Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder
Abstract
1. Introduction
2. Methods
3. Results
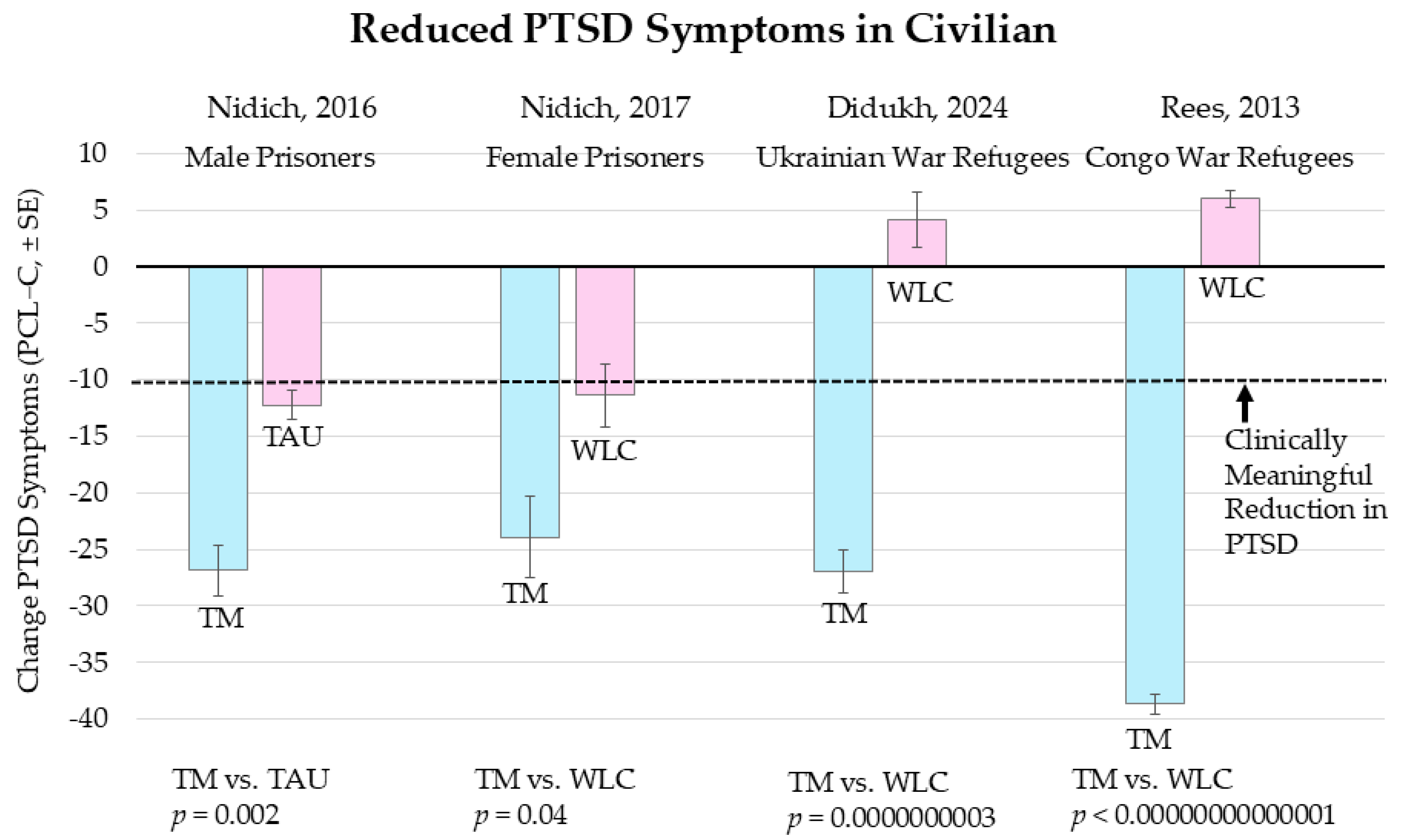
