Predictors of Chronic Ankle Instability Among Soccer Players
Abstract
1. Introduction
Bottom of Form
2. Materials and Methods
2.1. Study Design and Setting
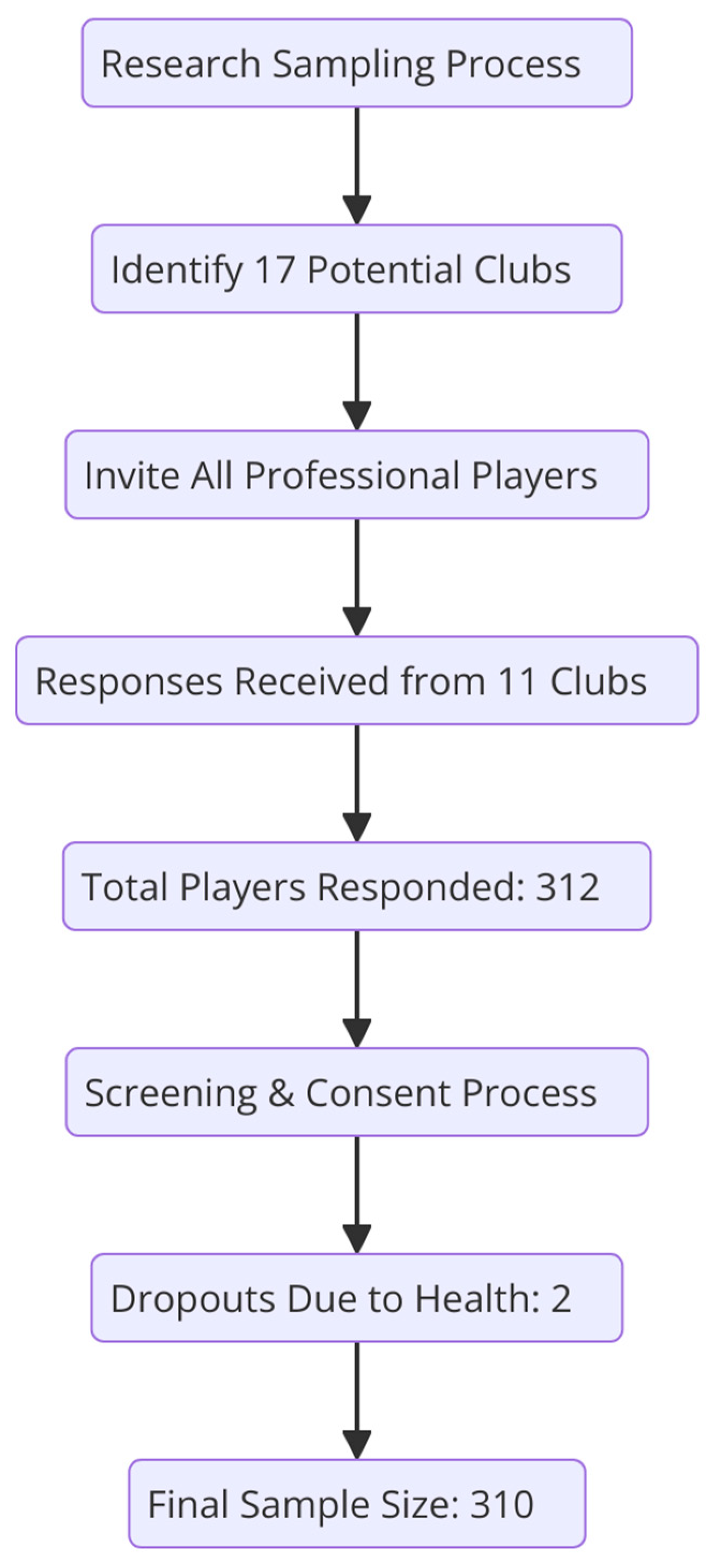
2.2. Participants and Sampling Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Sample Size
2.5. Outcome Variable
2.6. Data Collection and Procedure
2.7. Statistical Section
3. Results
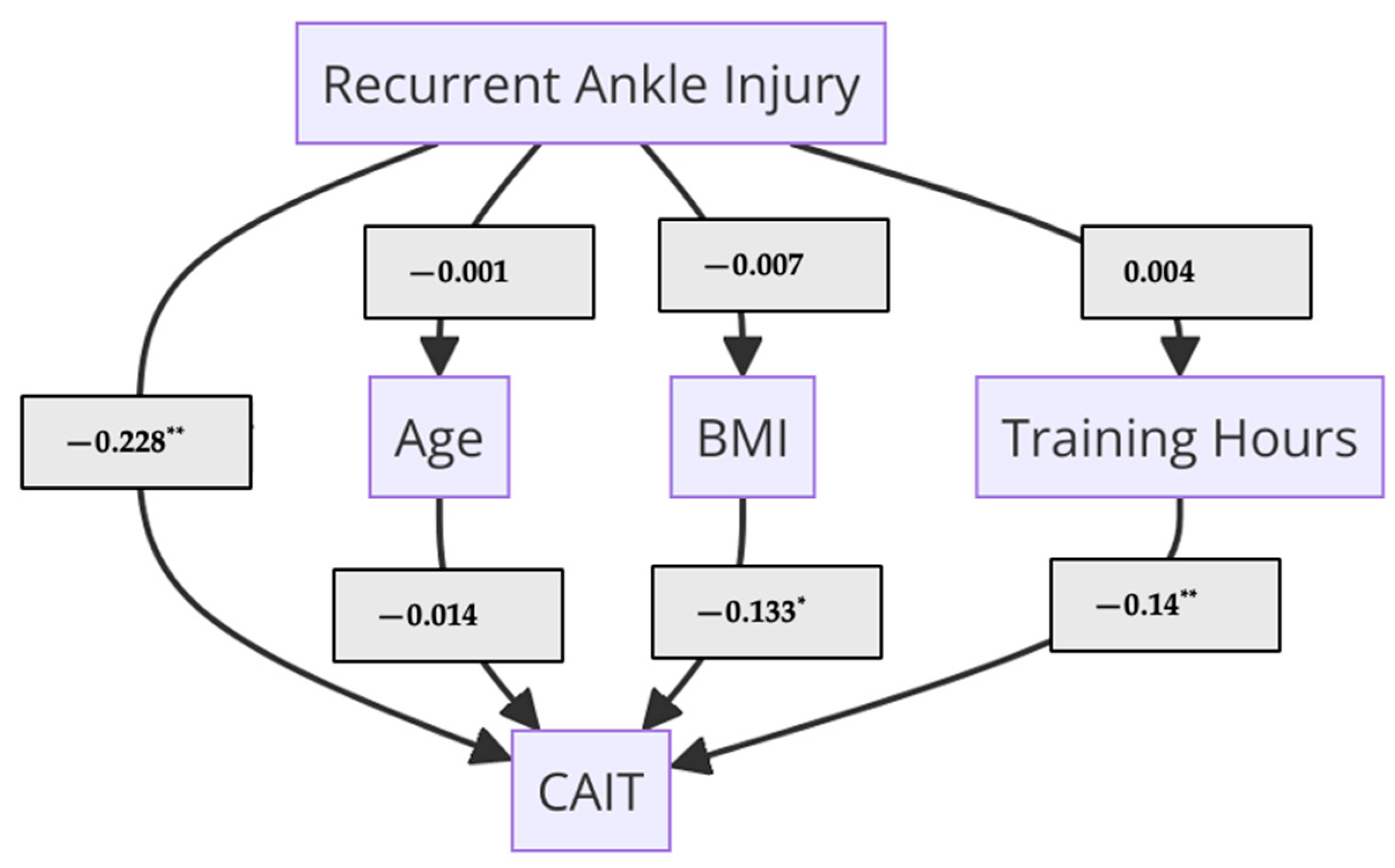
Mediation Analysis
4. Discussion
Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hunt, K.J.; Hurwit, D.; Robell, K.; Gatewood, C.; Botser, I.B.; Matheson, G. Incidence and epidemiology of foot and ankle injuries in elite collegiate athletes. Am. J. Sports Med. 2017, 45, 426–433. [Google Scholar] [PubMed]
- Hertel, J.; Corbett, R.O. An updated model of chronic ankle instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [PubMed]
- Torp, D.; Donovan, L. Chronic foot and ankle injuries. In Foot Ankle Biomechanics; Elsevier: Amsterdam, The Netherlands, 2023; pp. 507–525. [Google Scholar]
- Martin, R.L.; Davenport, T.E.; Fraser, J.J.; Sawdon-Bea, J.; Carcia, C.R.; Carroll, L.A.; Kivlan, B.R.; Carreira, D. Ankle stability and movement coordination impairments: Lateral ankle ligament sprains revision 2021: Clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy association. J. Orthop. Sport Phys. Ther. 2021, 51, CPG1–CPG80. [Google Scholar]
- Donovan, L.; Hetzel, S.; Laufenberg, C.R.; McGuine, T.A. Prevalence and impact of chronic ankle instability in adolescent athletes. Orthop. J. Sport Med. 2020, 8, 2325967119900962. [Google Scholar]
- Subramanian, S.S.; Teng, S.Y.; Senthil, P.; Gaowgeh, R.A.M.; Alfawaz, S.S.; Neamatallah, Z. Correlation between Level of Functional Ability and Sports Performance among Football Players with Chronic Ankle Instability (CAI). J. Pharm. Res. Int. 2021, 33, 415–424. [Google Scholar] [CrossRef]
- Van den Bekerom, M.P.J.; Kerkhoffs, G.M.M.J.; McCollum, G.A.; Calder, J.D.F.; van Dijk, C.N. Management of acute lateral ankle ligament injury in the athlete. Knee Surg. Sport Traumatol. Arthrosc. 2013, 21, 1390–1395. [Google Scholar]
- Al-Mahrouqi, M.M.; Macdonald, D.A.; Vicenzino, B.; Smith, M.D. Physical impairments in adults with ankle osteoarthritis: A systematic review and meta-analysis. J. Orthop. Sport Phys. Ther. 2018, 48, 449–459. [Google Scholar] [CrossRef]
- Abate Daga, F.; Panzolini, M.; Allois, R.; Baseggio, L.; Agostino, S. Age-Related Differences in Hamstring Flexibility in Prepubertal Soccer Players: An Exploratory Cross-Sectional Study. Front. Psychol. 2021, 12, 741756. [Google Scholar]
