Immune mRNA Expression and Fecal Microbiome Composition Change Induced by Djulis (Chenopodium formosanum Koidz.) Supplementation in Aged Mice: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of Djulis (C. formosanum) Powder
2.2. Experimental Aged Mice
2.3. Histopathological Analysis of Aged Mice’s Lungs
2.4. Synthesis of cDNA
2.5. Real-Time PCR for the mRNA Expression of Cytokines, T Cells, and Toll-like Receptors
2.6. Fecal Microbiome Analysis
2.7. Statistical Analysis
3. Results
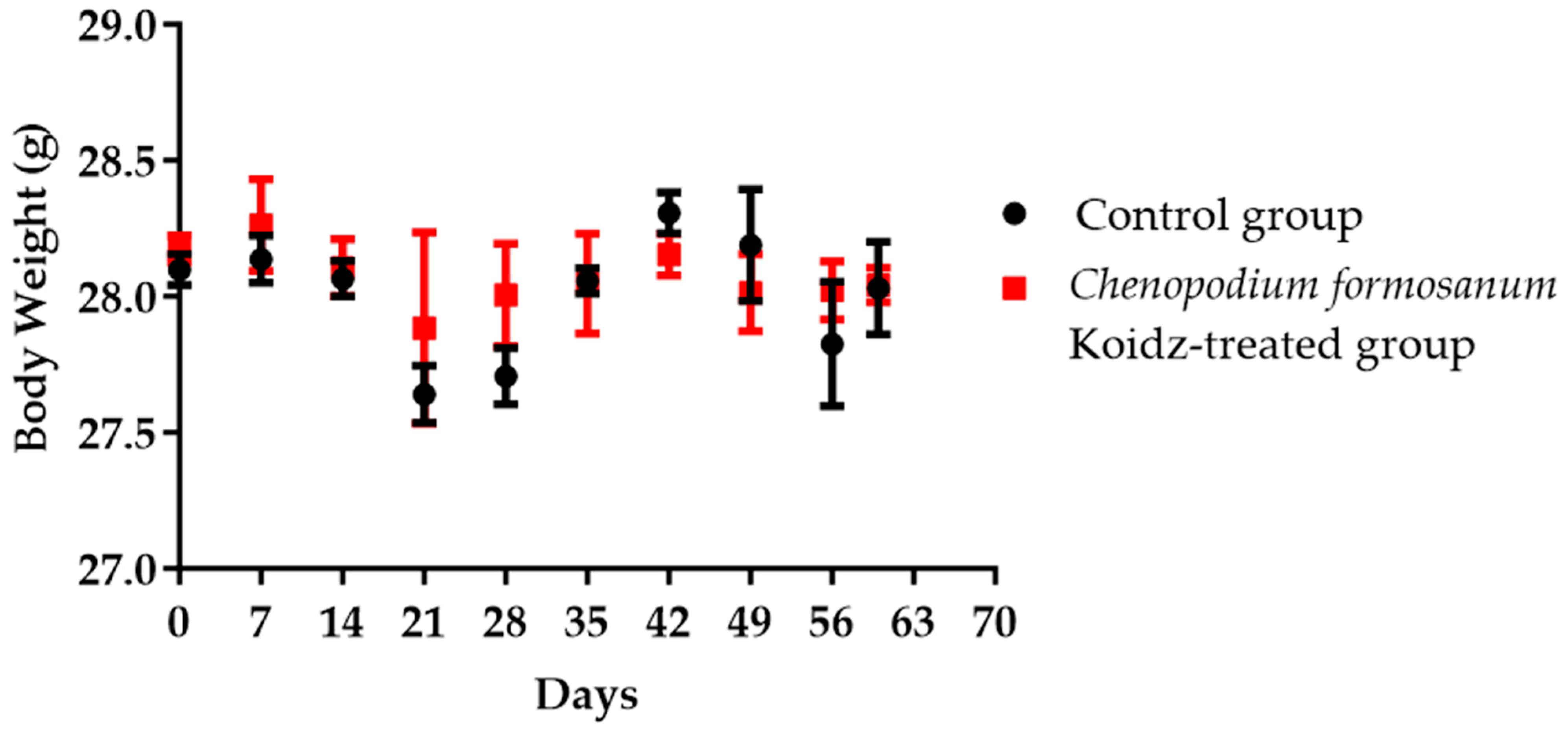
3.1. Body Weight of Aged Mice
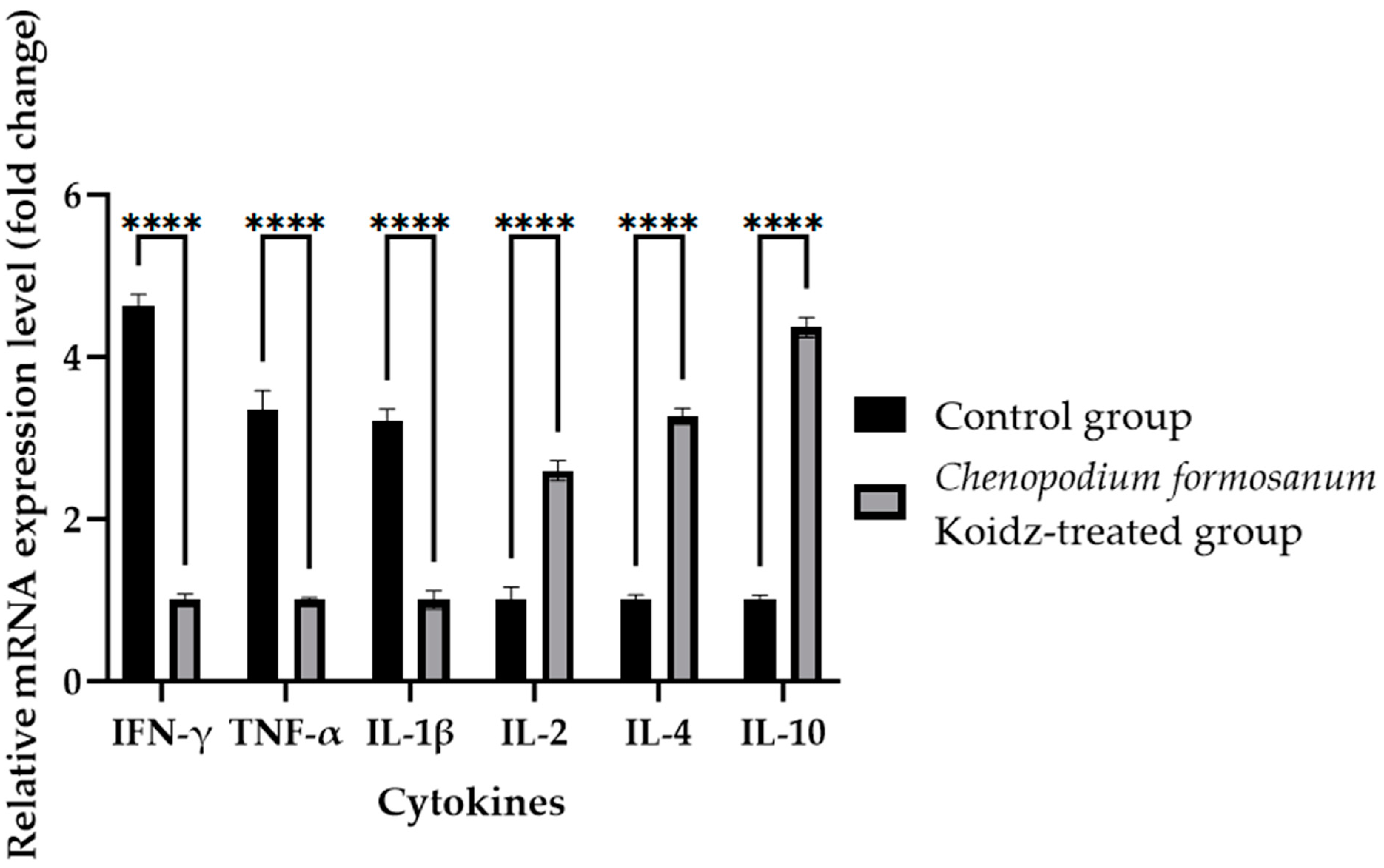
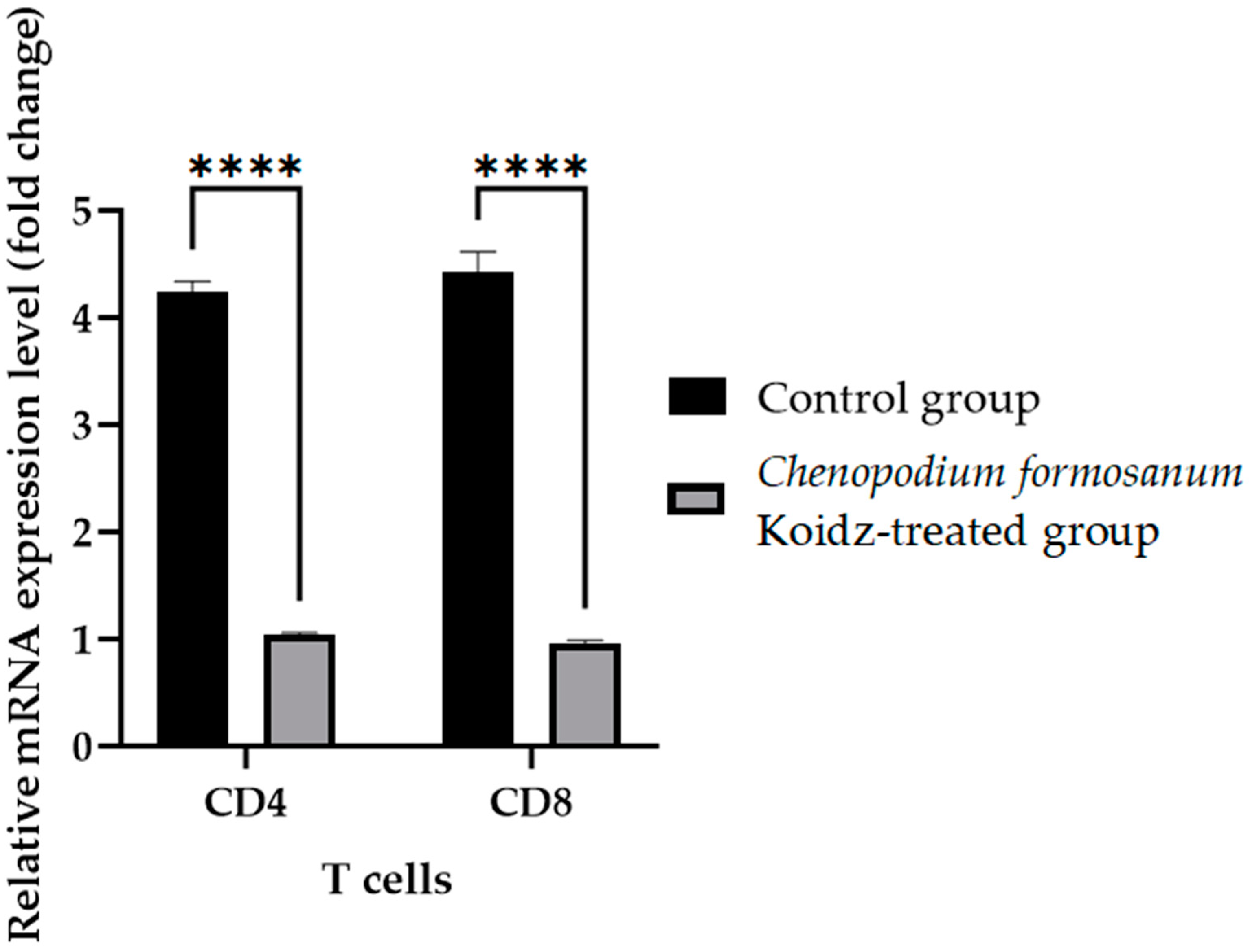
3.2. Cytokines and T Cell mRNA Levels in the Spleen after C. formosanum Treatment
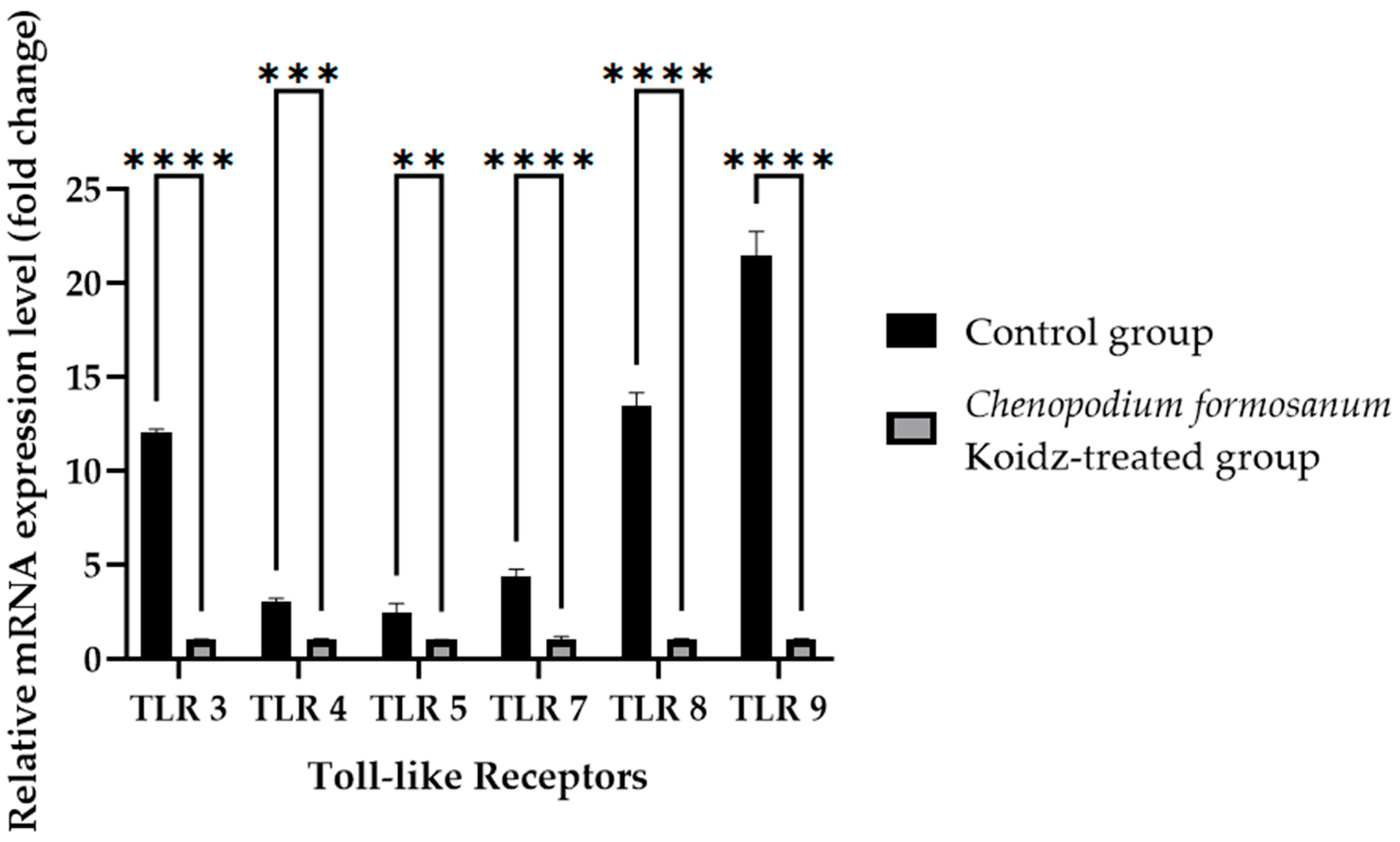
3.3. Toll-like Receptor mRNA Levels in the Spleen after C. formosanum Treatment
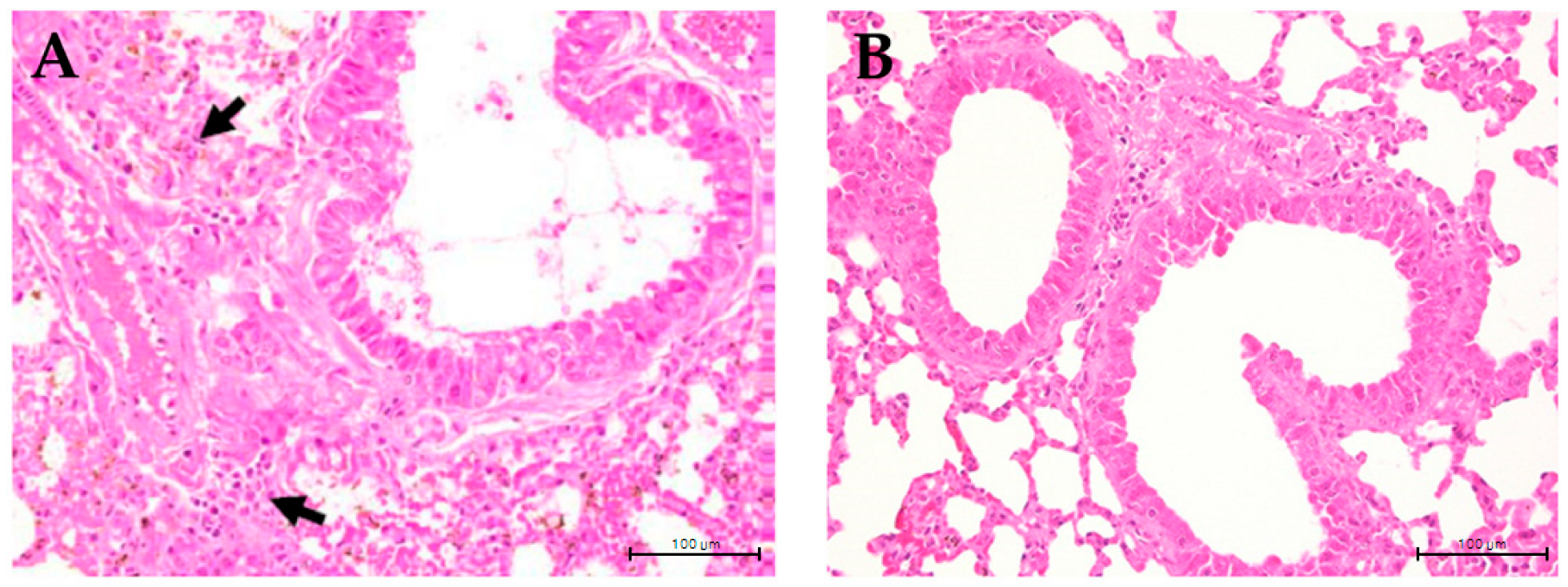
3.4. C. formosanum Treatment Reduced Hyperplasia of the Bronchial Epithelium
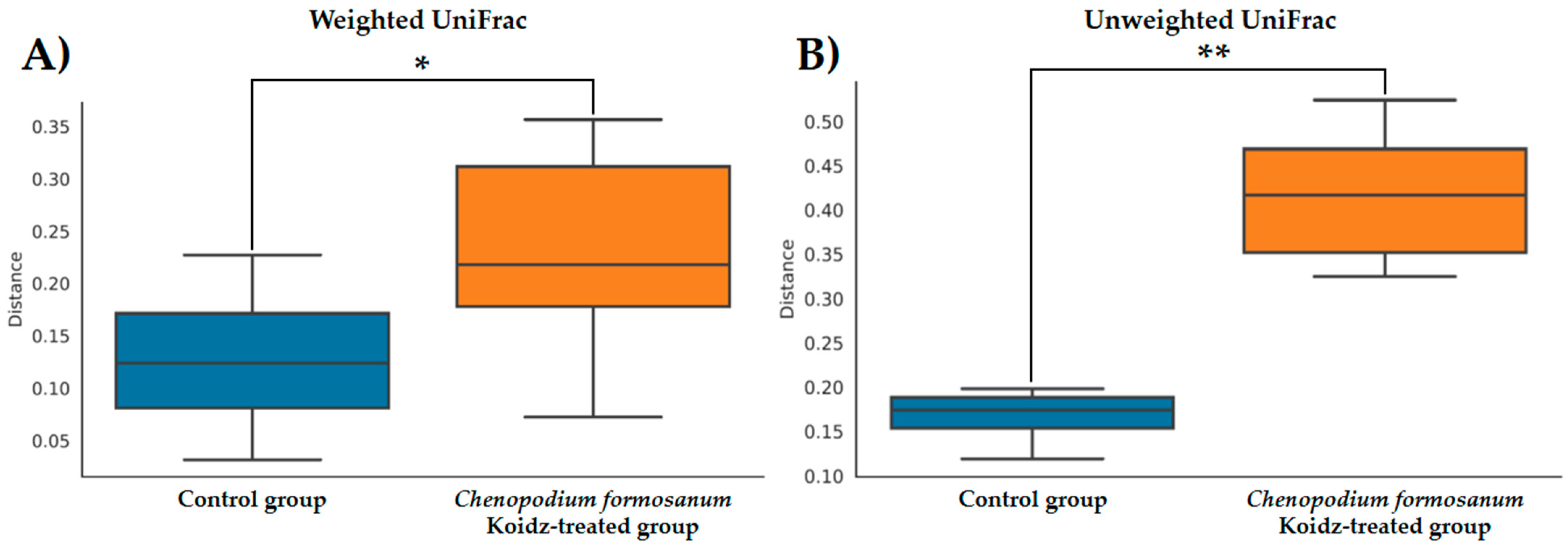
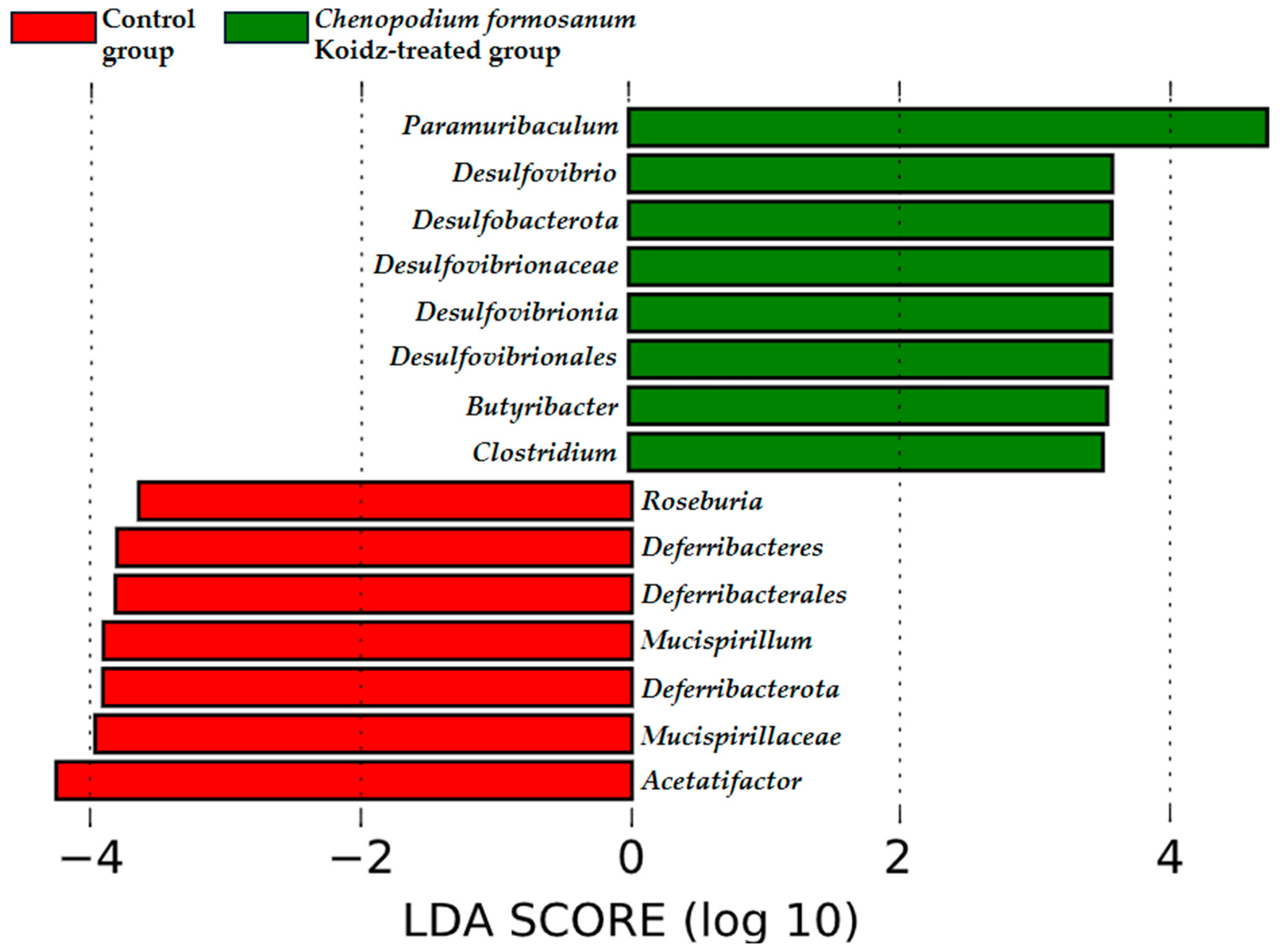
3.5. Administration of C. formosanum Enhanced Microbiota in Aged Mice
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oishi, Y.; Manabe, I. Macrophages in age-related chronic inflammatory diseases. NPJ Aging Mech. Dis. 2016, 2, 1–8. [Google Scholar] [CrossRef]
- Aokage, T.; Iketani, M.; Seya, M.; Meng, Y.; Ageta, K.; Naito, H.; Nakao, A.; Ohsawa, I. Attenuation of pulmonary damage in aged lipopolysaccharide-induced inflammation mice through continuous 2% hydrogen gas inhalation: A potential therapeutic strategy for geriatric inflammation and survival. Exp. Gerontol. 2023, 180, 112270. [Google Scholar] [CrossRef]
- Perret, J.L.; Wurzel, D.; Haydn Walters, E.; Lowe, A.J.; Lodge, C.J.; Bui, D.S.; Erbas, B.; Bowatte, G.; Russel, M.A.; Thompson, B.R.; et al. Childhood bronchitis’ and respiratory outcomes in middle-age: A prospective cohort study from age 7 to 53 years. BMJ Open Respir. Res. 2022, 9, e001212. [Google Scholar] [CrossRef]
- Canan, C.H.; Gokhale, N.S.; Carruthers, B.; Lafuse, W.P.; Schlesinger, L.S.; Torrelles, J.B.; Turner, J. Characterization of lung inflammation and its impact on macrophage function in aging. J. Leukoc. Biol. 2014, 96, 473–480. [Google Scholar] [CrossRef]
- Haynes, L.; Eaton, S.M.; Burns, E.M.; Rincon, M.; Swain, S.L. Inflammatory Cytokines Overcome Age-Related Defects in CD4 T Cell Responses In Vivo. J. Immunol. 2004, 172, 5194–5199. [Google Scholar] [CrossRef]
- Rea, I.M.; Gibson, D.S.; McGilligan, V.; McNerlan, S.E.; Denis Alexander, H.; Ross, O.A. Age and age-related diseases: Role of inflammation triggers and cytokines. Front. Immunol. 2018, 9, 586. [Google Scholar] [CrossRef]
- Nobs, S.P.; Kopf, M. Tissue-resident macrophages: Guardians of organ homeostasis. Trends Immunol. 2021, 42, 495–507. [Google Scholar] [CrossRef]
- Lowery, E.M.; Brubaker, A.L.; Kuhlmann, E.; Kovacs, E.J. The aging lung. Clin. Interv. Aging 2013, 8, 1489–1496. [Google Scholar] [CrossRef]
- Schneider, J.L.; Rowe, J.H.; Garcia-de-Alba, C.; Kim, C.F.; Sharpe, A.H.; Haigis, M.C. The aging lung: Physiology, disease, and immunity. Cell 2021, 184, 1990–2019. [Google Scholar] [CrossRef]
