Feasibility of Early Surgical Treatment for Adolescent Patients with Prolactinoma: A Case Report and Literature Review
Abstract
1. Introduction
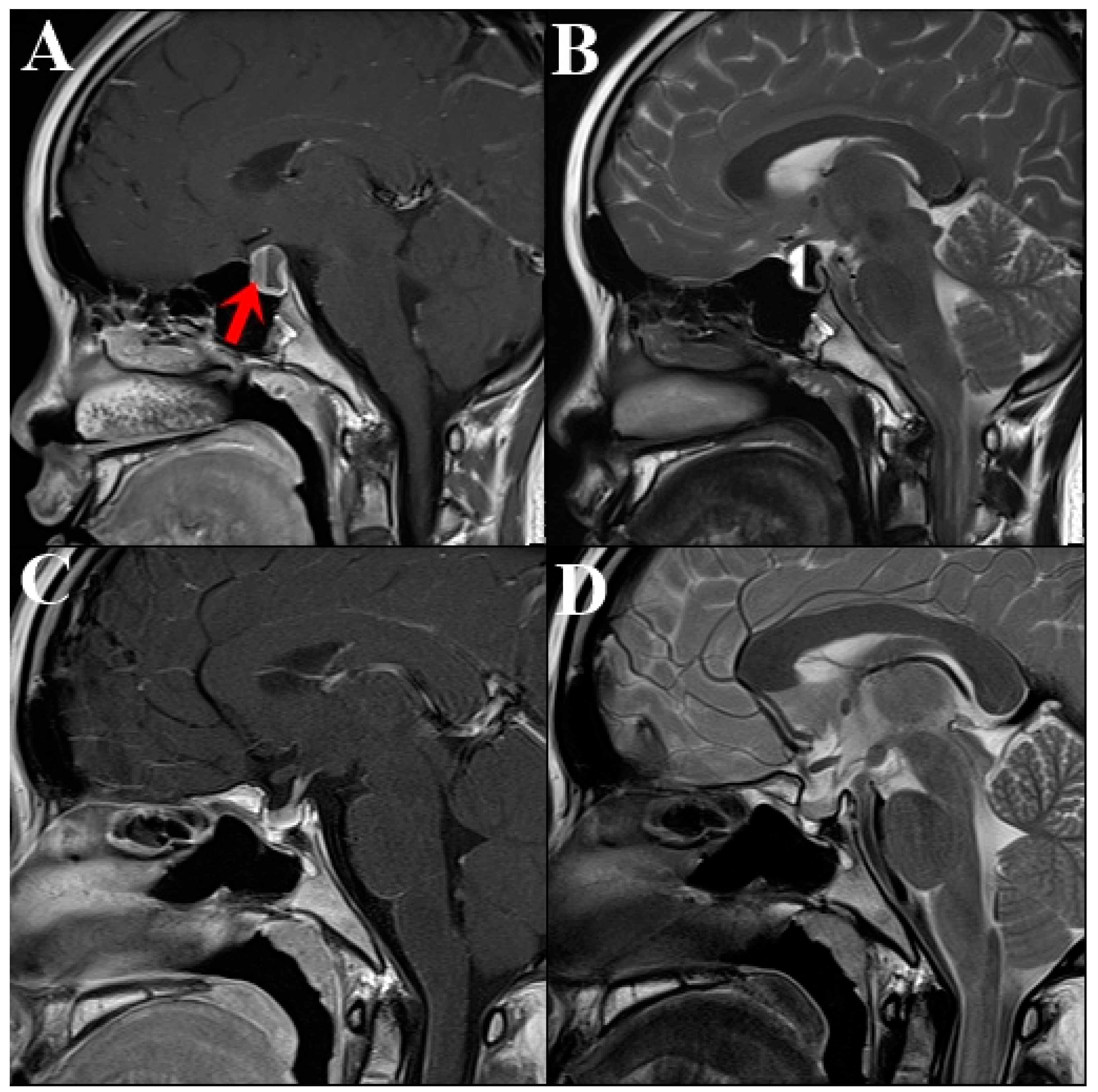
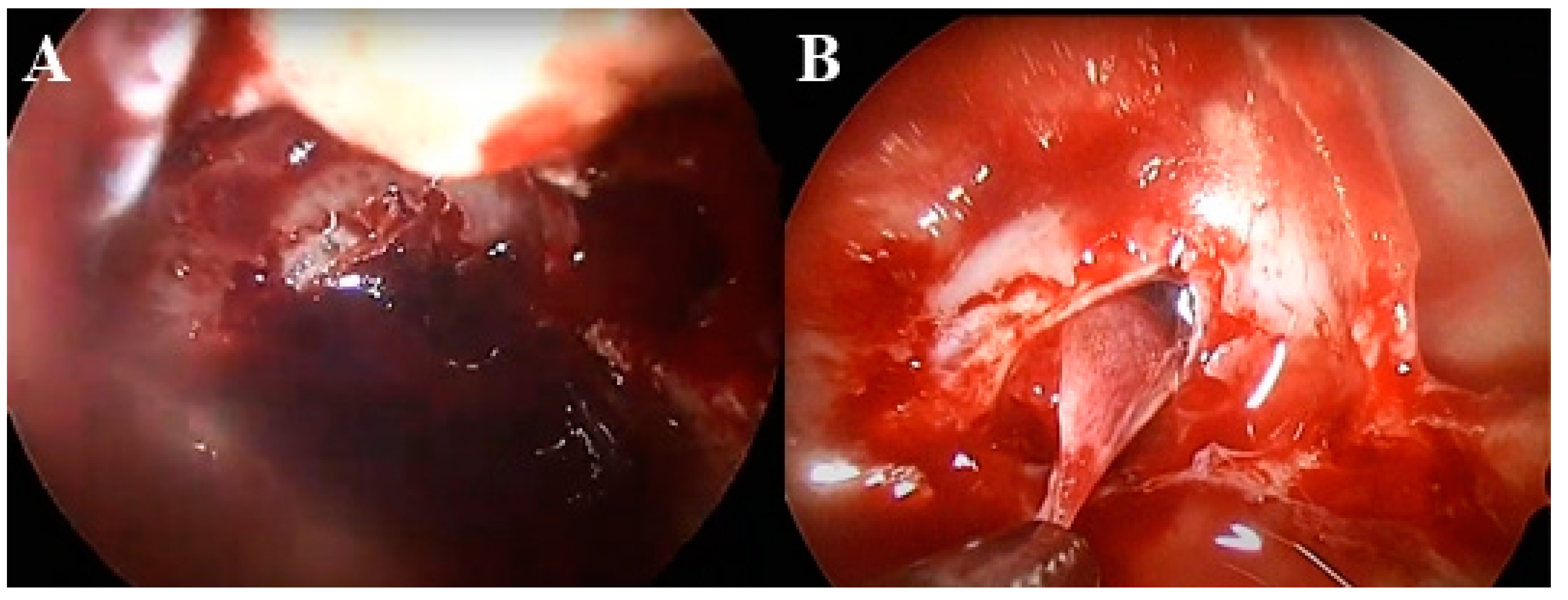
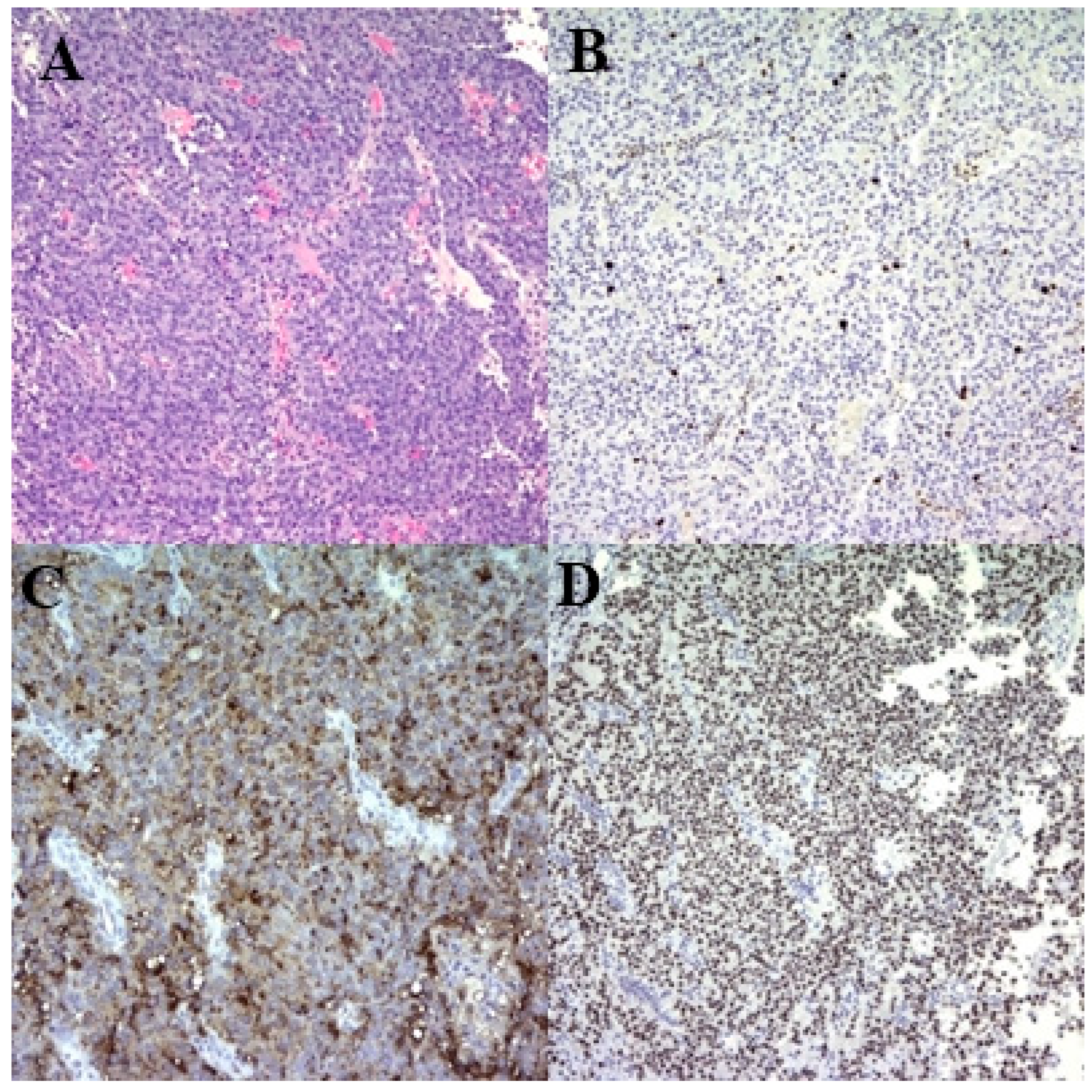
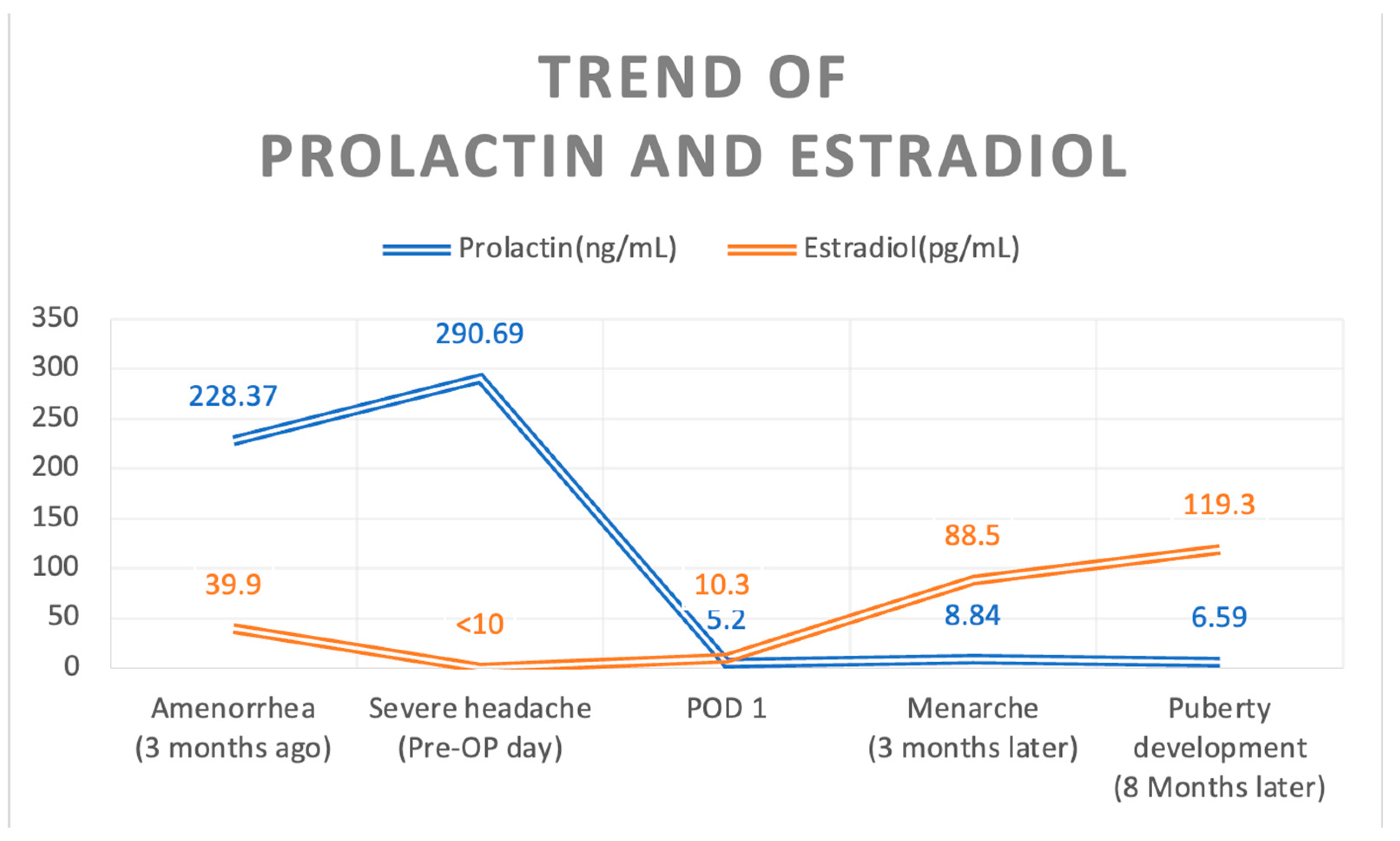
2. Case Description
3. Discussion
4. Learning Points
- Adolescents with prolactinomas may present with atypical symptoms that can mimic normal developmental variations, necessitating a high index of suspicion for accurate diagnosis.
- Prompt surgical intervention in adolescents with prolactinomas can lead to rapid normalization of prolactin levels and resolution of associated endocrine dysfunction, such as delayed puberty.
- High Ki-67 indices in prolactinomas, indicating increased proliferative activity, may predict resistance to dopamine agonist therapy and highlight the potential role of early surgical management.
- Postoperative outcomes in adolescent patients, including rapid onset of menarche and development of secondary sexual characteristics, underscore the effectiveness of surgical intervention in restoring normal hormonal function.
