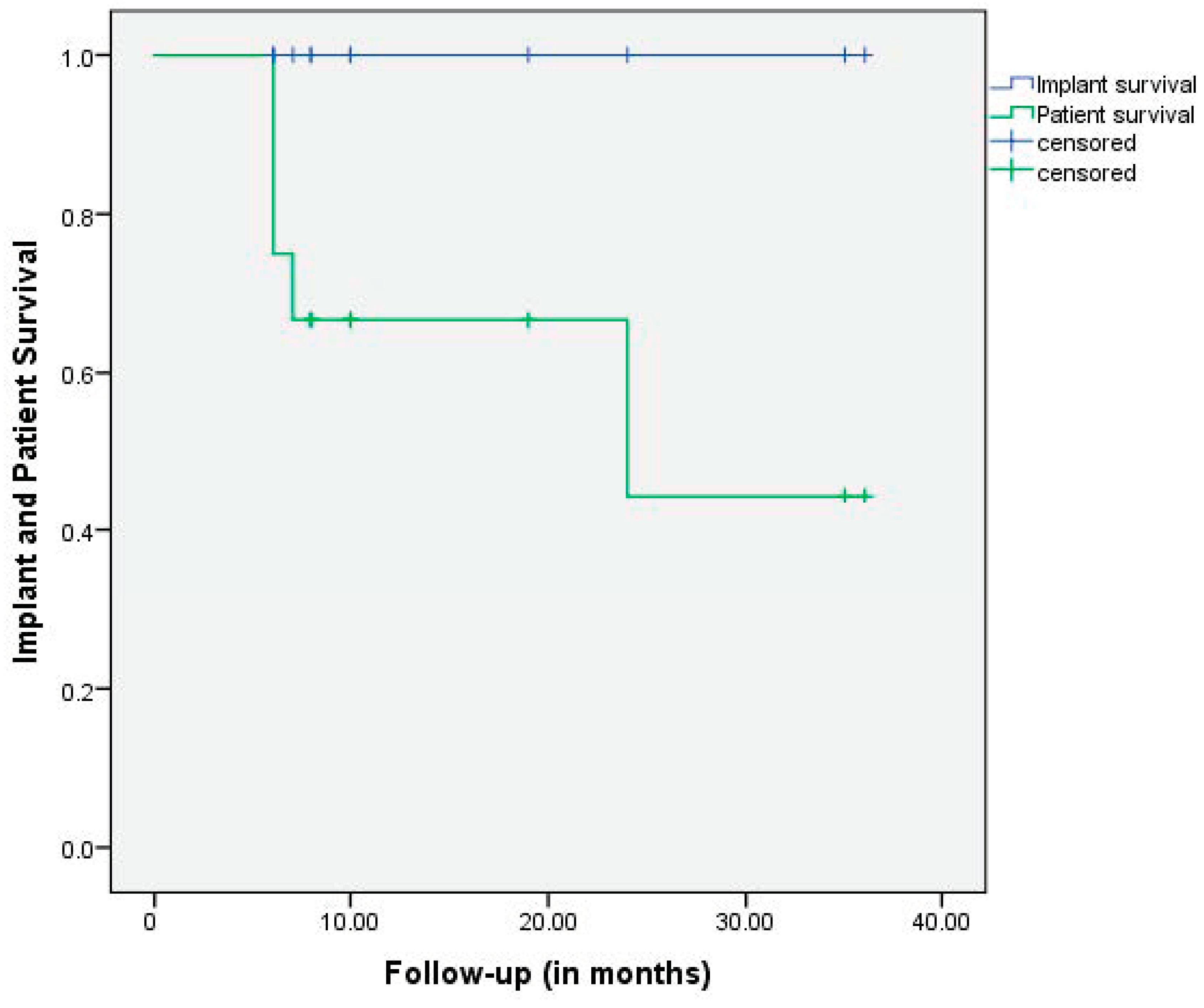
3. Results
3.1. Functional Analysis
3.2. Radiation Therapy
3.3. Implant-Related Findings
3.4. Complications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Papagelopoulos, P.J.; Galanis, E.C.; Savvidou, O.D.; Mavrogenis, A.F.; Jacofsky, D.J.; Frassica, F.J.; Sim, F.H. Advances and challenges in diagnosis and management of skeletal metastases. Orthopedics 2006, 29, 609–620, quiz 621–622. [Google Scholar] [CrossRef] [PubMed]
- Harrington, K.D. The management of acetabular insufficiency secondary to metastatic malignant disease. J. Bone Jt. Surg. Am. 1981, 63, 653–664. [Google Scholar] [CrossRef]
- Vielgut, I.; Sadoghi, P.; Gregori, M.; Kovar, F.M.; Pichler, K.; Maurer-Ertl, W.; Leithner, A. The modified Harrington procedure for metastatic peri-acetabular bone destruction. Int. Orthop. 2013, 37, 1981–1985. [Google Scholar] [CrossRef] [PubMed]
- Kask, G.; Nieminen, J.; van Iterson, V.; Naboistsikov, M.; Pakarinen, T.K.; Laitinen, M.K. Modified Harrington’s procedure for periacetabular metastases in 89 cases: A reliable method for cancer patients with good functional outcome, especially with long expected survival. Acta Orthop. 2020, 91, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Houdek, M.T.; Ferguson, P.C.; Abdel, M.P.; Griffin, A.M.; Hevesi, M.; Perry, K.I.; Rose, P.S.; Wunder, J.S.; Lewallen, D.G. Comparison of Porous Tantalum Acetabular Implants and Harrington Reconstruction for Metastatic Disease of the Acetabulum. J. Bone Jt. Surg. Am. 2020, 102, 1239–1247. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, J.; Gustafson, P.; Fornander, P.; Ornstein, E. The Harrington reconstruction for advanced periacetabular metastatic destruction: Good outcome in 32 patients. Acta Orthop. Scand. 2000, 71, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.S.; Salib, C.G.; Rose, P.S.; Sim, F.H.; Lewallen, D.G.; Abdel, M.P. Reconstruction of the hip after resection of periacetabular oncological lesions: A systematic review. Bone Jt. J. 2018, 100-b (Suppl. A), 22–30. [Google Scholar] [CrossRef] [PubMed]
- Renard, A.J.S.; Veth, R.P.H.; Schreuder, H.W.B.; Pruszczynski, M.; Keller, A.; van Hoesel, Q.; Bökkerink, J.P.M. The saddle prosthesis in pelvic primary and secondary musculoskeletal tumors: Functional results at several postoperative intervals. Arch. Orthop. Trauma Surg. 2000, 120, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, Y.; Ek, E.T.; Choong, P.F. Pelvic reconstruction using saddle prosthesis following limb salvage operation for periacetabular tumour. J. Orthop. Surg. 2006, 14, 155–162. [Google Scholar] [CrossRef]
