Clinical Presentations and Outcomes of Pediatric Rhegmatogenous Retinal Detachment: 11 Years’ Experience at a Tertiary Eye Center
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Past Ocular and Systemic History
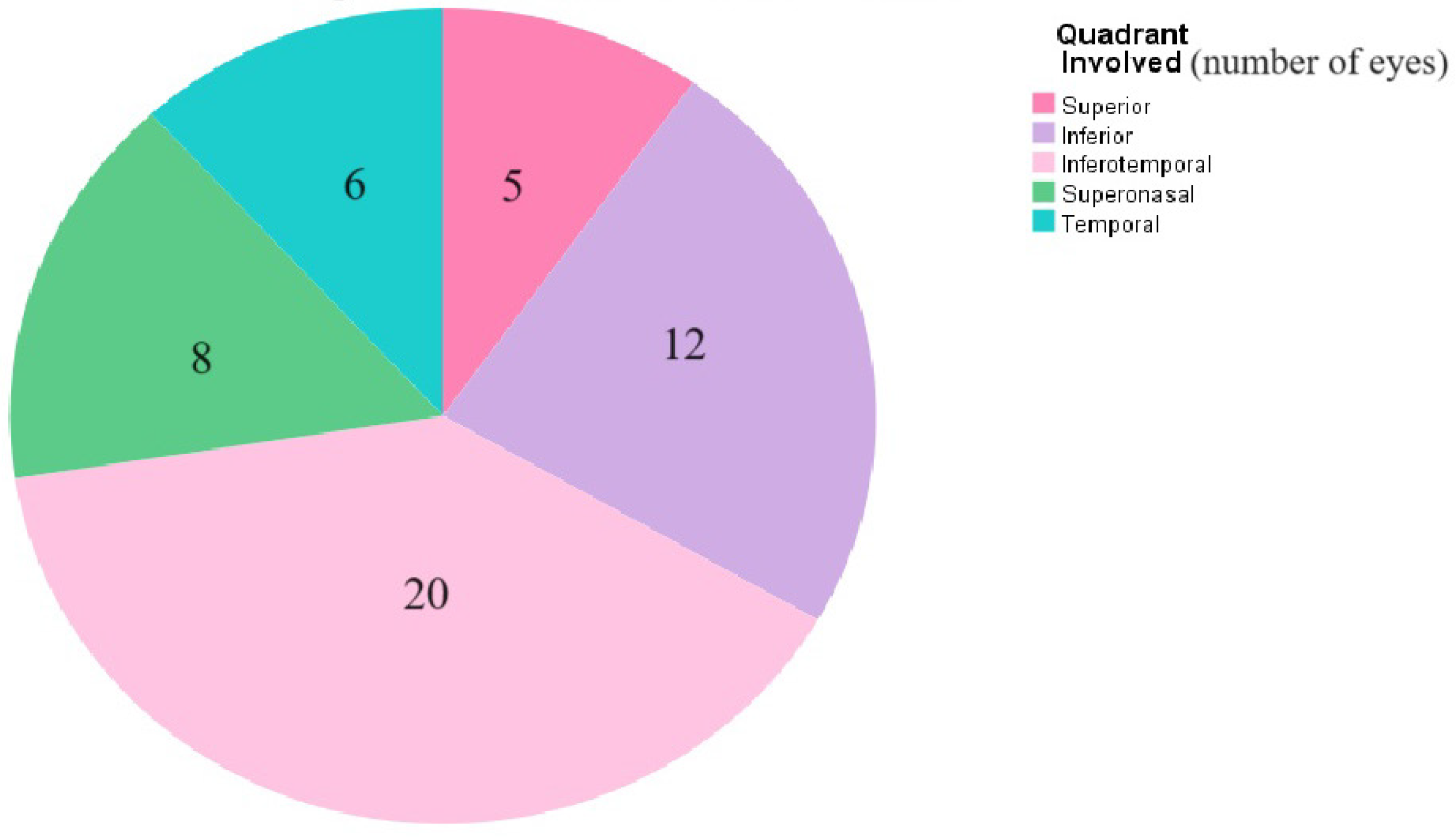
3.2. Examination on Presentation
3.3. Primary and Secondary Surgical Intervention in Children with RRD
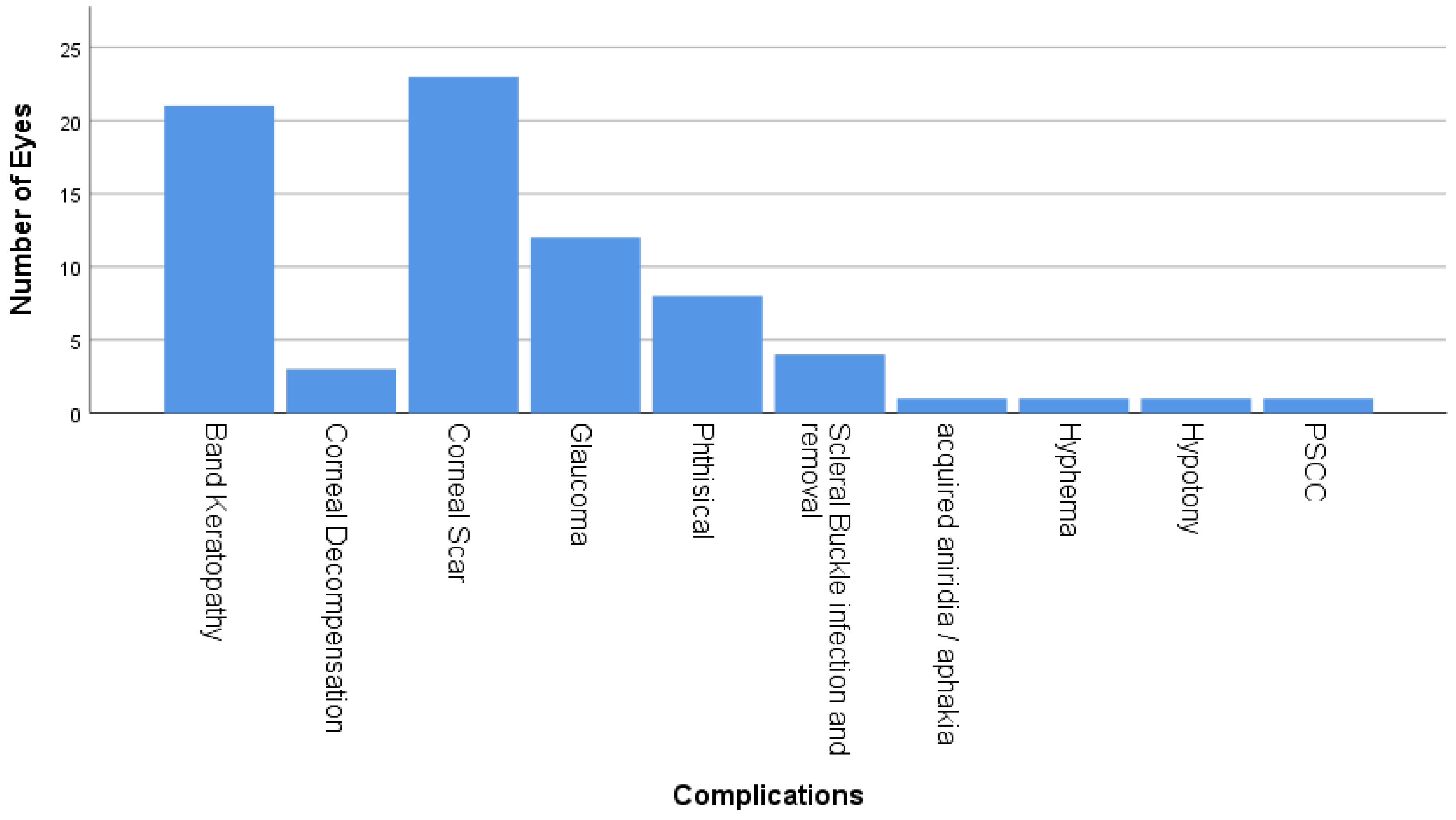
3.4. Complications Postoperatively
3.5. Final Visual Outcomes
3.6. Risk Factors for RRD
3.7. Factors Associated with Final Visual Acuity
3.8. Comparison of Initial and Final Visual Acuity:
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghazi, N.; Green, W. Pathology and pathogenesis of retinal detachment. Eye 2002, 16, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, C.D.; Peto, T.; Grauslund, J.; Green, A. Epidemiologic characteristics of retinal detachment surgery at a specialized unit in Denmark. Acta Ophthalmol. 2016, 94, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Meier, P. Retinal detachment in children: Differential diagnosis and current therapy. Klin. Monbl. Augenheilkd. 2008, 225, 779–790. [Google Scholar] [CrossRef] [PubMed]
- Winslow, R.L.; Tasman, W. Juvenile rhegmatogenous retinal detachment. Ophthalmology 1978, 85, 607–618. [Google Scholar] [CrossRef]
- Butler, T.K.H.; Kiel, A.W.; Orr, G.M. Anatomical and visual outcome of retinal detachment surgery in children. Br. J. Ophthalmol. 2001, 85, 1437–1439. [Google Scholar] [CrossRef]
- Haring, G.; Wiechens, B. Long-term results after scleral buckling surgery in uncomplicated juvenile retinal detachment without proliferative vitreoretinopathy. Retina 1998, 18, 501–505. [Google Scholar] [CrossRef]
- Akabane, N.; Yamamoto, S.; Tsukahara, I.; Ishida, M.; Mitamura, Y.; Yamamoto, T.; Takeuchi, S. Surgical outcomes in juvenile retinal detachment. Jpn. J. Ophthalmol. 2001, 45, 409–411. [Google Scholar] [CrossRef]
- Fivgas, G.D.; Capone, A., Jr. Pediatric rhegmatogenous retinal detachment. Retina 2001, 21, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, D.V.; Lyon, A.T.; Greenwald, M.J.; Mets, M.B. Rhegmatogenous retinal detachments in children: Risk factors and surgical outcomes. Ophthalmology 2003, 110, 1708–1713. [Google Scholar] [CrossRef]