5. New Findings
- This case report emphasizes the effectiveness of early surgical intervention in achieving biochemical remission and resolving endocrine symptoms in adolescent patients with prolactinomas, particularly those with high Ki-67 indices.
- The study highlights the unique challenges and successful outcomes associated with early surgical management in adolescents, contributing valuable insights into treatment strategies for this age group.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| DA | Dopamine agonists |
| MRI | Magnetic resonance imaging |
References
- Ottenhausen, M.; Conrad, J.; Wolters, L.M.; Ringel, F. Surgery as first-line treatment for prolactinoma? Discussion of the literature and results of a consecutive series of surgically treated patients. Neurosurg. Rev. 2023, 46, 128. [Google Scholar] [CrossRef] [PubMed]
- Molitch, M.E. Diagnosis and treatment of pituitary adenomas: A review. JAMA 2017, 317, 516–524. [Google Scholar] [CrossRef] [PubMed]
- CCannavò, S.; Venturino, M.; Curtò, L.; De Menis, E.; D’arrigo, C.; Tita, P.; Billeci, D.; Trimarchi, F. Clinical presentation and outcome of pituitary adenomas in teenagers. Clin. Endocrinol. 2003, 58, 519–527. [Google Scholar] [CrossRef] [PubMed]
- De Menis, E.; Visentin, A.; Billeci, D.; Tramontin, P.; Agostini, S.; Marton, E.; Conte, N. Pituitary adenomas in childhood and adolescence. Clinical analysis of 10 cases. J. Endocrinol. Investig. 2001, 24, 92–97. [Google Scholar] [CrossRef]
- Mindermann, T.; Wilson, C.B. Age-related and gender-related occurrence of pituitary adenomas. Clin. Endocrinol. 1994, 41, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Aflorei, E.D.; Korbonits, M. Epidemiology and etiopathogenesis of pituitary adenomas. J. Neurooncol 2014, 117, 379–394. [Google Scholar] [CrossRef] [PubMed]
- Andereggen, L.; Tortora, A.; Schubert, G.A.; Musahl, C.; Frey, J.; Luedi, M.M.; Mariani, L.; Beck, J.; Christ, E. Prolactinomas in adolescent and elderly patients—A comparative long-term analysis. Front. Surg. 2023, 10, 967407. [Google Scholar] [CrossRef] [PubMed]
- Minniti, G.; Esposito, V.; Piccirilli, M.; Fratticci, A.; Santoro, A.; Jaffrain-Rea, M.L. Diagnosis and management of pituitary tumours in the elderly: A review based on personal experience and evidence of literature. Eur. J. Endocrinol. 2005, 153, 723–735. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, S.M.C. DA therapy for prolactinomas: Do we need to rethink the place of surgery in prolactinoma management? Endocr. Oncol. 2022, 2, R31–R50. [Google Scholar] [CrossRef]
- Najafabadi, A.H.Z.; Zandbergen, I.M.; de Vries, F.; Broersen, L.H.A.; Marle, M.E.v.D.A.-V.; Pereira, A.M.; Peul, W.C.; Dekkers, O.M.; van Furth, W.R.; Biermasz, N.R. Surgery as a viable alternative first-line treatment for prolactinoma patients. A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2020, 105, e32–e41. [Google Scholar] [CrossRef]
- Steele, C.A.; MacFarlane, I.A.; Blair, J.; Cuthbertson, D.J.; Didi, M.; Mallucci, C.; Javadpour, M.; Daousi, C. Pituitary adenomas in childhood, adolescence and young adulthood: Presentation, management, endocrine and metabolic outcomes. Eur. J. Endocrinol. 2010, 163, 515–522. [Google Scholar] [CrossRef]