- Marco, R.A.; Sheth, D.S.; Boland, P.J.; Wunder, J.S.; Siegel, J.A.; Healey, J.H. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J. Bone Jt. Surg. Am. 2000, 82, 642–651. [Google Scholar] [CrossRef]
- Kimura, T. Multidisciplinary Approach for Bone Metastasis: A Review. Cancers 2018, 10, 156. [Google Scholar] [CrossRef] [PubMed]
- Meneghini, R.M.; Ford, K.S.; McCollough, C.H.; Hanssen, A.D.; Lewallen, D.G. Bone remodeling around porous metal cementless acetabular components. J. Arthroplast. 2010, 25, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Meneghini, R.M.; Meyer, C.; Buckley, C.A.; Hanssen, A.D.; Lewallen, D.G. Mechanical stability of novel highly porous metal acetabular components in revision total hip arthroplasty. J. Arthroplast. 2010, 25, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Pardos, A.; García-Rey, E.; Fernandez-Fernández, R.; Ortega-Chamarro, J. Do trabecular metal cups achieve better results when compared to hemispherical porous titanium cups in acetabular revision surgery? HIP Int. 2021, 31, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Fairen, M.; Murcia, A.; Blanco, A.; Meroño, A.; Murcia, A., Jr.; Ballester, J. Revision of failed total hip arthroplasty acetabular cups to porous tantalum components: A 5-year follow-up study. J. Arthroplast. 2010, 25, 865–872. [Google Scholar] [CrossRef]
- Davies, J.H.; Laflamme, G.Y.; Delisle, J.; Fernandes, J. Trabecular metal used for major bone loss in acetabular hip revision. J. Arthroplast. 2011, 26, 1245–1250. [Google Scholar] [CrossRef]
- Jenkins, D.R.; Odland, A.N.; Sierra, R.J.; Hanssen, A.D.; Lewallen, D.G. Minimum Five-Year Outcomes with Porous Tantalum Acetabular Cup and Augment Construct in Complex Revision Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2017, 99, e49. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.A.; Rose, P.S.; Yanagisawa, M.; Lewallen, D.G.; Sim, F.H. Surgical technique: Porous tantalum reconstruction for destructive nonprimary periacetabular tumors. Clin. Orthop. Relat. Res. 2012, 470, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Abdel, M.P.; von Roth, P.; Perry, K.I.; Rose, P.S.; Lewallen, D.G.; Sim, F.H. Early Results of Acetabular Reconstruction After Wide Periacetabular Oncologic Resection. J. Bone Jt. Surg. Am. 2017, 99, e9. [Google Scholar] [CrossRef]
