Enhancing Bystander Intervention: Insights from the Utstein Analysis of Out-of-Hospital Cardiac Arrests in Slovenia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Area and Population
2.3. Description of the Emergency Medical System
2.4. Data Collection
2.5. Statistical Methodology
2.6. Model Development
3. Results
3.1. Bystanders
Bystander Response and Location of OHCA
3.2. Results—Logistic Regression
3.3. Predicting ROSC
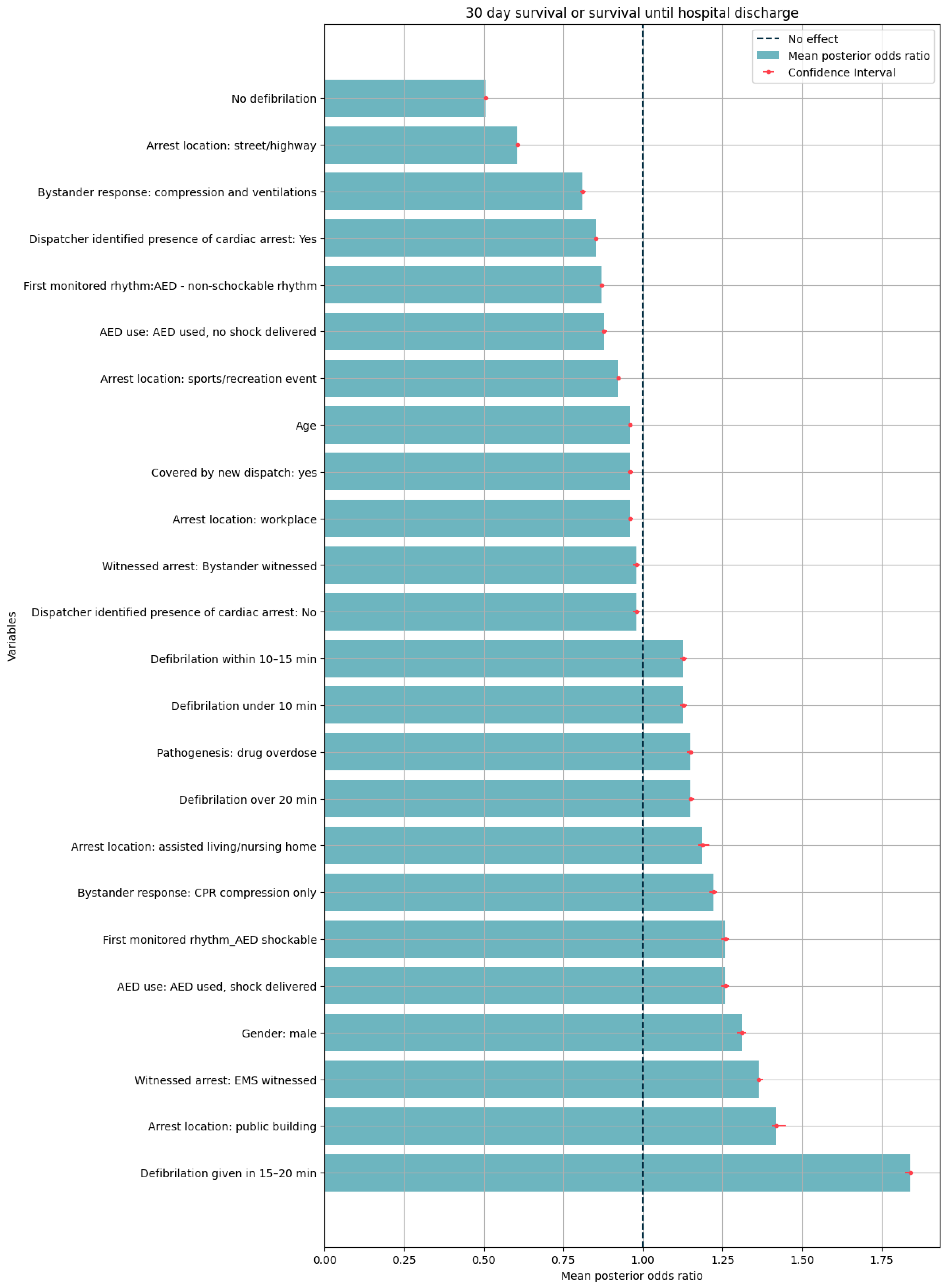
3.4. Predicting Survival until Hospital Discharge or 30-Day Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AED | automated external defibrillator |
| ALS | advanced life support |
| bCPR | CPR with ventilation and chest compressions |
| BLS | basic life support |
| CCs | chest compressions |
| CI | confidence interval |
| CPC | cerebral performance category |
| DNAR | do not attempt resuscitation |
| DNS | did not survive |
| EMS | emergency medical service |
| EuReCa TWO | European Registry of Cardiac Arrest Two |
| GDP | gross domestic product |
| IBM SPSS | International Business Machines Corporation Statistical Package for the Social Sciences |
| ID CA | identified cardiac arrest |
| ILCOR | International Liaison Committee on Resuscitation |
| OHCA | out-of-hospital cardiac arrest |
| PEA | pulseless electrical activity |
| ROSC | return of spontaneous circulation |
| S | survived |
| SD | standard deviation |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| Vent | ventilation |
| VF | ventricular fibrillation |
References
- Myat, A.; Song, K.-J.; Rea, T. Out-of-Hospital Cardiac Arrest: Current Concepts. Lancet 2018, 391, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Gräsner, J.-T.; Lefering, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, I.B.M.; Ortiz, F.R.; Maurer, H.; et al. EuReCa ONE 27 Nations, ONE Europe, ONE Registry: A Prospective One Month Analysis of out-of-Hospital Cardiac Arrest Outcomes in 27 Countries in Europe. Resuscitation 2016, 105, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Lancet, T. Out-of-Hospital Cardiac Arrest: A Unique Medical Emergency. Lancet 2018, 391, 911. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gan, Y.; Jiang, N.; Wang, R.; Chen, Y.; Luo, Z.; Zong, Q.; Chen, S.; Lv, C. The Global Survival Rate among Adult Out-of-Hospital Cardiac Arrest Patients Who Received Cardiopulmonary Resuscitation: A Systematic Review and Meta-Analysis. Crit. Care 2020, 24, 61. [Google Scholar] [CrossRef] [PubMed]