- Sarrazin, L.; Averbukh, E.; Halpert, M.; Hemo, I.; Rumelt, S. Traumatic paediatric retinal detachment: A comparison between open and closed globe injuries. Am. J. Ophthalmol. 2004, 137, 1042–1049. [Google Scholar] [CrossRef]
- Yokoyama, T.; Kato, T.; Minamoto, A.; Sugihara, A.; Imada, M.; Kuwabara, R. Characteristics and surgical outcomes of paediatric retinal detachment. Eye 2004, 18, 889–892. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.-Y.; Yang, C.-M.; Yang, C.-H.; Huang, J.-S.; Ho, T.-C.; Lin, C.-P.; Chen, M.-S.; Chen, L.-J.; Wang, J.-Y. Clinical characteristics and surgical outcomes of pediatric rhegmatogenous retinal detachment in Taiwan. Am. J. Ophthalmol. 2005, 139, 1067–1072. [Google Scholar] [CrossRef]
- Wang, N.K.; Tsai, C.-H.; Chen, Y.-P.; Yeung, L.; Wu, W.C.; Chen, T.L. Pediatric rhegmatogenous retinal detachment in East Asians. Ophthalmology 2005, 112, 1890–1895. [Google Scholar] [CrossRef]
- Rumelt, S.; Sarrazin, L.; Averbukh, E.; Halpert, M.; Hemo, I. Paediatric vs adult retinal detachment. Eye 2007, 21, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, C.R.; Singh, S.; Yu, F.; Kreiger, A.E.; Gupta, A.; Schwartz, S.D. Pediatric rhegmatogenous retinal detachment: Clinical features and surgical outcomes. Retina 2008, 28, 847–852. [Google Scholar] [CrossRef]
- Wadhwa, N.; Venkatesh, P.; Sampangi, R.; Garg, S. Rhegmatogenous retinal detachments in children in India: Clinical characteristics, risk factors, and surgical outcomes. J. AAPOS 2008, 12, 551–554. [Google Scholar] [CrossRef] [PubMed]
- Soheilian, M.; Ramezani, A.; Malihi, M.; Yaseri, M.; Ahmadieh, H.; Dehghan, M.H.; Azarmina, M.; Moradian, S.; Peyman, G.A. Clinical features and surgical outcomes of pediatric rhegmatogenous retinal detachment. Retina 2009, 29, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Oono, Y.; Uehara, K.; Haruta, M.; Yamakawa, R. Characteristics and surgical outcomes of pediatric rhegmatogenous retinal detachment. Clin. Ophthalmol. 2012, 6, 939–943. [Google Scholar] [CrossRef]
- Al-Zaaidi, S.; Al Rashaed, S.; Kahtani, A.; Asrar, E.; Harthi, A. Rhegmatogenous retinal detachment in children 16 years of age or younger. Clin. Ophthalmol. 2013, 7, 1001–1014. [Google Scholar] [CrossRef]
- Scharf, J.; Zonis, S. Juvenile retinal detachment. J. Pediatr. Ophthalmol. 1977, 14, 302–304. [Google Scholar] [CrossRef]
