Post-Mastectomy Breast Reconstruction Disparities: A Systematic Review of Sociodemographic and Economic Barriers
Abstract
:1. Introduction
2. Methods
2.1. Research Design
2.2. Search Term Definitions
2.3. Selection Criteria
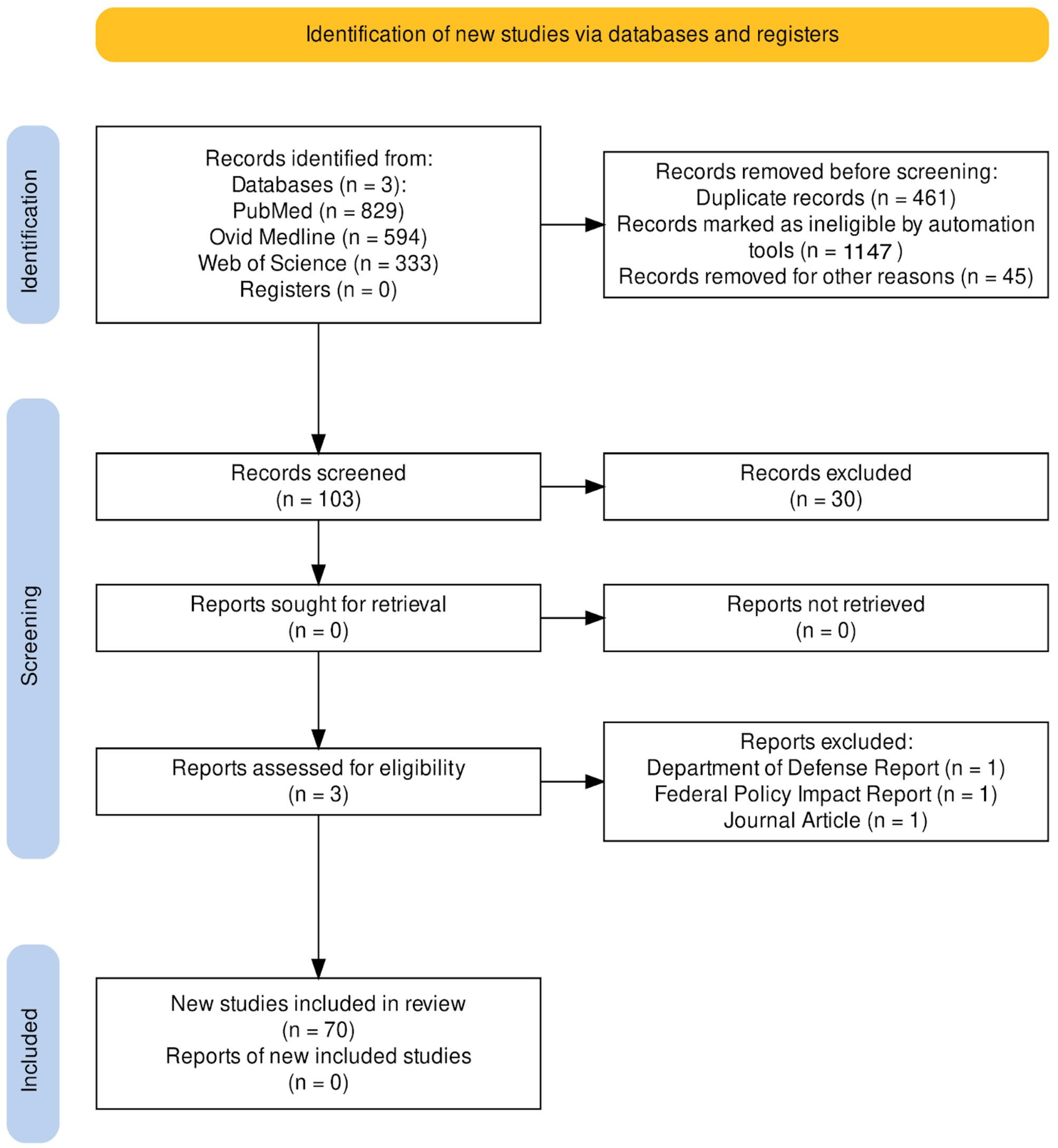
2.4. Sample Screening
2.5. Data Collection
3. Results
3.1. Rates of Reconstruction
3.2. Racial Disparities
3.3. Age Disparities
3.4. Insurance Disparities
3.5. Geographical Disparities
3.6. Travel Disparities
3.7. Income Disparities
3.8. Individual and Behavioral Disparities
3.9. Education Disparities
3.10. Language Disparities
3.11. Hospital Type Disparities
3.12. Healthcare System Disparities
3.13. Surgeon Disparities
3.14. Plastic Surgeon Density
4. Discussion
4.1. Future Considerations
4.2. Limitations
5. Conclusions
Supplementary Materials
Funding
Conflicts of Interest
References
- Merchant, S.J.; Goldstein, L.; Kruper, L.L. Patterns and Trends in Immediate Postmastectomy Reconstruction in California: Complications and Unscheduled Readmissions. Plast. Reconstr. Surg. 2015, 136, 10e–19e. [Google Scholar] [CrossRef] [PubMed]
- Liston, J.M.; Samuel, A.; Camacho, T.F.; Anderson, R.T.; Campbell, C.A.; Stranix, J.T. The State of Breast Cancer Reconstruction in Virginia: An Evidence-Based Framework for Identifying Locoregional Health Disparities. Ann. Plast. Surg. 2022, 89, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Weidman, A.A.; Kim, E.; Valentine, L.; Foppiani, J.; Alvarez, A.H.; Bustos, V.P.; Lee, B.T.; Lin, S.J. Outcomes of patients in rural communities undergoing autologous breast reconstruction: A comparison of cost and patient demographics with implications for rural health policy. Microsurgery 2024, 44, e31052. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.A.; Nelson, P.; Tchou, J.; Serletti, J.M.; Wu, L.C. The ethnic divide in breast reconstruction: A review of the current literature and directions for future research. Cancer Treat. Rev. 2012, 38, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Onega, T.; Weiss, J.; Kerlikowske, K.; Wernli, K.; Buist, D.S.; Henderson, L.M.; Goodrich, M.; Alford-Teaster, J.; Virnig, B.; Tosteson, A.N.; et al. The influence of race/ethnicity and place of service on breast reconstruction for Medicare beneficiaries with mastectomy. Springerplus 2014, 3, 416. [Google Scholar] [CrossRef] [PubMed]
- Doren, E.L.; Park, K.; Olson, J. Racial disparities in postmastectomy breast reconstruction following implementation of the affordable care act: A systematic review using a minority health and disparities research framework. Am. J. Surg. 2023, 226, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Tang, Y.; Wehby, G.L. Federal Health Coverage Mandates and Health Care Utilization: The Case of the Women’s Health and Cancer Rights Act and Use of Breast Reconstruction Surgery. J Womens Health 2015, 24, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Llaneras, J.; Klapp, J.M.; Boyd, J.B.; Granzow, J.; Moazzez, A.; Ozao-Choy, J.J.; Dauphine, C.; Goldberg, M.T. Post-Mastectomy Patients in an Urban Safety-Net Hospital: How Do Safety-Net Hospital Breast Reconstruction Rates Compare to National Breast Reconstruction Rates? Am. Surg. 2023, 89, 902–906. