Comparison of Dye Spread Pattern and Nerve Involvement between Suprainguinal and Infrainguinal Fascia Iliaca Blocks with Different Injectate Volumes: A Cadaveric Evaluation
Abstract
:1. Introduction
2. Materials and Methods
2.1. S-FICB Procedure
2.2. I-FICB Procedure
2.3. Anatomical Dissection Procedure
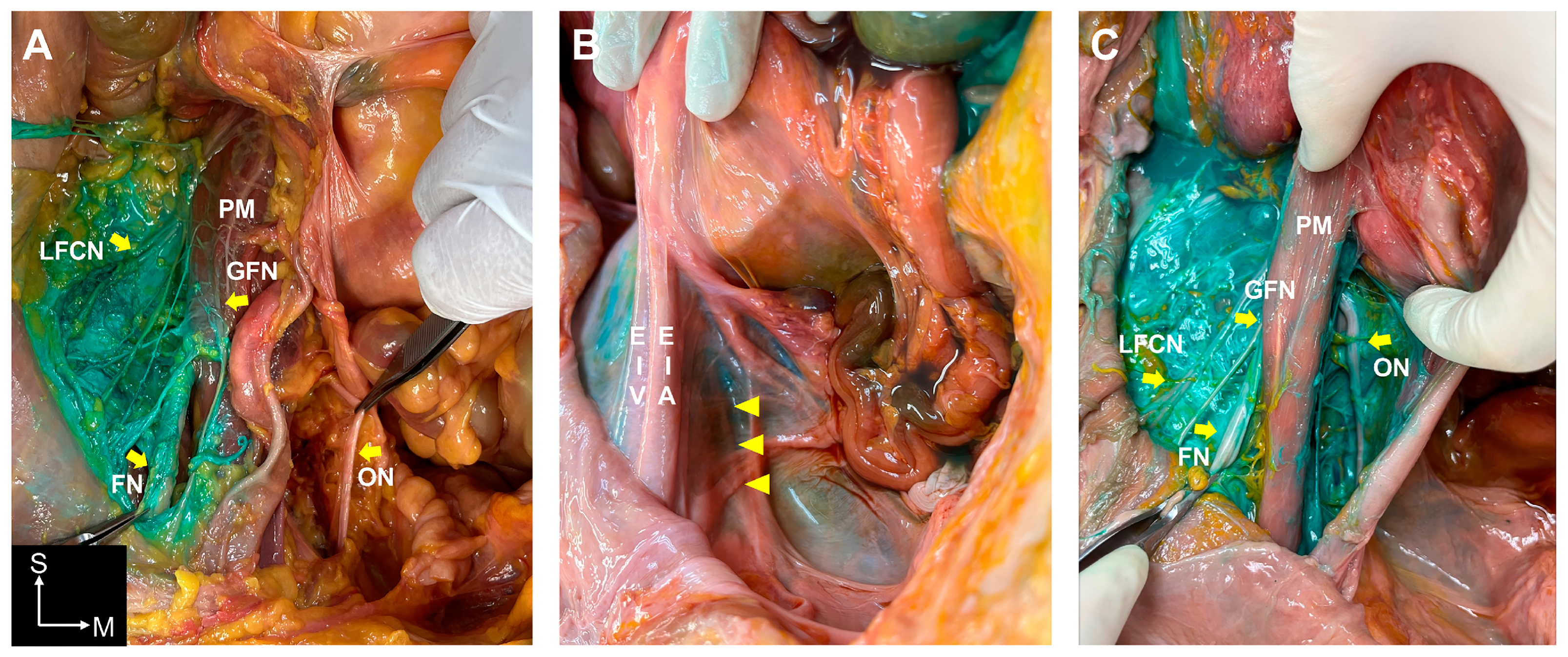
3. Results
3.1. Dye Spreading Patterns in the S-FICBs
3.2. Dye Spreading Patterns in the I-FICBs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Amiri, H.R.; Zamani, M.M.; Safari, S. Lumbar plexus block for management of hip surgeries. Anesthesiol. Pain Med. 2014, 4, e19407. [Google Scholar] [CrossRef] [PubMed]
- De Leeuw, M.; Zuurmond, W.; Perez, R. The psoas compartment block for hip surgery: The past, present, and future. Anesthesiol. Res. Pract. 2011, 2011, 159541. [Google Scholar] [CrossRef]
- Steenberg, J.; Møller, A. Systematic review of the effects of fascia iliaca compartment block on hip fracture patients before operation. Br. J. Anaesth. 2018, 120, 1368–1380. [Google Scholar] [CrossRef] [PubMed]
- O’reilly, N.; Desmet, M.; Kearns, R. Fascia iliaca compartment block. BJA Educ. 2019, 19, 191–197. [Google Scholar] [CrossRef]
- Sucher, J.F.; Barletta, J.F.; Shirah, G.R.; Prokuski, L.J.; Montanarella, P.D.; Dzandu, J.K.; Mangram, A.J. The safety of continuous fascia iliaca block in patients with hip fracture taking pre-injury anticoagulant and/or antiplatelet medications. Am. J. Surg. 2022, 224, 1473–1477. [Google Scholar] [CrossRef]
- Ten Hoope, W.; Smulders, P.S.; Baumann, H.M.; Hermanides, J.; Beenen, L.F.; Oostra, R.-J.; Marhofer, P.; Lirk, P.; Hollmann, M.W. A radiological cadaveric study of obturator nerve involvement and cranial injectate spread after different approaches to the fascia iliaca compartment block. Sci. Rep. 2023, 13, 12070. [Google Scholar] [CrossRef]
- Swenson, J.D.; Davis, J.J.; Stream, J.O.; Crim, J.R.; Burks, R.T.; Greis, P.E. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: The pattern of distribution and effects on the obturator nerve. J. Clin. Anesth. 2015, 27, 652–657. [Google Scholar] [CrossRef]
- Zhang, C.; Dai, W.; He, K. 95% effective volume of ropivacaine for ultrasound-guided supra-inguinal fascia iliaca compartment block. BMC Anesthesiol. 2023, 23, 98. [Google Scholar] [CrossRef] [PubMed]
- Desmet, M.; Vermeylen, K.; Van Herreweghe, I.; Carlier, L.; Soetens, F.; Lambrecht, S.; Croes, K.; Pottel, H.; Van de Velde, M. A longitudinal supra-inguinal fascia iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg. Anesth. Pain Med. 2017, 42, 327–333. [Google Scholar] [CrossRef]
- Shariat, A.N.; Hadzic, A.; Xu, D.; Shastri, U.; Kwofie, K.; Gandhi, K.; McCally, C.M.; Gratenstein, K.; Vandepitte, C.; Gadsden, J. Fascia lliaca block for analgesia after hip arthroplasty: A randomized double-blind, placebo-controlled trial. Reg. Anesth. Pain Med. 2013, 38, 201–205. [Google Scholar] [CrossRef]
