The Effect of Anesthesia Type on the Stability of the Surgical View on the Monitor in Retrograde Intrarenal Surgery for Renal Stone: A Prospective Observational Trial
Abstract
1. Introduction
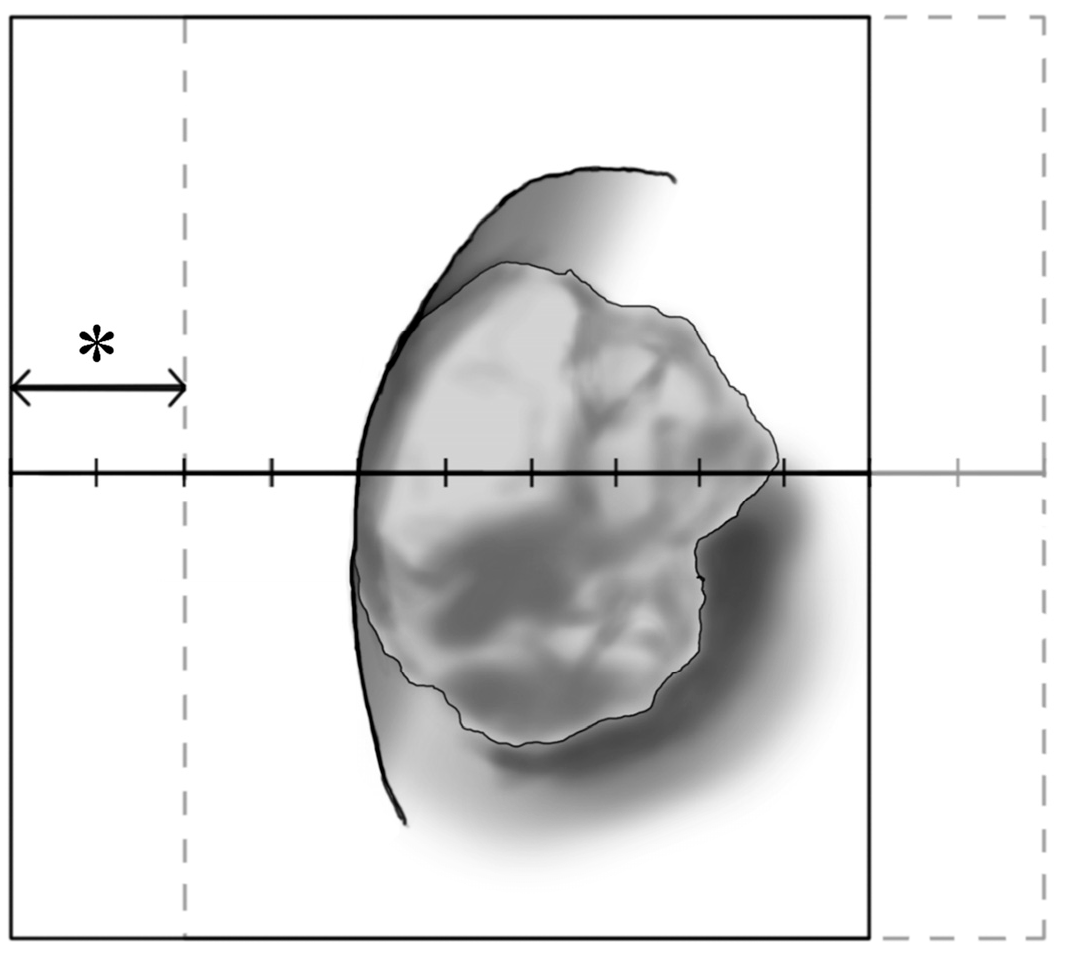
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Inoue, T.; Okada, S.; Hamamoto, S.; Fujisawa, M. Retrograde intrarenal surgery: Past, present, and future. Investig. Clin. Urol. 2021, 62, 121–135. [Google Scholar] [CrossRef]
- Schwartz, L.H.; Richaud, J.; Buffat, L.; Touboul, E.; Schlienger, M. Kidney mobility during respiration. Radiother. Oncol. 1994, 32, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Zeng, G.; Zhao, Z.; Yang, F.; Zhong, W.; Wu, W.; Chen, W. Retrograde intrarenal surgery with combined spinal-epidural vs general anesthesia: A prospective randomized controlled trial. J. Endourol. 2015, 29, 401–405. [Google Scholar] [CrossRef]
- Emiliani, E.; Talso, M.; Baghdadi, M.; Ghanem, S.; Golmard, J.; Pinheiro, H.; Gkentzis, A.; Buttice, S.; Traxer, O. The Use of Apnea During Ureteroscopy. Urology 2016, 97, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Gadzhiev, N.; Oibolatov, U.; Kolotilov, L.; Parvanyan, S.; Akopyan, G.; Petrov, S.; Cottone, C.M.; Sung, J.; Okhunov, Z. Reducing kidney motion: Optimizing anesthesia and combining respiratory support for retrograde intrarenal surgery: A pilot study. BMC Urol. 2019, 19, 61. [Google Scholar] [CrossRef]
- Cho, S.Y.; Park, H.; Park, J.S.; Kim, S.C.; Kwon, O.B.; Song, H.J.; Choi, M.J. Optimizing targeting strategies for lithotripsy through in-vitro and in vivo studies with consideration of respiratory regularity. BMC Urol. 2024, 24, 65. [Google Scholar] [CrossRef] [PubMed]
- Dogan, C.; Sahin, A.; Akgul, H.M.; Yazici, C.M.; Keles, A.; Ates, H.; Seramet, S. Does High Ventilation Mode Affect the Success Rates of Retrograde Intrarenal Surgery? A Single-Blind Randomized, Prospective, Single-Center Study. J. Endourol. 2023, 37, 1169–1173. [Google Scholar] [CrossRef]
- Sahan, M.; Sarilar, O.; Akbulut, M.F.; Demir, E.; Savun, M.; Sen, O.; Ozgor, F. Flexible ureterorenoscopy and laser lithotripsy with regional anesthesia vs general anesthesia: A prospective randomized study. Int. Braz. J. Urol. 2020, 46, 1010–1018. [Google Scholar] [CrossRef]
- Madsen, M.V.; Staehr-Rye, A.K.; Gatke, M.R.; Claudius, C. Neuromuscular blockade for optimising surgical conditions during abdominal and gynaecological surgery: A systematic review. Acta Anaesthesiol. Scand. 2015, 59, 1–16. [Google Scholar] [CrossRef]
- Torensma, B.; Martini, C.H.; Boon, M.; Olofsen, E.; In ’t Veld, B.; Liem, R.S.; Knook, M.T.; Swank, D.J.; Dahan, A. Deep Neuromuscular Block Improves Surgical Conditions during Bariatric Surgery and Reduces Postoperative Pain: A Randomized Double Blind Controlled Trial. PLoS ONE 2016, 11, e0167907. [Google Scholar] [CrossRef]