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.M.; Warnack, E.; Joseph, K.A. Breast Reconstruction in an Underserved Population: A Retrospective Study. Ann. Surg. Oncol. 2019, 26, 821–826. [Google Scholar] [CrossRef] [PubMed]
- Sisco, M.; Du, H.; Warner, J.P.; Howard, M.A.; Winchester, D.P.; Yao, K. Have we expanded the equitable delivery of postmastectomy breast reconstruction in the new millennium? Evidence from the national cancer data base. J. Am. Coll. Surg. 2012, 215, 658–666; discussion 666. [Google Scholar] [CrossRef] [PubMed]
- Restrepo, D.J.; Boczar, D.; Huayllani, M.T.; Sisti, A.; Gabriel, E.; McLaughlin, S.A.; Bagaria, S.; Spaulding, A.C.; Rinker, B.D.; Forte, A.J. Influence of Race, Income, Insurance, and Education on the Rate of Breast Reconstruction. Anticancer. Res. 2019, 39, 2969–2973. [Google Scholar] [CrossRef]
- White, M.J.; Prathibha, S.; Praska, C.; Ankeny, J.S.; LaRocca, C.J.; Owen, M.J.; Rao, M.M.; Tuttle, T.M.; Marmor, S.; Hui, J.Y.C. Disparities in post-mastectomy reconstruction use among American Indian and Alaska Native women. Plast. Reconstr. Surg. 2024, 154, 21e–32e. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, C.C.; Schneider, E.C.; Lipsitz, S.R.; Ko, C.Y.; Malin, J.L.; Epstein, A.M.; Weeks, J.C.; Kahn, K.L. Do Variations in Provider Discussions Explain Socioeconomic Disparities in Postmastectomy Breast Reconstruction? J. Am. Coll. Surg. 2008, 206, 605–615. [Google Scholar] [CrossRef]
- Albornoz, C.R.; Bach, P.B.; Pusic, A.L.; McCarthy, C.M.; Mehrara, B.J.; Disa, J.J.; Cordeiro, P.G.; Matros, E. The influence of sociodemographic factors and hospital characteristics on the method of breast reconstruction, including microsurgery: A U.S. population-based study. Plast. Reconstr. Surg. 2012, 129, 1071–1079. [Google Scholar] [CrossRef]
- Offodile, A.C.; Tsai, T.C.; Wenger, J.B.; Guo, L. Racial disparities in the type of postmastectomy reconstruction chosen. J. Surg. Res. 2015, 195, 368–376. [Google Scholar] [CrossRef]
- Sharma, K.; Grant, D.; Parikh, R.; Myckatyn, T. Race and Breast Cancer Reconstruction: Is There a Health Care Disparity? Plast. Reconstr. Surg. 2016, 138, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Connors, S.K.; Goodman, M.S.; Myckatyn, T.; Margenthaler, J.; Gehlert, S. Breast reconstruction after mastectomy at a comprehensive cancer center. Springerplus 2016, 5, 955. [Google Scholar] [CrossRef] [PubMed]
- Butler, P.D.; Morris, M.P.; Momoh, A.O. Persistent Disparities in Postmastectomy Breast Reconstruction and Strategies for Mitigation. Ann. Surg. Oncol. 2021, 28, 6099–6108. [Google Scholar] [CrossRef]
