The Effect of Combined Balance Exercise on Knee Range of Motion, Balance, Gait, and Functional Outcomes in Acute Phase Following Total Knee Arthroplasty: A Single-Blind Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Ethical Statement
2.3. Study Design
2.4. Experimental Procedure
2.5. Training Program
2.5.1. Combined Balance Exercise
2.5.2. General Physical Therapy
2.6. Outcome Measures
2.7. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yohannes, A.M.; Caton, S. Management of depression in older people with osteoarthritis: A systematic review. Aging Ment. Health 2010, 14, 637–651. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.E. Osteoarthritis year in review 2017: Clinical. Osteoarthr. Cartil. 2018, 26, 319–325. [Google Scholar] [CrossRef]
- Stannus, O.; Jones, G.; Cicuttini, F.; Parameswaran, V.; Quinn, S.; Burgess, J.; Ding, C. Circulating levels of IL-6 and TNF-α are associated with knee radiographic osteoarthritis and knee cartilage loss in older adults. Osteoarthr. Cartil. 2010, 18, 1441–1447. [Google Scholar] [CrossRef]
- Zacharias, A.; Green, R.; Semciw, A.; Kingsley, M.; Pizzari, T. Efficacy of rehabilitation programs for improving muscle strength in people with hip or knee osteoarthritis: A systematic review with meta-analysis. Osteoarthr. Cartil. 2014, 22, 1752–1773. [Google Scholar] [CrossRef]
- Roos, E.M.; Arden, N.K. Strategies for the prevention of knee osteoarthritis. Nat. Rev. Rheumatol. 2016, 12, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Strasser, E.M.; Draskovits, T.; Praschak, M.; Quittan, M.; Graf, A. Association between ultrasound measurements of muscle thickness, pennation angle, echogenicity and skeletal muscle strength in the elderly. Age 2013, 35, 2377–2388. [Google Scholar] [CrossRef] [PubMed]
- Levinger, I.; Levinger, P.; Trenerry, M.K.; Feller, J.A.; Bartlett, J.R.; Bergman, N.; McKenna, M.J.; Cameron-Smith, D. Increased inflammatory cytokine expression in the vastus lateralis of patients with knee osteoarthritis. Arthritis Rheum. 2011, 63, 1343–1348. [Google Scholar] [CrossRef]
- Franklin, P.D.; Li, W.; Ayers, D.C. The Chitranjan Ranawat Award: Functional outcome after total knee replacement varies with patient attributes. Clin. Orthop. Relat. Res. 2008, 466, 2597–2604. [Google Scholar] [CrossRef]
- Witjes, S.; Gouttebarge, V.; Kuijer, P.P.F.; van Geenen, R.C.; Poolman, R.W.; Kerkhoffs, G.M. Return to sports and physical activity after total and unicondylar knee arthroplasty: A systematic review and meta-analysis. Sports Med. 2016, 46, 269–292. [Google Scholar] [CrossRef]
- Cash, R.M.; Gonzalez, M.H.; Garst, J.; Barmada, R.; Stern, S.H. Proprioception after arthroplasty: Role of the posterior cruciate ligament. Clin. Orthop. Relat. Res.® 1996, 331, 172–178. [Google Scholar] [CrossRef]