- Meyer, K.C.; Rosenthal, N.S.; Soergel, P.; Peterson, K. Neutrophils and low-grade inflammation in the seemingly normal aging human lung. Mech. Ageing Dev. 1998, 104, 169–181. [Google Scholar] [CrossRef]
- Salehi, S.; Abedi, A.; Balakrishnan, S.; Gholamrezanezhad, A. Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. Am. J. Roentgenol. 2020, 215, 87–93. [Google Scholar] [CrossRef]
- Sherwani, S.; Khan, M.W.A. Cytokine response in SARS-CoV-2 infection in the Elderly. J. Inflamm. Res. 2020, 13, 737–747. [Google Scholar] [CrossRef]
- Pickard, J.M.; Zeng, M.Y.; Caruso, R.; Núñez, G. Gut microbiota: Role in pathogen colonization, immune responses, and inflammatory disease. Immunol. Rev. 2017, 279, 70–89. [Google Scholar] [CrossRef]
- West, C.E.; Jenmalm, M.C.; Prescott, S.L. The gut microbiota and its role in the development of allergic disease: A wider perspective. Clin. Exp. Allergy 2015, 45, 43–53. [Google Scholar] [CrossRef]
- McMahan, R.H.; Hulsebus, H.J.; Najarro, K.M.; Giesy, L.E.; Frank, D.N.; Kovacs, E.J. Changes in gut microbiome correlate with intestinal barrier dysfunction and inflammation following a 3-day ethanol exposure in aged mice. Alcohol 2023, 107, 136–143. [Google Scholar] [CrossRef]
- Tulic, M.K.; Piche, T.; Verhasselt, V. Lung–gut cross-talk: Evidence, mechanisms and implications for the mucosal inflammatory diseases. Clin. Exp. Allergy 2016, 46, 519–528. [Google Scholar] [CrossRef]
- Zhang, D.; Li, S.; Wang, N.; Tan, H.Y.; Zhang, Z.; Feng, Y. The Cross-Talk between Gut Microbiota and Lungs in Common Lung Diseases. Front. Microbiol. 2020, 11, 301. [Google Scholar] [CrossRef]
- Chunxi, L.; Haiyue, L.; Yanxia, L.; Jianbing, P.; Jin, S. The Gut Microbiota and Respiratory Diseases: New Evidence. J. Immunol. Res. 2020, 2020, 2340670. [Google Scholar] [CrossRef]
- Trivedi, R.; Barve, K. Gut microbiome a promising target for management of respiratory diseases. Biochem. J. 2020, 477, 2679–2696. [Google Scholar] [CrossRef]
- Frati, F.; Salvatori, C.; Incorvaia, C.; Bellucci, A.; Di Cara, G.; Marcucci, F.; Esposito, S. The role of the microbiome in asthma: The gut–lung axis. Int. J. Mol. Sci. 2019, 20, 123. [Google Scholar] [CrossRef]
- Barcik, W.; Boutin, R.C.T.; Sokolowska, M.; Finlay, B.B. The Role of Lung and Gut Microbiota in the Pathology of Asthma. Immunity 2020, 52, 241–255. [Google Scholar] [CrossRef]
- Corrêa, R.O.; Castro, P.R.; Moser, R.; Ferreira, C.M.; Quesniaux, V.F.J.; Vinolo, M.A.R.; Ryffel, B. Butyrate: Connecting the gut-lung axis to the management of pulmonary disorders. Front. Nutr. 2022, 9, 1011732. [Google Scholar] [CrossRef]
- Saint-Criq, V.; Lugo-Villarino, G.; Thomas, M. Dysbiosis, malnutrition and enhanced gut-lung axis contribute to age-related respiratory diseases. Ageing Res. Rev. 2021, 66, 101235. [Google Scholar] [CrossRef]
- Dumas, A.; Bernard, L.; Poquet, Y.; Lugo-Villarino, G.; Neyrolles, O. The role of the lung microbiota and the gut–lung axis in respiratory infectious diseases. Cell. Microbiol. 2018, 20, e12966. [Google Scholar] [CrossRef]
- Eladham, M.W.; Selvakumar, B.; Saheb Sharif-Askari, N.; Saheb Sharif-Askari, F.; Ibrahim, S.M.; Halwani, R. Unraveling the gut-Lung axis: Exploring complex mechanisms in disease interplay. Heliyon 2024, 10, e24032. [Google Scholar] [CrossRef]