- Hudson, J.R. Retinal detachments in children. Trans. Ophthalmol. Soc. 1965, 85, 79–91. [Google Scholar]
- Haimann, M.H.; Burton, T.C.; Brown, C.K. Epidemiology of retinal detachment. Arch. Ophthalmol. 1982, 100, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Smiddy, W.E.; Green, W.R. Retinal dialysis: Pathology and pathogenesis. Retina 1982, 2, 94–116. [Google Scholar] [CrossRef] [PubMed]
- Okinami, S.; Ogino, N.; Nishimura, T.; Tano, Y. Juvenile retinal detachment. Ophthalmologica 1987, 194, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Sadeh, A.D.; Dotan, G.; Bracha, R.; Lazar, M.; Loewenstein, A. Characteristics and outcomes of paediatric rhegmatogenous retinal detachment treated by segmental scleral buckling plus an encircling element. Eye 2001, 15, 31–33. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nagpal, M.; Nagpal, K.; Rishi, P.; Nagpal, P.N. Juvenile rhegmatogenous retinal detachment. Indian J. Ophthalmol. 2004, 52, 297–302. [Google Scholar]
- Kocaoglan, H.; Unlü, N.; Acar, M.A.; Sargin, M.; Aslan, B.S.; Duman, S. The efficacy of conventional rhegmatogenous retinal detachment surgery in the pediatric population. J. Pediatr. Ophthalmol. Strabismus. 2003, 40, 4–5. [Google Scholar] [CrossRef]

| First Author | Eyes/ Patients (n) | Mean Age (a); Sex (M/F,%) | Traumatic/Myopic/Congenital-Developmental/Other (%) | No. of Interventions (Mean) | Primary S.B/Vitrectomy (%) | Total Vitrectomy (%) | Combined S.B-Vitrectomy (%) | Use of Silicone Oil (%) |
|---|---|---|---|---|---|---|---|---|
| Haring [6] 1998 | 33/31 | 15; 54/46 | 24/42/0/NR | 1.2 | 100/0 | 3 | 0 | NR |
| Akabane [7] 2001 | 32/28 | 12.8; 65/35 | 22/38/16/24 | NR | 78/22 | 31 | 0 | NR |
| Fivgas [8] 2001 | 29/27 | 9.6; 70/30 | 25–60/3/45/51 | 2.2 | 28/72 | 92 | 0 | 72 |
| Weinberg [9] 2003 | 39/34 | 9.2; 79/21 | 36/NR/53/15 | 1.6 | 41/13 | 67 | 46 | 23 |
| Sarrazin [10] 2007 | 37/36 | 11; 86/14 | 100/0/0/0 | 74% > 1; Range 1–4 | NR | NR | 100 | 54 |
| Yokoyama [11] 2004 | 55/49 | 12; 86/14 | 27 /25(>4 D)/15/33 | 1.2 | 76/24 | 38 | 0 | NR |
| Chang [12] 2005 | 152/146 | 13.1; 70/30 | 33/37/12/17 | 1.5 | 61/39 | 44 | see vitrectomy | 32 |
| Wang [13] 2014 | 296/278 | 14.6; 74/26 | 31/79; 38 (>6 D)/17/0 | 1.34 | 76/5 | 55 | 19 | 9 |