- Alessio-Mazzola, M.; Solarino, G.; Marongiu, G.; Salini, V.; Placella, G. Total knee arthroplasty after anterior cruciate ligament reconstruction: A narrative review. Ann. Jt. 2024, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Khan, Z.A.; Sava, M.P.; von Eisenhart-Rothe, R.; Graichen, H.; Vendittoli, P.A.; Riviere, C.; Chen, A.F.; Leclercq, V.; Amsler, F. Definition of normal, neutral, deviant and aberrant coronal knee alignment for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 473–489. [Google Scholar] [CrossRef] [PubMed]
- Obrębska, P.; Skubich, J.; Piszczatowski, S. Gender differences in the knee joint loadings during gait. Gait Posture 2020, 79, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Cromwell, R.L.; Newton, R.A.; Forrest, G. Influence of vision on head stabilization strategies in older adults during walking. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2002, 57, M442–M448. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Woodhouse, L.J.; Thomas, S.G.; Finch, E. Physical impairments and functional limitations: A comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys. Ther. 1998, 78, 248–258. [Google Scholar] [CrossRef]
- McClelland, J. The place of modeling in cognitive science. Top. Cogn. Sci. 2009, 1, 11–38. [Google Scholar] [CrossRef]
- Piva, S.R.; Gil, A.B.; Almeida, G.J.; DiGioia, A.M., III; Levison, T.J.; Fitzgerald, G.K. A balance exercise program appears to improve function for patients with total knee arthroplasty: A randomized clinical trial. Phys. Ther. 2010, 90, 880–894. [Google Scholar] [CrossRef]
- Mizner, R.L.; Petterson, S.C.; Stevens, J.E.; Vandenborne, K.; Snyder-Mackler, L. Early quadriceps strength loss after total knee arthroplasty: The contributions of muscle atrophy and failure of voluntary muscle activation. JBJS 2005, 87, 1047–1053. [Google Scholar] [CrossRef]
- Cadore, E.L.; Rodríguez-Mañas, L.; Sinclair, A.; Izquierdo, M. Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: A systematic review. Rejuvenation Res. 2013, 16, 105–114. [Google Scholar] [CrossRef]
- Hill, K.D.; Williams, S.B.; Chen, J.; Moran, H.; Hunt, S.; Brand, C. Balance and falls risk in women with lower limb osteoarthritis or rheumatoid arthritis. J. Clin. Gerontol. Geriatr. 2013, 4, 22–28. [Google Scholar] [CrossRef]
- Morrow Jnr, J.; Jackson, A.; Disch, J.; Mood, D. Measurement and Evaluation in Human Performance; Human Kinetics: Champaign, IL, USA, 1995. [Google Scholar]
- Pollock, A.S.; Durward, B.R.; Rowe, P.J.; Paul, J.P. What is balance? Clin. Rehabil. 2000, 14, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Levinger, P.; Menz, H.B.; Wee, E.; Feller, J.A.; Bartlett, J.R.; Bergman, N.R. Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1082–1089. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Okuno, M.; Nakamura, T.; Yamamoto, K.; Hagino, H. Fall incidence and risk factors in patients after total knee arthroplasty. Arch. Orthop. Trauma Surg. 2012, 132, 555–563. [Google Scholar] [CrossRef]