- Fang, H.; Feng, X.; Xu, T.; Zhong, R.; Lu, D.; Zhang, H.; Shen, W.; Zhao, Y.; Wang, J. Gut-Spleen Axis: Microbiota via Vascular and Immune Pathways Improve Busulfan-Induced Spleen Disruption. MSphere 2023, 8, e00581-22. [Google Scholar] [CrossRef]
- Jarvis, D.E.; Sproul, J.S.; Navarro-Domínguez, B.; Krak, K.; Jaggi, K.; Huang, Y.F.; Lin, T.C.; Jellen, E.N.; Maughan, P.J. Chromosome-Scale Genome Assembly of the Hexaploid Taiwanese Goosefoot “Djulis” (Chenopodium formosanum). Genome Biol. Evol. 2022, 14, evac120. [Google Scholar] [CrossRef]
- Ker, Y.B.; Wu, H.L.; Chen, K.C.; Peng, R.Y. Nutrient composition of Chenopodium formosanum Koidz. bran: Fractionation and bioactivity of its soluble active polysaccharides. PeerJ 2022, 10, e13459. [Google Scholar] [CrossRef]
- Wu, C.T.; Wang, W.H.; Lin, W.S.; Hu, S.Y.; Chen, C.Y.; Chang, M.Y.; Lin, Y.S.; Li, C.P. Effects of different Chenopodium formosanum parts on antioxidant capacity and optimal extraction analysis by Taguchi method. Materials 2021, 14, 4679. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-W.; Chen, H.-J.; Xie, G.-R.; Shih, C.-K. Djulis (Chenopodium formosanum) Prevents Colon Carcinogenesis via Regulating Antioxidative and Apoptotic Pathways in Rats. Nutrients 2019, 11, 2168. [Google Scholar] [CrossRef]
- Złotek, U.; Gawlik-Dziki, U.; Dziki, D.; Awieca, M.; Nowak, R.; Martinez, E. Influence of Drying Temperature on Phenolic Acids Composition and Antioxidant Activity of Sprouts and Leaves of White and Red Quinoa. J. Chem. 2019, 2019, 7125169. [Google Scholar] [CrossRef]
- Liu, M.; Zhu, K.; Yao, Y.; Chen, Y.; Guo, H.; Ren, G.; Yang, X.; Li, J. Antioxidant, anti-inflammatory, and antitumor activities of phenolic compounds from white, red, and black Chenopodium quinoa seed. Cereal Chem. 2020, 97, 703–713. [Google Scholar] [CrossRef]
- Lin, Y.K.; Chung, Y.M.; Lin, Y.H.; Lin, Y.H.; Hu, W.C.; Chiang, C.F. Health functional properties of unhulled red djulis (Chenopodium formosanum) in anti-aging. Int. J. Food Prop. 2021, 24, 833–844. [Google Scholar] [CrossRef]
- Huang, H.W.; Cheng, M.C.; Chen, B.Y.; Wang, C.Y. Effects of high pressure extraction on the extraction yield, phenolic compounds, antioxidant and anti-tyrosinase activity of Djulis hull. J. Food Sci. Technol. 2019, 56, 4016–4024. [Google Scholar] [CrossRef]
- Tung, Y.T.; Zeng, J.L.; Ho, S.T.; Xu, J.W.; Li, S.; Wu, J.H. Anti-nafld effect of djulis hull and its major compound, rutin, in mice with high-fat diet (Hfd)-induced obesity. Antioxidants 2021, 10, 1694. [Google Scholar] [CrossRef]
- Huang, Y.C.; Tung, C.L.; Ho, S.T.; Li, W.S.; Li, S.; Tung, Y.T.; Wu, J.H. Nutraceutical Potential of Djulis (Chenopodium formosanum) Hull: Phytochemicals, Antioxidant Activity, and Liver Protection. Antioxidants 2024, 13, 721. [Google Scholar] [CrossRef]
- Lin, M.; Han, P.; Li, Y.; Wang, W.; Lai, D.; Zhou, L. Quinoa secondary metabolites and their biological activities or functions. Molecules 2019, 24, 2512. [Google Scholar] [CrossRef]
- Souza, S.P.; Roos, A.A.; Gindri, A.L.; Domingues, V.O.; Ascari, J.; Guerra, G.P. Neuroprotective effect of red quinoa seeds extract on scopolamine-induced declarative memory deficits in mice: The role of acetylcholinesterase and oxidative stress. J. Funct. Foods 2020, 69, 103958. [Google Scholar] [CrossRef]