| Rumelt [14] 2007 | 144/127 (115 RRD) | 10.8; 73/27 | 42/14; 3 (>6 D)/36/22 | 67% 1; 19% 2; 14% 3 to 8 | NR | NR | NR | NR |
| Gonzales [15] 2008 | 46/45 | 9.8; 71/29 | 43/17 (>4 D)/35/11 | 50% > 1 (range 1–3) | 26/44 | 74 | 30 | 57 |
| Wadhwa [16] 2008 | 230/216 | 11.1; 82/18 | 34/14/24/28 | 1.98 | 37/0 (see association) | 69 | 63 | 69 |
| Soheilian [17] 2009 | 127/108 | 12.1; 81/19 | 43/9 (8 > 8 D)/38 (some)/2 | 1.55 | 31/0 (see association) | 75 | 63 | 65 |
| Oono [18] 2012 | 48/44 | 12.3; 88/12 | 38 /44 (>3 D); 25 (alone)/10/27 | 1.46 | 77/23 | NR | 0 | 19 |
| Marfan Syndrome | Dominant Mutations in the Fibrillin-1 | If there’s RD in One Eye Other Eye will be Affected in around 70% |
|---|---|---|
| Wagner disease and erosive vitreoretinopathy | Autosomal dominant vitreoretinopathy caused by mutations in the VCAN gene 3. | Myopia, night blindness, presenile cataract, retinal detachment, optically empty central vitreous, peripheral strands and veils, chorioretinal atrophy, adult-onset glaucoma and ocular hypertension have been reported. |
| Stickler syndrome | Autosomal dominant. Mutations reported in COL2A1, COL11A1, COL11A2, COL9A1, and COL9A2 genes. | Most common ophthalmic complication of stickler in RD accounts for around 70%. |
| Knobloch syndrome | Autosomal recessive disorder caused by mutation in the COL18A1 gene. | Characterized by high myopia ranging from (−10 to −20 D), vitreoretinal degeneration with retinal detachment, and occipital encephalocele. |
| X-linked juvenile retinoschisis | Affects males early in life; mutation of RS1 gene. | It is characterized by radial streaks in macula secondary to foveal schisis as well as splitting of the peripheral temporal retina. RD can occur only after break of both inner and outer retinal layers. |
| Choroidal coloboma | Inherited or can occur sporadically. Can happen secondary to failure of closure of the embryonic fissure. | RRD secondary to congenital colobomas has been reported to reach up to 8% in children. |
| Retinal vascular disease | Retinal vascular disease is a usual cause of tractional retinal detachment but rhegmatogenous retinal detachments (RRDs) can also occur as late sequelae of tractional retinal detachments. | Retinal vascular diseases can cause RRD including regressed retinopathy of prematurity (ROP), familial exudative vitreoretinopathy (FEVR), persistent fetal vasculature, incontinentia pigmenti, uveitis, and sickle cell retinopathy. |