- Moutzouri, M.; Gleeson, N.; Billis, E.; Tsepis, E.; Panoutsopoulou, I.; Gliatis, J. The effect of total knee arthroplasty on patients’ balance and incidence of falls: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3439–3451. [Google Scholar] [CrossRef] [PubMed]
- de Lima, F.; Melo, G.; Fernandes, D.A.; Santos, G.M.; Neto, F.R. Effects of total knee arthroplasty for primary knee osteoarthritis on postural balance: A systematic review. Gait Posture 2021, 89, 139–160. [Google Scholar] [CrossRef]
- Wang, Y.-Q.; Qu, G.-B.; Yang, J.-F. Impact of preoperative balance training on postoperative functional recovery of patients after total knee arthroplasty: A systematic review and meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 3154–3164. [Google Scholar]
- Liao, C.-D.; Liou, T.-H.; Huang, Y.-Y.; Huang, Y.-C. Effects of balance training on functional outcome after total knee replacement in patients with knee osteoarthritis: A randomized controlled trial. Clin. Rehabil. 2013, 27, 697–709. [Google Scholar] [CrossRef]
- Blasco, J.-M.; Acosta-Ballester, Y.; Martínez-Garrido, I.; García-Molina, P.; Igual-Camacho, C.; Roig-Casasús, S. The effects of preoperative balance training on balance and functional outcome after total knee replacement: A randomized controlled trial. Clin. Rehabil. 2020, 34, 182–193. [Google Scholar] [CrossRef]
- Domínguez-Navarro, F.; Igual-Camacho, C.; Silvestre-Muñoz, A.; Roig-Casasús, S.; Blasco, J.M. Effects of balance and proprioceptive training on total hip and knee replacement rehabilitation: A systematic review and meta-analysis. Gait Posture 2018, 62, 68–74. [Google Scholar] [CrossRef]
- Jogi, P.; Overend, T.J.; Spaulding, S.J.; Zecevic, A.; Kramer, J.F. Effectiveness of balance exercises in the acute post-operative phase following total hip and knee arthroplasty: A randomized clinical trial. SAGE Open Med. 2015, 3, 2050312115570769. [Google Scholar] [CrossRef]
- Doma, K.; Grant, A.; Morris, J. The effects of balance training on balance performance and functional outcome measures following total knee arthroplasty: A systematic review and meta-analysis. Sports Med. 2018, 48, 2367–2385. [Google Scholar] [CrossRef]
- Castrodad, I.M.D.; Recai, T.M.; Abraham, M.M.; Etcheson, J.I.; Mohamed, N.S.; Edalatpour, A.; Delanois, R.E. Rehabilitation protocols following total knee arthroplasty: A review of study designs and outcome measures. Ann. Transl. Med. 2019, 7 (Suppl. 7), S255. [Google Scholar] [CrossRef] [PubMed]
- Pagnotta, G.; Rich, E.; Eckardt, P.; Lavin, P.; Burriesci, R. The effect of a rapid rehabilitation program on patients undergoing unilateral total knee arthroplasty. Orthop. Nurs. 2017, 36, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Meier, W.; Mizner, R.; Marcus, R.; Dibble, L.; Peters, C.; Lastayo, P.C. Total knee arthroplasty: Muscle impairments, functional limitations, and recommended rehabilitation approaches. J. Orthop. Sports Phys. Ther. 2008, 38, 246–256. [Google Scholar] [CrossRef] [PubMed]