- Sanz, A.; Pablos, C.; Ballester, R.; Sánchez-Alarcos, J.V.; Huertas, F. Range of motion and injury occurrence in elite spanish soccer academies. Not only a hamstring shortening—Related problem. J. Strength Cond. Res. 2020, 34, 1924–1932. [Google Scholar]
- Lin, J.-Z.; Lin, Y.-A.; Tai, W.-H.; Chen, C.-Y. Influence of landing in neuromuscular control and ground reaction force with ankle instability: A narrative review. Bioengineering 2022, 9, 68. [Google Scholar] [CrossRef]
- Fong, D.T.P.; Chan, Y.-Y.; Mok, K.-M.; Yung, P.S.H.; Chan, K.-M. Understanding acute ankle ligamentous sprain injury in sports. BMC Sports Sci. Med. Rehabil. 2009, 1, 1–14. [Google Scholar]
- Alghadir, A.H.; Iqbal, Z.A.; Iqbal, A.; Ahmed, H.; Ramteke, S.U. Effect of chronic ankle sprain on pain, range of motion, proprioception, and balance among athletes. Int. J. Environ. Res. Public Health 2020, 17, 5318. [Google Scholar] [CrossRef]
- Park, H.S.; Oh, J.K.; Kim, J.Y.; Yoon, J.H. The Effect of Strength and Balance Training on Kinesiophobia, Ankle Instability, Function, and Performance in Elite Adolescent Soccer Players with Functional Ankle Instability: A Prospective Cluster Randomized Controlled Trial. J. Sport Sci. Med. 2024, 23, 593–602. [Google Scholar]
- Yang, Y.; Wu, Y.; Zhu, W. Recent advances in the management of chronic ankle instability. Chin. J. Traumatol. 2025, 28, 35–42. [Google Scholar]
- Zhang, J.; Yang, K.; Wang, C.; Gu, W.; Li, X.; Fu, S.; Song, G.; Wang, J.; Wu, C.; Zhu, H.; et al. Risk factors for chronic ankle instability after first episode of lateral ankle sprain: A retrospective analysis of 362 cases. J. Sport Health Sci. 2023, 12, 606–612. [Google Scholar]
- Cain, M.S.; Ban, R.J.; Chen, Y.-P.; Geil, M.D.; Goerger, B.M.; Linens, S.W. Four-week ankle-rehabilitation programs in adolescent athletes with chronic ankle instability. J. Athl. Train. 2020, 55, 801–810. [Google Scholar]
- Li, C.; Huang, Y.; Wang, G.; Xie, K.; Chen, J.; Ma, J.; Kui, X.; Luo, J.; Zhao, W.; Zhang, Y.; et al. Analysis of the Multi-Dimension Risk Factors Associated with Chronic Ankle Instability: A Retrospective Cohort Study. Res. Sq. 2024. preprint. [Google Scholar] [CrossRef]
- Cottom, J.M.; Graney, C.T.; Sisovsky, C. Evaluation of BMI with an all inside arthroscopic Broström procedure for chronic lateral ankle instability: An analysis of 113 patients. J. Foot Ankle Surg. 2020, 59, 1008–1012. [Google Scholar]
