Abstract
Background and Objectives: Knee osteoarthritis is a serious burden for modern countries. Timing of surgery and treatment choice are still a matter of controversy in the orthopedic literature. The purpose of this study was to ascertain the incidence and hospitalization trends of high tibial osteotomy in Italy from 2001 to 2016. Materials and Methods: Data are sourced from the National Hospital Discharge Reports (SDO) of the Italian Ministry of Health between 2001 and 2016. Results: A total of 34,402 high tibial osteotomies were performed over the study period in Italy. The cumulative incidence was 3.6 cases per 100,000 residents. The age classes 50–54, 55–59 showed the higher number of procedures. In pediatric patients (0–19 years), high tibial osteotomies are also largely performed. The majority of patients having surgery were men with a M/F ratio of 1.5. The mean age of patients was 44.2 ± 19.2 years. Males were significantly younger than females (43.3 ± 20.7 vs. 45.6 ± 17.7). The average length of hospitalization was 6.1 ± 7.3 days. Over the course of the analysis, a declining trend in hospital stay length was seen. The main primary diagnosis codes were “Varus knee” (736.42 ICD-9-CM code, 33.9%), “Osteoarthrosis, localized, primary, leg region” (715.16 ICD-9-CM code, 9.5%). Conclusions: Over the study period, high tibial osteotomies in Italy almost halved. Varus deformity and knee osteoarthritis are the leading causes requiring high tibial osteotomy. Except for the pediatric setting, results showed that from the 20–24 age class to the 50–54 age class, there was an increasing request for knee osteotomy, whereas in those aged >60 years, the incidence progressively decreased. The evident decline in HTO performed over the years in Italy seems to reflect a minor role for knee osteotomy in the management of knee OA, as it seems to be primarily reserved for younger male patients.
1. Introduction
Knee osteoarthritis (OA) is becoming extremely common in modern countries. Symptomatic OA of the knee affects 14 million patients in the USA, more than half of whom are under the age of 65 [1]. Tricompartmental knee OA is generally managed with total knee arthroplasty (TKA). However, tricompartmental arthritis is significantly less common than single compartmental disease (17% vs. 50%, respectively) [2].
Patients with unicompartmental knee OA who need surgical intervention have increased over time due to changes in demography and physical activity attitudes [3,4]. Treatment options for unicompartmental OA or osteonecrosis include tibial or femoral osteotomy and unicompartmental knee arthroplasty (UKA) [5,6,7,8,9]. In clinical practice, the patient’s age, level of physical activity, and severity of deformity play a role in the treatment choice [3,8,10,11,12]. The two procedures address pain relief by using different biomechanical principles. While keeping the other compartments’ native knee kinematics, UKA replaces the weight-bearing surface of a single osteoarthritic compartment [13]. Conversely, knee osteotomy, by changing joint surface alignment, underloads the chondropathic compartment and corrects the angular knee deformity that led to arthritis [14].
In general, osteotomies can be monoplanar or biplanar, opening-wedge or closing-wedge. Knee osteotomies can be divided into high tibial osteotomy (HTO) and distal femoral osteotomy (DFO). The most popular procedures worldwide are medial opening-wedge HTO for the treatment of varus knee deformity and lateral closing-wedge DFO for the treatment of valgus knee deformity [15].
Possible complications following HTO can be found intraoperatively or postoperatively and are divided into osteo-ligament, infectious, vascular–nervous, hardware-related, and malalignments [16,17,18,19]. Osteo-ligament complications include fractures, intra-articular or related to the osteotomy site (hinge fractures). The latter were classified by Takeuchi et al. into three types [20]. In type I, the fracture line is an extension of the osteotomy line and is proximal or at the height of the proximal tibiofibular joint. In type II, the fracture reaches the distal portion of the proximal tibiofibular joint. Type III corresponds to fractures of the lateral tibial plateau. Delayed union and pseudarthrosis of the osteotomy site are possible, especially in opening osteotomies. High or low patella and changes in the tibial slope (excess or defect) are other possible osteo-ligament complications. Infections can be divided into superficial, deep, related to the hardware or the bone graft. Vasculo-nervous complications include thromboembolic disease (deep vein thrombosis and pulmonary embolism), paralysis of the common peroneal nerve or its branches (in osteotomies involving the fibula or proximal tibiofibular joint), lesions of the popliteal or anterior tibial artery. Hardware-related complications include intolerance (discomfort) to the implanted device, loosening, breakage of the device or screws. Finally, malalignments, which can be assessed by calculating the mechanical axis on an x-ray of the lower limb under load, can be divided into loss of correction, overcorrection, and undercorrection.
When comparing knee osteotomy to UKA, the first showed improved postoperative ROM, higher rates of return to sports, bone stock preservation, and better functional outcomes [21]. In contrast, the latter is burdened by fewer complication rates than knee osteotomy, such as peroneal palsy, deep vein thrombosis, reduced postoperative pain, and lower revision rates [22].
Over time, the increasing popularity of TKA and UKA has led to a decline in the need for knee osteotomies in developed countries [23,24]. However, because of better functional results, symptomatic, physically demanding, young, and active patients with radiographical evidence of mild to moderate knee OA are still recognized as the ideal candidates for knee osteotomy [25,26,27].
Despite the abundance of literature regarding outcomes of knee osteotomies and knee arthroplasty, there are few studies dealing with the incidence trends of HTO over the years. This registry-based study’s aim was to evaluate the incidence of HTO carried out in Italy between 2001 and 2016.
2. Materials and Methods
2.1. Study Design and Selection of Study Participants
The National Hospital Discharge Records (SDO), an official database made available by the Italian Ministry of Health and encompassing data from all Italian private and public hospitals, served as the source for the analysis of the current study. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) is used to code diagnoses. The following main procedure code was used to define HTO: 77.87 ICD-9-CM code. Data about individual research subjects are accessible from 2001 to 2016. The patient’s gender, age, place of residence, hospitalization area, length of stay, primary diagnoses, and primary procedures are all included in these anonymized data. In order to determine the prevalence of HTO in Italy, population data from the National Institute for Statistics (ISTAT) were used for each year. Additionally, the incidence rates were stratified by year, age class, and gender. All patients included in the present study underwent an HTO even though the main procedure code was related to other knee procedures. Exclusion was applied when a diagnosis code associated with the HTO procedure was atypical and did not match with the 77.87 ICD-9-CM code.