- Zhao, Y.; Jin, D.; Lian, W.; Xing, B.; Feng, M.; Liu, X.; Wang, R. Clinical characteristics and surgical outcome of prolactinoma in patients under 14 years old. Medicine 2019, 98, e14380. [Google Scholar] [CrossRef]
- Buchfelder, M.; Zhao, Y.; Schlaffer, S.M. Surgery for prolactinomas to date. Neuroendocrinology 2019, 109, 77–81. [Google Scholar] [CrossRef]
- Stumpf, M.A.M.; Pinheiro, F.M.M.; Silva, G.O.; Cescato, V.A.S.; Musolino, N.R.C.; Cunha-Neto, M.B.C.; Glezer, A. How to manage intolerance to DA in patients with prolactinoma. Pituitary 2023, 26, 187–196. [Google Scholar] [CrossRef]
- Ali, S.; Miller, K.K.; Freudenreich, O. Management of psychosis associated with a prolactinoma: Case report and review of the literature. Psychosomatics 2010, 51, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Ioachimescu, A.G.; Fleseriu, M.; Hoffman, A.R.; Vaughan Iii, T.B.; Katznelson, L. Psychological effects of DA treatment in patients with hyperprolactinemia and prolactin-secreting adenomas. Eur. J. Endocrinol. 2019, 180, 31–40. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, S.M.C.; Baranoff, J.; Rushworth, R.L.; Butler, J.; Sorbello, J.; Vorster, J.; Thompson, T.; McCormack, A.I.; Inder, W.J.; Torpy, D.J. Impulse control disorders in dopamine agonist-treated hyperprolactinemia: Prevalence and risk factors. J. Clin. Endocrinol. Metab. 2020, 105, dgz076. [Google Scholar] [CrossRef] [PubMed]
- Hinojosa-Amaya, J.M.; Johnson, N.; González-Torres, C.; Varlamov, E.V.; Yedinak, C.G.; McCartney, S.; Fleseriu, M. Depression and impulsivity self-assessment tools to identify dopamine agonist side effects in patients with pituitary adenomas. Front. Endocrinol. 2020, 11, 579606. [Google Scholar] [CrossRef]
- Miermeister, C.P.; Petersenn, S.; Buchfelder, M.; Fahlbusch, R.; Lüdecke, D.K.; Hölsken, A.; Bergmann, M.; Knappe, H.U.; Hans, V.H.; Flitsch, J.; et al. Histological criteria for atypical pituitary adenomas—Data from the German pituitary adenoma registry suggests modifications. Acta Neuropathol. Commun. 2015, 3, 50. [Google Scholar] [CrossRef]
- Thapar, K.; Kovacs, K.; Scheithauer, B.W.; Stefaneanu, L.; Horvath, E.; Pernicone, P.J.; Murray, D.; Laws, E.R. Proliferative activity and invasiveness among pituitary adenomas and carcinomas: An analysis using the MIB-1 antibody. Neurosurgery 1996, 38, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Burger, P.C.; Shibata, T.; Kleihues, P. The use of the monoclonal antibody Ki-67 in the identification of proliferating cells: Application to surgical neuropathology. Am. J. Surg. Pathol. 1986, 10, 611–617. [Google Scholar] [CrossRef]
- Mastronardi, L.; Guiducci, A.; Spera, C.; Puzzilli, F.; Liberati, F.; Maira, G. Ki-67 labelling index and invasiveness among anterior pituitary adenomas: Analysis of 103 cases using the MIB-1 monoclonal antibody. J. Clin. Pathol. 1999, 52, 107–111. [Google Scholar] [CrossRef]
- Bălinişteanu, B.; Cîmpean, A.M.; Ceauşu, A.R.; Corlan, A.S.; Melnic, E.; Raica, M. High Ki-67 expression is associated with prolactin secreting pituitary adenomas. Bosn. J. Basic Med. Sci. 2017, 17, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Yonezawa, K.; Tamaki, N.; Kokunai, T. Clinical features and growth fractions of pituitary adenomas. Surg. Neurol. 1997, 48, 494–500. [Google Scholar] [CrossRef]