- Johnstone, T.; Thawanyarat, K.; Rowley, M.; Francis, S.; Camacho, J.M.; Singh, D.; Navarro, Y.; Shah, J.K.; Nazerali, R.S. Racial Disparities in Postoperative Breast Reconstruction Outcomes: A National Analysis. J. Racial Ethn. Health Disparities 2023, 11, 1199–1210. [Google Scholar] [CrossRef]
- Li, A.; Luaces, M.A.; De Souza, M. Cultural Beliefs Regarding Breast Reconstruction in a Minority Group. ePlasty 2023, 23, e45. [Google Scholar] [PubMed]
- Alderman, A.K.; Hawley, S.T.; Janz, N.K.; Mujahid, M.S.; Morrow, M.; Hamilton, A.S.; Graff, J.J.; Katz, S.J. Racial and Ethnic Disparities in the Use of Postmastectomy Breast Reconstruction: Results from a Population-Based Study. J. Clin. Oncol. 2009, 27, 5325–5330. [Google Scholar] [CrossRef] [PubMed]
- Iskandar, M.E.; Dayan, E.; Lucido, D.; Samson, W.; Sultan, M.; Dayan, J.H.; Boolbol, S.K.; Smith, M.L. Factors influencing incidence and type of postmastectomy breast reconstruction in an urban multidisciplinary cancer center. Plast. Reconstr. Surg. 2015, 135, 270e–276e. [Google Scholar] [CrossRef] [PubMed]
- Butler, P.D.; Familusi, O.; Serletti, J.M.; Fox, J.P. Influence of race, insurance status, and geographic access to plastic surgeons on immediate breast reconstruction rates. Am. J. Surg. 2018, 215, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Wirth, L.S.; Hinyard, L.; Keller, J.; Bucholz, E.; Schwartz, T. Geographic variations in racial disparities in postmastectomy breast reconstruction: A SEER database analysis. Breast J. 2019, 25, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, J.R.; Stankowski-Drengler, T.J.; Tucholka, J.L.; Poore, S.O.; Wilke, L.G.; Greenberg, C.C.; Neuman, H.B. Utility of Health Services Regions in Examining Socioeconomic Disparities in Receipt of Breast Reconstruction. Breast J. 2020, 26, 1895–1897. [Google Scholar] [CrossRef] [PubMed]
- Yalamanchili, S.; Madzia, J.; Dembinski, D.; Ortman, M.; Gobble, R. A look at racial and socioeconomic disparities in post-mastectomy breast reconstruction at a midwestern academic hospital. Breast J. 2021, 27, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Alvidrez, J.; Castille, D.; Laude-Sharp, M.; Rosario, A.; Tabor, D. The National Institute on Minority Health and Health Disparities Research Framework. Am. J. Public. Health. 2019, 109 (Suppl. S1), S16–S20. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, A.R.; Willcox, L.M.; Abolghasemi, D.M.; Jiang, R.; Wei, Z.Z.; Arciero, C.A.; Subhedar, P.D. Did Medicaid Expansion Mitigate Disparities in Post-mastectomy Reconstruction Rates? Am. Surg. 2022, 88, 846–851. [Google Scholar] [CrossRef] [PubMed]
- Enewold, L.R.; McGlynn, K.A.; Zahm, S.H.; Poudrier, J.; Anderson, W.F.; Shriver, C.D.; Zhu, K. Breast reconstruction after mastectomy among Department of Defense beneficiaries by race. Cancer 2014, 120, 3033–3039. [Google Scholar] [CrossRef]