2.2. Calculation Methodology
A series of descriptive statistical analyses was carried out by means of the R program (v4.4.1), a software environment for statistical computing and graphics.
2.3. Data Collection and Statistical Analysis
For categorical variables, frequency and percentage are provided; for continuous variables, means and standard deviations are provided. Incidence rates were calculated by dividing the number of annual cases by the size of the population, as reported each year by ISTAT, a legally required electronic national population registry.
3. Results
3.1. Demographics
From 2001 to 2016, 34,402 HTOs were performed in Italy, with a cumulative incidence of 3.6 cases per 100,000 residents. About 9.5% of patients required intervention for a trauma, and in 94.2% of cases, the intervention was the charge of the SSN.
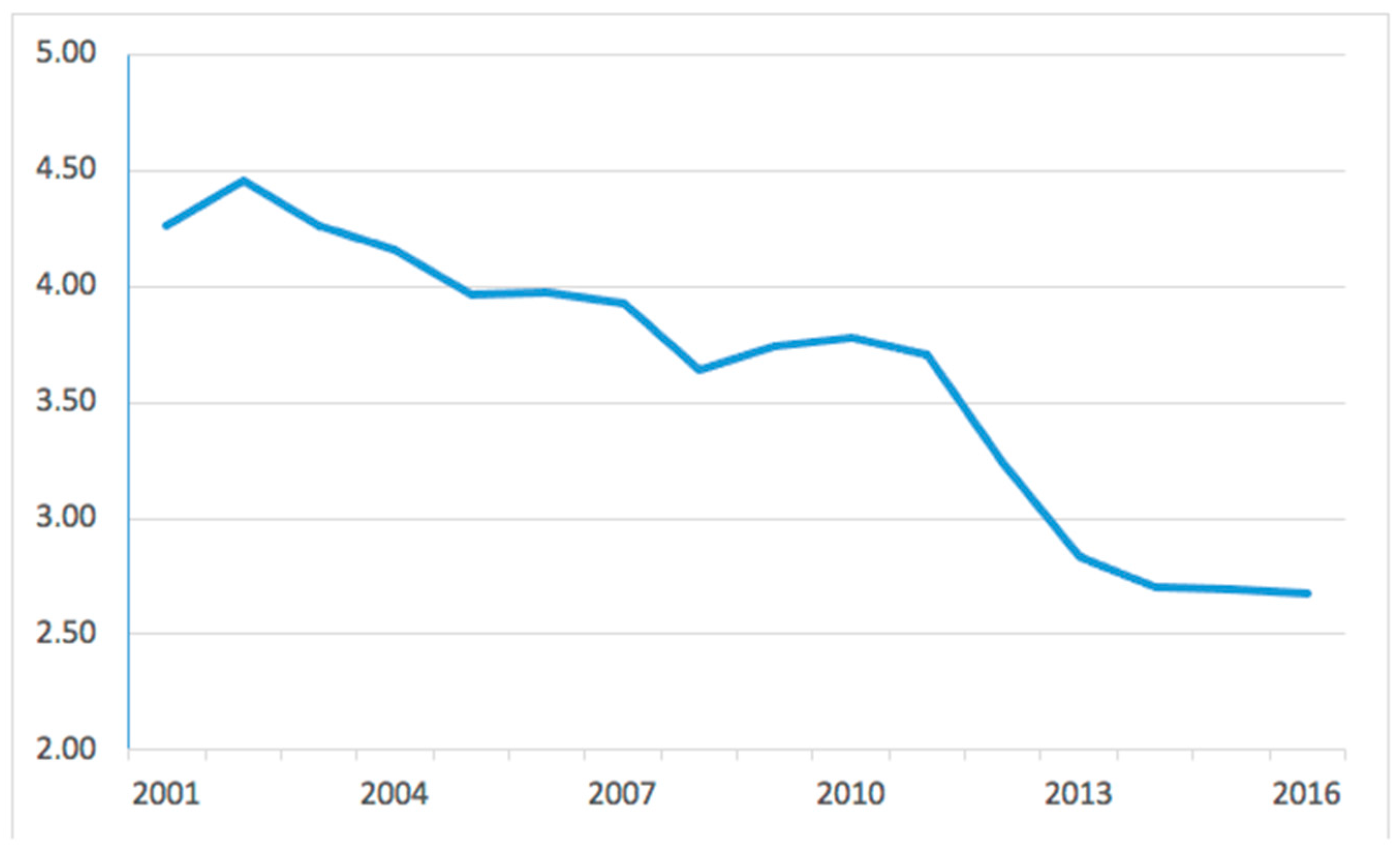
The incidence trend was decreasing, from a maximum of 4.5 in 2002 to a minimum of 2.7 cases per 100,000 residents in 2016 (Figure 1).
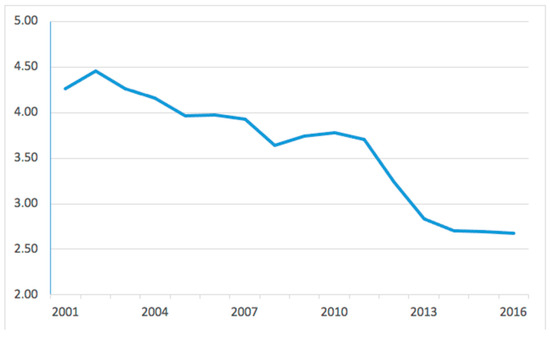
Figure 1.
Incidence of high tibial osteotomies per 100,000 residents from 2001 to 2016 in Italy.