- Bruintjes, M.H.; van Helden, E.V.; Braat, A.E.; Dahan, A.; Scheffer, G.J.; van Laarhoven, C.J.; Warle, M.C. Deep neuromuscular block to optimize surgical space conditions during laparoscopic surgery: A systematic review and meta-analysis. Br. J. Anaesth. 2017, 118, 834–842. [Google Scholar] [CrossRef]
- Ledowski, T.; Goodwin-Walters, A.; Quinn, P.; Calvert, M. The effect of deep muscle relaxation on the force required during Latissimus Dorsi dissection for breast reconstructive surgery: Results of a prospective, double-blinded observational pilot study. BMC Anesthesiol. 2017, 17, 27. [Google Scholar] [CrossRef][Green Version]
- Rosenberg, J.; Herring, W.J.; Blobner, M.; Mulier, J.P.; Rahe-Meyer, N.; Woo, T.; Li, M.K.; Grobara, P.; Assaid, C.A.; Fennema, H.; et al. Deep Neuromuscular Blockade Improves Laparoscopic Surgical Conditions: A Randomized, Controlled Study. Adv. Ther. 2017, 34, 925–936. [Google Scholar] [CrossRef]
- Ozdemir-van Brunschot, D.M.D.; Braat, A.E.; van der Jagt, M.F.P.; Scheffer, G.J.; Martini, C.H.; Langenhuijsen, J.F.; Dam, R.E.; Huurman, V.A.; Lam, D.; d’Ancona, F.C.; et al. Deep neuromuscular blockade improves surgical conditions during low-pressure pneumoperitoneum laparoscopic donor nephrectomy. Surg. Endosc. 2018, 32, 245–251. [Google Scholar] [CrossRef]
- Srisubat, A.; Potisat, S.; Lojanapiwat, B.; Setthawong, V.; Laopaiboon, M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst. Rev. 2014, 11, CD007044. [Google Scholar] [CrossRef]
- Froese, A.B.; Bryan, A.C. Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology 1974, 41, 242–255. [Google Scholar] [CrossRef] [PubMed]
- Krayer, S.; Rehder, K.; Vettermann, J.; Didier, E.P.; Ritman, E.L. Position and motion of the human diaphragm during anesthesia-paralysis. Anesthesiology 1989, 70, 891–898. [Google Scholar] [CrossRef]
- Wang, J.J.; Ho, S.T.; Liu, H.S.; Tzeng, J.I.; Tze, T.S.; Liaw, W.J. The effect of spinal versus general anesthesia on postoperative pain and analgesic requirements in patients undergoing lower abdominal surgery. Reg. Anesth. 1996, 21, 281–286. [Google Scholar] [PubMed]
- Gonano, C.; Leitgeb, U.; Sitzwohl, C.; Ihra, G.; Weinstabl, C.; Kettner, S.C. Spinal versus general anesthesia for orthopedic surgery: Anesthesia drug and supply costs. Anesth. Analg. 2006, 102, 524–529. [Google Scholar] [CrossRef]
- Imbelloni, L.E.; Fornasari, M.; Fialho, J.C.; Sant’Anna, R.; Cordeiro, J.A. General anesthesia versus spinal anesthesia for laparoscopic cholecystectomy. Rev. Bras. Anestesiol. 2010, 60, 217–227. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kessous, R.; Weintraub, A.Y.; Wiznitzer, A.; Zlotnik, A.; Pariente, G.; Polachek, H.; Press, F.; Aricha-Tamir, B.; Leizerovich, A.; Sheiner, E. Spinal versus general anesthesia in cesarean sections: The effects on postoperative pain perception. Arch. Gynecol. Obstet. 2012, 286, 75–79. [Google Scholar] [CrossRef]