- Ramalingam, K.; Ji, L.; Pairawan, S.; Molina, D.C.; Lum, S.S. Improvement in Breast Reconstruction Disparities following Medicaid Expansion under the Affordable Care Act. Ann. Surg. Oncol. 2021, 28, 5558–5567. [Google Scholar] [CrossRef]
- Butler, P.D.; Nelson, J.A.; Fischer, J.P.; Wink, J.D.; Chang, B.; Fosnot, J.; Wu, L.C.; Serletti, J.M. Racial and age disparities persist in immediate breast reconstruction: An updated analysis of 48,564 patients from the 2005 to 2011 American College of Surgeons National Surgery Quality Improvement Program data sets. Am. J. Surg. 2016, 212, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, E.; Giladi, A.M.; Wu, L.; Chung, K.C. Effect of federal and state policy changes on racial/ethnic variation in immediate postmastectomy breast reconstruction. Plast. Reconstr. Surg. 2015, 135, 1285–1294. [Google Scholar] [CrossRef]
- Gooch, J.C.; Guth, A.; Yang, J.; Zhu, C.; Park, J.; Telem, D.; Bui, D.; O’hea, B.; Khan, S. Increases in Postmastectomy Reconstruction in New York State Are Not Related to Changes in State Law. Plast. Reconstr. Surg. 2019, 144, 159e–166e. [Google Scholar] [CrossRef]
- Mandelbaum, A.; Nakhla, M.; Seo, Y.J.; Dobaria, V.; Attai, D.J.; Baker, J.L.; Thompson, C.K.; DiNome, M.L.; Benharash, P.; Lee, M.K. National trends and predictors of mastectomy with immediate breast reconstruction. Am. J. Surg. 2021, 222, 773–779. [Google Scholar] [CrossRef]
- Boczar, D.; Restrepo, D.J.; Sisti, A.; Huayllani, M.T.; Spaulding, A.C.; Gabriel, E.; Bagaria, S.; Mclaughlin, S.; Parker, A.S.; Forte, A.J. Influence of Facility Characteristics on Access to Breast Reconstruction: A 12-Year National Cancer Database Analysis. Anticancer. Res. 2019, 39, 6881–6885. [Google Scholar] [CrossRef]
- Friedman-Eldar, O.; Burke, J.; Silva, I.d.C.; Baumrucker, C.C.; Valle, F.; Lessard, A.-S.; Kassira, W.; Franceschi, D.; Kesmodel, S.B.; Avisar, E.; et al. Stalled at the intersection: Insurance status and disparities in post-mastectomy breast reconstruction. Breast Cancer Res. Treat. 2022, 194, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Nkana, Z.H.; Wood, K.L.; Karczewski, A.M.; A Gunderson, K.; Lyon, S.M.; Dingle, A.M.; O Poore, S. Evaluation of Racial Disparities in Postoperative Outcomes Following Breast Reconstruction at a Single Institution in Wisconsin. WMJ 2021, 120 (Suppl. S1), S42–S47. [Google Scholar] [PubMed]
- Shippee, T.P.; Kozhimannil, K.B.; Rowan, K.; Virnig, B.A. Health insurance coverage and racial disparities in breast reconstruction after mastectomy. Womens Health Issues 2014, 24, e261–e269. [Google Scholar] [CrossRef] [PubMed]
- Tseng, W.H.M.; Stevenson, T.R.M.; Canter, R.J.M.; Chen, S.L.M.; Khatri, V.P.M.; Bold, R.J.M.; Martinez, S.R.M. Sacramento Area Breast Cancer Epidemiology Study (SABES): Use of Post-Mastectomy Breast Reconstruction along the Rural to Urban Continuum. Plast. Reconstr. Surg. 2010, 126, 1815–1824. [Google Scholar] [CrossRef]