The male/female ratio (M/F) was 1.5 and the mean age of patients was 44.2 ± 19.2 years. Males were significantly younger than females (43.3 ± 20.7 vs. 45.6 ± 17.7, respectively, p < 0.0001).
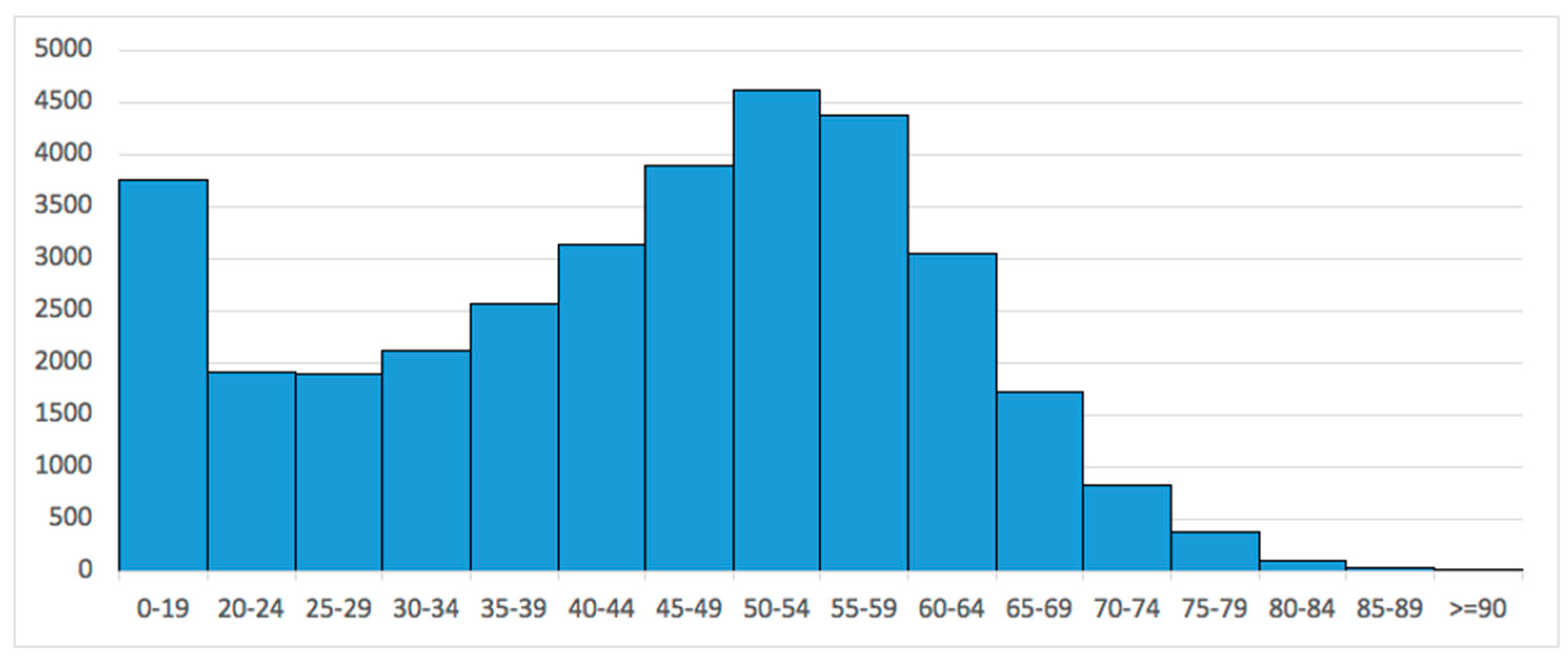
Stratifying by age groups, the 50–54-year-old (13.4%) and the 55–59-year-old (12.7%) age groups required HTO the most. Pediatric patients largely required HTO, with 10.9% of patients in the 0–19-year-old age group (Figure 2).
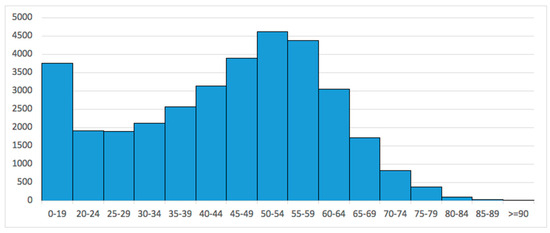
Figure 2.
Number of high tibial osteotomies performed in Italy from 2001 to 2016, stratified by age groups.