- Joglekar, S.B.; Rose, P.S.; Lewallen, D.G.; Sim, F.H. Tantalum acetabular cups provide secure fixation in THA after pelvic irradiation at minimum 5-year followup. Clin. Orthop. Relat. Res. 2012, 470, 3041–3047. [Google Scholar] [CrossRef]
- Zoccali, C.; Giannicola, G.; Zoccali, G.; Checcucci, E.; di Uccio, A.S.; Attala, D.; Villani, C. The iliac stemmed cup in reconstruction of the acetabular defects secondary to tumor resection: A systematic review of literature. Arch. Orthop. Trauma Surg. 2023, 143, 3659–3667. [Google Scholar] [CrossRef] [PubMed]
- Eisler, T.; Svensson, O.; Muren, C.; Elmstedt, E. Early loosening of the stemmed McMinn cup. J. Arthroplast. 2001, 16, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Tsagozis, P.; Wedin, R.; Brosjö, O.; Bauer, H. Reconstruction of metastatic acetabular defects using a modified Harrington procedure. Acta Orthop. 2015, 86, 690–694. [Google Scholar] [CrossRef] [PubMed]
- Shahid, M.; Saunders, T.; Jeys, L.; Grimer, R. The outcome of surgical treatment for peri-acetabular metastases. Bone Jt. J. 2014, 96-b, 132–136. [Google Scholar] [CrossRef]
| PRS® a | |
|---|---|
| n | 12 |
| Enrollment period | 2020–2023 |
| Follow-up b (in months) | 15 ± 11 [6–36] |
| Age b (in years) | 70 ± 8 [56–79] |
| Women (%) | 7 (58) |
| BMI b | 26 ± 4 [19–34] |
| ASA score c | 3 ± 1 [2–4] |
| Right joint; n (%) | 8 (67) |
| DOD d | 5/12 |
| HHS preoperatively e | 37 ± 22 [18–87] |
| HHS at latest follow-up e | 75 ± 15 [53–93] |
| Implant related findings | |
| Overall PRS implant size b (mm) | 56 ± 4 [52–68] |
| Tripolar acetabular systems; n (%) | 6 (50) |
| ->PRS® a implant size b (mm) | 60 ± 4 [56–68] |
| Cemented PE-Cup; n (%) | 6 (50) |
| ->PRS® a implant size b (mm) | 54 ± 2 [52–56] |
| Modular metal augments; n (%) | 2 (17) |
| Number of additional fixation screws b | 3 ± 1 [2–7] |
| Added screw lengths (mm) b | 161 ± 56 [100–290] |
| Lengths of 8 mm screw (mm) b | 90 ± 10 [70–100] |
| Added lengths of solely 6 mm screws (mm) b | 71 ± 56 [0–100] |
| Duration of surgery (minutes) b | 172 ± 34 [118–220] |
| Patient Number | Age (Years) | Primary Tumor | ASA a | Mobilization Preoperative | Mobilization at Latest FU b | Follow-Up (Months) | Patient Survival | Implant Survival (Yes/No) |
|---|---|---|---|---|---|---|---|---|
| #1 | 70 | Multiple myeloma | 3 | Two crutches | Unaided | 24 | DOD c | yes |