- Naghibi, K.; Saryazdi, H.; Kashefi, P.; Rohani, F. The comparison of spinal anesthesia with general anesthesia on the postoperative pain scores and analgesic requirements after elective lower abdominal surgery: A randomized, double-blinded study. J. Res. Med. Sci. 2013, 18, 543–548. [Google Scholar] [PubMed]
- Seehusen, D.A.; Johnson, D.R.; Earwood, J.S.; Sethuraman, S.N.; Cornali, J.; Gillespie, K.; Doria, M.; Farnell, E.t.; Lanham, J. Improving women’s experience during speculum examinations at routine gynaecological visits: Randomised clinical trial. BMJ 2006, 333, 171. [Google Scholar] [CrossRef]
- Moettus, A.; Sklar, D.; Tandberg, D. The effect of physician gender on women’s perceived pain and embarrassment during pelvic examination. Am. J. Emerg. Med. 1999, 17, 635–637. [Google Scholar] [CrossRef] [PubMed]
- Capdevila, X.; Aveline, C.; Delaunay, L.; Bouaziz, H.; Zetlaoui, P.; Choquet, O.; Jouffroy, L.; Herman-Demars, H.; Bonnet, F. Factors Determining the Choice of Spinal Versus General Anesthesia in Patients Undergoing Ambulatory Surgery: Results of a Multicenter Observational Study. Adv. Ther. 2020, 37, 527–540. [Google Scholar] [CrossRef] [PubMed]
- El-Boghdadly, K.; Bailey, C.R.; Wiles, M.D. Postoperative sore throat: A systematic review. Anaesthesia 2016, 71, 706–717. [Google Scholar] [CrossRef]
- Gan, T.J.; Belani, K.G.; Bergese, S.; Chung, F.; Diemunsch, P.; Habib, A.S.; Jin, Z.; Kovac, A.L.; Meyer, T.A.; Urman, R.D.; et al. Fourth Consensus Guidelines for the Management of Postoperative Nausea and Vomiting. Anesth. Analg. 2020, 131, 411–448. [Google Scholar] [CrossRef]
- Chu, L.; Sternberg, K.M.; Averch, T.D. Preoperative stenting decreases operative time and reoperative rates of ureteroscopy. J. Endourol. 2011, 25, 751–754. [Google Scholar] [CrossRef]
- Assimos, D.; Krambeck, A.; Miller, N.L.; Monga, M.; Murad, M.H.; Nelson, C.P.; Pace, K.T.; Pais, V.M., Jr.; Pearle, M.S.; Preminger, G.M.; et al. Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART I. J. Urol. 2016, 196, 1153–1160. [Google Scholar] [CrossRef]
- Sorokin, I.; Cardona-Grau, D.K.; Rehfuss, A.; Birney, A.; Stavrakis, C.; Leinwand, G.; Herr, A.; Feustel, P.J.; White, M.D. Stone volume is best predictor of operative time required in retrograde intrarenal surgery for renal calculi: Implications for surgical planning and quality improvement. Urolithiasis 2016, 44, 545–550. [Google Scholar] [CrossRef]
- Whitehurst, L.; Pietropaolo, A.; Geraghty, R.; Kyriakides, R.; Somani, B.K. Factors affecting operative time during ureteroscopy and stone treatment and its effect on outcomes: Retrospective results over 6.5 years. Ther. Adv. Urol. 2020, 12, 1756287220934403. [Google Scholar] [CrossRef] [PubMed]
- Dexter, F.; Aker, J.; Wright, W.A. Development of a measure of patient satisfaction with monitored anesthesia care: The Iowa Satisfaction with Anesthesia Scale. Anesthesiology 1997, 87, 865–873. [Google Scholar] [CrossRef]