3.2. Length of the Hospitalization
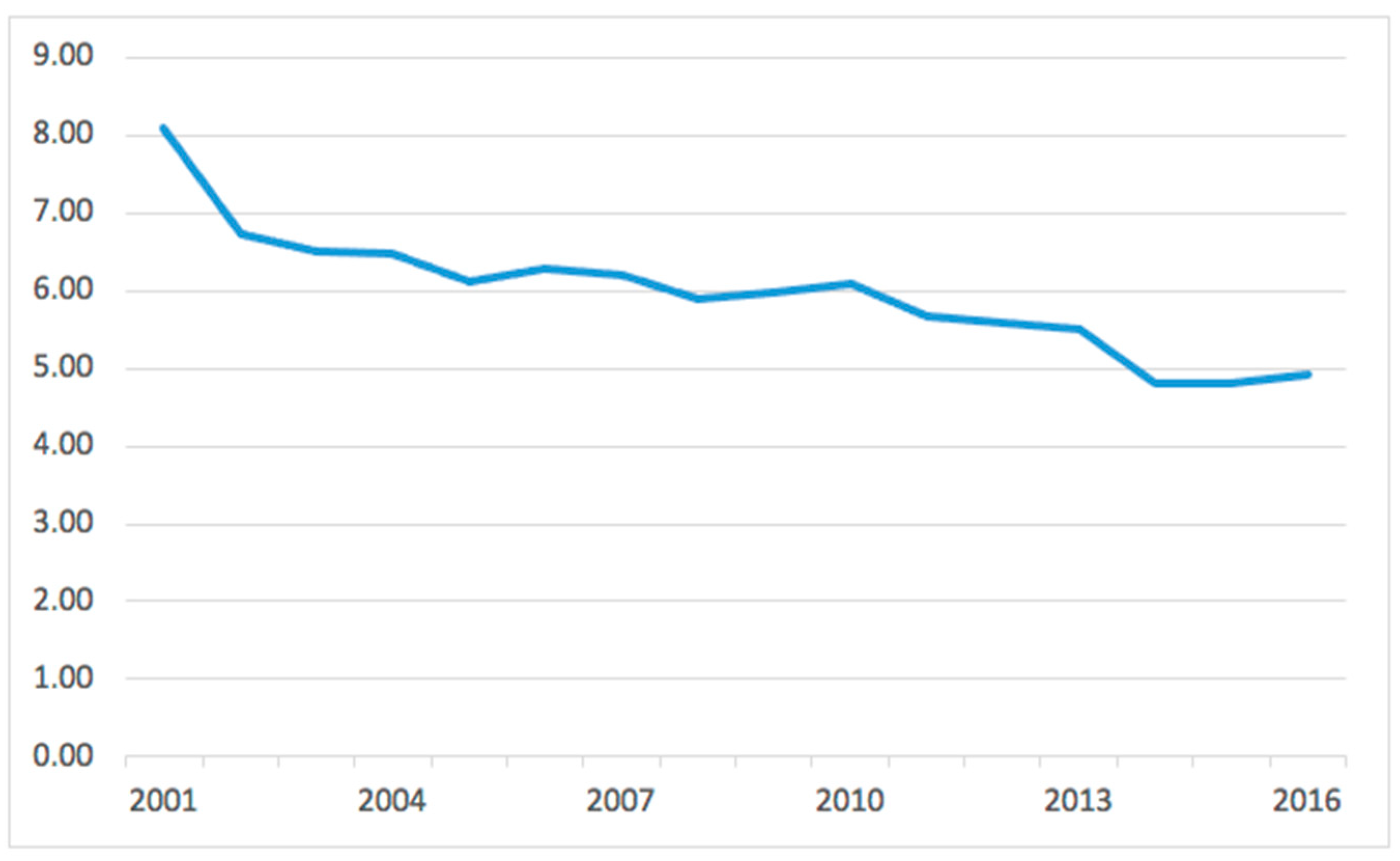
The average length of hospitalization was 6.1 ± 7.3 days, with a decreasing trend (from 8.1 ± 7.6 days in 2001 to 4.9 ± 6.6 days in 2016). Median values halved from 2001 to 2016, decreasing from 6 to 3 days of hospital stay (Figure 3).
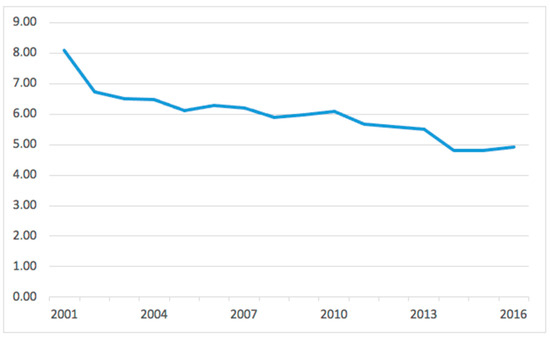
Figure 3.
Average days of hospitalization per year.
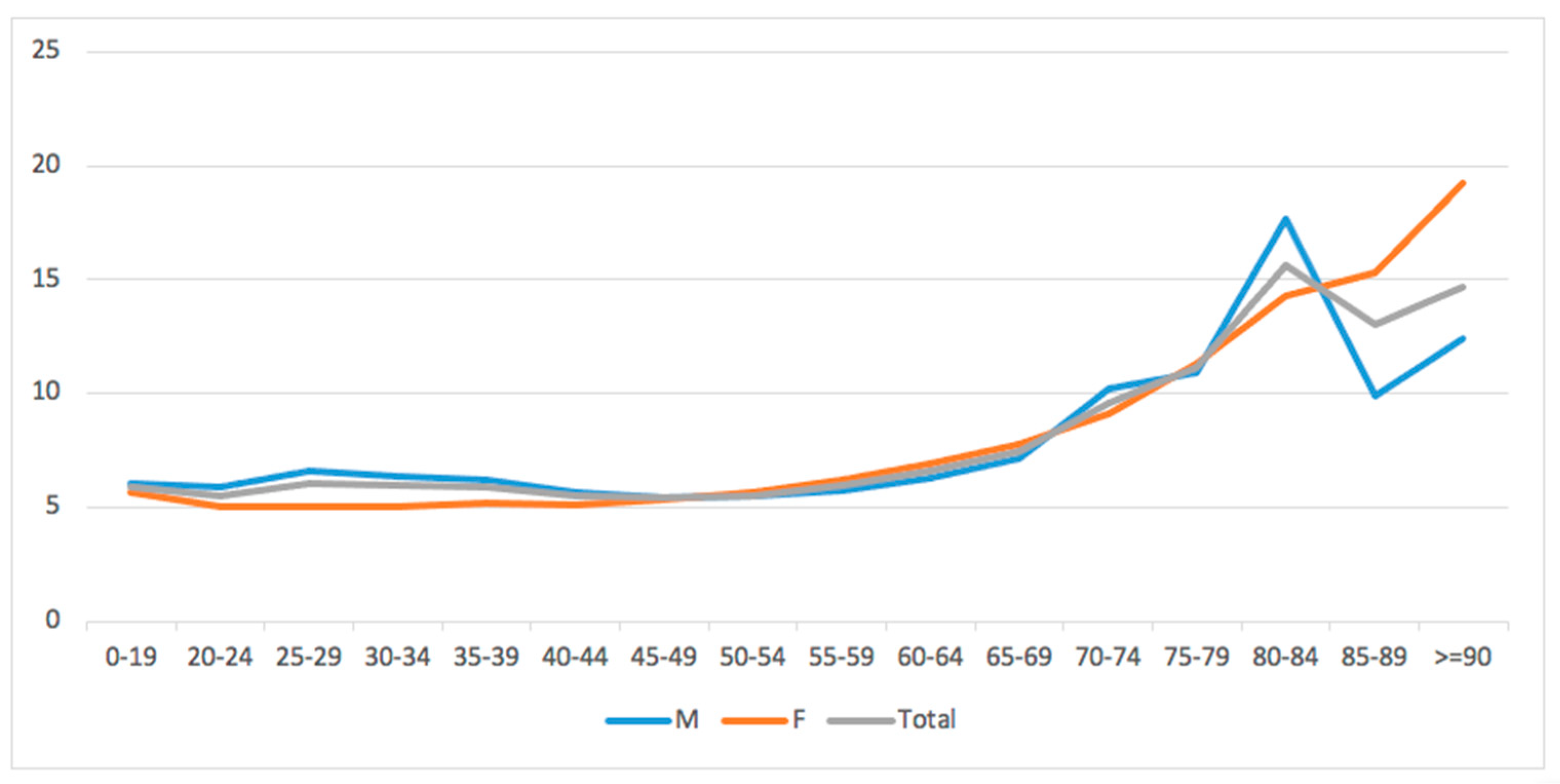
No gender differences were found, while older patients (>70 years) showed on average the highest length of hospital stay (p < 0.001) (Figure 4).