| #2 | 59 | Prostate cancer | 4 | Wheelchair | Cane | 7 | DOD c | yes |
| #3 | 76 | Breast cancer | 3 | Wheelchair | Two crutches | 6 | DOD c | yes |
| #4 | 73 | Non-Hodgkin lymphoma | 4 | Wheelchair | Cane | 35 | AWD d | yes |
| #5 | 82 | Breast cancer | 3 | Wheelchair | Two crutches | 6 | DOD c | yes |
| #6 | 74 | Breast cancer | 3 | Wheelchair | Unaided | 19 | AWD d | yes |
| #7 | 69 | Renal cell carcinoma | 3 | Two crutches | Two crutches | 6 | DOD c | yes |
| #8 | 56 | Bronchial cancer | 4 | Wheelchair | Two crutches | 10 | AWD d | yes |
| #9 | 60 | Bronchial cancer | 4 | Wheelchair | Walking frame | 8 | AWD d | yes |
| #10 | 79 | Prostate cancer | 3 | Two crutches | Cane | 10 | AWD d | yes |
| #11 | 66 | Breast cancer | 3 | Two crutches | Cane | 8 | AWD d | yes |
| #12 | 75 | Breast cancer | 2 | Wheelchair | Cane | 36 | AWD d | yes |
| Complications | Mechanical Failure | Dislocation | Local Progression of Tumor | Infection | Decubitus | Hematoma | Nerve Injuries | Impaired Soft Tissue | Ʃ |
|---|---|---|---|---|---|---|---|---|---|
| Major | 0 | 0 | 1 a | 0 | 0 | 0 | 0 | 1 | 2 |
| Minor | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 3 |
| Overall | 1 | 1 | 1 | 1 | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frieler, S.; Gebert, C.; Hanusrichter, Y.; Godolias, P.; Wessling, M. The Modified Harrington Procedure for Metastatic Peri-Acetabular Bone Lesion Using a Novel Highly Porous Titanium Revision Shell with Long Lever Arm Screw. Medicina 2024, 60, 1047. https://doi.org/10.3390/medicina60071047
Frieler S, Gebert C, Hanusrichter Y, Godolias P, Wessling M. The Modified Harrington Procedure for Metastatic Peri-Acetabular Bone Lesion Using a Novel Highly Porous Titanium Revision Shell with Long Lever Arm Screw. Medicina. 2024; 60(7):1047. https://doi.org/10.3390/medicina60071047
Chicago/Turabian StyleFrieler, Sven, Carsten Gebert, Yannik Hanusrichter, Periklis Godolias, and Martin Wessling. 2024. "The Modified Harrington Procedure for Metastatic Peri-Acetabular Bone Lesion Using a Novel Highly Porous Titanium Revision Shell with Long Lever Arm Screw" Medicina 60, no. 7: 1047. https://doi.org/10.3390/medicina60071047
APA StyleFrieler, S., Gebert, C., Hanusrichter, Y., Godolias, P., & Wessling, M. (2024). The Modified Harrington Procedure for Metastatic Peri-Acetabular Bone Lesion Using a Novel Highly Porous Titanium Revision Shell with Long Lever Arm Screw. Medicina, 60(7), 1047. https://doi.org/10.3390/medicina60071047