- Lin, C.-I.; Houtenbos, S.; Lu, Y.-H.; Mayer, F.; Wippert, P.-M. The epidemiology of chronic ankle instability with perceived ankle instability-a systematic review. J. Foot Ankle Res. 2021, 14, 41. [Google Scholar]
- Mollà-Casanova, S.; Inglés, M.; Serra-Añó, P. Effects of balance training on functionality, ankle instability, and dynamic balance outcomes in people with chronic ankle instability: Systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 1694–1709. [Google Scholar]
- Soligard, T.; Schwellnus, M.; Alonso, J.-M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R.; et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br. J. Sports Med. 2016, 50, 1030–1041. [Google Scholar] [PubMed]
- Goulart Neto, A.M.; Maffulli, N.; Migliorini, F.; de Menezes, F.S.; Okubo, R. Validation of Foot and Ankle Ability Measure (FAAM) and the Foot and Ankle Outcome Score (FAOS) in individuals with chronic ankle instability: A cross-sectional observational study. J. Orthop. Surg. Res. 2022, 17, 38. [Google Scholar] [PubMed]
- Suttmiller, A.M.B.; McCann, R.S. Injury-related fear in individuals with and without chronic ankle instability: A systematic review. J. Sport Rehabil. 2021, 30, 1203–1212. [Google Scholar] [PubMed]
- Bamber, Z.A.; Wheeler, P.C.; He, X.; Ling, S.K.K.; Yung, P.S.H.; Fong, D.T.P. Screening for laterally deviated plantar pressure during stance using the Cumberland ankle instability tool and anthropometric measures. Res. Sport Med. 2021, 29, 323–335. [Google Scholar]
- Peng, D.; Tang, H.; Mao, M.; Song, Q.; Mao, D.; Wang, J.; Sun, W. Correlations of strength, proprioception, and dynamic balance to the Cumberland Ankle Instability Tool Score among patients with chronic ankle instability: A cross-sectional study. BMC Musculoskelet. Disord. 2024, 25, 970. [Google Scholar]
- Figlioli, F.; Belmonte, G.; Giustino, V.; Canzone, A.; Ferrantello, E.; Gervasi, M.; Fernández-Peña, E.; Battaglia, G.; Bianco, A.; Patti, A. Applicability of the Cumberland Ankle Instability Tool in Elite Volleyball Athletes: A Cross-Sectional Observational Study. Sports 2024, 12, 71. [Google Scholar] [CrossRef]
- Hantal, Ş.; Şaylı, U.; Subaşı, F.; Çil, E.; Koç, E.; Yeral, A.; Akyol, T. Chronic ankle instability and associated factors in the general population: A pilot study. Adv. Rehabil. 2022, 36, 40–46. [Google Scholar]
- Donahue, M.; Simon, J.; Docherty, C.L. Critical review of self-reported functional ankle instability measures. Foot Ankle Int. 2011, 32, 1140–1146. [Google Scholar]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar]