| Patient Characteristics | G Group | S Group | p-Value |
|---|---|---|---|
| (n = 34) | (n = 32) | ||
| Sex (M/F) | 18/16 | 21/11 | 0.295 |
| Age (y) | 55.6 ± 15.7 | 51.5 ± 13.9 | 0.268 |
| Height (cm) | 162.2 ± 10.9 | 163.3 ± 9.8 | 0.668 |
| Weight (kg) | 64.8 ± 15.0 | 67.4 ± 12.2 | 0.433 |
| BMI (kg/m2) | 24.4 ± 3.8 | 25.3 ± 4.0 | 0.380 |
| ASA physical status class (I/II/III) | 16/13/5 | 19/12/1 | 0.234 |
| Operation Characteristics | G Group | S Group | p-Value |
|---|---|---|---|
| (n = 34) | (n = 32) | ||
| Dominant stone type | 6/22/1/3/0 | 2/26/0/0/3 | 0.054 |
| (UA/COM/COD/St/CA) | |||
| Stone position | 17/8/7 | 18/8/6 | 0.949 |
| (LK/RK/BK) | |||
| Number of stones | 2 [1, 3] | 2 [1, 3] | 0.649 |
| Total stone volume (cm3) | 0.5 [0.2, 0.9] | 0.4 [0.2, 0.8] | 0.496 |
| Lasing time (min) | 21 [10, 35] | 20 [5, 30] | 0.418 |
| Operation time (min) | 62 [45, 90] | 50 [39, 67] | 0.048 |
| Anesthesia time (min) | 101 ± 36 | 82 ± 25 | 0.014 |
| Surgical Field Oscillation | G Group | S Group | MD (95% CI) | p-Value |
|---|---|---|---|---|
| (n = 34) | (n = 32) | |||
| Grade 1 | 3.3 ± 1.5 | 5.2 ± 1.7 | 1.9 ± 0.4 (1.1, 2.7) | <0.001 |
| Grade 2 | 3.3 ± 1.8 | 4.8 ± 1.7 | 1.5 ± 0.4 (0.7, 2.4) | <0.001 |
| AG | 3.3 ± 1.6 | 5.0 ± 1.6 | 1.7 ± 0.4 (1.0, 2.5) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Won, D.; Cho, S.Y.; No, H.-J.; Lee, J.; Hwang, J.-Y.; Kim, T.K.; Chang, J.-E.; Kim, H.; Choi, J.-H.; Lee, J.-M. The Effect of Anesthesia Type on the Stability of the Surgical View on the Monitor in Retrograde Intrarenal Surgery for Renal Stone: A Prospective Observational Trial. Medicina 2024, 60, 1435. https://doi.org/10.3390/medicina60091435
Won D, Cho SY, No H-J, Lee J, Hwang J-Y, Kim TK, Chang J-E, Kim H, Choi J-H, Lee J-M. The Effect of Anesthesia Type on the Stability of the Surgical View on the Monitor in Retrograde Intrarenal Surgery for Renal Stone: A Prospective Observational Trial. Medicina. 2024; 60(9):1435. https://doi.org/10.3390/medicina60091435
Chicago/Turabian StyleWon, Dongwook, Sung Yong Cho, Hyun-Joung No, Jiwon Lee, Jin-Young Hwang, Tae Kyong Kim, Jee-Eun Chang, Hyerim Kim, Jae-Hyun Choi, and Jung-Man Lee. 2024. "The Effect of Anesthesia Type on the Stability of the Surgical View on the Monitor in Retrograde Intrarenal Surgery for Renal Stone: A Prospective Observational Trial" Medicina 60, no. 9: 1435. https://doi.org/10.3390/medicina60091435
APA StyleWon, D., Cho, S. Y., No, H.-J., Lee, J., Hwang, J.-Y., Kim, T. K., Chang, J.-E., Kim, H., Choi, J.-H., & Lee, J.-M. (2024). The Effect of Anesthesia Type on the Stability of the Surgical View on the Monitor in Retrograde Intrarenal Surgery for Renal Stone: A Prospective Observational Trial. Medicina, 60(9), 1435. https://doi.org/10.3390/medicina60091435