- An, J.; Ryu, H.-K.; Lyu, S.-J.; Yi, H.-J.; Lee, B.-H. Effects of preoperative telerehabilitation on muscle strength, range of motion, and functional outcomes in candidates for total knee arthroplasty: A single-blind randomized controlled trial. Int. J. Environ. Res. Public Health 2021, 18, 6071. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-G.; An, J.; Lee, B.-H. The effect of progressive dynamic balance training on physical function, the ability to balance and quality of life among elderly women who underwent a total knee arthroplasty: A double-blind randomized control trial. Int. J. Environ. Res. Public Health 2021, 18, 2513. [Google Scholar] [CrossRef]
- McConnell, J. Management of patellofemoral pain: Where are we now? Int. SportsMed J. 2001, 2, 1–9. [Google Scholar]
- Svensson, M.; Lind, V.; Löfgren Harringe, M. Measurement of knee joint range of motion with a digital goniometer: A reliability study. Physiother. Res. Int. 2019, 24, e1765. [Google Scholar] [CrossRef]
- Niknam, H.; Esteki, A.; Salavati, M.; Kahrizi, S. Reliability of Zebris motion analysis system in healthy athletes and athletes with anterior cruciate ligament reconstruction. Asian J. Sports Med. 2017, 8, e42040. [Google Scholar] [CrossRef]
- Morris, S.; Morris, M.E.; Iansek, R. Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Phys. Ther. 2001, 81, 810–818. [Google Scholar]
- Nordin, E.; Rosendahl, E.; Lundin-Olsson, L. Timed “Up & Go” test: Reliability in older people dependent in activities of daily living—Focus on cognitive state. Phys. Ther. 2006, 86, 646–655. [Google Scholar] [PubMed]
- Skoffer, B.; Maribo, T.; Mechlenburg, I.; Hansen, P.M.; Søballe, K.; Dalgas, U. Efficacy of preoperative progressive resistance training on postoperative outcomes in patients undergoing total knee arthroplasty. Arthritis Care Res. 2016, 68, 1239–1251. [Google Scholar] [CrossRef] [PubMed]
- Intaruk, R.; Phadungkit, S.; Kanpai, A.; Pawanta, K.; Srihapol, N.; Saengsuwan, J.; Amatachaya, S.; Thaweewannakij, T. Test-retest reliability and minimal detectable change of four functional tests in community-dwelling older adults with high risk of falls. Turk. J. Phys. Med. Rehabil. (2587-1250) 2024, 70, 164–170. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Kehlet, H.; Søballe, K. Fast-track hip and knee replacement—What are the issues? Acta Orthop. 2010, 81, 271–272. [Google Scholar] [CrossRef]
- Amano, T.; Tamari, K.; Tanaka, S.; Uchida, S.; Ito, H.; Morikawa, S.; Kawamura, K. Factors for assessing the effectiveness of early rehabilitation after minimally invasive total knee arthroplasty: A prospective cohort study. PLoS ONE 2016, 11, e0159172. [Google Scholar] [CrossRef]