- Oving, I.; Masterson, S.; Tjelmeland, I.B.M.; Jonsson, M.; Semeraro, F.; Ringh, M.; Truhlar, A.; Cimpoesu, D.; Folke, F.; Beesems, S.G.; et al. First-Response Treatment after out-of-Hospital Cardiac Arrest: A Survey of Current Practices across 29 Countries in Europe. Scand. J. Trauma. Resusc. Emerg. Med. 2019, 27, 112. [Google Scholar] [CrossRef] [PubMed]
- Blewer, A.L.; Ho, A.F.W.; Shahidah, N.; White, A.E.; Pek, P.P.; Ng, Y.Y.; Mao, D.R.; Tiah, L.; Chia, M.Y.-C.; Leong, B.S.-H.; et al. Impact of Bystander-Focused Public Health Interventions on Cardiopulmonary Resuscitation and Survival: A Cohort Study. Lancet Public Health 2020, 5, e428–e436. [Google Scholar] [CrossRef] [PubMed]
- Škufca Strle, M.; Baznik, Š.; Skufca Sterle, M.; Baznik, S. Kako Izboljšati Preživetje Po Kardiopulmonalni Reanimaciji? In Zbornik Prispevkov: Urgentna Medicina: Izbrana Poglavja; Vajd, R., Gričar, M., Eds.; Slovensko Združenje za Urgentno Medicino: Ljubljana, Slovenia, 2013; pp. 218–222. [Google Scholar]
- Gräsner, J.-T.; Wnent, J.; Herlitz, J.; Perkins, G.D.; Lefering, R.; Tjelmeland, I.; Koster, R.W.; Masterson, S.; Rossell-Ortiz, F.; Maurer, H.; et al. Survival after Out-of-Hospital Cardiac Arrest in Europe—Results of the EuReCa TWO Study. Resuscitation 2020, 148, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Breckwoldt, J.; Lockey, A.; Bossaert, L.; Mistiaen, L.; Georgiou, M. National Implementation of CPR Training Programmes for School Children in Europe. Resuscitation 2013, 84, S40. [Google Scholar] [CrossRef]
- Perkins, G.D.; Jacobs, I.G.; Nadkarni, V.M.; Berg, R.A.; Bhanji, F.; Biarent, D.; Bossaert, L.L.; Brett, S.J.; Chamberlain, D.; de Caen, A.R.; et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: A Statement for Healthcare Professionals from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015, 132, 1286–1300. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. STROBE Initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef]
- Gross Domestic Product by Measures and Year. Available online: https://www.stat.si/statweb (accessed on 24 February 2024).