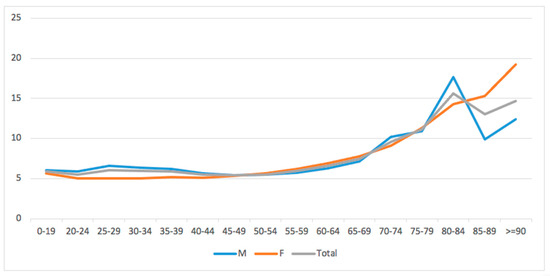
Figure 4.
Average days of hospitalization stratified by age groups and gender.
3.3. Main Primary Diagnoses
The main primary diagnoses codes were “Varus knee” (736.42 ICD-9-CM code, 33.9%), “Osteoarthrosis, localized, primary, leg region” (715.16 ICD-9-CM code, 9.5%), “Osteoarthrosis, localized, secondary, leg region” (715.26 ICD-9-CM code, 6.1%), “Valgus knee” (736.41 ICD-9-CM code, 5.4%), “Fracture” (733.82 ICD-9-CM code, 5.8%), “Trauma of the lower limbs” (905.4 ICD-9-CM code, 5.4%), “Chondromalacia” (717.7 ICD-9-CM code, 3.6%).
4. Discussion
The current study is the first to present national trends for HTO in the Italian population. An official national register was used to assess the number of surgical procedures carried out in Italian public and private hospitals over the study period. The main finding of the present study was the number of HTO performed in Italy per 100,000 person-years. A dramatic decrease in the incidence of knee osteotomy has been shown over the years, almost halving from 2001 to 2016.
Regarding recent decades, many authors have reported similar decreasing trends of HTO in Western countries [28,29,30,31]. A 22-year Finnish population-based study reported a slight increase in incidence of knee osteotomies in patients <50 years, still confirming a general decline in the overall incidence of knee osteotomies [30]. Conversely, in Eastern countries, an opposite trend was observed. A Korean study reported an increase in HTO by 210% from 2009 to 2013, especially in patients aged from 55 to 64 years; a Japanese study reported an increase in HTO from 2.6% in 2007 to 5.5% in 2014. The improvement in TKA outcomes over recent decades and the evidence that UKAs have been used to treat individuals with less severe forms of arthritis may be the cause of the reduced need for osteotomies worldwide [32]. However, further studies are needed to investigate these continental variations in knee surgery preferences, taking into account the well-known specific features of knee anatomy in Asian people [33,34,35,36].
The present study showed that Italian males more frequently undergo HTO. Moreover, males are on average younger than females when undergoing surgery. Many orthopedic diseases have shown a gender prevalence [37,38,39,40,41,42]; varus deformity, with consequent medial compartment OA, is typically more common in men [43,44] and it may justify the M/F discrepancy in Italian patients requiring HTO. Furthermore, female gender was found to be an independent risk factor for failure in a 2019 study by Keenan et al. that examined 111 HTO patients with an average follow-up length of 12 years [45].
The age-specific subanalysis of patients included in the present study revealed that HTO is largely performed in pediatric patients (0–19 years of age class). The most common cause of genu varum requiring HTO in the pediatric setting is Blount disease; patients typically present in their second decade of life with severe genu varum, procurvatum, and internal tibial torsion [46,47]. Standard management for “adolescent tibia vara” (Blount disease) is proximal tibial osteotomy with or without associated fibular osteotomy [48,49,50,51]. However, recurrence of varus deformity after HTO in Blount disease has been described [52,53].
Data showed that from the age class of 20–24 years to the age class of 50–54 years, there were increasing requests for HTO in the Italian population. In those aged >60 years, the incidence of knee osteotomy progressively decreased. These results are in line with the current literature. An epidemiological analysis in Japan showed more requests for tibial osteotomy in patients <55 years, whereas UKA seemed to be preferred in patients >55 years [54]; in Korea, the largest increase in incidence of HTO and UKA was observed in the 55–64-year-old age group, with TKA becoming predominant in patients >75 years [55]. These trends, similar among countries, may have been influenced by reports suggesting that HTO is more appropriate for younger and active patients, whereas UKA is preferrable in elderly patients with lower activity levels [10,12,31]. It seems evident from the literature reported and from results of the present study that knee osteotomy plays a role in delaying knee OA progression, whereas knee arthroplasty represents the final option for osteoarthritic knees.
From 2001 to 2016, a trend toward shorter hospital stays for HTO procedures was seen. Hospitals frequently reduce duration of stay over time for economic reasons, which most likely explains the disparity. However, this claim is unsupported by any evidence.