- Tung, Y.T.; Zeng, J.L.; Ho, S.T.; Xu, J.W.; Lin, I.H.; Wu, J.H. Djulis hull improves insulin resistance and modulates the gut microbiota in high-fat diet (Hfd)-induced hyperglycaemia. Antioxidants 2022, 11, 45. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.T.; Lu, W.C.; Chan, Y.J.; Huang, P.H.; Chiang, P.Y.; Chen, R.S.; Li, P.H. Effect of extruded djulis (Chenopodium formosanum) snacks on the ameliorative potential against diabetic cardiomyopathy. J. Funct. Foods 2024, 116, 106154. [Google Scholar] [CrossRef]
- Lee, C.W.; Chen, H.J.; Chien, Y.H.; Hsia, S.M.; Chen, J.H.; Shih, C.K. Synbiotic combination of djulis (Chenopodium formosanum) and lactobacillus acidophilus inhibits colon carcinogenesis in rats. Nutrients 2020, 12, 103. [Google Scholar] [CrossRef]
- Chu, C.C.; Chen, S.Y.; Chyau, C.C.; Fu, Z.H.; Liu, C.C.; Duh, P.D. Protective effect of Djulis (Chenopodium formosanum) and its bioactive compounds against carbon tetrachloride-induced liver injury, in vivo. J. Funct. Foods 2016, 26, 585–597. [Google Scholar] [CrossRef]
- Chyau, C.C.; Chu, C.C.; Chen, S.Y.; Duh, P.D. Djulis (Chenopodiun formosaneum) and its bioactive compounds protect against oxidative stress in human HepG2 cells. J. Funct. Foods 2015, 18, 159–170. [Google Scholar] [CrossRef]
- Isnain, F.S.; Liao, N.-C.; Tsai, H.-Y.; Hsu, J.-L.; Tsai, P.-J.; Wardani, A.K.; Chen, Y.K. Protective Effect of Ethanolic Extract of Djulis Hull on Indomethacin-Induced Gastric Injury. Appl. Sci. 2023, 13, 594. [Google Scholar] [CrossRef]
- Chen, S.Y.; Chu, C.C.; Chyau, C.C.; Yang, J.W.; Duh, P.D. Djulis (Chenopodium formosanum) and its bioactive compounds affect vasodilation, angiotensin converting enzyme activity, and hypertension. Food Biosci. 2019, 32, 100469. [Google Scholar] [CrossRef]
- Hou, C.Y.; Hsieh, C.C.; Huang, Y.C.; Kuo, C.H.; Chen, M.H.; Hsieh, C.W.; Cheng, K.C. Development of Functional Fermented Dairy Products Containing Taiwan Djulis (Chenopodium formosanum Koidz.) in Regulating Glucose Utilization. Fermentation 2022, 8, 423. [Google Scholar] [CrossRef]
- Chyau, C.C.; Chu, C.C.; Chen, S.Y.; Duh, P.D. The inhibitory effects of Djulis (Chenopodium formosanum) and its bioactive compounds on adipogenesis in 3T3-L1 adipocytes. Molecules 2018, 23, 1780. [Google Scholar] [CrossRef]
- Hong, Y.H.; Huang, Y.L.; Liu, Y.C.; Tsai, P.J. Djulis (Chenopodium formosanum Koidz.) Water Extract and Its Bioactive Components Ameliorate Dermal Damage in UVB-Irradiated Skin Models. BioMed Res. Int. 2016, 2016, 7368797. [Google Scholar] [CrossRef]
- Zhang, Q.; Xing, B.; Sun, M.; Zhou, B.; Ren, G.; Qin, P. Changes in bio-accessibility, polyphenol profile and antioxidants of quinoa and djulis sprouts during in vitro simulated gastrointestinal digestion. Food Sci. Nutr. 2020, 8, 4232–4241. [Google Scholar] [CrossRef]
- Li, P.H.; Chan, Y.J.; Hou, Y.W.; Lu, W.C.; Chen, W.H.; Tseng, J.Y.; Mulio, A.T. Functionality of djulis (Chenopodium formosanum) by-products and in vivo anti-diabetes effect in type 2 diabetes mellitus patients. Biology 2021, 10, 160. [Google Scholar] [CrossRef]