| Characteristic | N (%) |
|---|---|
| Age in years (mean ± SD [range], median) | 10.1 ± 4.6 [2–18], 10.0 |
| Gender | |
| Male | 49 (70.0) |
| Female | 21 (30.0) |
| Laterality | |
| Right Eye | 31 (44.3) |
| Left eye | 20 (28.6) |
| Both eyes | 19 (27.1) |
| History of Previous Ocular Surgeries | |
| Cataract extraction + intraocular lens implantation | 3 (3.4) |
| Trabeculectomy | 5 (5.6) |
| Ahmed valve implant | 1 (1.1) |
| Lens aspiration + anterior vitrectomy | 7 (4.2) |
| Deep sclerotomy | 1 (1.1) |
| PPV + PPL + silicone oil | 2 (2.2) |
| Primary repair then, PPV, PPL removal of an intraocular foreign body | 4 (4.5) |
| Primary repair + penetrating keratoplasty later on | 1 (1.1) |
| Interval between the previous surgery and the diagnosis of RRD in days (mean ± SD [range], median) | 1533 ± 1388 [2–4280], 1265 |
| Predisposing Ocular Pathologies | 58 (65.2) |
| Stickler syndrome | 22 (37.9) |
| Congenital cataract | 7 (12.1) |
| High myopia | 12 (20.7) |
| Congenital glaucoma | 5 (8.6) |
| Retinopathy of prematurity | 5 (8.6) |
| Primary congenital glaucoma | 2 (3.4) |
| Anterior uveitis | 1 (1.1) |
| Optic nerve coloboma | 1 (1.1) |
| Familial exudative vitreoretinopathy | 1 (1.1) |
| Nanophthalmos | 1 (1.1) |
| Paras planitis | 1 (1.1) |
| Sickle cell anemia | 1 (1.1) |
| Family History of Congenital Syndromes | 19 (27.1) |
| Stickler | 14 (73.7) |
| Down syndrome | 2 (10.6) |
| Familial exudative vitreoretinopathy | 1 (5.3) |
| Joubert syndrome | 1 (5.3) |
| Sickle cell anemia | 1 (5.3) |
| Final VA | |
| ≥20/200 | 37 (41.6) |
| CF | 15 (16.9) |
| NLP-HM | 31 (34.8) |
| Final IOP | |
| Low | 1 (1.1) |
| Normal | 68 (76.4) |
| High | 3 (3.4) |
| Attached Retina | 85 (95.5) |
| Follow-up duration in months (mean ± SD [range], median) | 33.7 ± 31.8 [2–144], 24.0 |
| Variable | Failed Primary Surgery—Yes (n = 26) n (%) | p Value |
|---|---|---|
| Gender | ||
| Male (n = 67) | 22 (32.8) | 0.190 |
| Female (n = 22) | 4 (18.2) | |
| Age in years | ||
| ≤5 (n = 21) | 6 (28.6) | 0.941 |
| >5 (n = 68) | 20 (29.4) | |
| Laterality | ||
| Unilateral (n = 51) | 13 (25.5) | 0.371 |
| Bilateral (n = 38) | 13 (34.2) | |
| Trauma | ||
| Yes (n = 23) | 7 (30.4) | 0.881 |