- Grmec, Š.; Križmarič, M.; Mally, Š.; Koželj, A.; Špindler, M.; Lešnik, B. Utstein Style Analysis of Out-of-Hospital Cardiac Arrest—Bystander CPR and End Expired Carbon Dioxide. Resuscitation 2007, 72, 404–414. [Google Scholar] [CrossRef]
- Fink, A.; Čander, D.; Kelebuda, D.; Gorjup, D.; Strnad, M.; Špindler, M.; Brezovnik, M.; Rajapakse, R.; Koren, T. (Eds.) Slovenski Indeks Za Nujno Medicinsko Pomoč, 1st ed.; Ministrstvo za Zdravje, Služba za Razvoj in Organizacijo Dejavnosti Nujne Medicinske Pomoči: Ljubljana, Slovenia, 2017; ISBN 978-961-6523-60-8. [Google Scholar]
- Petravić, L.; Burger, E.; Keše, U.; Kulovec, D.; Miklič, R.; Poljanšek, E.; Tomšič, G.; Pintarič, T.; Lopes, M.F.; Turnšek, E.; et al. How Can Out-of-Hospital Cardiac Arrest (OHCA) Data Collection in Slovenia Be Improved? Medicina 2023, 59, 1050. [Google Scholar] [CrossRef]
- Repše, J. Vloga Certificiranih Prvih Posredovalcev v Sistemu Zaščite in Reševanja: Diplomsko Delo = Role of Certified First Responders in Rescue and Protection System. Bachelor’s Thesis, University of Ljubljana, Ljubljana, Slovenia, 2022. [Google Scholar]
- Perkins, G.D.; Gräsner, J.-T.; Semeraro, F.; Olasveengen, T.; Soar, J.; Lott, C.; Van De Voorde, P.; Madar, J.; Zideman, D.; Mentzelopoulos, S.; et al. European Resuscitation Council Guidelines 2021: Executive Summary. Resuscitation 2021, 161, 1–60. [Google Scholar] [CrossRef] [PubMed]
- Petravić, L.; Burger, E.; Kulovec, D.; Lopes, M.F.; Pintarič, T.; Poljanšek, E.; Šircelj, G.; Tomšič, G.; Turnšek, E.; Brezovnik, M.; et al. SiOHCA: Out-of-Hospital Cardiac Arrests in Slovenia, 2022; Data File; 2024. Available online: https://www.adp.fdv.uni-lj.si/opisi/siohca22/ (accessed on 22 February 2024).
- Tenny, S.; Boktor, S.W. Incidence. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Burger, E. Untapped Bystander Potential in Slovenia: Out-of-Hospital Cardiac Arrests Utstein Style Report—Data Analysis. 2024. Available online: https://zenodo.org/records/10660023 (accessed on 15 February 2024).
- SURS Slovenian Population in 2023. Slovenian Census Data from 2023. 2023. Available online: https://www.stat.si/StatWeb/en (accessed on 22 February 2024).