- Lyu, J.L.; Liu, Y.J.; Wen, K.C.; Chiu, C.Y.; Lin, Y.H.; Chiang, H.M. Protective Effect of Djulis (Chenopodium formosanum) Extract against UV-and AGEs-Induced Skin Aging via Alleviating Oxidative Stress and Collagen Degradation. Molecules 2022, 27, 2332. [Google Scholar] [CrossRef]
- Chu, C.C.; Chen, S.Y.; Chyau, C.C.; Wang, S.C.; Chu, H.L.; Duh, P.D. Djulis (Chenopodium formosanum) and Its Bioactive Compounds Protect Human Lung Epithelial A549 Cells from Oxidative Injury Induced by Particulate Matter via Nrf2 Signaling Pathway. Molecules 2022, 27, 253. [Google Scholar] [CrossRef]
- Lin, T.A.; Ke, B.J.; Cheng, S.C.; Lee, C.L. Red quinoa bran extract prevented alcoholic fatty liver disease via increasing antioxidative system and repressing fatty acid synthesis factors in mice fed alcohol liquid diet. Molecules 2021, 26, 6973. [Google Scholar] [CrossRef]
- Lin, T.A.; Ke, B.J.; Cheng, C.S.; Wang, J.J.; Wei, B.L.; Lee, C.L. Red quinoa bran extracts protects against carbon tetrachloride-induced liver injury and fibrosis in mice via activation of antioxidative enzyme systems and blocking TGF-β1 pathway. Nutrients 2019, 11, 395. [Google Scholar] [CrossRef]
- Hsieh, C.C.; Yu, S.H.; Kuo, H.C.; Cheng, K.W.; Hsu, C.C.; Lin, Y.P.; Angkawijaya, A.E.; Cheng, K.-C. Alleviation of PM2.5-induced alveolar macrophage inflammation using extract of fermented Chenopodium formosanum Koidz sprouts via regulation of NF-κB pathway. J. Ethnopharmacol. 2024, 318, 116980. [Google Scholar] [CrossRef]
- Shackelford, C.; Long, G.; Wolf, J.; Okerberg, C.; Herbert, R. Quantitative Toxicologic Pathology Qualitative and Quantitative Analysis of Nonneoplastic Lesions in Toxicology Studies. Toxicol. Pathol. 2002, 30, 93–96. [Google Scholar] [CrossRef]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H. Author Correction: Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 2019, 37, 1091. [Google Scholar] [CrossRef]
- Bokulich, N.A.; Subramanian, S.; Faith, J.J.; Gevers, D.; Gordon, J.I.; Knight, R.; Mills, D.A.; Caporaso, J.G. Quality-filtering vastly improves diversity estimates from Illumina amplicon sequencing. Nat. Methods 2013, 10, 57–59. [Google Scholar] [CrossRef]
- Lozupone, C.; Knight, R. UniFrac: A new phylogenetic method for comparing microbial communities. Appl. Environ. Microbiol. 2005, 71, 8228–8235. [Google Scholar] [CrossRef]
- Kawai, T.; Ikegawa, M.; Ori, D.; Akira, S. Decoding Toll-like receptors: Recent insights and perspectives in innate immunity. Immunity 2024, 57, 649–673. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, H.; Lee, J.H.; Hwangbo, C. Toll-like receptor 4 (TLR4): New insight immune and aging. Immun. Ageing 2023, 20, 67. [Google Scholar] [CrossRef] [PubMed]
- Duan, T.; Du, Y.; Xing, C.; Wang, H.Y.; Wang, R.F. Toll-Like Receptor Signaling and Its Role in Cell-Mediated Immunity. Front. Immunol. 2022, 13, 812774. [Google Scholar] [CrossRef] [PubMed]
- Sameer, A.S.; Nissar, S. Toll-Like Receptors (TLRs): Structure, Functions, Signaling, and Role of Their Polymorphisms in Colorectal Cancer Susceptibility. BioMed Res. Int. 2021, 2021, 1157023. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, W.; Blankenhaus, B.; Brunn, M.L.; Meiners, J.; Breloer, M. Elucidating different pattern of immunoregulation in BALB/c and C57BL/6 mice and their F1 progeny. Sci. Rep. 2021, 11, 1536. [Google Scholar] [CrossRef]