| No (n = 66) | 19 (28.8) | |
| Underwent primary repair | ||
| Yes (n = 5) | 1 (20.0) | 0.641 |
| No (n = 84) | 25 (29.8) | |
| Past ocular history | ||
| Congenital cataract | ||
| Yes (n = 9) | 3 (33.3) | 0.774 |
| No (n = 80) | 23 (28.8) | |
| Congenital glaucoma | ||
| Yes (n = 7) | 3 (42.9) | 0.408 |
| No (n = 82) | 23 (28.0) | |
| Visual acuity at presentation (20 missing) | ||
| HM-LP/NLP (n = 33) | 12 (36.4) | 0.347 |
| CF (n = 27) | 6 (22.2) | |
| ≥20/200 (n = 9) | 4 (44.4) | |
| Proliferative vitreoretinopathy on presentation | ||
| Yes (n = 52) | 18 (34.6) | 0.184 |
| No (n = 37) | 8 (21.6) | |
| Macula | ||
| On (n = 5) | 1 (20.0) | 0.641 |
| Off (n = 84) | 25 (29.8) | |
| Lens status at presentation | ||
| Phakic (n = 48) | 8 (16.7) | 0.017 * |
| Cataract (n = 26) | 12 (46.2) | |
| Aphakia/pseudophakia (n = 15) | 6 (40.0) | |
| Preoperative IOP | ||
| Normal (n = 84) | 24 (28.6) | 0.585 |
| High (n = 5) | 2 (40.0) | |
| Surgical procedures | ||
| Pars plana lens aspiration | ||
| Yes (n = 51) | 19 (37.3) | 0.053 |
| No (n = 38) | 7 (18.4) | |
| Encircling band | ||
| Yes (n = 71) | 22 (31.0) | 0.465 |
| No (n = 18) | 4 (22.2) | |
| Peeling of posterior hyaloid | ||
| Yes (n = 28) | 6 (21.4) | 0.274 |
| No (n = 61) | 20 (32.8) |
| Variable | Good Vision ≥20/200 Yes (n = 31) n (%) | p Value |
|---|---|---|
| Gender | ||
| Male (n = 63) | 27 (42.9) | 0.066 |
| Female (n = 20) | 4 (20.0) | |
| Age in years | ||
| ≤5 (n = 18) | 1 (5.6) | 0.002 * |
| >5 (n = 65) | 30 (46.2) | |
| Laterality | ||
| Unilateral (n = 49) | 16 (32.7) | 0.288 |
| Bilateral (n = 34) | 15 (44.1) | |
| Trauma | ||
| Yes (n = 23) | 9 (39.1) | 0.835 |
| No (n = 60) | 22 (36.7) | |
| Underwent primary repair | ||
| Yes (n = 5) | 3 (60.0) | 0.280 |
| No (n = 78) | 28 (35.9) | |
| Past ocular history | ||
| Congenital cataract | ||
| Yes (n = 9) | 2 (22.2) | 0.320 |
| No (n = 74) | 29 (39.2) | |
| Congenital glaucoma | ||
| Yes (n = 6) | 1 (16.7) | 0.277 |
| No (n = 77) | 30 (39.0) | |
| Visual acuity at presentation (17 missing) | ||
| HM-LP/NLP (n = 31) | 9 (29.0) | 0.031 * |
| CF (n = 26) | 10 (38.5) | |
| ≥20/200 (n = 9) | 7 (77.8) | |
| Proliferative vitreoretinopathy on presentation | ||
| Yes (n = 48) | 12 (25.0) | 0.006 * |
| No (n = 35) | 19 (54.3) | |
| Macula | ||