- Beaulieu-Jones, B.R.M.; Fefferman, A.; Woods, A.P.; Shewmaker, G.; Zhang, T.; Roh, D.S.; E Sachs, T.; Merrill, A.M.; Ko, N.Y.; Cassidy, M.R.M. Impact of Race, Ethnicity, Primary Language, and Insurance on Reconstruction after Mastectomy for Patients with Breast Cancer at an Urban, Academic Safety-Net Hospital. J. Am. Coll. Surg. 2023, 236, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.; Friedman-Eldar, O.; Halfteck, G.; Silva, I.d.C.; Baumrucker, C.C.; Reyes, F.V.; Lessard, A.-S.; Kassira, W.; Franceschi, D.; Kesmodel, S.B.; et al. Persistent and interdependent: Racial disparities and their mechanisms in postmastectomy breast reconstruction. Surgery 2022, 172, 25–30. [Google Scholar] [CrossRef] [PubMed]
- DeCoster, R.C.; Jr, R.F.B.; Burns, J.C.; Dugan, A.J.; Edmunds, R.W.; Rinker, B.D.; Webster, J.M.; Vasconez, H.C. Rural-Urban Differences in Breast Reconstruction Utilization Following Oncologic Resection. J. Rural. Health 2020, 36, 347–354. [Google Scholar] [CrossRef] [PubMed]
- DeCoster, R.C.; Stout, M.A.B.; Burns, J.C.; Shrout, M.A.B.; Wetzel, M.B.; Dugan, A.J.; Rinker, B.D.; Butterfield, T.A.; Webster, J.M.; Vasconez, H.C. Appalachian Status is a Negative Predictor of Breast Reconstruction Following Breast Cancer Resection. Ann. Plast. Surg. 2019, 83, e15–e19. [Google Scholar] [CrossRef] [PubMed]
- Rosson, G.D.; Singh, N.K.; Ahuja, N.; Jacobs, L.K.; Chang, D.C. Multilevel analysis of the impact of community vs patient factors on access to immediate breast reconstruction following mastectomy in Maryland. Arch. Surg. 2008, 143, 1076–1081; discusion 1081. [Google Scholar] [CrossRef] [PubMed]
- Sergesketter, A.R.; Thomas, S.M.; Lane, W.O.; Orr, J.P.; Shammas, R.L.; Fayanju, O.M.; Greenup, R.A.; Hollenbeck, S.T. Decline in Racial Disparities in Postmastectomy Breast Reconstruction: A Surveillance, Epidemiology, and End Results Analysis from 1998 to 2014. Plast. Reconstr. Surg. 2019, 143, 1560–1570. [Google Scholar] [CrossRef] [PubMed]
- Tseng, J.F.; Kronowitz, S.J.; Sun, C.C.; Perry, A.C.; Hunt, K.K.; Babiera, G.V.; Newman, L.A.; Singletary, S.E.; Mirza, N.Q.; Ames, F.C.; et al. The effect of ethnicity on immediate reconstruction rates after mastectomy for breast cancer. Cancer 2004, 101, 1514–1523. [Google Scholar] [CrossRef] [PubMed]
- Epstein, S.; Tran, B.N.; Cohen, J.B.; Lin, S.J.; Singhal, D.; Lee, B.T. Racial disparities in postmastectomy breast reconstruction: National trends in utilization from 2005 to 2014. Cancer 2018, 124, 2774–2784. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.M.; Njoroge, M.W.; Mundy, L.R.; Sergesketter, A.R.; Stukes, B.; Shammas, R.L.; Langdell, H.C.; Geng, Y.; Hollenbeck, S.T. Evaluating Disparities in Pathways to Breast Reconstruction. J. Reconstr. Microsurg. 2023, 39, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Connors, S.K.; Goodman, M.S.; Myckatyn, T.; Margenthaler, J.; Gehlert, S. Racial Disparities in Breast Reconstruction at a Comprehensive Cancer Center. J. Racial Ethn. Health Disparities 2022, 9, 2323–2333. [Google Scholar] [CrossRef] [PubMed]