- Tillgren, S.M.; Nieto-Fontarigo, J.J.; Cerps, S.; Ramu, S.; Menzel, M.; Mahmutovic Persson, I.; Meissner, A.; Akbarshahi, H.; Uller, L. C57Bl/6N mice have an attenuated lung inflammatory response to dsRNA compared to C57Bl/6J and BALB/c mice. J. Inflamm. 2023, 20, 6. [Google Scholar] [CrossRef]
- Harris, D.; Garrett, K.; Uppuganti, S.; Creecy, A.; Nyman, J.S. The BALB/c mouse as a preclinical model of the age-related deterioration in the lumbar vertebra. Bone 2020, 137, 115438. [Google Scholar] [CrossRef]
- Roberts, A.; Paddock, C.; Vogel, L.; Butler, E.; Zaki, S.; Subbarao, K. Aged BALB/c Mice as a Model for Increased Severity of Severe Acute Respiratory Syndrome in Elderly Humans. J. Virol. 2005, 79, 5833–5838. [Google Scholar] [CrossRef]
- Tang, Y.; Li, X.; Zhang, B.; Chen, P.X.; Liu, R.; Tsao, R. Characterisation of phenolics, betanins and antioxidant activities in seeds of three Chenopodium quinoa Willd. genotypes. Food Chem. 2015, 166, 380–388. [Google Scholar] [CrossRef]
- Hu, Y.; Zhang, J.; Zou, L.; Fu, C.; Li, P.; Zhao, G. Chemical characterization, antioxidant, immune-regulating and anticancer activities of a novel bioactive polysaccharide from Chenopodium quinoa seeds. Int. J. Biol. Macromol. 2017, 99, 622–629. [Google Scholar] [CrossRef]
- Song, C.; Lv, W.; Li, Y.; Nie, P.; Lu, J.; Geng, Y.; Heng, Z. Alleviating the effect of quinoa and the underlying mechanism on hepatic steatosis in high-fat diet-fed rats. Nutr. Metab. 2021, 18, 106. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, Y.; Qiu, B.; Fan, S.; Ding, H.; Liu, Z. Quinoa whole grain diet compromises the changes of gut microbiota and colonic colitis induced by dextran Sulfate sodium in C57BL/6 mice. Sci. Rep. 2018, 8, 14916. [Google Scholar] [CrossRef] [PubMed]
- Paśko, P.; Bartoń, H.; Zagrodzki, P.; Gorinstein, S.; Fołta, M.; Zachwieja, Z. Anthocyanins, total polyphenols and antioxidant activity in amaranth and quinoa seeds and sprouts during their growth. Food Chem. 2009, 115, 994–998. [Google Scholar] [CrossRef]
- Zhou, Z.Y.; Deng, Y.; Wen, Y.L.; Cheng, Y.Q.; Li, K.X.; Chen, H.P. Chronic low-grade inflammation is involved in TLR4 knockout-induced spontaneous obesity in aged mice. Biomed. Pharmacother. 2022, 147, 112637. [Google Scholar] [CrossRef]
- Baumann, A.; Hernández-Arriaga, A.; Brandt, A.; Sánchez, V.; Nier, A.; Jung, F.; Kehm, R.; Hohn, A.; Grune, T.; Frahm, C.; et al. Microbiota profiling in aging-associated inflammation and liver degeneration. Int. J. Med. Microbiol. 2021, 311, 151500. [Google Scholar] [CrossRef] [PubMed]
- Buford, T.W. (Dis)trust your gut: The gut microbiome in age-related inflammation, health, and disease. Microbiome 2017, 5, 80. [Google Scholar] [CrossRef]
- Price, C.E.; O’Toole, G.A. The gut-lung axis in cystic Fibrosis. J. Bacteriol. 2021, 203, 10–1128. [Google Scholar] [CrossRef]
- Xu, X.; Li, G.; Zhang, D.; Zhu, H.; Liu, G.H.; Zhang, Z. Gut Microbiota is Associated with Aging-Related Processes of a Small Mammal Species under High-Density Crowding Stress. Adv. Sci. 2023, 10, 2205346. [Google Scholar] [CrossRef]
