A Rare Case of Solitary Neurofibroma Misdiagnosed as Diabetic Foot Ulcer in the Toe Tip Region
Abstract
1. Introduction
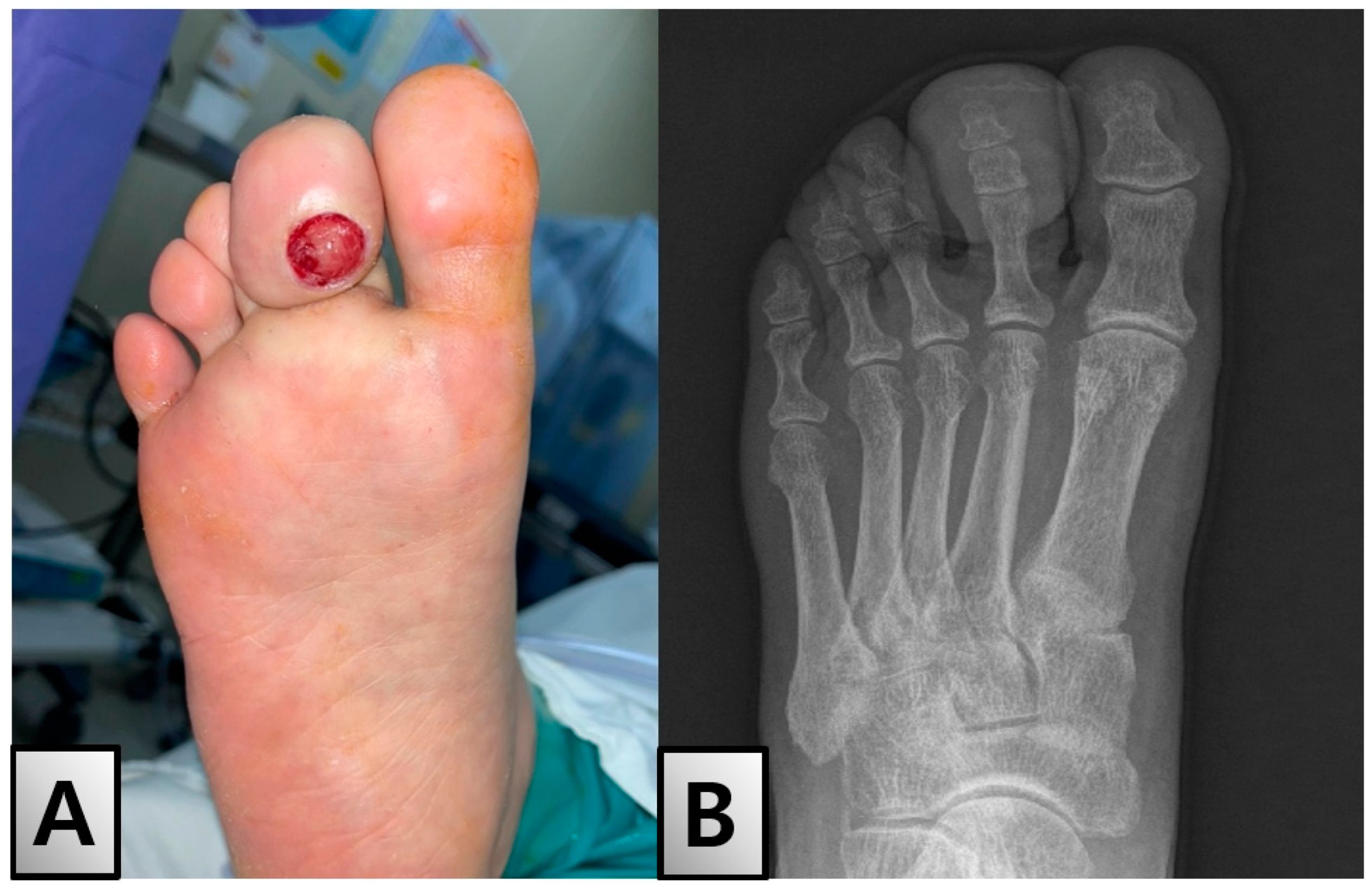
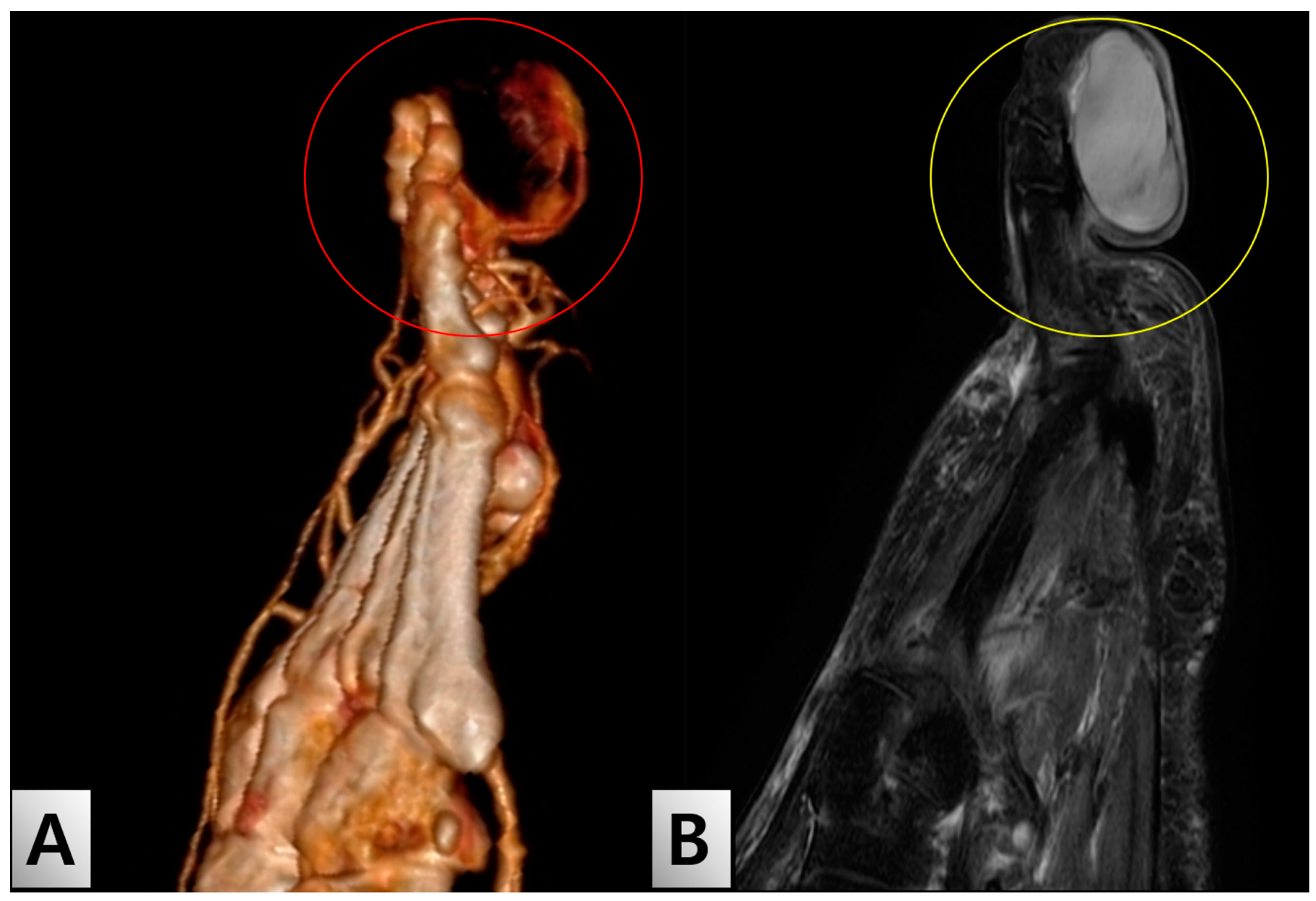
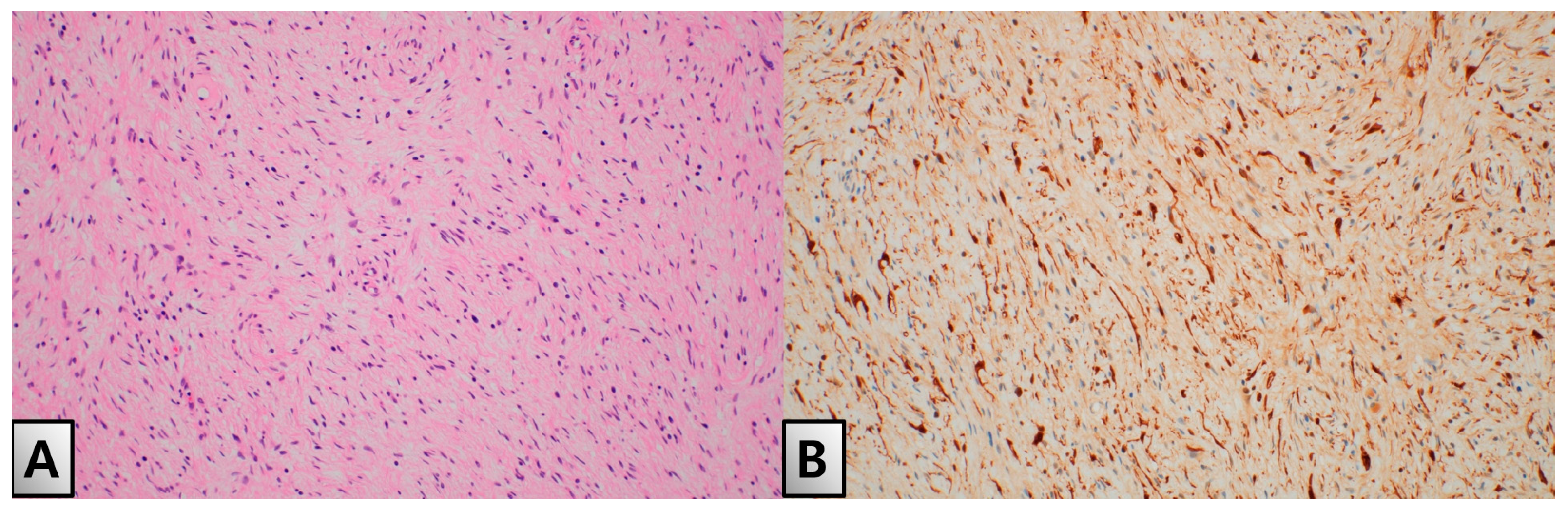
2. Case Presentation
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoda, S.A. Enzinger and Weiss’s Soft Tissue Tumors. Am. J. Clin. Pathol. 2020, 154, 424. [Google Scholar] [CrossRef]
- Mahmud, S.A.; Shah, N.; Chattaraj, M.; Gayen, S. Solitary Encapsulated Neurofibroma Not Associated with Neurofibromatosis-1 Affecting Tongue in a 73-Year-Old Female. Case Rep. Dent. 2016, 2016, 3630153. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers and Their Recurrence. N. Engl. J. Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef] [PubMed]
- Aagaard, T.V.; Moeini, S.; Skou, S.T.; Madsen, U.R.; Brorson, S. Benefits and Harms of Exercise Therapy for Patients with Diabetic Foot Ulcers: A Systematic Review. Int. J. Low. Extrem. Wounds 2022, 21, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.W.; Selvin, E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr. Diab. Rep. 2019, 19, 86. [Google Scholar] [CrossRef] [PubMed]