| On (n = 5) | 3 (60.0) | 0.280 |
| Off (n = 78) | 28 (35.9) | |
| Lens status at presentation | ||
| Phakic (n = 46) | 23 (50.0) | 0.025 * |
| Cataract (n = 24) | 6 (25.0) | |
| Aphakia/pseudophakia (n = 13) | 2 (15.4) | |
| Preoperative IOP | ||
| Normal (n = 78) | 30 (38.5) | 0.408 |
| High (n = 5) | 1 (20.0) | |
| Surgical procedures | ||
| PPL lens aspiration | ||
| Yes (n = 48) | 16 (33.3) | 0.376 |
| No (n = 35) | 15 (42.9) | |
| Encircling band | ||
| Yes (n = 67) | 25 (37.3) | 0.989 |
| No (n = 16) | 6 (37.5) | |
| Peeling of posterior hyaloid | ||
| Yes (n = 25) | 13 (52.0) | 0.070 |
| No (n = 58) | 18 (31.0) | |
| Tamponade used (n = 80) | ||
| Gas (n = 4) | 4 (100) | 0.006 * |
| Silicone oil (n = 76) | 27 (37.4) |
| Final Visual Acuity | Visual Acuity at Presentation | Total | ||
|---|---|---|---|---|
| NLP/LP-HM | CF | ≥20/200 | ||
| ≥20/200 | 9 | 10 | 7 | 26 (39.4%) |
| CF | 4 | 7 | 1 | 12 (18.2%) |
| NLP/LP-HM | 18 | 9 | 1 | 28 (42.4%) |
| Total | 31 (47.0%) | 26 (39.4%) | 9 (13.6%) | 66 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alabbasi, O.; Magliyah, M.S.; Albalawi, H.B.; Alsharif, H.M.; Alsharif, E.M.; Abu El-Asrar, A. Clinical Presentations and Outcomes of Pediatric Rhegmatogenous Retinal Detachment: 11 Years’ Experience at a Tertiary Eye Center. Medicina 2024, 60, 1442. https://doi.org/10.3390/medicina60091442
Alabbasi O, Magliyah MS, Albalawi HB, Alsharif HM, Alsharif EM, Abu El-Asrar A. Clinical Presentations and Outcomes of Pediatric Rhegmatogenous Retinal Detachment: 11 Years’ Experience at a Tertiary Eye Center. Medicina. 2024; 60(9):1442. https://doi.org/10.3390/medicina60091442
Chicago/Turabian StyleAlabbasi, Omar, Moustafa S. Magliyah, Hani Basher Albalawi, Heba M. Alsharif, Eman M. Alsharif, and Ahmed Abu El-Asrar. 2024. "Clinical Presentations and Outcomes of Pediatric Rhegmatogenous Retinal Detachment: 11 Years’ Experience at a Tertiary Eye Center" Medicina 60, no. 9: 1442. https://doi.org/10.3390/medicina60091442
APA StyleAlabbasi, O., Magliyah, M. S., Albalawi, H. B., Alsharif, H. M., Alsharif, E. M., & Abu El-Asrar, A. (2024). Clinical Presentations and Outcomes of Pediatric Rhegmatogenous Retinal Detachment: 11 Years’ Experience at a Tertiary Eye Center. Medicina, 60(9), 1442. https://doi.org/10.3390/medicina60091442