The analysis of the primary diagnosis codes revealed a clear predominance of varus knee deformity and knee osteoarthritis as the leading causes requiring HTO in the Italian population. Accordingly, although valgus knee can also be managed with medial closing-wedge HTO, it is extremely more common to perform a lateral closing-wedge DFO. It is known that varus alignment may determine medial compartment knee osteoarthritis, and a correction osteotomy may interfere with this pathologic process [56,57]. Timing of surgery and treatment choice, particularly HTO vs. UKA, are still a matter of controversy in the orthopedic literature.
Noteworthy is that, when conducting epidemiologic studies on trends for consecutive years, it should always be taken into account that possible emergency situations may influence the incidence and hospitalization rates of orthopedic interventions. Moldovan et al. showed that the COVID-19 pandemic severely affected the volume of hip and knee arthroplasty in Romania, with unfavorable financial implications [58]. For this reason, it is important to continually collect clinical data and analyze how trends vary under the influence of external factors [58].
The study presents a list of limitations. First of all, the ICD-9-CM is the source for all reported diagnoses and procedures, based on administrative data from various hospitals and areas. Finding incorrect diagnoses or coding errors might be challenging given the large number of hospitals involved. In order to mitigate potential errors, we have stated our inclusion and exclusion criteria. The fact that hospitalizations in Italy’s healthcare system are anonymous and patients are not issued a unique ID number means that there are no outcome scores in this study. In other words, patients who had many procedures may have been counted more than once. Third, because ICD-9 classification was performed by surgeons, there can be variations between observers.
5. Conclusions
Overall, 34,402 HTOs were performed over the study period in Italy. The incidence of knee osteotomy over the years has almost halved from 2001 to 2016. Interestingly, HTO is largely performed in pediatric patients in order to correct alignment deformities. In line with the literature, results showed that from the 20–24-year-old age class to the 50–54-year-old age class, there were increasing requests for HTO, whereas in those aged >60 years, the incidence of knee osteotomy progressively decreased. As expected, varus deformity and knee osteoarthtitis were the leading diagnoses managed with HTO. The evident decline in HTO performed over the years in Italy seems to reflect a minor role for knee osteotomy in the management of knee OA, as it seems to be primarily reserved for younger male patients. Further studies are necessary in order to define the best standards of care for knee OA and the future of knee osteotomies. Moreover, it is important to continually collect clinical data and analyze how trends vary under the influence of external factors.
Author Contributions
Conceptualization, U.G.L. and S.C.; methodology, A.M.; software, G.S. and V.C.; validation, A.M., C.C. and D.G.; formal analysis, M.D.; investigation, A.M.; resources, A.M.; data curation, S.C.; writing—original draft preparation, C.C.; writing—review and editing, V.C.; visualization, G.S.; supervision, R.P.; project administration, U.G.L.; funding acquisition, U.G.L. and R.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of The Declaration of Helsinki. The Institutional Review Board of Campus Bio-Medico University of Rome ruled that no formal ethics approval was required in this particular case. The access to the database is on request. All data were obtained by the Direzione Generale della Programmazione Sanitaria—Banca Dati SDO of the Italian Ministry of Health.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The access to the database is on request. All data were obtained by the Direzione Generale della Programmazione Sanitaria—Banca Dati SDO of the Italian Ministry of Health.
Acknowledgments
We thank the Direzione Generale della Programmazione Sanitaria—Banca Dati SDO of the Italian Ministry of Health for the support in providing data for this research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Deshpande, B.R.; Katz, J.N.; Solomon, D.H.; Yelin, E.H.; Hunter, D.J.; Messier, S.P.; Suter, L.G.; Losina, E. Number of Persons with Symptomatic Knee Osteoarthritis in the US: Impact of Race and Ethnicity, Age, Sex, and Obesity. Arthritis Care Res. 2016, 68, 1743–1750. [Google Scholar] [CrossRef]
- Stoddart, J.C.; Dandridge, O.; Garner, A.; Cobb, J.; van Arkel, R.J. The compartmental distribution of knee osteoarthritis—A systematic review and meta-analysis. Osteoarthr. Cartil. 2021, 29, 445–455. [Google Scholar] [CrossRef]
- Gomoll, A.H. High tibial osteotomy for the treatment of unicompartmental knee osteoarthritis: A review of the literature, indications, and technique. Phys. Sportsmed. 2011, 39, 45–54. [Google Scholar] [CrossRef]
- Gomoll, A.H.; Farr, J.; Gillogly, S.D.; Kercher, J.S.; Minas, T. Surgical management of articular cartilage defects of the knee. Instr. Course Lect. 2011, 60, 461–483. [Google Scholar]
- Akizuki, S.; Shibakawa, A.; Takizawa, T.; Yamazaki, I.; Horiuchi, H. The long-term outcome of high tibial osteotomy: A ten- to 20-year follow-up. J. Bone Jt. Surg. Br. 2008, 90, 592–596. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.J.; Robertsson, O.; Graves, S.; Price, A.J.; Arden, N.K.; Judge, A.; Beard, D.J. Knee replacement. Lancet 2012, 379, 1331–1340. [Google Scholar] [CrossRef]