- Zaveri, S.; Nevid, D.; Ru, M.; Moshier, E.; Pisapati, K.; Reyes, S.A.; Port, E.; Romanoff, A. Racial Disparities in Time to Treatment Persist in the Setting of a Comprehensive Breast Center. Ann. Surg. Oncol. 2022, 29, 6692–6703. [Google Scholar] [CrossRef] [PubMed]
- Kamali, P.; Zettervall, S.L.; Wu, W.; Ibrahim, A.M.S.; Medin, C.; Rakhorst, H.A.; Schermerhorn, M.L.; Lee, B.T.; Lin, S.J. Differences in the Reporting of Racial and Socioeconomic Disparities among Three Large National Databases for Breast Reconstruction. Plast. Reconstr. Surg. 2017, 139, 795–807. [Google Scholar] [CrossRef] [PubMed]
- Obinero, C.G.; Pedroza, C.; Bhadkamkar, M.; Blakkolb, C.L.; Kao, L.S.; Greives, M.R. We are moving the needle: Improving racial disparities in immediate breast reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2024, 88, 161–170. [Google Scholar] [CrossRef]
- Le Blanc, J.; Golshan, M.; Lannin, D.; Greenup, R.; Berger, E.R.; Saridakis, A.; Horowitz, N.; Zanieski, G.; Avraham, T.; Mastrioanni, M.; et al. Association of Medicaid Expansion with Post-mastectomy Reconstruction Rates. Ann. Surg. Oncol. 2022, 29, 2181–2189. [Google Scholar] [CrossRef] [PubMed]
- Fasano, G.; Bayard, S.; Tamimi, R.; An, A.; Zenilman, M.E.; Davis, M.; Newman, L.; Bea, V.J. Postmastectomy Breast Reconstruction Patterns at an Urban Academic Hospital and the Impact of Surgeon Gender. Ann. Surg. Oncol. 2022, 29, 5437–5444. [Google Scholar] [CrossRef] [PubMed]
- Levine, S.M.; Levine, A.; Raghubir, J.; Levine, J.P. A 10-year review of breast reconstruction in a university-based public hospital. Ann. Plast. Surg. 2012, 69, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Holliday, T.L.; Suggs, P.D.; Thompson, S.N.; Richmond, B.K. Disparities in Rural Breast Cancer Care: Factors Affecting Choice of Breast Reconstruction in a West Virginia Tertiary Care Hospital. Am. Surg. 2017, 83, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Matros, E.; Yueh, J.H.; Bar-Meir, E.D.; Slavin, S.A.; Tobias, A.M.; Lee, B.T. Sociodemographics, referral patterns, and Internet use for decision-making in microsurgical breast reconstruction. Plast. Reconstr. Surg. 2010, 125, 1087–1094. [Google Scholar] [CrossRef]
- Wexelman, B.; Schwartz, J.A.; Lee, D.; Estabrook, A.; Ma, A.M.T. Socioeconomic and geographic differences in immediate reconstruction after mastectomy in the United States. Breast J. 2014, 20, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Kamali, P.; Ricci, J.A.; Curiel, D.A.B.; Cohen, J.B.; Chattha, A.B.; Rakhorst, H.A.; Lee, B.T.M.; Lin, S.J.M. Immediate Breast Reconstruction among Patients with Medicare and Private Insurance: A Matched Cohort Analysis. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1552. [Google Scholar] [CrossRef] [PubMed]