- Pilavaki, M.; Chourmouzi, D.; Kiziridou, A.; Skordalaki, A.; Zarampoukas, T.; Drevelengas, A. Imaging of peripheral nerve sheath tumors with pathologic correlation: Pictorial review. Eur. J. Radiol. 2004, 52, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Cheer, K.; Shearman, C.; Jude, E.B. Managing complications of the diabetic foot. BMJ 2009, 339, 1304–1307. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hingorai, A.; LaMuraglia, G.M.; Henke, P.; Meissner, M.H.; Loretz, L.; Zinszer, K.M.; Driver, V.R.; Frykberg, R.; Carman, T.L.; Marston, W.; et al. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in Collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J. Vasc. Surg. 2016, 63, 3S–21S. [Google Scholar] [CrossRef] [PubMed]
- Monteiro-Soares, M.; Boyko, E.J.; Ribeiro, J.; Ribeiro, I.; Dinis-Ribeiro, M. Risk stratification systems for diabetic foot ulcers: A systematic review. Diabetologia 2011, 54, 1190–1199. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Lipsky, B.A. Diabetic foot infections: Stepwise medical and surgical management. Int. Wound J. 2004, 1, 123–132. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Result | Reference Range |
|---|---|---|
| HbA1c (%) | 6.4 | 4.0–5.6 |
| Fasting Blood Glucose (mg/dL) | 180 | 70–100 |
| CRP (mg/L) | 12.5 | 0–10 |
| WBC (×109/L) | 8.6 | 4.0–11.0 |
| Total Cholesterol (mg/dL) | 190 | <200 |
| LDL Cholesterol (mg/dL) | 99 | <100 |
| HDL Cholesterol (mg/dL) | 41 | >40 |
| Triglycerides (mg/dL) | 145 | <150 |