- Tadel, S.; Horvat, M.; Noc, M. Treatment of Out-of-Hospital Cardiac Arrest in Ljubljana: Outcome Report According to the ‘Utstein’ Style. Resuscitation 1998, 38, 169–176. [Google Scholar] [CrossRef]
- Randjelovic, S.S.; Nikolovski, S.S.; Tijanic, J.Z.; Obradovic, I.A.; Fiser, Z.Z.; Lazic, A.D.; Raffay, V.I. Out-of-Hospital Cardiac Arrest Prospective Epidemiology Monitoring during the First Five Years of EuReCa Program Implementation in Serbia. Prehosp. Disaster Med. 2023, 38, 95–102. [Google Scholar] [CrossRef]
- Važanić, D. Out-of-Hospital Cardiac Arrest Outcomes—Bystander Cardiopulmonary Resuscitation Rate Improvement. Acta Clin. Croat. 2022, 61, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Zalihić, A.; Šljivo, A.; Ribić, E.; Gavranović, A.; Brigić, L. Bystanders’ Cardiopulmonary Resuscitation Involvement in the Treatment of out-of-Hospital Cardiac Arrest Events and Educational Status Regarding Basic Life Support Measures and Automated External Defibrillator Usage among Residents in Canton Sarajevo, Bosnia and Herzegovina. Med. Glas. Ljek. Komore Zenicko-Doboj. Kantona 2022, 9, 127–133. [Google Scholar] [CrossRef]
- Zaletel, M.; Vardič, D.; Hladnik, M. Zdravstveni Statistični Letopis Slovenije 2022; Nacionalni Inštitut za Javno Zdravje: Ljubljana, Slovenia, 2024. [Google Scholar]
- Ručigaj, S.; Demšar, L. AED Baza Slovenije: Stanje Evidence Javno Dostopnih Naprav AED in Ažurnost Informacij o Napravah Vpisanih v Bazo = A Follow-up on Slovenian Public-Access AEDs Database. In Urgentna Medicina: Izbrana Poglavja 2018; Slovensko združenje za Urgentno Medicino = Slovenian Society for Emergency Medicine: Ljubljana, Slovenia, 2018; pp. 370–373. [Google Scholar]
- Mateja, Kotnik Veliko Mladih Živi Skupaj s Starši, Čedalje več Starejših Prebiva Samih. Delo. 2022. Available online: https://www.delo.si/novice/slovenija/od-starsev-se-odselijo-pri-starosti-296-leta (accessed on 22 February 2024).
- Brooks, S.C. Public Access Defibrillation Is a Failed Strategy. Can. J. Emerg. Med. 2024, 26, 5–6. [Google Scholar] [CrossRef]
- Chan, P.S.; Krumholz, H.M.; Spertus, J.A.; Jones, P.G.; Cram, P.; Berg, R.A.; Peberdy, M.A.; Nadkarni, V.; Mancini, M.E.; Nallamothu, B.K. Automated External Defibrillators and Survival After In-Hospital Cardiac Arrest. JAMA 2010, 304, 2129–2136. [Google Scholar] [CrossRef]
- Elhussain, M.O.; Ahmed, F.K.; Mustafa, N.M.; Mohammed, D.O.; Mahgoub, I.M.; Alnaeim, N.A.; Ali, R.; Bushra, N.; Ahamed, H.K.; Abdelrahman, N. The Role of Automated External Defibrillator Use in the Out-of-Hospital Cardiac Arrest Survival Rate and Outcome: A Systematic Review. Cureus 2023, 15, e47721. [Google Scholar] [CrossRef]
- Strnad, M.; Borovnik Lesjak, V.; Jerot, P.; Esih, M. Prehospital Predictors of Survival in Patients with Out-of-Hospital Cardiac Arrest. Medicina 2023, 59, 1717. [Google Scholar] [CrossRef] [PubMed]
