Safety and Early Return to Sports for Early ACL Reconstruction in Young Athletes: A Retrospective Study
Abstract
:1. Introduction
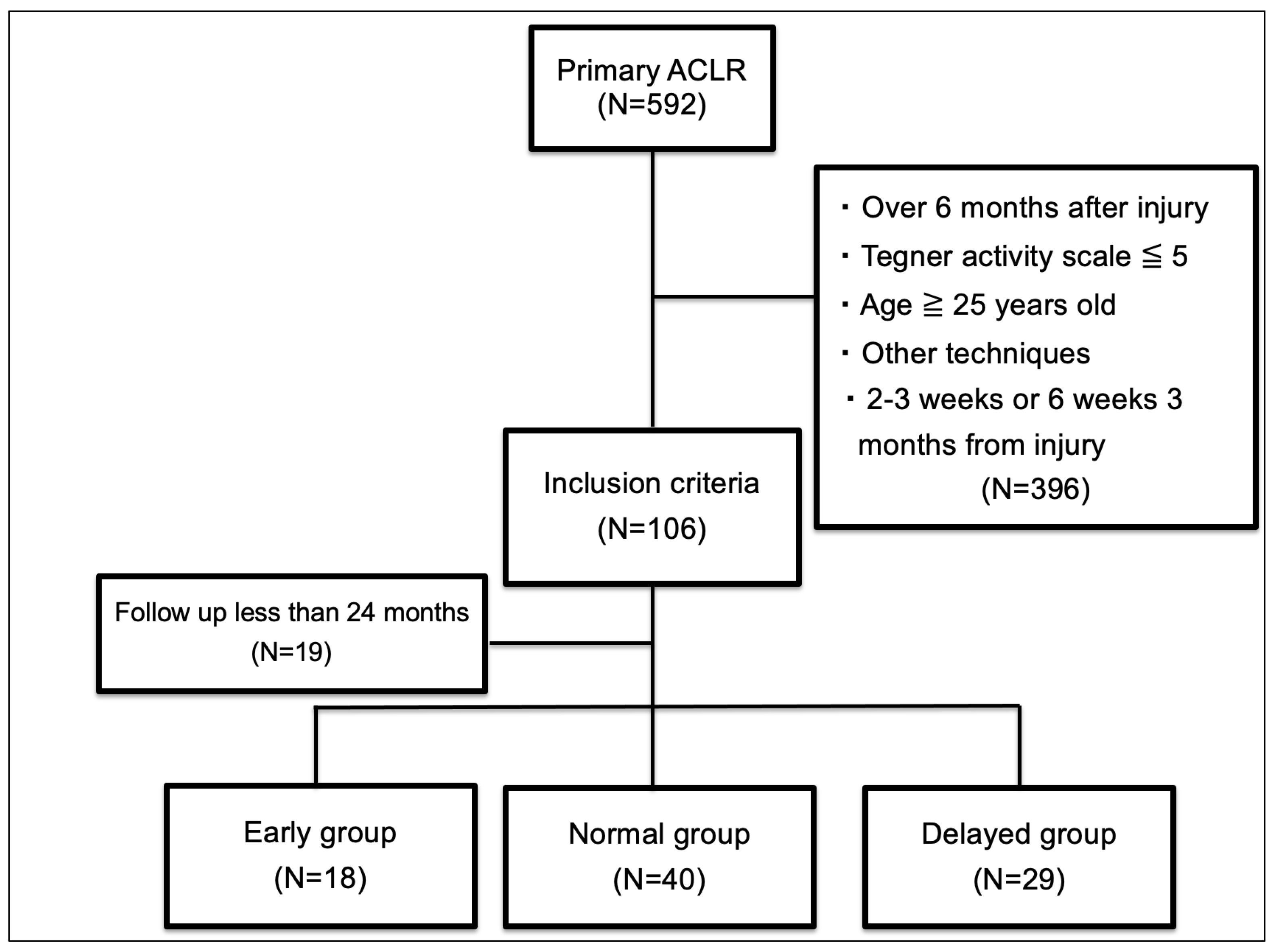
2. Materials and Methods
3. Results
3.1. Patient Characteristics
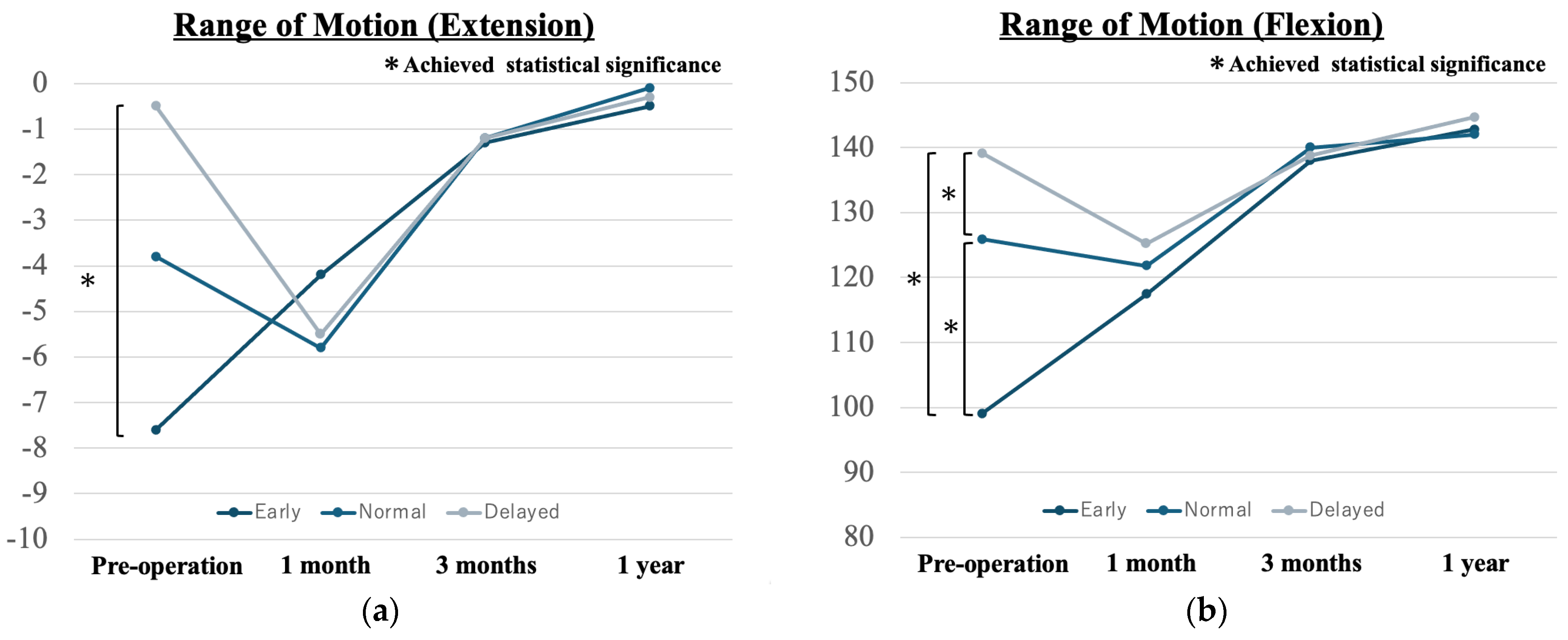
3.2. Postoperative Complications
3.3. Postoperative Sports Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shelbourne, K.D.; Wilckens, J.H.; Mollabashy, A.; DeCarlo, M. Arthrofibrosis in Acute Anterior Cruciate Ligament Reconstruction. The Effect of Timing of Reconstruction and Rehabilitation. Am. J. Sport. Med. 1991, 19, 332–336. [Google Scholar] [CrossRef]
- Almekinders, L.C.; Moore, T.; Freedman, D.; Taft, T.N. Post-Operative Problems following Anterior Cruciate Ligament Reconstruction. Knee Surg. Sport. Traumatol. Arthrosc. 1995, 3, 78–82. [Google Scholar] [CrossRef]
- Wasilewski, S.A.; Covall, D.J.; Cohen, S. Effect of Surgical Timing on Recovery and Associated Injuries after Anterior Cruciate Ligament Reconstruction. Am. J. Sport. Med. 1993, 21, 338–342. [Google Scholar] [CrossRef]
- Sachs, R.A.; Daniel, D.M.; Stone, M.L.; Garfein, R.F. Patellofemoral Problems after Anterior Cruciate Ligament Reconstruction. Am. J. Sport. Med. 1989, 17, 760–765. [Google Scholar] [CrossRef]
- Bottoni, C.R.; Liddell, T.R.; Trainor, T.J.; Freccero, D.M.; Lindell, K.K. Postoperative Range of Motion following Anterior Cruciate Ligament Reconstruction Using Autograft Hamstrings: A Prospective, Randomized Clinical Trial of Early versus Delayed Reconstructions. Am. J. Sport. Med. 2008, 36, 656–662. [Google Scholar] [CrossRef]
- Herbst, E.; Hoser, C.; Gföller, P.; Hepperger, C.; Abermann, E.; Neumayer, K.; Musahl, V.; Fink, C. Impact of Surgical Timing on the Outcome of Anterior Cruciate Ligament Reconstruction. Knee Surg. Sport. Traumatol. Arthrosc. 2016, 25, 569–577. [Google Scholar] [CrossRef]