- PPaek, K.-I.; Kim, S.-H.; Song, S.-H.; Choi, S.-W.; Koh, H.-S.; Youm, J.-Y.; Kim, Y. Clinical significance of Ki-67 labeling index in pituitary macroadenoma. J. Korean Med. Sci. 2005, 20, 489–494. [Google Scholar] [CrossRef]
- Lu, C.; Liu, Y.; Lu, Z.; Huan, C. Ki-67 and clinical correlations in patients with resistant prolactinomas. Ann. Clin. Lab. Sci. 2020, 50, 199–204. [Google Scholar]
- Olarescu, N.C.; Perez-Rivas, L.G.; Gatto, F.; Cuny, T.; Tichomirowa, M.A.; Tamagno, G.; Gahete, M.D. Aggressive and malignant prolactinomas. Neuroendocrinology 2019, 109, 57–69. [Google Scholar] [CrossRef]
- Tng, E.L.; Teo, A.E.; Aung, A.T. Macroprolactinoma with secondary resistance to DA: A case report and review of the literature. J. Med. Case Rep. 2023, 17, 96. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.-Y.; Lee, C.-H.; Yang, M.-Y.; Shen, C.-C.; Yang, Y.-P.; Chien, Y.; Huang, Y.-F.; Lai, C.-M.; Cheng, W.-Y. Treatment of hyperprolactinemia: A single-institute experience. J. Chin. Med. Assoc. 2021, 84, 1019–1022. [Google Scholar] [CrossRef]
- Lee, Y.; Ku, C.R.; Kim, E.H.; Hong, J.W.; Lee, E.J.; Kim, S.H. Early prediction of long-term response to cabergoline in patients with macroprolactinomas. Endocrinol. Metab. 2014, 29, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Menucci, M.; Quiñones-Hinojosa, A.; Burger, P.; Salvatori, R. Effect of dopaminergic drug treatment on surgical findings in prolactinomas. Pituitary 2011, 14, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Wang, F.; Liu, Z.; Jiao, B. Effects of preoperative bromocriptine treatment on prolactin-secreting pituitary adenoma surgery. Exp. Ther. Med. 2016, 11, 1977–1982. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.K.; Vance, M.L.; Boulos, P.T.; Laws, E.R. Surgical outcomes in hyporesponsive prolactinomas: Analysis of patients with resistance or intolerance to dopamine agonists. Pituitary 2005, 8, 53–60. [Google Scholar] [CrossRef]
- Vermeulen, E.; D’haens, J.; Stadnik, T.; Unuane, D.; Barbe, K.; Van Velthoven, V.; Gläsker, S. Predictors of dopamine agonist resistance in prolactinoma patients. BMC Endocr. Disord. 2020, 20, 68. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, Y.-H.; Li, C.-R.; Wang, Y.-T.; Chen, S.-Y. Feasibility of Early Surgical Treatment for Adolescent Patients with Prolactinoma: A Case Report and Literature Review. Medicina 2024, 60, 1345. https://doi.org/10.3390/medicina60081345
Tsai Y-H, Li C-R, Wang Y-T, Chen S-Y. Feasibility of Early Surgical Treatment for Adolescent Patients with Prolactinoma: A Case Report and Literature Review. Medicina. 2024; 60(8):1345. https://doi.org/10.3390/medicina60081345
Chicago/Turabian StyleTsai, Yu-Hung, Chi-Ruei Li, Yu-Ting Wang, and Se-Yi Chen. 2024. "Feasibility of Early Surgical Treatment for Adolescent Patients with Prolactinoma: A Case Report and Literature Review" Medicina 60, no. 8: 1345. https://doi.org/10.3390/medicina60081345
APA StyleTsai, Y.-H., Li, C.-R., Wang, Y.-T., & Chen, S.-Y. (2024). Feasibility of Early Surgical Treatment for Adolescent Patients with Prolactinoma: A Case Report and Literature Review. Medicina, 60(8), 1345. https://doi.org/10.3390/medicina60081345