- Rucigaj, S.; Podobnik, B.; Gradisek, P.; Sostaric, M. “AED Database of Slovenia”—An Analysis of Operation of Slovenian National Public Access Defibrillators Registry. Resuscitation 2019, 142, e47–e48. [Google Scholar] [CrossRef]
- Rao, P.; Kern, K.B. Improving Community Survival Rates from Out-of-Hospital Cardiac Arrest. Curr. Cardiol. Rev. 2018, 14, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Chocron, R.; Jobe, J.; Guan, S.; Kim, M.; Shigemura, M.; Fahrenbruch, C.; Rea, T. Bystander Cardiopulmonary Resuscitation Quality: Potential for Improvements in Cardiac Arrest Resuscitation. J. Am. Heart Assoc. 2021, 10, e017930. [Google Scholar] [CrossRef] [PubMed]
- Noc, M.; Weil, M.H.; Tang, W.; Turner, T.; Fukui, M. Mechanical Ventilation May Not Be Essential for Initial Cardiopulmonary Resuscitation. Chest 1995, 108, 821–827. [Google Scholar] [CrossRef]
- Hallstrom, A.; Cobb, L.; Johnson, E.; Copass, M. Cardiopulmonary Resuscitation by Chest Compression Alone or with Mouth-to-Mouth Ventilation. N. Engl. J. Med. 2000, 342, 1546–1553. [Google Scholar] [CrossRef]
- Virkkunen, I.; Kujala, S.; Ryynänen, S.; Vuori, A.; Pettilä, V.; Yli-Hankala, A.; Silfvast, T. Bystander Mouth-to-Mouth Ventilation and Regurgitation during Cardiopulmonary Resuscitation. J. Intern. Med. 2006, 260, 39–42. [Google Scholar] [CrossRef] [PubMed]
- SOS-KANTO Study Group. Cardiopulmonary Resuscitation by Bystanders with Chest Compression Only (SOS-KANTO): An Observational Study. Lancet 2007, 369, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Cabrini, L.; Biondi-Zoccai, G.; Landoni, G.; Greco, M.; Vinciguerra, F.; Greco, T.; Ruggeri, L.; Sayeg, J.; Zangrillo, A. Bystander-Initiated Chest Compression-Only CPR Is Better than Standard CPR in out-of-Hospital Cardiac Arrest. HSR Proc. Intensive Care Cardiovasc. Anesth. 2010, 2, 279–285. [Google Scholar]
- Pourghaderi, A.R.; Kogtikov, N.; Lees, M.H.; Cai, W.; Pin Pek, P.; Fu Wah Ho, A.; Ming Ng, W.; Kwak, J.; Elgin White, A.; Lynn Lim, S.; et al. Maximum Expected Survival Rate Model for Public Access Defibrillator Placement. Resuscitation 2022, 170, 213–221. [Google Scholar] [CrossRef]
- Birkun, A.; Gautam, A.; Trunkwala, F. Global Prevalence of Cardiopulmonary Resuscitation Training among the General Public: A Scoping Review. Clin. Exp. Emerg. Med. 2021, 8, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Rajapakse, R.; Noč, M.; Kersnik, J. Public Knowledge of Cardiopulmonary Resuscitation in Republic of Slovenia. Wien. Klin. Wochenschr. 2010, 122, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Generacija Rešuje Življenja|ZD Litija. Available online: https://zd-litija.si/generacija-resuje-zivljenja/ (accessed on 22 February 2024).
- Osnovnošolske Ekipe Prve Pomoči—Rdeči Križ Slovenije—Območno Združenje Ljubljana. Available online: https://www.rdecikrizljubljana.si/sl/Osnovnosolske_ekipe_prve_pomoci/ (accessed on 22 February 2024).