- Ferguson, D.; Palmer, A.; Khan, S.; Oduoza, U.; Atkinson, H. Early or Delayed Anterior Cruciate Ligament Reconstruction: Is One Superior? A Systematic Review and Meta-Analysis. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1277–1289. [Google Scholar] [CrossRef]
- Kwok, C.S.; Harrison, T.; Servant, C. The Optimal Timing for Anterior Cruciate Ligament Reconstruction with Respect to the Risk of Postoperative Stiffness. Arthroscopy 2013, 29, 556–565. [Google Scholar] [CrossRef]
- Eriksson, K.; von Essen, C.; Jönhagen, S.; Barenius, B. No Risk of Arthrofibrosis after Acute Anterior Cruciate Ligament Reconstruction. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 26, 2875–2882. [Google Scholar] [CrossRef]
- von Essen, C.; Eriksson, K.; Barenius, B. Acute ACL Reconstruction Shows Superior Clinical Results and Can Be Performed Safely without an Increased Risk of Developing Arthrofibrosis. Knee Surg. Sport. Traumatol. Arthrosc. 2019, 28, 2036–2043. [Google Scholar] [CrossRef]
- Raviraj, A.; Anand, A.; Kodikal, G.; Chandrashekar, M.; Pai, S. A Comparison of Early and Delayed Arthroscopically-Assisted Reconstruction of the Anterior Cruciate Ligament Using Hamstring Autograft. J. Bone Jt. Surgery. Br. Vol. 2010, 92, 521–526. [Google Scholar] [CrossRef]
- Shen, X.; Liu, T.; Xu, S.; Chen, B.; Tang, X.; Xiao, J.; Qin, Y. Optimal Timing of Anterior Cruciate Ligament Reconstruction in Patients with Anterior Cruciate Ligament Tear: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2022, 5, e2242742. [Google Scholar] [CrossRef]
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of Secondary Injury in Younger Athletes after Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Am. J. Sport. Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef]
- Yamanashi, Y.; Mutsuzaki, H.; Iwai, K.; Ikeda, K.; Kinugasa, T. Failure Risks in Anatomic Single-Bundle Anterior Cruciate Ligament Reconstruction via the Outside-in Tunnel Technique Using a Hamstring Autograft. J. Orthop. 2019, 16, 504–507. [Google Scholar] [CrossRef]
