Predictive Value of Serial Rapid Shallow Breathing Index Measurements for Extubation Success in Intensive Care Unit Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
2.2. Study Design
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mehta, A.B.; Syeda, S.N.; Wiener, R.S.; Walkey, A.J. Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. J. Crit. Care 2015, 30, 1217–1221. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.N.; Ganatra, K.D.; Bates, J.H.; Young, M.P. Variation in the rapid shallow breathing index associated with common measurement techniques and conditions. Respir. Care 2009, 54, 1462–1466. [Google Scholar] [PubMed]
- Walsh, T.S.; Dodds, S.; McArdle, F. Evaluation of simple criteria to predict successful weaning from mechanical ventilation in intensive care patients. Br. J. Anaesth. 2004, 92, 793–799. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rose, L.; Adhikari, N.K.; Leasa, D.; Fergusson, D.A.; McKim, D. Cough augmentation techniques for extubation or weaning critically ill patients from mechanical ventilation. Cochrane Database Syst. Rev. 2017, 1, CD011833. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, C.; Maccari, J.G.; Vieira, S.R.; Oliveira, R.P.; Savi, A.; Machado, A.S.; Tonietto, T.F.; Cremonese, R.V.; Wickert, R.; Pinto, K.B.; et al. Impact of a mechanical ventilation weaning protocol on the extubation failure rate in difficult-to-wean patients. J. Bras. Pneumol. 2012, 38, 364–371. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Perren, A.; Previsdomini, M.; Llamas, M.; Cerutti, B.; Györik, S.; Merlani, G.; Jolliet, P. Patients’ prediction of extubation success. Intensive Care Med. 2010, 36, 2045–2052. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.L.; Tobin, M.J. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N. Engl. J. Med. 1991, 324, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- Fadaii, A.; Amini, S.S.; Bagheri, B.; Taherkhanchi, B. Assessment of rapid shallow breathing index as a predictor for weaning in respiratory care unit. Tanaffos 2012, 11, 28–31. [Google Scholar] [PubMed]
- Baptistella, A.R.; Mantelli, L.M.; Matte, L.; Carvalho, M.E.D.R.U.; Fortunatti, J.A.; Costa, I.Z.; Haro, F.G.; Turkot, V.L.O.; Baptistella, S.F.; de Carvalho, D.; et al. Prediction of extubation outcome in mechanically ventilated patients: Development and validation of the Extubation Predictive Score (ExPreS). PLoS ONE 2021, 16, e0248868. [Google Scholar] [CrossRef]