- Vajd, R.; Gričar, M.; Prestor, J.; Bračko, V. (Eds.) Mednarodni Simpozij o Urgentni Medicini, 24 Urgentna Medicina: Izbrana Poglavja 2017: Zbornik = International Symposium of Emergency Medicine, 24 Emergency Medicine: Choosen Topics 2017; Slovensko Združenje za Urgentno Medicino = Slovenian Society for Emergency Medicine: Ljubljana, Slovenia, 2017; p. 409. [Google Scholar]
- Vajd, R.; Zelinka, M. (Eds.) Mednarodni Simpozij o Urgentni Medicini, 29 Urgentna Medicina = International Symposium of Emergency Medicine, 29 Emergency Medicine: Choosen Topics 2023; Slovensko Združenje za Urgentno Medicino = Slovenian Society for Emergency Medicine: Ljubljana, Slovenia, 2023; p. 360. [Google Scholar]
- Wissenberg, M.; Lippert, F.K.; Folke, F.; Weeke, P.; Hansen, C.M.; Christensen, E.F.; Jans, H.; Hansen, P.A.; Lang-Jensen, T.; Olesen, J.B.; et al. Association of National Initiatives to Improve Cardiac Arrest Management with Rates of Bystander Intervention and Patient Survival After Out-of-Hospital Cardiac Arrest. JAMA 2013, 310, 1377–1384. [Google Scholar] [CrossRef] [PubMed]
- Simmons, K.M.; McIsaac, S.M.; Ohle, R. Impact of Community-Based Interventions on out-of-Hospital Cardiac Arrest Outcomes: A Systematic Review and Meta-Analysis. Sci. Rep. 2023, 13, 10231. [Google Scholar] [CrossRef]
- Schroeder, D.C.; Semeraro, F.; Greif, R.; Bray, J.; Morley, P.; Parr, M.; Kondo Nakagawa, N.; Iwami, T.; Finke, S.-R.; Malta Hansen, C.; et al. KIDS SAVE LIVES: Basic Life Support Education for Schoolchildren: A Narrative Review and Scientific Statement from the International Liaison Committee on Resuscitation. Circulation 2023, 147, 1854–1868. [Google Scholar] [CrossRef]

| Measure | All Cases (n, %) |
|---|---|
| Population served (n) | 1,520,895 |
| Total number of cases | 294 |
| Resuscitation attempted | 206 (70.0) |
| Mean age in years (SD) | 69.73 (16.67) |
| Male gender | 199 (67.7) |
| Location of collapse | |
| At home | 203 (69) |
| At work | 1 (0) |
| Place of sports/recreation | 2 (1) |
| Street/highway | 34 (12) |
| Public building | 5 (2) |
| Residential care/nursing home | 16 (5) |
| Educational institution | 0 (0) |
| Other | 32 (11) |
| Witnessed collapse | |
| Bystander | 168 (57) |
| EMS | 32 (11) |
| Unwitnessed | 92 (31) |
| Unknown | 2 (1) |
| Bystander response | |
| Bystander CPR | |
| no CPR | 92 (31) |
| bCPR | 22 (7) |
| CCs only | 127 (43) |
| CPR but no further details provided | 13 (4) |
| Unknown | 40 (13) |
| AED use before EMS arrival | |
| Analyze | 58 (20) |
| Shock | 17 (6) |
| First rhythm (% of resuscitation attempted cases) | |
| Ventricular fibrillation | 41 (14) |
| Ventricular tachycardia | 2 (1) |
| Pulseless electrical activity | 43 (15) |
| Asystole | 63 (21) |
| Bradycardia | 2 (1) |
| AED non-shockable | 35 (12) |
| AED shockable | 17 (6) |
| Not recorded | 0 (0) |
| Etiology | |
| Cardiac/medical | 216 (73) |
| Trauma | 24 (8) |
| Overdose | 2 (1) |
| Drowning | 0 (0) |
| Electrocution | 0 (0) |
| Asphyxia | 12 (4) |
| Not recorded | 40 (14) |
| EMS Process | |
| First responder activated | 60 (20) |
| First responder performed CPR | 60 (20) |
| First defibrillation time (mean, mm:ss) | 25:16 |
| Drugs given | 150 (51) |
| Hospital Process | |
| Reperfusion attempted | 30 (10) |
| Organ donation | 3 (1) |
| Targeted temp control | |
| Indicated—done | 24 (8) |
| Indicated—not done | 0 (0) |
| Not indicated | 30 (10) |
| Unknown | 227 (77) |
| Dispatcher process | |
| Dispatcher ID CA | |
| Yes | 198 (67) |