- Franceschi, F.; Longo, U.G.; Ruzzini, L.; Marinozzi, A.; Maffulli, N.; Denaro, V. Simultaneous arthroscopic implantation of autologous chondrocytes and high tibial osteotomy for tibial chondral defects in the varus knee. Knee 2008, 15, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Lyons, M.C.; MacDonald, S.J.; Somerville, L.E.; Naudie, D.D.; McCalden, R.W. Unicompartmental versus total knee arthroplasty database analysis: Is there a winner? Clin. Orthop. Relat. Res. 2012, 470, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.G.; Cui, Q.; Kuskowski, M.; Mihalko, W.M.; Saleh, K.J. Outcomes of total and unicompartmental knee arthroplasty for secondary and spontaneous osteonecrosis of the knee. J. Bone Jt. Surg. Am. 2006, 88 (Suppl. 3), 76–82. [Google Scholar]
- Fu, D.; Li, G.; Chen, K.; Zhao, Y.; Hua, Y.; Cai, Z. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis: A meta-analysis. J. Arthroplast. 2013, 28, 759–765. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Gougoulias, N.; Caine, D.; Denaro, V. Sport injuries: A review of outcomes. Br. Med. Bull. 2011, 97, 47–80. [Google Scholar] [CrossRef] [PubMed]
- Spahn, G.; Hofmann, G.O.; von Engelhardt, L.V.; Li, M.; Neubauer, H.; Klinger, H.M. The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 96–112. [Google Scholar] [CrossRef]
- Borus, T.; Thornhill, T. Unicompartmental knee arthroplasty. J. Am. Acad. Orthop. Surg. 2008, 16, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.C.; Byun, S.J. High tibial osteotomy. Knee Surg. Relat. Res. 2012, 24, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Vena, G.; D’Adamio, S.; Amendola, A. Complications of osteotomies about the knee. Sports Med. Arthrosc. Rev. 2013, 21, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.; Birmingham, T.B.; Willits, K.; Litchfield, R.; Lebel, M.E.; Giffin, J.R. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am. J. Sports Med. 2014, 42, 1118–1126. [Google Scholar] [CrossRef] [PubMed]
- Miltenberg, B.; Puzzitiello, R.N.; Ruelos, V.C.B.; Masood, R.; Pagani, N.R.; Moverman, M.A.; Menendez, M.E.; Ryan, S.P.; Salzler, M.J.; Drager, J. Incidence of Complications and Revision Surgery After High Tibial Osteotomy: A Systematic Review. Am. J. Sports Med. 2024, 52, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Valkering, K.P.; van den Bekerom, M.P.; Kappelhoff, F.M.; Albers, G.H. Complications after tomofix medial opening wedge high tibial osteotomy. J. Knee Surg. 2009, 22, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Woodacre, T.; Ricketts, M.; Evans, J.T.; Pavlou, G.; Schranz, P.; Hockings, M.; Toms, A. Complications associated with opening wedge high tibial osteotomy—A review of the literature and of 15 years of experience. Knee 2016, 23, 276–282. [Google Scholar] [CrossRef]
- Takeuchi, R.; Ishikawa, H.; Kumagai, K.; Yamaguchi, Y.; Chiba, N.; Akamatsu, Y.; Saito, T. Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: A new classification of lateral hinge fracture. Arthroscopy 2012, 28, 85–94. [Google Scholar] [CrossRef]
- Belsey, J.; Yasen, S.K.; Jobson, S.; Faulkner, J.; Wilson, A.J. Return to Physical Activity After High Tibial Osteotomy or Unicompartmental Knee Arthroplasty: A Systematic Review and Pooling Data Analysis. Am. J. Sports Med. 2021, 49, 1372–1380. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Mai, X.; Wang, J.; Feng, E.; Huang, Y. Unicompartmental Knee Arthroplasty vs High Tibial Osteotomy for Knee Osteoarthritis: A Systematic Review and Meta-Analysis. J. Arthroplast. 2018, 33, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Koskinen, E.; Paavolainen, P.; Eskelinen, A.; Pulkkinen, P.; Remes, V. Unicondylar knee replacement for primary osteoarthritis: A prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007, 78, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.; Mowat, F.; Ong, K.; Chan, N.; Lau, E.; Halpern, M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J. Bone Jt. Surg. Am. 2005, 87, 1487–1497. [Google Scholar]
- Amendola, A.; Bonasia, D.E. Results of high tibial osteotomy: Review of the literature. Int. Orthop. 2010, 34, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Wolcott, M.; Traub, S.; Efird, C. High tibial osteotomies in the young active patient. Int. Orthop. 2010, 34, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.M.; Crockett, H.C.; Slawski, D.P.; Madsen, M.W.; Windsor, R.E. High tibial osteotomy. J. Am. Acad. Orthop. Surg. 2005, 13, 279–289. [Google Scholar] [CrossRef] [PubMed]
- Culliford, D.; Maskell, J.; Judge, A.; Cooper, C.; Prieto-Alhambra, D.; Arden, N.K.; COASt Study Group. Future projections of total hip and knee arthroplasty in the UK: Results from the UK Clinical Practice Research Datalink. Osteoarthr. Cartil. 2015, 23, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Culliford, D.J.; Maskell, J.; Beard, D.J.; Murray, D.W.; Price, A.J.; Arden, N.K. Temporal trends in hip and knee replacement in the United Kingdom: 1991 to 2006. J. Bone Jt. Surg. Br. 2010, 92, 130–135. [Google Scholar] [CrossRef]
- Niinimäki, T.T.; Eskelinen, A.; Ohtonen, P.; Junnila, M.; Leppilahti, J. Incidence of osteotomies around the knee for the treatment of knee osteoarthritis: A 22-year population-based study. Int. Orthop. 2012, 36, 1399–1402. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; McCormick, F.M.; Schairer, W.W.; Frank, R.M.; Provencher, M.T.; Roche, M.W. Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. J. Arthroplast. 2014, 29, 1586–1589. [Google Scholar] [CrossRef] [PubMed]
- Niinimäki, T.T.; Murray, D.W.; Partanen, J.; Pajala, A.; Leppilahti, J.I. Unicompartmental knee arthroplasties implanted for osteoarthritis with partial loss of joint space have high re-operation rates. Knee 2011, 18, 432–435. [Google Scholar] [CrossRef] [PubMed]
- Han, H.S.; Kang, S.B. Brief followup report: Does high-flexion total knee arthroplasty allow deep flexion safely in Asian patients? Clin. Orthop. Relat. Res. 2013, 471, 1492–1497. [Google Scholar] [CrossRef]