- De Noronha, M.; Refshauge, K.M.; Kilbreath, S.L.; Figueiredo, V.G. Cross-cultural adaptation of the Brazilian-Portuguese version of the Cumberland Ankle Instability Tool (CAIT). Disabil. Rehabil. 2008, 30, 1959–1965. [Google Scholar]
- Hadadi, M.; Ebrahimi Takamjani, I.; Ebrahim Mosavi, M.; Aminian, G.; Fardipour, S.; Abbasi, F. Cross-cultural adaptation, reliability, and validity of the Persian version of the Cumberland Ankle Instability Tool. Disabil. Rehabil. 2017, 39, 1644–1649. [Google Scholar] [CrossRef] [PubMed]
- Korakakis, V.; Abassi, M.; Kotsifak, A.; Manai, H.; AbuEsba, A. Cross-cultural adaptation and psychometric properties’ evaluation of the modern standard Arabic version of Cumberland Ankle Instability Tool (CAIT) in professional athletes. PLoS ONE 2019, 14, e0217987. [Google Scholar] [CrossRef]
- Ko, J.; Rosen, A.B.; Brown, C.N. Cross-cultural adaptation and validation of the Korean version of the Cumberland Ankle Instability Tool. Int. J. Sports Phys. Ther. 2015, 10, 1007. [Google Scholar]
- Kunugi, S.; Masunari, A.; Noh, B.; Mori, T.; Yoshida, N.; Miyakawa, S. Cross-cultural adaptation, reliability, and validity of the Japanese version of the Cumberland ankle instability tool. Disabil. Rehabil. 2017, 39, 50–58. [Google Scholar] [CrossRef]
- Vuurberg, G.; Kluit, L.; van Dijk, C.N. The Cumberland Ankle Instability Tool (CAIT) in the Dutch population with and without complaints of ankle instability. Knee Surg. Sport Traumatol. Arthrosc. 2018, 26, 882–891. [Google Scholar] [CrossRef]
- Tsekoura, M.; Billis, E.; Fousekis, K.; Christakou, A.; Tsepis, E. Cross cultural adaptation, reliability, and validity of the Greek version of the Cumberland Ankle Instability Tool. Physiother. Theory Pract. 2021, 37, 954–962. [Google Scholar] [CrossRef]
- Hui, J.Y.-N.; Tong, A.H.-K.; Chui, V.W.-T.; Fong, D.T.P.; Chau, W.-W.; Yung, P.S.-H.; Ling, S.K.-K. Cross-cultural adaptation, reliability and validity of the Cantonese-Chinese Cumberland Ankle Instability Tool (CAIT-HK). Foot 2023, 56, 102015. [Google Scholar] [CrossRef]
- Rodríguez-Fernández, Á.L.; Rebollo-Roldán, J.; Jiménez-Rejano, J.J.; Güeita-Rodríguez, J. Psychometric properties of the Spanish version of the Cumberland Ankle Instability Tool. Disabil. Rehabil. 2015, 37, 1888–1894. [Google Scholar] [CrossRef]
- Geerinck, A.; Beaudart, C.; Salvan, Q.; Van Beveren, J.; D’Hooghe, P.; Bruyère, O.; Kaux, J.-F. French translation and validation of the Cumberland Ankle Instability Tool, an instrument for measuring functional ankle instability. Foot Ankle Surg. 2020, 26, 391–397. [Google Scholar] [CrossRef]