- Bander, Z.A.; Nitert, M.D.; Mousa, A.; Naderpoor, N. The gut microbiota and inflammation: An overview. Int. J. Environ. Res. Public. Health 2020, 17, 7618. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Yang, X.; Chatterjee, V.; Wu, M.H.; Yuan, S.Y. The gut–lung axis in systemic inflammation role of mesenteric lymph as a conduit. Am. J. Respir. Cell Mol. Biol. 2021, 64, 19–28. [Google Scholar] [CrossRef]
- Hakansson, A.; Molin, G. Gut microbiota and inflammation. Nutrients 2011, 3, 637–687. [Google Scholar] [CrossRef]
- Madan, J.C.; Koestle, D.C.; Stanton, B.A.; Davidson, L.; Moulton, L.A.; Housman, M.L.; Moore, J.H.; Guill, M.F.; Morrison, H.G.; Sogin, M.L.; et al. Serial analysis of the gut and respiratory microbiome in cystic fibrosis in infancy: Interaction between intestinal and respiratory tracts and impact of nutritional exposures. mBio 2012, 3, 10-1128. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.S.; Prause, M.; Williams, K.; Barrès, R.; Billestrup, N. Butyrate inhibits IL-1β-induced inflammatory gene expression by suppression of NF-κB activity in pancreatic beta cells. J. Biol. Chem. 2022, 298, 102312. [Google Scholar] [CrossRef] [PubMed]
- Cleophas, M.C.P.; Ratter, J.M.; Bekkering, S.; Quintin, J.; Schraa, K.; Stroes, E.S.; Netea, M.G.; Joosten, L.A.B. Effects of oral butyrate supplementation on inflammatory potential of circulating peripheral blood mononuclear cells in healthy and obese males. Sci. Rep. 2019, 9, 775. [Google Scholar] [CrossRef] [PubMed]
- Säemann, M.D.; Böhmig, G.A.; Österreicher, C.H.; Burtscher, H.; Parolini, O.; Diakos, C.; Stockl, J.; Horl, W.H.; Zlabinger, G.J. Anti-inflammatory effects of sodium butyrate on human monocytes: Potent inhibition of IL-12 and up-regulation of IL-10 production. FASEB J. 2000, 14, 2380–2382. [Google Scholar] [CrossRef]
- Fukae, J.; Amasaki, Y.; Yamashita, Y.; Bohgaki, T.; Yasuda, S.; Jodo, S.; Atsumi, T.; Koike, T. Butyrate suppresses tumor necrosis factor α production by regulating specific messenger RNA degradation mediated through a cis-acting AU-rich element. Arthritis Rheum. 2005, 52, 2697–2707. [Google Scholar] [CrossRef]
- Singh, V.; Lee, G.D.; Son, H.W.; Koh, H.; Kim, E.S.; Unno, T.; Shin, J.H. Butyrate producers, “The Sentinel of Gut”: Their intestinal significance with and beyond butyrate, and prospective use as microbial therapeutics. Front. Microbiol. 2023, 13, 1103836. [Google Scholar] [CrossRef]
| Name | Type | Length | Primer Sequence | Product Size | Tm | Ref. Sequence |
|---|---|---|---|---|---|---|
| Mouse IL-1β | Forward | 21 | GAAATGCCACCTTTTGACAGTG | 115 bp | 60 °C | NM_008361.4 |
| Reverse | 22 | TGGATGCTCTCATCAGGACAG | ||||
| Mouse IL-2 | Forward | 23 | TGAGCAGGATGGAGAATTACAGG | 119 bp | 60 °C | NM_008366.3 |
| Reverse | 23 | GTCCAAGTTCATCTTCTAGGCAC | ||||
| Mouse IL-4 | Forward | 20 | CCATATCCACGGATGCGACA | 254 bp | 60 °C | NM_021283.2 |
| Reverse | 20 | AAGCCCGAAAGAGTCTCTGC | ||||
| Mouse IL-10 | Forward | 21 | GCTCTTACTGACTGGCATGAG | 104 bp | 60 °C | NM_010548.2 |
| Reverse | 20 | CGCAGCTCTAGGAGCATGTG | ||||
| Mouse IFN-γ | Forward | 20 | ACTGTGATTGCGGGGTTGTA | 198 bp | 60 °C | NM_008337.4 |