- Lasam, M.P.; Lee, K.J.; Chang, C.B.; Kang, Y.G.; Kim, T.K. Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin. Orthop. Relat. Res. 2013, 471, 1472–1483. [Google Scholar] [CrossRef] [PubMed]
- Mullaji, A.B.; Marawar, S.V.; Mittal, V. A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J. Arthroplast. 2009, 24, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Yau, W.P.; Chiu, K.Y.; Tang, W.M.; Ng, T.P. Coronal bowing of the femur and tibia in Chinese: Its incidence and effects on total knee arthroplasty planning. J. Orthop. Surg. 2007, 15, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.Y.; Smith, C.L.; Zhang, X.; Hsu, H.C.; Wang, D.Y.; Luo, Z.P. Tensile forces attenuate estrogen-stimulated collagen synthesis in the ACL. Biochem. Biophys. Res. Commun. 2004, 317, 1221–1225. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Mazzola, A.; Carotti, S.; Francesconi, M.; Catapano, S.; Magrì, F.; Perrone, G.; Morini, S.; De Salvatore, S.; Denaro, V. The role of estrogen and progesterone receptors in the rotator cuff disease: A retrospective cohort study. BMC Musculoskelet. Disord. 2021, 22, 891. [Google Scholar] [CrossRef]
- Longo, U.G.; Mazzola, A.; Magrì, F.; Catapano, S.; De Salvatore, S.; Carotti, S.; Denaro, V. Histological, radiological and clinical analysis of the supraspinatus tendon and muscle in rotator cuff tears. BMC Musculoskelet. Disord. 2023, 24, 127. [Google Scholar] [CrossRef]
- Shen, P.C.; Wang, P.H.; Wu, P.T.; Wu, K.C.; Hsieh, J.L.; Jou, I.M. The Estrogen Receptor-β Expression in De Quervain’s Disease. Int. J. Mol. Sci. 2015, 16, 26452–26462. [Google Scholar] [CrossRef]
- Toesca, A.; Pagnotta, A.; Zumbo, A.; Sadun, R. Estrogen and progesterone receptors in carpal tunnel syndrome. Cell Biol. Int. 2008, 32, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.D.; Panossian, V.; Hatch, J.D.; Liu, S.H.; Finerman, G.A. Combined effects of estrogen and progesterone on the anterior cruciate ligament. Clin. Orthop. Relat. Res. 2001, 383, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Bellemans, J.; Colyn, W.; Vandenneucker, H.; Victor, J. The Chitranjan Ranawat award: Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin. Orthop. Relat. Res. 2012, 470, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Vandekerckhove, P.T.K.; Matlovich, N.; Teeter, M.G.; MacDonald, S.J.; Howard, J.L.; Lanting, B.A. The relationship between constitutional alignment and varus osteoarthritis of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2873–2879. [Google Scholar] [CrossRef] [PubMed]
- Keenan, O.J.F.; Clement, N.D.; Nutton, R.; Keating, J.F. Older age and female gender are independent predictors of early conversion to total knee arthroplasty after high tibial osteotomy. Knee 2019, 26, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Janoyer, M. Blount disease. Orthop. Traumatol. Surg. Res. 2019, 105, S111–S121. [Google Scholar] [CrossRef] [PubMed]
- Sachs, O.; Katzman, A.; Abu-Johar, E.; Eidelman, M. Treatment of Adolescent Blount Disease Using Taylor Spatial Frame with and Without Fibular Osteotomy: Is There any Difference? J. Pediatr. Orthop. 2015, 35, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Feldman, D.S.; Madan, S.S.; Koval, K.J.; van Bosse, H.J.; Bazzi, J.; Lehman, W.B. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J. Pediatr. Orthop. 2003, 23, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Spencer, S.A.; Hedequist, D. Proximal tibial osteotomy and Taylor Spatial Frame application for correction of tibia vara in morbidly obese adolescents. J. Pediatr. Orthop. 2013, 33, 276–281. [Google Scholar] [CrossRef]
- Paloski, M.; Taylor, B.C.; Iobst, C.; Pugh, K.J. Pediatric and adolescent applications of the Taylor Spatial Frame. Orthopedics 2012, 35, 518–527. [Google Scholar] [CrossRef][Green Version]
- Price, C.T.; Scott, D.S.; Greenberg, D.A. Dynamic axial external fixation in the surgical treatment of tibia vara. J. Pediatr. Orthop. 1995, 15, 236–243. [Google Scholar] [CrossRef]
- Chotigavanichaya, C.; Salinas, G.; Green, T.; Moseley, C.F.; Otsuka, N.Y. Recurrence of varus deformity after proximal tibial osteotomy in Blount disease: Long-term follow-up. J. Pediatr. Orthop. 2002, 22, 638–641. [Google Scholar] [CrossRef] [PubMed]
- Gonzàlez-Herranz, P. Recurrence of varus deformity after proximal tibial osteotomy in Blount disease: Long-term follow-up. J. Pediatr. Orthop. 2005, 25, 130. [Google Scholar] [CrossRef] [PubMed]
- Kawata, M.; Sasabuchi, Y.; Inui, H.; Taketomi, S.; Matsui, H.; Fushimi, K.; Chikuda, H.; Yasunaga, H.; Tanaka, S. Annual trends in knee arthroplasty and tibial osteotomy: Analysis of a national database in Japan. Knee 2017, 24, 1198–1205. [Google Scholar] [CrossRef]
- Koh, I.J.; Kim, M.W.; Kim, J.H.; Han, S.Y.; In, Y. Trends in High Tibial Osteotomy and Knee Arthroplasty Utilizations and Demographics in Korea from 2009 to 2013. J. Arthroplast. 2015, 30, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, G.M.; van Tol, A.W.; Bergink, A.P.; Belo, J.N.; Bernsen, R.M.; Reijman, M.; Pols, H.A.P.; Bierma-Zeinstra, S.M.A. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007, 56, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Sharma, L.; Song, J.; Dunlop, D.; Felson, D.; Lewis, C.E.; Segal, N.; Torner, J.; Cooke, T.D.V.; Hietpas, J.; Lynch, J.; et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann. Rheum. Dis. 2010, 69, 1940–1945. [Google Scholar] [CrossRef]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. An Investigation for Future Practice of Elective Hip and Knee Arthroplasties during COVID-19 in Romania. Medicina 2023, 59, 314. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).