- Clement, N.D.; Bardgett, M.; Weir, D.; Holland, J.; Gerrand, C.; Deehan, D.J. What is the minimum clinically important difference for the WOMAC index after TKA? Clin. Orthop. Relat. Res.® 2018, 476, 2005–2014. [Google Scholar] [CrossRef]
- Rogers, M.W.; Tamulevicius, N.; Semple, S.J.; Krkeljas, Z. Efficacy of home-based kinesthesia, balance & agility exercise training among persons with symptomatic knee osteoarthritis. J. Sports Sci. Med. 2012, 11, 751. [Google Scholar]
- Balci, P.; Tunay, V.; Baltaci, G.; Atay, A. The effects of two different closed kinetic chain exercises on muscle strength and proprioception in patients with patellofemoral pain syndrome. Acta Orthop. Traumatol. Turc. 2009, 43, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar]
- Kumar, D.; Manal, K.T.; Rudolph, K.S. Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthr. Cartil. 2013, 21, 298–305. [Google Scholar] [CrossRef]
- Bączkowicz, D.; Skiba, G.; Czerner, M.; Majorczyk, E. Gait and functional status analysis before and after total knee arthroplasty. Knee 2018, 25, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.C.; Jehu, D.A.; Pang, M.Y. Falls after total knee arthroplasty: Frequency, circumstances, and associated factors—A prospective cohort study. Phys. Ther. 2018, 98, 767–778. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, Y.; Okada, S. Risk of fall in patients during the early months after total knee arthroplasty. J. Arthritis 2014, 3, 139. [Google Scholar]
- LaStayo, P.C.; Meier, W.; Marcus, R.L.; Mizner, R.; Dibble, L.; Peters, C. Reversing muscle and mobility deficits 1 to 4 years after TKA: A pilot study. Clin. Orthop. Relat. Res.® 2009, 467, 1493–1500. [Google Scholar] [CrossRef]
- Studenski, S. Bradypedia: Is gait speed ready for clinical use? J. Nutr. Health Aging 2009, 13, 878. [Google Scholar] [CrossRef]
- Neptune, R.R.; Sasaki, K.; Kautz, S.A. The effect of walking speed on muscle function and mechanical energetics. Gait Posture 2008, 28, 135–143. [Google Scholar] [CrossRef]
| Week | Exercise Program | |||
|---|---|---|---|---|
| 1st week |  |  |  |  |
| Exercise | Seated torso rotations | Sit to stand | Shift weight to one side | Step-ups and step-downs |
| Practice | Each 10 reps/2 sets | Each 10 reps/2 sets | Each 10 reps/2 sets | Each 10 reps/2 sets |
| 2–3rd week |  |  |  |  |
| Exercise | Trunk rotations while standing | Side step-ups and downs | Standing on one leg while holding onto a walker | Lifting knees high and walking forward |
| Practice | Each 10 reps/2 sets | Each 10 reps/2 sets | Each 10 reps/2 sets | Each 10 reps/2 sets |
| 4th week |  |  |  |  |
| Exercise | Side step-ups and step-downs | Figure-eight walking | Heel raises while walking with a walker | Using a walker to perform up-and-down movements |
| Practice | Each 10 reps/2 sets | Each 1 min/2 reps | Each 1 min/2 reps | Each 10 reps/2 sets |