- Hefti, E.; Müller, W.; Jakob, R.P.; Stäubli, H.U. Evaluation of Knee Ligament Injuries with the IKDC Form. Knee Surg. Sport. Traumatol. Arthrosc. 1993, 1, 226–234. [Google Scholar] [CrossRef]
- Mayr, H.O.; Weig, T.G.; Plitz, W. Arthrofibrosis following ACL Reconstruction—Reasons and Outcome. Arch. Orthop. Trauma Surg. 2004, 124, 518–522. [Google Scholar] [CrossRef]
- Meighan, A.A.S.; Keating, J.F.; Will, E. Outcome after Reconstruction of the Anterior Cruciate Ligament in Athletic Patients. A Comparison of Early Versus Delayed Surgery. J. Bone Jt. Surgery. Br. Vol. 2003, 85, 521–524. [Google Scholar] [CrossRef]
- Robertson, G.A.; Coleman, S.G.; Keating, J.F. Knee Stiffness following Anterior Cruciate Ligament Reconstruction: The Incidence and Associated Factors of Knee Stiffness following Anterior Cruciate Ligament Reconstruction. Knee 2009, 16, 245–247. [Google Scholar] [CrossRef]
- Svantesson, E.; Sundemo, D.; Senorski, E.H.; Alentorn-Geli, E.; Musahl, V.; Fu, F.H.; Desai, N.; Stalman, A.; Samuelsson, K. Double-Bundle Anterior Cruciate Ligament Reconstruction Is Superior to Single-Bundle Reconstruction in Terms of Revision Frequency: A Study of 22,460 Patients from the Swedish National Knee Ligament Register. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 3884–3891. [Google Scholar] [CrossRef]
- Suomalainen, P.; Moisala, A.S.; Paakkala, A.; Kannus, P.; Jarvela, T. Double-Bundle versus Single-Bundle Anterior Cruciate Ligament Reconstruction: Randomized Clinical and Magnetic Resonance Imaging Study with 2-Year Follow-Up. Am. J. Sport. Med. 2011, 39, 1615–1622. [Google Scholar] [CrossRef]
- Grindem, H.; Snyder-Mackler, L.; Moksnes, H.; Engebretsen, L.; Risberg, M.A. Simple Decision Rules Can Reduce Reinjury Risk by 84% after ACL Reconstruction: The Delaware-Oslo ACL Cohort Study. Br. J. Sport. Med. 2016, 50, 804–808. [Google Scholar] [CrossRef] [PubMed]