- Wright, C.J.; Arnold, B.L.; Ross, S.E.; Linens, S.W. Recalibration and validation of the Cumberland Ankle Instability Tool cutoff score for individuals with chronic ankle instability. Arch. Phys. Med. Rehabil. 2014, 95, 1853–1859. [Google Scholar] [CrossRef]
- Kobayashi, T.; Koshino, Y.; Miki, T. Abnormalities of foot and ankle alignment in individuals with chronic ankle instability: A systematic review. BMC Musculoskelet. Disord. 2021, 22, 1–8. [Google Scholar]
- Ching, S.-H.; Chiu, Y.-C.; Liao, Y.-C.; Yang, S.-H.; Tsai, Y.-J. A new mouse model of ankle instability induced by multiple mechanical sprains with controlled inversion angle and speed. Front. Bioeng. Biotechnol. 2022, 10, 927987. [Google Scholar]
- Mendez-Rebolledo, G.; Guzmán-Venegas, R.; Cruz-Montecinos, C.; Watanabe, K.; Calatayud, J.; Martinez-Valdes, E. Individuals with chronic ankle instability show altered regional activation of the peroneus longus muscle during ankle eversion. Scand. J. Med. Sci. Sports 2024, 34, e14535. [Google Scholar] [PubMed]
- Ahmad-Shushami, A.H.; A-Hamid, M.S.; Khair, M.H.; Ali, M.O. Impact of Previous Ankle Injuries on Professional Footballers’ Preseason Functional Ankle Assessment. Malays. Orthop. J. 2023, 17, 73. [Google Scholar]
- Liu, Z.; Yamaguchi, R.; Fu, S.; Zhao, H.; Li, Y.; Kobayashi, Y.; Gong, Y.; Kumai, T. Epidemiology of ankle sprain and chronic ankle instability in elite adolescent dancesport athletes. Phys. Sportsmed. 2024. [Google Scholar] [CrossRef]
- Dolan, P.; Kenny, I.; Glynn, L.; Campbell, M.; Warrington, G.D.; Cahalan, R.; Harrison, A.; Lyons, M.; Comyns, T. Risk factors for acute ankle sprains in field-based, team contact sports: A systematic review of prospective etiological studies. Phys. Sportsmed. 2023, 51, 517–530. [Google Scholar]
- Kawabata, S.; Murata, K.; Iijima, H.; Nakao, K.; Kawabata, R.; Terada, H.; Kojima, T.; Takasu, C.; Kano, T.; Kanemura, N. Ankle instability as a prognostic factor associated with the recurrence of ankle sprain: A systematic review. Foot 2023, 54, 101963. [Google Scholar] [CrossRef]
- Neri, S.G.R.; Harvey, L.A.; Tiedemann, A.; Gadelha, A.B.; Lima, R.M. Obesity and falls in older women: Mediating effects of muscle quality, foot loads and postural control. Gait Posture 2020, 77, 138–143. [Google Scholar]
- Melloni, M.A.S.; San-Martin, J.E.S.; de Oliveira Barbeta, C.J.; Gonçalves, E.M.; Júnior, G.G. Anthropometric and body composition variables as risk factors for musculoskeletal injureis in athletes and military personnel: A systematic review. Rev. Contemp. 2024, 4, e4898. [Google Scholar]