| No | 30 (10) |
| Unknown | 66 (22) |
| Dispatcher CPR | |
| Yes | 241 (82) |
| No | 53 (18) |
| Unknown | 0 (0) |
| Outcomes (% of those where resuscitation was attempted) | |
| ROSC | 85 (41) |
| Survival to hospital | |
| Ongoing CPR | 11 (5) |
| Alive with ROSC | 68 (33) |
| Survival | |
| To hospital discharge | 27 (13) |
| 30 days | 30 (14) |
| Neurological outcomes on discharge | |
| CPC 1–2 | 26 (13) |
| mRS 0–3 | 17 (8) |
| Resuscitation not attempted | |
| DNAR | 33 (11) |
| Obviously dead | 55 (19) |
| Signs of life | 0 (0) |
| Bystander Response | Dispatcher Gave CPR Instructions | Dispatcher Did Not Give CPR Instructions | ||
|---|---|---|---|---|
| EMS Performed CPR (n, %) | EMS Did Not Perform CPR (n, %) | EMS Performed CPR (n, %) | EMS Did Not Perform CPR (n, %) | |
| Chest compressions | 105 (51%) | 18 (51%) | 0 | 4 (8%) |
| Chest compressions together with ventilation | 21 (10%) | 0 | 0 | 1 (2%) |
| No bystander CPR | 45 (22%) | 13 (37%) | 0 | 34 (64%) |
| Unknown | 35 (17%) | 4 (11%) | 0 | 14 (26%) |
| SUM | 206 | 35 | 0 | 53 |
| Outcome Evaluated | R2 | Mean Age + CI of Those Who Survived until Hospital Discharge | Mean Age + CI of Those Who Did Not Survive | Mean Response Time + CI Those Who Survived until Hospital Discharge | Mean Response Time + CI Those Who Did Not Survive | % of Males in Cohort That Survived until Hospital Discharge | % of Males in Cohort That Did Not Survive |
|---|---|---|---|---|---|---|---|
| ROSC S = 85 DNS = 121 | −0.615886171 | 66.02 (62.6–69.44) | 70.68 (67.93–73.42) N = 121 | 10 min 43 s (9 min 32.6 s–11 min 55.12 s) | 14 min 32 s (12 min 16 s–16 min 48 s) | 69.41 (59) | 66.27 (169) |
| 30-day survival S = 27 DNS = 255 | −0.486323581 | 58.81 (53.88–63.75) | 70.84 (68.82–72.86) N = 255 | 9 min 41 s (87 min 43.47 s–11 min 44 s) | 13 min 20 s (12 min 4 s–14 min 35 s) | 85.18 (23) | 71.07 (86) |
| Survival to discharge S = 27 DNS = 254 | −0.359089312 | 58.48 (53.63–63.33) | 70.87 (68.85–72.89) N = 254 | 8 min 56.48 s (7 min 32.31 s–10 min 20.64 s) | 13 min 20 s (12 min 4 s–14 min 35 s) | 85.18 (23) | 66.14 (168) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petravić, L.; Miklič, R.; Burger, E.; Keše, U.; Kulovec, D.; Poljanšek, E.; Tomšič, G.; Pintarič, T.; Lopes, M.F.; Brezovnik, M.; et al. Enhancing Bystander Intervention: Insights from the Utstein Analysis of Out-of-Hospital Cardiac Arrests in Slovenia. Medicina 2024, 60, 1227. https://doi.org/10.3390/medicina60081227
Petravić L, Miklič R, Burger E, Keše U, Kulovec D, Poljanšek E, Tomšič G, Pintarič T, Lopes MF, Brezovnik M, et al. Enhancing Bystander Intervention: Insights from the Utstein Analysis of Out-of-Hospital Cardiac Arrests in Slovenia. Medicina. 2024; 60(8):1227. https://doi.org/10.3390/medicina60081227
Chicago/Turabian StylePetravić, Luka, Rok Miklič, Evgenija Burger, Urša Keše, Domen Kulovec, Eva Poljanšek, Gašper Tomšič, Tilen Pintarič, Miguel Faria Lopes, Miha Brezovnik, and et al. 2024. "Enhancing Bystander Intervention: Insights from the Utstein Analysis of Out-of-Hospital Cardiac Arrests in Slovenia" Medicina 60, no. 8: 1227. https://doi.org/10.3390/medicina60081227
APA StylePetravić, L., Miklič, R., Burger, E., Keše, U., Kulovec, D., Poljanšek, E., Tomšič, G., Pintarič, T., Lopes, M. F., Brezovnik, M., & Strnad, M. (2024). Enhancing Bystander Intervention: Insights from the Utstein Analysis of Out-of-Hospital Cardiac Arrests in Slovenia. Medicina, 60(8), 1227. https://doi.org/10.3390/medicina60081227