- Hanada, M.; Yoshikura, T.; Matsuyama, Y. Muscle Recovery at 1 Year after the Anterior Cruciate Ligament Reconstruction Surgery Is Associated with Preoperative and Early Postoperative Muscular Strength of the Knee Extension. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1759–1764. [Google Scholar] [CrossRef]
- Logerstedt, D.; Lynch, A.; Axe, M.J.; Snyder-Mackler, L. Pre-Operative Quadriceps Strength Predicts IKDC2000 Scores 6 Months after Anterior Cruciate Ligament Reconstruction. Knee 2012, 20, 208–212. [Google Scholar] [CrossRef]
- Eitzen, I.; Holm, I.; A Risberg, M. Preoperative Quadriceps Strength Is a Significant Predictor of Knee Function Two Years after Anterior Cruciate Ligament Reconstruction. Br. J. Sport. Med. 2009, 43, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.C.; Wojtys, E.M.; Brandon, C.; Palmieri-Smith, R.M. Muscle Atrophy Contributes to Quadriceps Weakness after Anterior Cruciate Ligament Reconstruction. J. Sci. Med. Sport 2015, 19, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Iriuchishima, T.; Shirakura, K.; Horaguchi, T.; Wada, N.; Sohmiya, M.; Tazawa, M.; Fu, F.H. Age as a Predictor of Residual Muscle Weakness after Anterior Cruciate Ligament Reconstruction. Knee Surg. Sport. Traumatol. Arthrosc. 2011, 20, 173–178. [Google Scholar] [CrossRef]
- Brown, M.; A Hurlburt, G.; A Koenig, Z.; Richards, D. The Multivariate Relationship between Primary Anterior Cruciate Ligament Reconstruction Timing and Revision Rates: A 10-Year Analysis. Cureus 2022, 14, e21023. [Google Scholar] [CrossRef]
- Kennedy, J.; Jackson, M.P.; O’kelly, P.; Moran, R. Timing of Reconstruction of the Anterior Cruciate Ligament in Athletes and the Incidence of Secondary Pathology within the Knee. J. Bone Jt. Surgery. Br. Vol. 2010, 92, 362–366. [Google Scholar] [CrossRef]
- Duchman, K.R.; Westermann, R.W.; Spindler, K.P.; Reinke, E.K.; Huston, L.J.; Amendola, A.; Group, M.K.; Wolf, B.R. The Fate of Meniscus Tears Left In Situ at the Time of Anterior Cruciate Ligament Reconstruction: A 6-Year Follow-up Study from the Moon Cohort. Am. J. Sport. Med. 2015, 43, 2688–2695. [Google Scholar] [CrossRef]