- Obeng-Gyasi, S.; Rose, J.; Dong, W.; Kim, U.; Koroukian, S. Is Medicaid Expansion Narrowing Gaps in Surgical Disparities for Low-Income Breast Cancer Patients? Ann. Surg. Oncol. 2022, 29, 1763–1769. [Google Scholar] [CrossRef] [PubMed]
- Aliu, O.; Giladi, A.M.; Chung, K.C. Trends in Medicaid beneficiaries’ receipt of breast reconstruction procedures following Pre-Affordable Care Act (ACA) Medicaid expansion in New York State. Am. J. Surg. 2018, 216, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Moroni, E.A.M.; Bustos, S.S.; Mehta, M.B.; Munoz-Valencia, A.; Douglas, N.K.O.M.; Bustos, V.P.; Evans, S.; Diego, E.J.; De La Cruz, C. Disparities in Access to Postmastectomy Breast Reconstruction: Does Living in a Specific ZIP Code Determine the Patient’s Reconstructive Journey? Ann. Plast. Surg. 2022, 88 (Suppl. S3), S279–S283. [Google Scholar] [CrossRef] [PubMed]
- Stankowski, T.J.; Schumacher, J.R.; Hanlon, B.M.; Tucholka, J.L.; Venkatesh, M.; Yang, D.-Y.; Poore, S.O.; Neuman, H.B. Barriers to Breast Reconstruction for Socioeconomically Disadvantaged Women. Breast Cancer Res. Treat. 2022, 195, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.L.; Newman, A.S.; Lin, I.C.; Reinke, C.E.; Karakousis, G.C.; Czerniecki, B.J.; Wu, L.C.; Kelz, R.R. Trends in immediate breast reconstruction across insurance groups after enactment of breast cancer legislation. Cancer 2013, 119, 2462–2468. [Google Scholar] [CrossRef] [PubMed]
- Momoh, A.O.; Griffith, K.A.M.; Hawley, S.T.P.; Morrow, M.; Ward, K.C.P.; Hamilton, A.S.; Shumway, D.; Katz, S.J.M.; Jagsi, R.M. Patterns and Correlates of Knowledge, Communication, and Receipt of Breast Reconstruction in a Modern Population-Based Cohort of Patients with Breast Cancer. Plast. Reconstr. Surg. 2019, 144, 303–313. [Google Scholar] [CrossRef]
- Siegel, E.; Tseng, J.; Giuliano, A.; Amersi, F.; Alban, R.F. Treatment at Academic Centers Increases Likelihood of Reconstruction after Mastectomy for Breast Cancer Patients. J. Surg. Res. 2020, 247, 156–162. [Google Scholar] [CrossRef]
- Tung, L.; Jeong, Y.J.; Lane, C.; Carey, J.N.; Sposto, R.; Schechter, N.R.; Sener, S.F.; Lang, J.E. Factors Leading to Decreased Rates of Immediate Postmastectomy Reconstruction. J. Surg. Res. 2019, 238, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Vora, H.; Chung, A.; Lewis, A.; Mirocha, J.; Amersi, F.; Giuliano, A.; Alban, R.F. Reconstruction among patients undergoing mastectomy: The effect of surgical deserts. J. Surg. Res. 2018, 223, 237–242. [Google Scholar] [CrossRef]
- Meade, A.E.; Cummins, S.M.; Farewell, J.T.; Duque, S.B.; Mulqueen, S.K.B.; Chuah, A.B.; Zhang, A.Y. Breaking Barriers to Breast Reconstruction among Socioeconomically Disadvantaged Patients at a Large Safety-net Hospital. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4410. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.L.; Newman, A.S.; Reinke, C.E.; Lin, I.C.; Karakousis, G.C.; Czerniecki, B.J.; Wu, L.C.; Kelz, R.R. Racial disparities in immediate breast reconstruction after mastectomy: Impact of state and federal health policy changes. Ann. Surg. Oncol. 2013, 20, 399–406. [Google Scholar] [CrossRef]