- Boles, J.M.; Bion, J.; Connors, A.; Herridge, M.; Marsh, B.; Melot, C.; Pearl, R.; Silverman, H.; Stanchina, M.; Vieillard-Baron, A.; et al. Weaning from mechanical ventilation. Eur. Respir. J. 2007, 29, 1033–1056. [Google Scholar] [CrossRef]
- Song, J.; Qian, Z.; Zhang, H.; Wang, M.; Yu, Y.; Ye, C.; Hu, W.; Gong, S. Diaphragmatic ultrasonography-based rapid shallow breathing index for predicting weaning outcome during a pressure support ventilation spontaneous breathing trial. BMC Pulm. Med. 2022, 22, 337. [Google Scholar] [CrossRef] [PubMed]
- Soo Hoo, G.W.; Park, L. Variations in the measurement of weaning parameters: A survey of respiratory therapists. Chest 2002, 121, 1947–1955. [Google Scholar] [CrossRef] [PubMed]
- Shingala, H.B.; Abouzgheib, W.B.; Darrouj, J.; Pratter, M.R. Comparison of rapid shallow breathing index measured on pressure support ventilation and spontaneous breathing trial to predict weaning from mechanical ventilation. Chest 2009, 136, 32S. [Google Scholar] [CrossRef]
- Karthika, M.; Al Enezi, F.A.; Pillai, L.V.; Arabi, Y.M. Rapid shallow breathing index. Ann. Thorac. Med. 2016, 11, 167–176. [Google Scholar] [PubMed]
- Tanios, M.A.; Nevins, M.L.; Hendra, K.P.; Cardinal, P.; Allan, J.E.; Naumova, E.N.; Epstein, S.K. A randomized, controlled trial of the role of weaning predictors in clinical decision making. Crit. Care Med. 2006, 34, 2530–2535. [Google Scholar] [CrossRef]
- Purro, A.; Appendini, L.; De Gaetano, A.; Gudjonsdottir, M.; Donner, C.F.; Rossi, A. Physiologic determinants of ventilator dependence in long-term mechanically ventilated patients. Am. J. Respir. Crit. Care Med. 2000, 161, 1115–1123. [Google Scholar] [CrossRef] [PubMed]
- Danaga, A.R.; Gut, A.L.; Antunes, L.C.; Ferreira, A.L.; Yamaguti, F.A.; Christovan, J.C.; Teixeira, U.; Guedes, C.A.; Sasseron, A.B.; Martin, L.C. Evaluation of the diagnostic performance and cut-off value for the rapid shallow breathing index in predicting extubation failure. J. Bras. Pneumol. 2009, 35, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Chao, D.C.; Scheinhorn, D.J. Determining the best threshold of rapid shallow breathing index in a therapist-implemented patient-specific weaning protocol. Respir. Care 2007, 52, 159–165. [Google Scholar] [PubMed]