- Weiss, C.B.; Lundberg, M.; Hamberg, P.; E DeHaven, K.; Gillquist, J. Non-Operative Treatment of Meniscal Tears. J. Bone Jt. Surg. 1989, 71, 811–822. [Google Scholar] [CrossRef]
| Characteristics | Early Group (N = 18) | Normal Group (N = 40) | Delayed Group (N = 29) | p Value | Effect Size | Power |
|---|---|---|---|---|---|---|
| Mean time; injury to operation (day) | 4.2 ± 1.5 (2–7) | 32.7 ± 5.8 (22–42) | 122.2 ± 25.8 (90–179) | <0.01 * | 0.93 | 1.0 |
| Age (year) | 19.9 ± 3.0 (14–25) | 19.3 ± 3.0 (15–25) | 17.2 ± 2.8 (14–24) | <0.01 * | 0.23 | 0.8 |
| Height (cm) | 163.1 ± 9.1 (152–183) | 164.1 ± 8.3 (151–182) | 163.3 ± 8.2 (152–180) | 0.88 | 0.04 | 0.07 |
| Weight (kg) | 61.6 ± 10.3 (51–84) | 62.4 ± 14.2 (46–106) | 61.6 ± 12.1 (41–85) | 0.96 | 0.14 | 0.57 |
| Male | 7 | 11 | 9 | 0.69 | 0.09 | 0.11 |
| Female | 11 | 29 | 20 | |||
| Mean TAS | 7.4 ± 1.2 | 7.1 ± 1.0 | 6.8 ± 0.6 | 0.09 | 0.16 | 0.48 |
| 6 | 6 | 12 | 9 | |||
| 7 | 4 | 20 | 19 | |||
| 8 | 2 | 1 | 0 | |||
| 9 | 4 | 7 | 1 | |||
| 10 | 2 | 0 | 0 | |||
| Total meniscus tear | 11 | 20 | 15 | 0.73 | 0.09 | 0.73 |
| MM tear | 1 | 2 | 1 | 0.93 | ||
| LM tear | 7 | 16 | 11 | 0.98 | ||
| MM + LM tear | 3 | 2 | 3 | 0.35 | ||
| Concomitant meniscal suture | 10 | 17 | 15 | 0.59 | 0.11 | 0.14 |
| Early Group N = 18 | Normal Group N = 40 | Delayed Group N = 29 | p Value | Effect Size | Power | |
|---|---|---|---|---|---|---|
| Total complications | 6 (33.3%) | 9 (22.5%) | 6 (20.7%) | 0.11 | 0.14 | |
| Graft rupture | 2 (11.1%) | 5 (12.5%) | 2 (6.9%) | 0.75 | ||
| Contralateral injury | 2 (11.1%) | 2 (5%) | 3(10.3%) | 0.63 | ||
| Meniscal tear | 1 (5.6%) | 1 (2.5%) | 1 (3.4%) | 0.84 | ||
| Manipulation | 1 (5.6%) | 1 (2.5%) | 0 (0%) | 0.46 | ||
| Infection | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Fracture | 0 (0%) | 0 (0%) | 0 (0%) | |||
| KT-1000 | N = 11 | N = 30 | N = 18 | 0.42 | 0.42 | 0.15 |