- Mahmoudi, E.; Lu, Y.; Metz, A.K.; Momoh, A.O.; Chung, K.C. Association of a Policy Mandating Physician-Patient Communication with Racial/Ethnic Disparities in Postmastectomy Breast Reconstruction. JAMA Surg. 2017, 152, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Nasser, J.S.; Fahmy, J.N.; Song, Y.; Wang, L.; Chung, K.C. Regional Implicit Racial Bias and Rates of Breast Reconstruction, Complications, and Cost among US Patients with Breast Cancer. JAMA Netw. Open 2023, 6, e2325487. [Google Scholar] [CrossRef] [PubMed]
- Odom, E.B.; Schmidt, A.C.; Myckatyn, T.M.; Buck, D.W. A Cross-Sectional Study of Variations in Reimbursement for Breast Reconstruction: Is a Healthcare Disparity on the Horizon? Ann. Plast. Surg. 2018, 80, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Stankowski, T.J.; Alagoz, E.; Jacobson, N.; Neuman, H.B. Factors Associated with Socioeconomic Disparities in Breast Reconstruction: Perspectives of Wisconsin Surgeons. Clin. Breast Cancer 2023, 23, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Retrouvey, H.; Solaja, O.; Gagliardi, A.R.; Webster, F.; Zhong, T. Barriers of Access to Breast Reconstruction: A Systematic Review. Plast. Reconstr. Surg. 2019, 143, 465e–476e. [Google Scholar] [CrossRef] [PubMed]
| Study Category | Number and Percentage of Topic Discussed (n = 70) |
|---|---|
| Sociodemographic | 61 (87.1%) |
| Insurance | 38 (54.2%) |
| Geography | 21 (30%) |
| Hospital type | 13 (18.6%) |
| Income | 12 (17.1) |
| Surgeon | 9 (12.86%) |
| Education level of patient | 5 (7.14%) |
| Communication | 5 (7.14%) |
| Federal mandates | 5 (7.14%) |
| Patient satisfaction | 1 (1.4%) |
| Decision making | 1 (1.4%) |
| Reimbursement | 1 (1.4%) |
| Language | 1 (1.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vangsness, K.L.; Juste, J.; Sam, A.-P.; Munabi, N.; Chu, M.; Agko, M.; Chang, J.; Carre, A.L. Post-Mastectomy Breast Reconstruction Disparities: A Systematic Review of Sociodemographic and Economic Barriers. Medicina 2024, 60, 1169. https://doi.org/10.3390/medicina60071169
Vangsness KL, Juste J, Sam A-P, Munabi N, Chu M, Agko M, Chang J, Carre AL. Post-Mastectomy Breast Reconstruction Disparities: A Systematic Review of Sociodemographic and Economic Barriers. Medicina. 2024; 60(7):1169. https://doi.org/10.3390/medicina60071169
Chicago/Turabian StyleVangsness, Kella L., Jonathan Juste, Andre-Phillippe Sam, Naikhoba Munabi, Michael Chu, Mouchammed Agko, Jeff Chang, and Antoine L. Carre. 2024. "Post-Mastectomy Breast Reconstruction Disparities: A Systematic Review of Sociodemographic and Economic Barriers" Medicina 60, no. 7: 1169. https://doi.org/10.3390/medicina60071169