| Week | Exercises | Practice |
|---|---|---|
| 1–2nd week | Knee range of motion exercises in a seated position Leg extension exercises while lying down Leg lifting exercises while lying down Ankle dorsiflexion/plantarflexion exercises | Each 5 s/10 reps/5 sets |
| 3–4th week | Knee range of motion exercises in a seated position Knee extension exercises with resistance in a seated position Knee flexion exercises while standing Knee extension with resistance while standing Hip abduction exercises while standing. | Each 5 s/10 reps/5 sets |
| Characteristics | CBE Group (n = 19) | Control Group (n = 19) | X2/t (p) |
|---|---|---|---|
| Age (years) | 73.6 (4.8) a | 72.3 (4.6) | 0.865 (0.393) |
| Affected side (Rt/Lt) | 8/11 | 10/9 | 0.422 (0.516) |
| Height (cm) | 154.8 (3.9) | 152.5 (7.1) | 1.248 (0.222) |
| Weight (kg) | 63.7 (7.9) | 60.5 (8.6) | 1.185 (0.244) |
| BMI (kg/m2) | 26.5 (2.6) | 25.9 (3.0) | 0.585 (0.562) |
| BMD (T-score) | −2.3 (1.2) | −3.3 (2.4) | 1.562 (0.127) |
| Hypertension, N (%) (Yes/No) | 14 (73.7%)/5 (26.3%) | 12 (63.2%)/7 (36.8%) | 0.487 (0.485) |
| Diabetes mellitus, N (%) (Yes/No) | 11 (57.9%)/8 (42.1%) | 10 (52.6%)/9 (47.4%) | 0.106 (0.744) |
| Hyperlipidemia, N (%) (Yes/No) | 13 (68.4%)/6 (31.6%) | 9 (47.4%)/10 (52.63%) | 1.727 (0.189) |
| Depression, N (%) (Yes/No) | 3 (15.8%)/16 (84.2%) | 2 (10.5%)/17 (89.5%) | 0.230 (0.631) |
| Variable | CBE Group (n = 19) | Control Group (n = 19) | p-Value | Time | Group | Time × Group | ||
|---|---|---|---|---|---|---|---|---|
| F(p) | F(p) | F(p) | η2p | |||||
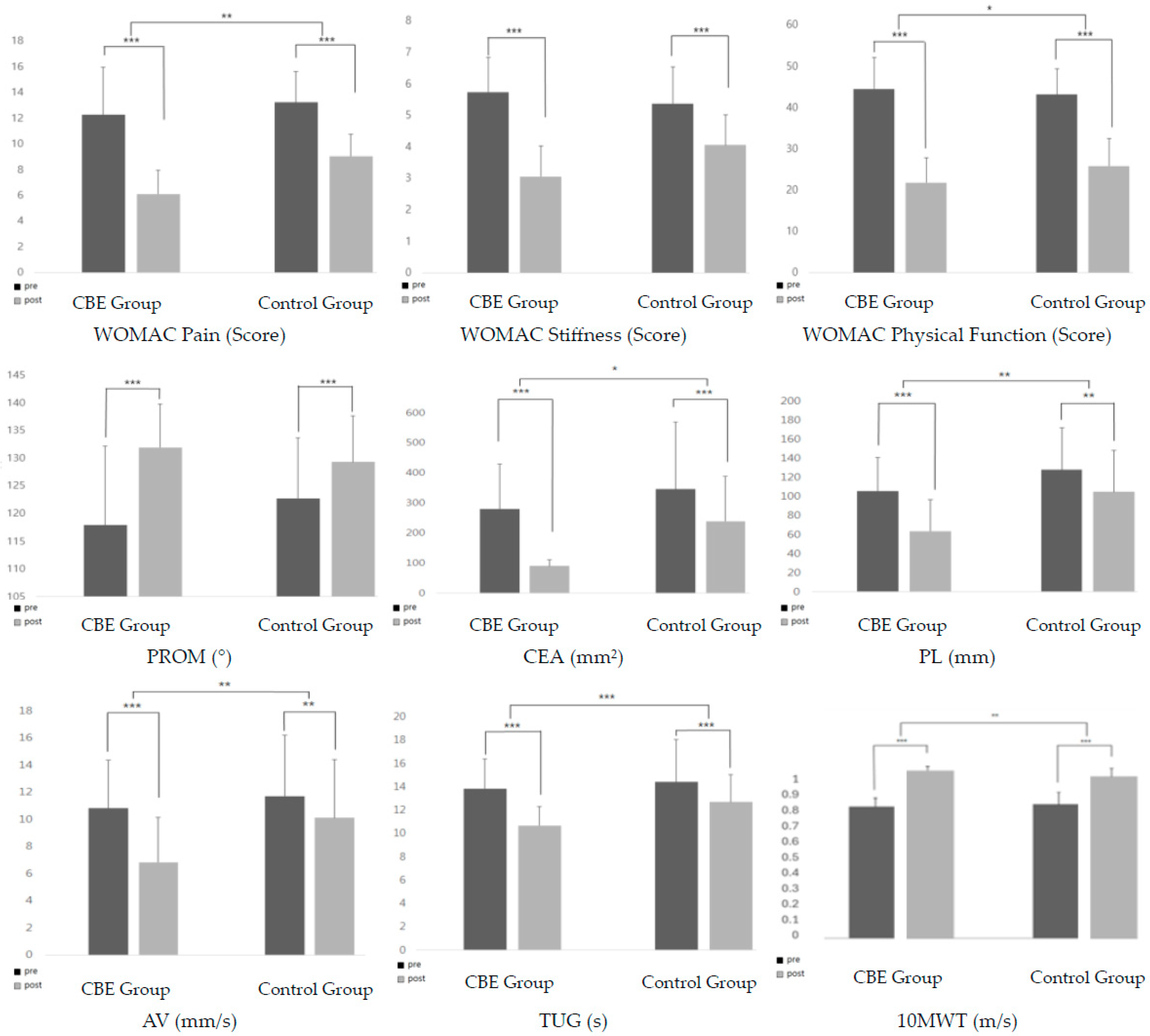
| WOMAC Pain | Pre-test | 12.26 (3.72) a | 13.22 (2.42) | 0.309 | 197.336 (0.000) | 7.307 (0.010) | 6.523 (0.015) | 0.153 |
| Post-test | 6.11 (1.85) | 9.05 (1.68) | ||||||
| Mean difference | 6.16 (2.77) | 4.26 (1.66) | 0.015 | |||||
| p-value | 0.000 | 0.000 | ||||||
| WOMAC Stiffness | Pre-test | 5.74 (1.09) | 5.37 (1.16) | 0.322 | 100.940 (0.000) | 1.290 (0.264) | 11.814 (0.001) | 0.247 |
| Post-test | 3.05 (0.97) | 4.05 (0.97) | ||||||
| Mean difference | 2.68 (1.29) | 1.32 (1.15) | 0.001 | |||||
| p-value | 0.000 | 0.000 | ||||||
| WOMAC Physical Function | Pre-test | 44.47 (7.567) | 43.11 (6.315) | 0.549 | 264.960 (0.000) | 0.578 (0.452) | 4.879 (0.034) | 0.119 |
| Post-test | 21.79 (5.931) | 25.84 (6.585) | ||||||
| Mean difference | 22.68 (7.18) | 17.26 (7.92) | 0.034 | |||||
| p-value | 0.000 | 0.000 | ||||||
| WOMAC Total (Score) | Pre-test | 63.95 (7.656) | 61.63 (8.908) | 0.396 | 365.912 (0.000) | 1.784 (0.190) | 12.558 (0.001) | 0.259 |
| Post-test | 30.95 (6.811) | 38.95 (8.256) | ||||||
| Mean difference | 33.00 (8.266) | 22.68 (9.627) | 0.001 | |||||
| p-value | 0.000 | 0.000 | ||||||
| PROM (°) Knee Flexion | Pre-test | 117.95 (14.24) | 122.68 (11.01) | 0.259 | 47.505 (0.000) | 0.113 (0.738) | 6.057 (0.019) | 0.144 |