| ≤−2 mm | 0% (0/11) | 3.3% (1/30) | 5.6% (1/18) | |||
| −1~2 mm | 100% (11/11) | 83.3% (25/30) | 83.3% (15/18) | |||
| ≥3 mm | 0% (0/11) | 13.3% (4/30) | 11.1% (2/18) |
| Early Group | Normal Group | Delayed Group | p Value | Effect Size | Power | |
|---|---|---|---|---|---|---|
| 3 months | N = 14 | N = 30 | N = 22 | |||
| Hamstrings (%) | 69.5 ± 17.2 | 74.6 ± 14.7 | 79.6 ± 14.0 | 0.15 | 0.18 | 0.39 |
| Quadriceps (%) | 69.2 ± 15.5 | 73.9 ± 19.2 | 73.5 ± 12.3 | 0.66 | 0.09 | 0.12 |
| 6 months | N = 15 | N = 20 | N = 20 | |||
| Hamstrings (%) | 87.5 ± 16.9 | 88.2 ± 19.4 | 87.3 ± 10.1 | 0.98 | 0 | 0.05 |
| Quadriceps (%) | 81.2 ± 16.2 | 80.6 ± 16.6 | 82.1 ± 10.1 | 0.95 | 0.03 | 0.06 |
| 1 year | N = 12 | N = 30 | N = 20 | |||
| Lysholm score | 98.3 ± 2.5 | 98.9 ± 2.4 | 98.2 ± 4.9 | 0.80 | 0.01 | 0.08 |
| Mean TAS | 7.9 ± 1.7 | 6.9 ± 1.0 | 6.7 ± 1.0 | 0.01 * | 0.15 | 0.81 |
| 4 | 1 | 0 | 1 | |||
| 5 | 0 | 1 | 1 | |||
| 6 | 1 | 6 | 5 | |||
| 7 | 3 | 18 | 14 | |||
| 8 | 2 | 1 | 0 | |||
| 9 | 3 | 3 | 1 | |||
| 10 | 2 | 0 | 0 | |||
| Time to return to sport from injury (months) | 8.6 ± 1.6 | 10.2 ± 1.9 | 14.1 ± 2.8 | <0.01 * | 0.5 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamanashi, Y.; Mutsuzaki, H.; Kawashima, T.; Ikeda, K.; Deie, M.; Kinugasa, T. Safety and Early Return to Sports for Early ACL Reconstruction in Young Athletes: A Retrospective Study. Medicina 2024, 60, 1229. https://doi.org/10.3390/medicina60081229
Yamanashi Y, Mutsuzaki H, Kawashima T, Ikeda K, Deie M, Kinugasa T. Safety and Early Return to Sports for Early ACL Reconstruction in Young Athletes: A Retrospective Study. Medicina. 2024; 60(8):1229. https://doi.org/10.3390/medicina60081229
Chicago/Turabian StyleYamanashi, Yuki, Hirotaka Mutsuzaki, Tatsuhiro Kawashima, Kotaro Ikeda, Masataka Deie, and Tomonori Kinugasa. 2024. "Safety and Early Return to Sports for Early ACL Reconstruction in Young Athletes: A Retrospective Study" Medicina 60, no. 8: 1229. https://doi.org/10.3390/medicina60081229