| Reverse | 20 | ACATTCGAGTGCTGTCTGGC | ||||
| Mouse TNF-α | Forward | 23 | CCCTCACACTCAGATCATCTTCT | 60 bp | 60 °C | M13049.1 |
| Reverse | 19 | GCTACGACGTGGGCTACAG | ||||
| Mouse CD4 | Forward | 21 | AGGTGATGGGACCTACCTCTC | 102 bp | 60 °C | NM_013488.3 |
| Reverse | 20 | GGGGCCACCACTTGAACTAC | ||||
| Mouse CD8 | Forward | 19 | CCGTTGACCCGCTTTCTGT | 120 bp | 60 °C | NM_009857.1 |
| Reverse | 21 | CGGCGTCCATTTTCTTTGGAA | ||||
| Mouse β-actin | Forward | 20 | GGCTGTATTCCCCTCCATCG | 153 bp | 60 °C | NM_007393.5 |
| Reverse | 22 | CCAGTTGGTAACAATGCCATGT | ||||
| Mouse TLR3 | Forward | 22 | GTGAGATACAACGTAGCTGACTG | 161 bp | 60 °C | AF355152.1 2 |
| Reverse | 23 | TCCTGCATCCAAGATAGCAAGT | ||||
| Mouse TLR4 | Forward | 20 | AGCTCCTGACCTTGGTCTTG | 266 bp | 60 °C | NM_025817.4 |
| Reverse | 20 | CGCAGGGGAACTCAATGAGG | ||||
| Mouse TLR5 | Forward | 21 | GCAGGATCATGGCATGTCAAC | 129 bp | 60 °C | NM_016928.4 |
| Reverse | 21 | ATCTGGGTGAGGTTACAGCCT | ||||
| Mouse TLR7 | Forward | 21 | ATGTGGACACGGAAGAGACAA | 207 bp | 60 °C | AY035889.1 1 |
| Reverse | 22 | GGTAAGGGTAAGATTGGTGGTG | ||||
| Mouse TLR8 | Forward | 21 | GAAAACATGCCCCCTCAGTCA | 110 bp | 60 °C | AY035890.11 |
| Reverse | 23 | CGTCACAAGGATAGCTTCTGGAA | ||||
| Mouse TLR9 | Forward | 21 | ATGGTTCTCCGTCGAAGGACT | 117 bp | 60 °C | AF314224.1 |
| Reverse | 19 | GAGGCTTCAGCTCACAGGG |
| Control Group | Chenopodium formosanum Koidz-Treated Group | ||
|---|---|---|---|
| Aged Mouse | Degree of Lesions | Aged Mouse | Degree of Lesions |
| Control mouse 1 | 3 | Treated mouse 1 | 1 |
| Control mouse 2 | 3 | Treated mouse 2 | 2 |
| Control mouse 3 | 3 | Treated mouse 3 | 1 |
| Control mouse 4 | 2 | Treated mouse 4 | 1 |
| Control mouse 5 | 3 | Treated mouse 5 | 1 |
| Control mouse 6 | 3 | Treated mouse 6 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villanueva, B.H.A.; Huang, H.-Y.; Tyan, Y.-C.; Lin, P.-J.; Li, C.-W.; Minh, H.; Tayo, L.L.; Chuang, K.-P. Immune mRNA Expression and Fecal Microbiome Composition Change Induced by Djulis (Chenopodium formosanum Koidz.) Supplementation in Aged Mice: A Pilot Study. Medicina 2024, 60, 1545. https://doi.org/10.3390/medicina60091545
Villanueva BHA, Huang H-Y, Tyan Y-C, Lin P-J, Li C-W, Minh H, Tayo LL, Chuang K-P. Immune mRNA Expression and Fecal Microbiome Composition Change Induced by Djulis (Chenopodium formosanum Koidz.) Supplementation in Aged Mice: A Pilot Study. Medicina. 2024; 60(9):1545. https://doi.org/10.3390/medicina60091545
Chicago/Turabian StyleVillanueva, Brian Harvey Avanceña, Huai-Ying Huang, Yu-Chang Tyan, Pei-Ju Lin, Chang-Wei Li, Hoang Minh, Lemmuel L. Tayo, and Kuo-Pin Chuang. 2024. "Immune mRNA Expression and Fecal Microbiome Composition Change Induced by Djulis (Chenopodium formosanum Koidz.) Supplementation in Aged Mice: A Pilot Study" Medicina 60, no. 9: 1545. https://doi.org/10.3390/medicina60091545
APA StyleVillanueva, B. H. A., Huang, H.-Y., Tyan, Y.-C., Lin, P.-J., Li, C.-W., Minh, H., Tayo, L. L., & Chuang, K.-P. (2024). Immune mRNA Expression and Fecal Microbiome Composition Change Induced by Djulis (Chenopodium formosanum Koidz.) Supplementation in Aged Mice: A Pilot Study. Medicina, 60(9), 1545. https://doi.org/10.3390/medicina60091545