| Post-test | 131.95 (7.89) | 129.32 (8.37) | ||||||
| Mean difference | 14.00 (11.79) | 6.63 (5.58) | 0.021 | |||||
| p-value | 0.000 | 0.000 | ||||||
| Variable | CBE Group (n= 19) | Control Group (n= 19) | p-Value | Time | Group | Time × Group | ||
|---|---|---|---|---|---|---|---|---|
| F(p) | F(p) | F(p) | η2p | |||||
| CEA (mm2) | Pre-test | 279.78 (150.75) a | 345.97 (224.43) | 0.294 | 54.618 (0.000) | 5.407 (0.026) | 4.175 (0.048) | 0.104 |
| Post-test | 90.30 (21.24) | 238.57 (150.32) | ||||||
| Mean difference | 189.48 (140.48) | 107.39 (104.52) | 0.048 | |||||
| p-value | 0.000 | 0.000 | ||||||
| PL (mm) | Pre-test | 105.81 (34.75) | 127.78 (44.63) | 0.099 | 86.668 (0.000) | 6.644 (0.014) | 7.464 (0.010) | 0.172 |
| Post-test | 63.86 (32.41) | 104.87 (43.36) | ||||||
| Mean difference | 41.95 (23.17) | 22.91 (19.63) | 0.010 | |||||
| p-value | 0.000 | 0.000 | ||||||
| AV (mm/s) | Pre-test | 10.80 (3.57) | 11.71 (4.51) | 0.494 | 42.337 (0.000) | 2.979 (0.093) | 7.564 (0.009) | 0.174 |
| Post-test | 6.82 (3.34) | 10.10 (4.31) | ||||||
| Mean difference | 3.97 (3.01) | 1.61 (2.22) | 0.009 | |||||
| p-value | 0.000 | 0.005 | ||||||
| TUG (s) | Pre-test | 13.83 (2.54) | 14.39 (3.63) | −0.584 | 84.502 (0.000) | 2.465 (0.125) | 7.347 (0.010) | 0.169 |
| Post-test | 10.67 (1.63) | 12.67 (2.35) | ||||||
| Mean difference | 3.15 (1.37) | 1.71 (1.85) | 0.010 | |||||
| p-value | 0.000 | 0.001 | ||||||
| Variable | CBE Group (n= 19) | Control Group (n= 19) | p-Value | Time | Group | Time × Group | ||
|---|---|---|---|---|---|---|---|---|
| F(p) | F(p) | F(p) | η2p | |||||
| 10MWT (m/s) | Pre-test | 0.813 (0.69) a | 0.79 (0.60) | 0.726 | 40.108 (0.000) | 1.769 (0.192) | 4.288 (0.046) | 0.106 |
| Post-test | 1.00 (0.89) | 0.88 (0.74) | ||||||
| Mean difference | 0.187 (0.60) | 0.09 (0.47) | 0.046 | |||||
| p-value | 0.000 | 0.012 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
An, J.; Cheon, S.-J.; Lee, B.-H. The Effect of Combined Balance Exercise on Knee Range of Motion, Balance, Gait, and Functional Outcomes in Acute Phase Following Total Knee Arthroplasty: A Single-Blind Randomized Controlled Trial. Medicina 2024, 60, 1389. https://doi.org/10.3390/medicina60091389
An J, Cheon S-J, Lee B-H. The Effect of Combined Balance Exercise on Knee Range of Motion, Balance, Gait, and Functional Outcomes in Acute Phase Following Total Knee Arthroplasty: A Single-Blind Randomized Controlled Trial. Medicina. 2024; 60(9):1389. https://doi.org/10.3390/medicina60091389
Chicago/Turabian StyleAn, Jungae, Seong-Jin Cheon, and Byoung-Hee Lee. 2024. "The Effect of Combined Balance Exercise on Knee Range of Motion, Balance, Gait, and Functional Outcomes in Acute Phase Following Total Knee Arthroplasty: A Single-Blind Randomized Controlled Trial" Medicina 60, no. 9: 1389. https://doi.org/10.3390/medicina60091389