- Verceles, A.C.; Diaz-Abad, M.; Geiger-Brown, J.; Scharf, S.M. Testing the prognostic value of the rapid shallow breathing index in predicting successful weaning in patients requiring prolonged mechanical ventilation. Heart Lung 2012, 41, 546–552. [Google Scholar] [CrossRef]
- Dos Reis, H.F.; Almeida, M.L.; da Silva, M.F.; Moreira, J.O.; Rocha, M. de S. Association between the rapid shallow breathing index and extubation success in patients with traumatic brain injury. Rev. Bras. Ter. Intensiva 2013, 25, 212–217. [Google Scholar] [CrossRef]
- Boutou, A.K.; Abatzidou, F.; Tryfon, S.; Nakou, C.; Pitsiou, G.; Argyropoulou, P.; Stanopoulos, I. Diagnostic accuracy of the rapid shallow breathing index to predict a successful spontaneous breathing trial outcome in mechanically ventilated patients with chronic obstructive pulmonary disease. Heart Lung 2011, 40, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Oribabor, C.E.; Mansuroglu, N.; Khusid, F.; Patten, A.; Suleiman, M.; Primiano, J.; Leonard, L.; Antony, T. Low extubation times in cardiac surgery patients using the rapid shallow breathing index. Chest 2005, 128, 273S. [Google Scholar] [CrossRef]
- Seymour, C.W.; Cross, B.J.; Cooke, C.R.; Gallop, R.L.; Fuchs, B.D. Physiologic impact of closed-system endotracheal suctioning in spontaneously breathing patients receiving mechanical ventilation. Respir. Care 2009, 54, 367–374. [Google Scholar] [PubMed]
- Segal, L.N.; Fiel, S.B.; Ruggiero, S.; Scoopo, F.; Oei, E. Use of the rate of change of the RSBI during spontaneous breathing trial as an accurate predictor of weaning outcome. Crit. Care Med. 2005, 33, A20. [Google Scholar] [CrossRef]
- Segal, L.N.; Oei, E.; Oppenheimer, B.W.; Goldring, R.M.; Bustami, R.T.; Ruggiero, S.; Berger, K.I.; Fiel, S.B. Evolution of pattern of breathing during a spontaneous breathing trial predicts successful extubation. Intensive Care Med. 2010, 36, 487–495. [Google Scholar] [CrossRef]
- Karthika, M.; Al Enezi, F.A.; Pillai, L.V.; Arabi, Y.M. Rate of Change of Rapid Shallow Breathing Index and Extubation Outcome in Mechanically Ventilated Patients. Crit. Care Res. Pract. 2023, 2023, 9141441. [Google Scholar] [CrossRef]
| Demographic Data | Success (n = 53) | Failure (n = 33) | Total (n = 86) | p-Value |
|---|---|---|---|---|
| Gender (n%) | ||||
| Female | 22 | 10 | 32 (37.2) | 0.584 |
| Male | 31 | 23 | 54 (62.8) | |
| Age (years) | ||||