- Vermeylen, K.; Desmet, M.; Leunen, I.; Soetens, F.; Neyrinck, A.; Carens, D.; Caerts, B.; Seynaeve, P.; Hadzic, A.; Van de Velde, M. Supra-inguinal injection for fascia iliaca compartment block results in more consistent spread towards the lumbar plexus than an infra-inguinal injection: A volunteer study. Reg. Anesth. Pain Med. 2019, 44, 483–491. [Google Scholar] [CrossRef]
- Kumar, K.; Pandey, R.K.; Bhalla, A.P.; Kashyap, L.; Garg, R.; Darlong, V.; Malhotra, R.; Yadav, C.S. Comparison of conventional infrainguinal versus modified proximal suprainguinal approach of fascia iliaca compartment block for postoperative analgesia in total hip arthroplasty. A prospective randomized study. Acta Anaesthesiol. Belg. 2015, 66, 95–100. [Google Scholar] [PubMed]
- Bansal, K.; Sharma, N.; Singh, M.R.; Sharma, A.; Roy, R.; Sethi, S. Comparison of suprainguinal approach with infrainguinal approach of fascia iliaca compartment block for postoperative analgesia. Indian J. Anaesth. 2022, 66, S294–S299. [Google Scholar] [PubMed]
- Qian, Y.; Guo, Z.; Huang, J.; Zhang, Q.; An, X.; Hu, H.; Zhu, F.; Wang, X. Electromyographic comparison of the efficacy of ultrasound-guided suprainguinal and infrainguinal fascia iliaca compartment block for blockade of the obturator nerve in total knee arthroplasty: A prospective randomized controlled trial. Clin. J. Pain 2020, 36, 260–266. [Google Scholar] [CrossRef]
- Kantakam, P.; Maikong, N.; Sinthubua, A.; Mahakkanukrauh, P.; Tran, D.Q.; Leurcharusmee, P. Cadaveric investigation of the minimum effective volume for ultrasound-guided suprainguinal fascia iliaca block. Reg. Anesth. Pain Med. 2021, 46, 757–762. [Google Scholar] [CrossRef]
- Bendtsen, T.F.; Pedersen, E.M.; Moriggl, B.; Hebbard, P.; Ivanusic, J.; Børglum, J.; Nielsen, T.D.; Peng, P. Suprainguinal fascia iliaca block: Does it block the obturator nerve? Reg. Anesth. Pain Med. 2021, 46, 832. [Google Scholar] [CrossRef] [PubMed]
- Bendtsen, T.F.; Pedersen, E.M.; Moriggl, B.; Hebbard, P.; Ivanusic, J.; Børglum, J.; Nielsen, T.D.; Peng, P. Anatomical considerations for obturator nerve block with fascia iliaca compartment block. Reg. Anesth. Pain Med. 2021, 46, 806–812. [Google Scholar] [CrossRef]
- Iacovazzo, C.; Sara, R.; Buonanno, P.; Vargas, M.; Coviello, A.; Punzo, R.; Maffei, V.; Marra, A. The effects of the pericapsular nerve group block on postoperative pain in patients with hip fracture: A multicenter study. Diagnostics 2024, 14, 827. [Google Scholar] [CrossRef]
- Girón-Arango, L.; Peng, P.W.; Chin, K.J.; Brull, R.; Perlas, A. Pericapsular nerve group (peng) block for hip fracture. Reg. Anesth. Pain Med. 2018, 43, 859–863. [Google Scholar] [CrossRef]
- Mosaffa, F.; Taheri, M.; Rasi, A.M.; Samadpour, H.; Memary, E.; Mirkheshti, A. Comparison of pericapsular nerve group (peng) block with fascia iliaca compartment block (ficb) for pain control in hip fractures: A double-blind prospective randomized controlled clinical trial. Orthop. Traumatol. Surg. Res. 2022, 108, 103135. [Google Scholar] [CrossRef]