- Kawabata, S.; Ozone, K.; Minegishi, Y.; Oka, Y.; Terada, H.; Takasu, C.; Kojima, T.; Kano, T.; Kanemura, N.; Murata, K. Chronic Ankle Joint Instability Induces Ankle Sensorimotor Dysfunction: A Controlled Laboratory Study. Am. J. Sports Med. 2024, 52, 739–749. [Google Scholar] [CrossRef]
- Tan, F.; Harput, G.; Ulusoy, B.; Guney-Deniz, H. The influence of unstable surfaces on ankle muscle activation during functional exercises. J. Bodyw. Mov. Ther. 2024, 40, 602–609. [Google Scholar] [PubMed]
- Yekdaneh, A. Effects of Balance and Strength Training for Ankle Proprioception in People with Chronic Ankle Instability: A Randomized Controlled Study. J. Am. Podiatr. Med. Assoc. 2024, 114, 23-008. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, K.; Javanshir, K.; Saadi, F.; Goharpey, S.; Shaterzadeh Yazdi, M.J.; Calvo-Lobo, C.; López-López, D.; Nassadj, G. The Effect of Additional Neuromuscular Training on Peri-Ankle Muscle Morphology and Function in Chronic Ankle Instability Subjects: A Randomized Controlled Trial. Sports Health 2024, 19417381241258468. [Google Scholar] [CrossRef]
- McClean, Z.J.; Pasanen, K.; Lun, V.; Charest, J.; Herzog, W.; Werthner, P.; Black, A.; Vleuten, R.V.; Lacoste, E.; Jordan, M.J. A Biopsychosocial Model for Understanding Training Load, Fatigue, and Musculoskeletal Sport Injury in University Athletes: A Scoping Review. J. Strength Cond. Res. 2024, 38, 1177–1188. [Google Scholar]
- Ribeiro, N.; Martinho, D.V.; Pereira, J.R.; Rebelo, A.; Monasterio, X.; Gonzalo-Skok, O.; Valente-Dos-Santos, J.; Tavares, F. Injury Risk in Elite Young Male Soccer Players: A Review on the Impact of Growth, Maturation, and Workload. J. Strength Cond. Res. 2024, 38, 1834–1848. [Google Scholar]
- Martin, S.; Edouard, P.; Sanchez, X.; Ivarsson, A. Overuse injury and affects in competitive sport: A prospective longitudinal study. Scand. J. Med. Sci. Sports 2024, 34, e14644. [Google Scholar]
- Brennemann, L. Foot and Ankle Complex Injury Prevention for Adolescent Basketball Players: Holistic Guidelines for Trainers. Bachelor’s Thesis, Satakunta University of Applied Sciences, Pori, Poland, 2024. [Google Scholar]
- Bsoul, N.; Ning, L.; Cai, L.; Mazmanyan, D.; Porter, D. Evidence-based clinical practice guidelines for the management of acute ankle injuries according to: A PRISMA systematic review and quality appraisal with AGREE II. BMC Musculoskelet. Disord. 2024, 25, 523. [Google Scholar]