| Mean ± SD | 56.15 ± 11.3 | 51.88 ± 12.81 | 54.51 ± 12.1 | 0.268 |
| Disease | Frequency (%) |
|---|---|
| Pneumonia | 34.9 |
| Heart failure | 20.9 |
| COPD exacerbation | 14.0 |
| Sepsis | 10.5 |
| Other | 19.8 |
| Failure | Success | |||||||||
| Median | Minimum | Maximum | Mean | SD | Median | Minimum | Maximum | Mean | SD | |
| RSBA-1 | 84.00 | 56.00 | 100.00 | 76.94 | 12.81 | 72.00 | 54.00 | 96.00 | 74.00 | 9.85 |
| RSBI-1a | 85.00 | 54.00 | 100.00 | 81.18 | 10.86 | 76.00 | 54.00 | 96.00 | 75.60 | 11.11 |
| RSBI-2 | 85.00 | 70.00 | 102.00 | 85.45 | 6.48 | 80.00 | 54.00 | 102.00 | 79.38 | 10.81 |
| RSBI-2a | 92.00 | 65.00 | 120.00 | 91.00 | 10.48 | 80.00 | 54.00 | 97.00 | 78.83 | 14.72 |
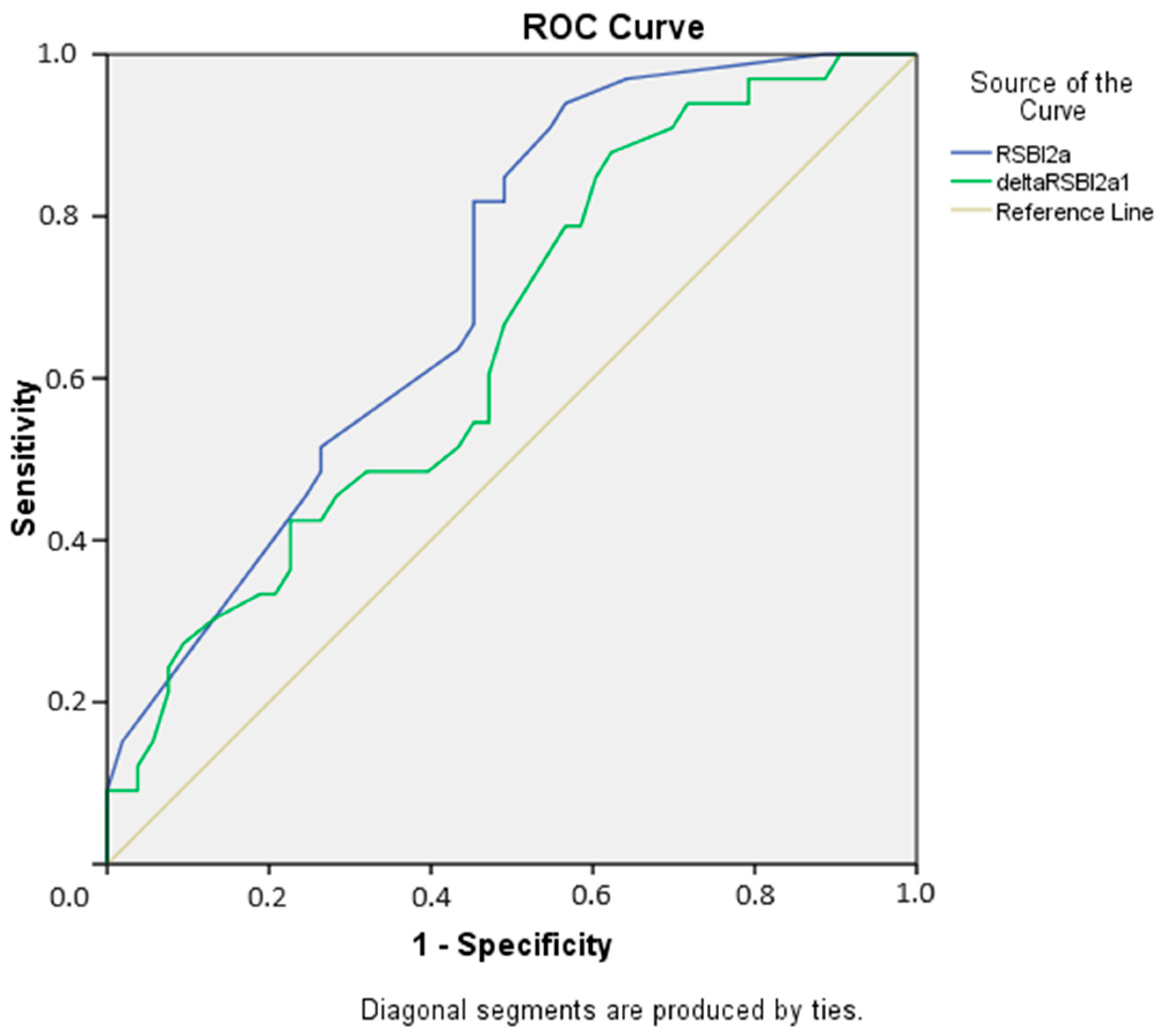
| Cut-Off Value | Sensitivity (%) | Specificity (%) | PPV (%) | N (%) | Test Accuracy (%) | OR (95% CI) | p-Value |
|---|---|---|---|---|---|---|---|
| RSBI-2a ≤ 72 | 43.4 | 93.9 | 92 | 50.8 | 62.79 | 11.883 (2.574–54.858) | <0.001 |
| ΔRSBI ≤ −3 | 37.7 | 87.9 | 83.3 | 46.8 | 56.98 | 4.394 (1.345–14.354) | 0.013 |
| Both Criteria | 30.2 | 100 | 100 | 47.1 | 56.97 | 29.48 * (3.924–221.469) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turhan, S.; Tutan, D.; Şahiner, Y.; Kısa, A.; Özdemir, S.Ö.; Tutan, M.B.; Kayır, S.; Doğan, G. Predictive Value of Serial Rapid Shallow Breathing Index Measurements for Extubation Success in Intensive Care Unit Patients. Medicina 2024, 60, 1329. https://doi.org/10.3390/medicina60081329
Turhan S, Tutan D, Şahiner Y, Kısa A, Özdemir SÖ, Tutan MB, Kayır S, Doğan G. Predictive Value of Serial Rapid Shallow Breathing Index Measurements for Extubation Success in Intensive Care Unit Patients. Medicina. 2024; 60(8):1329. https://doi.org/10.3390/medicina60081329
Chicago/Turabian StyleTurhan, Semin, Duygu Tutan, Yeliz Şahiner, Alperen Kısa, Sibel Önen Özdemir, Mehmet Berksun Tutan, Selçuk Kayır, and Güvenç Doğan. 2024. "Predictive Value of Serial Rapid Shallow Breathing Index Measurements for Extubation Success in Intensive Care Unit Patients" Medicina 60, no. 8: 1329. https://doi.org/10.3390/medicina60081329
APA StyleTurhan, S., Tutan, D., Şahiner, Y., Kısa, A., Özdemir, S. Ö., Tutan, M. B., Kayır, S., & Doğan, G. (2024). Predictive Value of Serial Rapid Shallow Breathing Index Measurements for Extubation Success in Intensive Care Unit Patients. Medicina, 60(8), 1329. https://doi.org/10.3390/medicina60081329