| Creatinine (mg/dL) | 0.9 | 0.6–1.2 |
| Blood Urea Nitrogen (BUN) (mg/dL) | 15 | 7-20 |
| Albumin (g/dL) | 4 | 3.5–5.0 |
| Alanine Aminotransferase (ALT) (IU/L) | 25 | 7–56 |
| Aspartate Aminotransferase (AST) (IU/L) | 22 | 10–40 |
| Hemoglobin (g/dL) | 13.5 | 13.8–17.2 (males) |
| 12.1–15.1 (females) | ||
| Platelets (×109/L) | 250 | 150–450 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, H.-J.; Kim, S.-Y.; Oh, M.-H.; Lim, S.; Choi, H.-J. A Rare Case of Solitary Neurofibroma Misdiagnosed as Diabetic Foot Ulcer in the Toe Tip Region. Medicina 2024, 60, 1200. https://doi.org/10.3390/medicina60081200
Nam H-J, Kim S-Y, Oh M-H, Lim S, Choi H-J. A Rare Case of Solitary Neurofibroma Misdiagnosed as Diabetic Foot Ulcer in the Toe Tip Region. Medicina. 2024; 60(8):1200. https://doi.org/10.3390/medicina60081200
Chicago/Turabian StyleNam, Ha-Jong, Se-Young Kim, Mee-Hye Oh, Soomin Lim, and Hwan-Jun Choi. 2024. "A Rare Case of Solitary Neurofibroma Misdiagnosed as Diabetic Foot Ulcer in the Toe Tip Region" Medicina 60, no. 8: 1200. https://doi.org/10.3390/medicina60081200
APA StyleNam, H.-J., Kim, S.-Y., Oh, M.-H., Lim, S., & Choi, H.-J. (2024). A Rare Case of Solitary Neurofibroma Misdiagnosed as Diabetic Foot Ulcer in the Toe Tip Region. Medicina, 60(8), 1200. https://doi.org/10.3390/medicina60081200