- Meta, F.; Clark, S.C.; Tagliero, A.J.; Hevesi, M.; Saris, D.B.F.; Krych, A.J. Athlete-Specific Considerations of Cartilage Injuries. Sports Med. Arthrosc. 2024, 32, 60–67. [Google Scholar]
- Young, K.L.; Morris, B.; Herda, T.J. The role of strength and conditioning in the prevention and treatment of chronic lateral ankle instability. Strength Cond. J. 2022, 44, 61–75. [Google Scholar]
| Variable | M | SE | 95% CI [Lower, Upper] | SD |
|---|---|---|---|---|
| Ar-CAIT | 18.6 | 0.31 | [18.0, 19.2] | 5.6 |
| Age | 17.4 | 0.21 | [17.0, 17.9] | 3.8 |
| Height (cm) | 169.1 | 0.46 | [168.2, 170.0] | 8.1 |
| Weight (kg) | 65.8 | 0.61 | [64.6, 67.0] | 10.8 |
| BMI | 22.9 | 0.18 | [22.6, 23.3] | 3.2 |
| Training Years | 5.3 | 0.17 | [5.0, 5.6] | 3.01 |
| Training Hours | 2.1 | 0.05 | [2.0, 2.2] | 0.95 |
| RAIs | 1.5 | 0.07 | [0.07, 1.7] | 1.2 |
| Variable | Ar-CAIT | Age | Height | Weight | BMI | Training Years | Training Hours |
|---|---|---|---|---|---|---|---|
| Age | −0.030 | ||||||
| Height | 0.089 | 0.002 | |||||
| Weight | −0.072 | 0.145 | 0.506 * | ||||
| BMI | −0.158 * | 0.119 | −0.034 | 0.810 * | |||
| Training Years | 0.087 | 0.388 | 0.001 | 0.077 | 0.049 | ||
| Training Hours | 0.169 * | −0.032 | 0.096 | −0.118 * | −0.211 * | −0.035 | |
| RAIs | −0.273 ** | 0.079 | 0.044 | 0.122 | 0.107 | 0.049 | 0.009 |
| 95% CI | Assumption Testing (<10) | ||||||
|---|---|---|---|---|---|---|---|
| Predictors | Unstandardized | Standardized | t | p | Lower | Upper | VIF |
| (Intercept) | 18.652 | 59.455 | <0.001 | 18.024 | 19.279 | ||
| (Intercept) | 24.562 | 9.406 | <0.001 | 19.423 | 29.700 | ||
| Age | −0.020 | −0.014 | −0.252 | 0.802 | −0.178 | 0.137 | 1.054 |
| BMI | −0.232 | −0.133 | −2.400 | 0.017 | −0.423 | −0.042 | 1.079 |
| Training Hours | 0.828 | 0.140 | 2.578 | 0.010 | 0.196 | 1.460 | 1.038 |
| RAIs | −1.283 | −0.285 | −5.302 | <0.001 | −1.759 | −0.807 | 1.016 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, A. Predictors of Chronic Ankle Instability Among Soccer Players. Medicina 2025, 61, 555. https://doi.org/10.3390/medicina61040555
Alanazi A. Predictors of Chronic Ankle Instability Among Soccer Players. Medicina. 2025; 61(4):555. https://doi.org/10.3390/medicina61040555
Chicago/Turabian StyleAlanazi, Ahmad. 2025. "Predictors of Chronic Ankle Instability Among Soccer Players" Medicina 61, no. 4: 555. https://doi.org/10.3390/medicina61040555
APA StyleAlanazi, A. (2025). Predictors of Chronic Ankle Instability Among Soccer Players. Medicina, 61(4), 555. https://doi.org/10.3390/medicina61040555