- Behrends, M.; Yap, E.N.; Zhang, A.L.; Kolodzie, K.; Kinjo, S.; Harbell, M.W.; Aleshi, P. Preoperative fascia iliaca block does not improve analgesia after arthroscopic hip surgery, but causes quadriceps muscles weakness: A randomized, double-blind trial. Anesthesiology 2018, 129, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Eshag, M.M.E.; Hasan, L.O.M.; Elshenawy, S.; Ahmed, M.S.; Emad Mostafa, A.E.-M.; Abdelghafar, Y.A.; Althawadi, Y.J.; Ibraheem, N.M.; Badr, H.; AbdelQadir, Y.H. Fascia iliaca compartment block for postoperative pain after total hip arthroplasty: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2024, 24, 95. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Leng, X.; Hu, X.; Cheng, J.; Ao, Y. The effect of fascia iliaca block on postoperative pain and analgesic consumption for patients undergoing primary total hip arthroplasty: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2021, 16, 444. [Google Scholar] [CrossRef]
- Safa, B.; Trinh, H.; Lansdown, A.; McHardy, P.G.; Gollish, J.; Kiss, A.; Kaustov, L.; Choi, S. Ultrasound-guided suprainguinal fascia iliaca compartment block and early postoperative analgesia after total hip arthroplasty: A randomised controlled trial. Br. J. Anaesth. 2024, 133, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, J.; Ondruschka, B.; Prietzel, T.; Zwirner, J.; Hammer, N. A systematic review and meta-analysis of the hip capsule innervation and its clinical implications. Sci. Rep. 2021, 11, 5299. [Google Scholar] [CrossRef]


| Nerves | S-FICB | I-FICB | ||
|---|---|---|---|---|
| 30 mL (n = 3) | 60 mL (n = 3) | 30 mL (n = 3) | 60 mL (n = 3) | |
| Ilioinguinal nerve | --- | +++ | --- | --- |
| Iliohypogastric nerve | --- | +++ | --- | --- |
| Genitofemoral nerve | +++ | +++ | --- | --- |
| Lateral femoral cutaneous nerve | +++ | +++ | +++ | +++ |
| Femoral nerve | +++ | +++ | +++ | +++ |
| Obturator nerve | --- | +++ | --- | --- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, T.-H.; Jun, B.; Yang, H.-M.; Kim, S.H. Comparison of Dye Spread Pattern and Nerve Involvement between Suprainguinal and Infrainguinal Fascia Iliaca Blocks with Different Injectate Volumes: A Cadaveric Evaluation. Medicina 2024, 60, 1391. https://doi.org/10.3390/medicina60091391
Cho T-H, Jun B, Yang H-M, Kim SH. Comparison of Dye Spread Pattern and Nerve Involvement between Suprainguinal and Infrainguinal Fascia Iliaca Blocks with Different Injectate Volumes: A Cadaveric Evaluation. Medicina. 2024; 60(9):1391. https://doi.org/10.3390/medicina60091391
Chicago/Turabian StyleCho, Tae-Hyeon, Byongnam Jun, Hun-Mu Yang, and Shin Hyung Kim. 2024. "Comparison of Dye Spread Pattern and Nerve Involvement between Suprainguinal and Infrainguinal Fascia Iliaca Blocks with Different Injectate Volumes: A Cadaveric Evaluation" Medicina 60, no. 9: 1391. https://doi.org/10.3390/medicina60091391