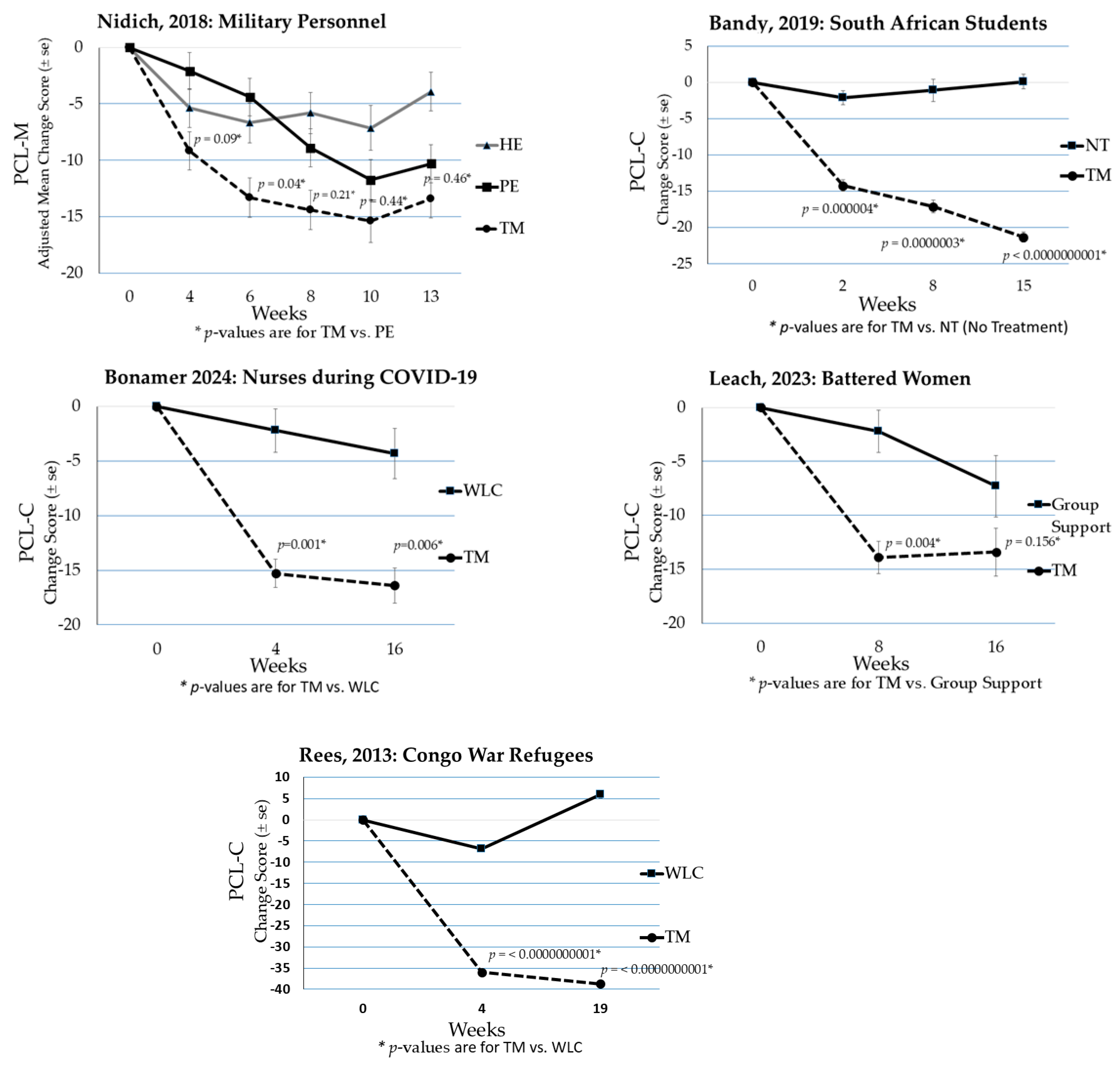
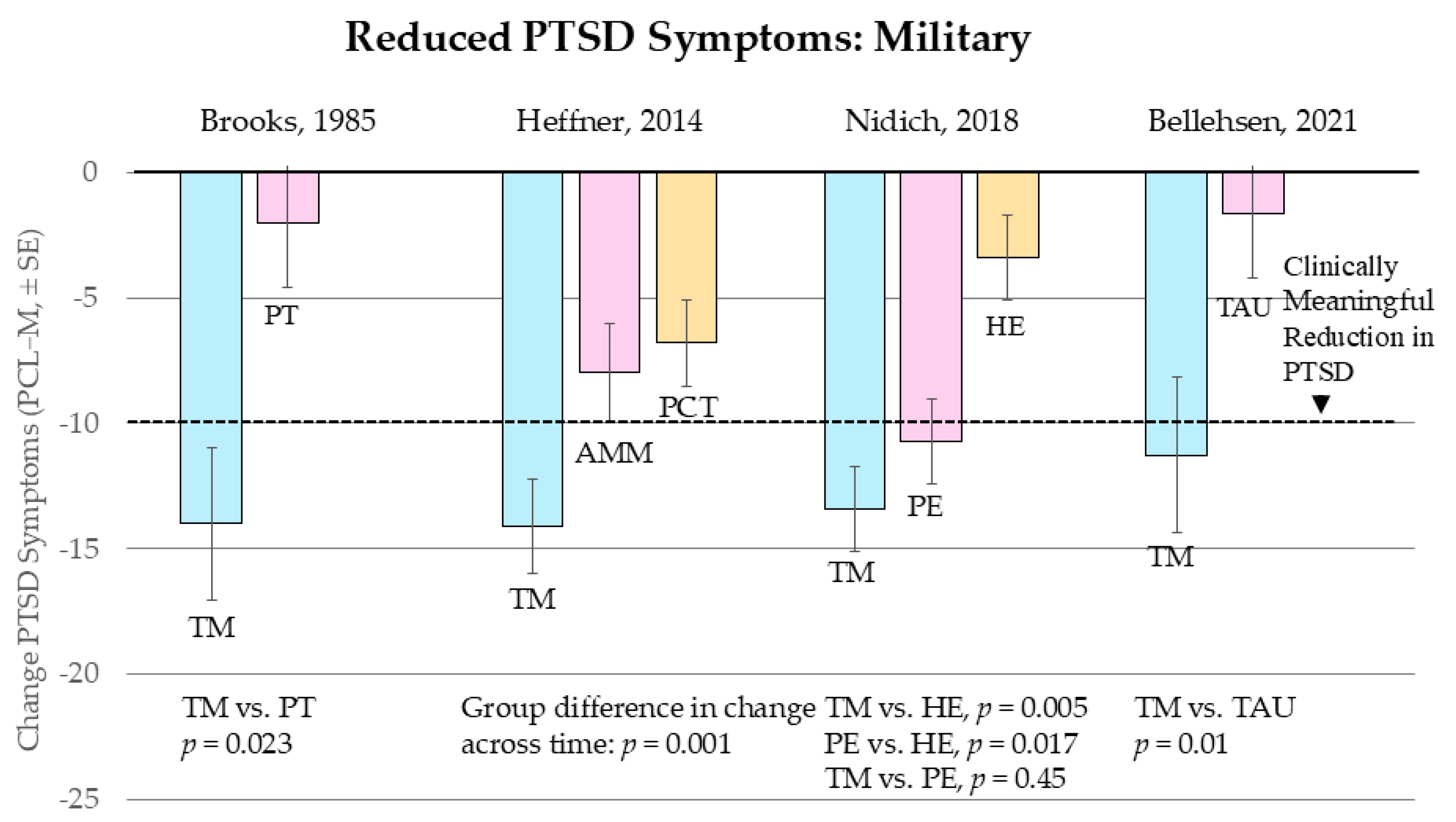
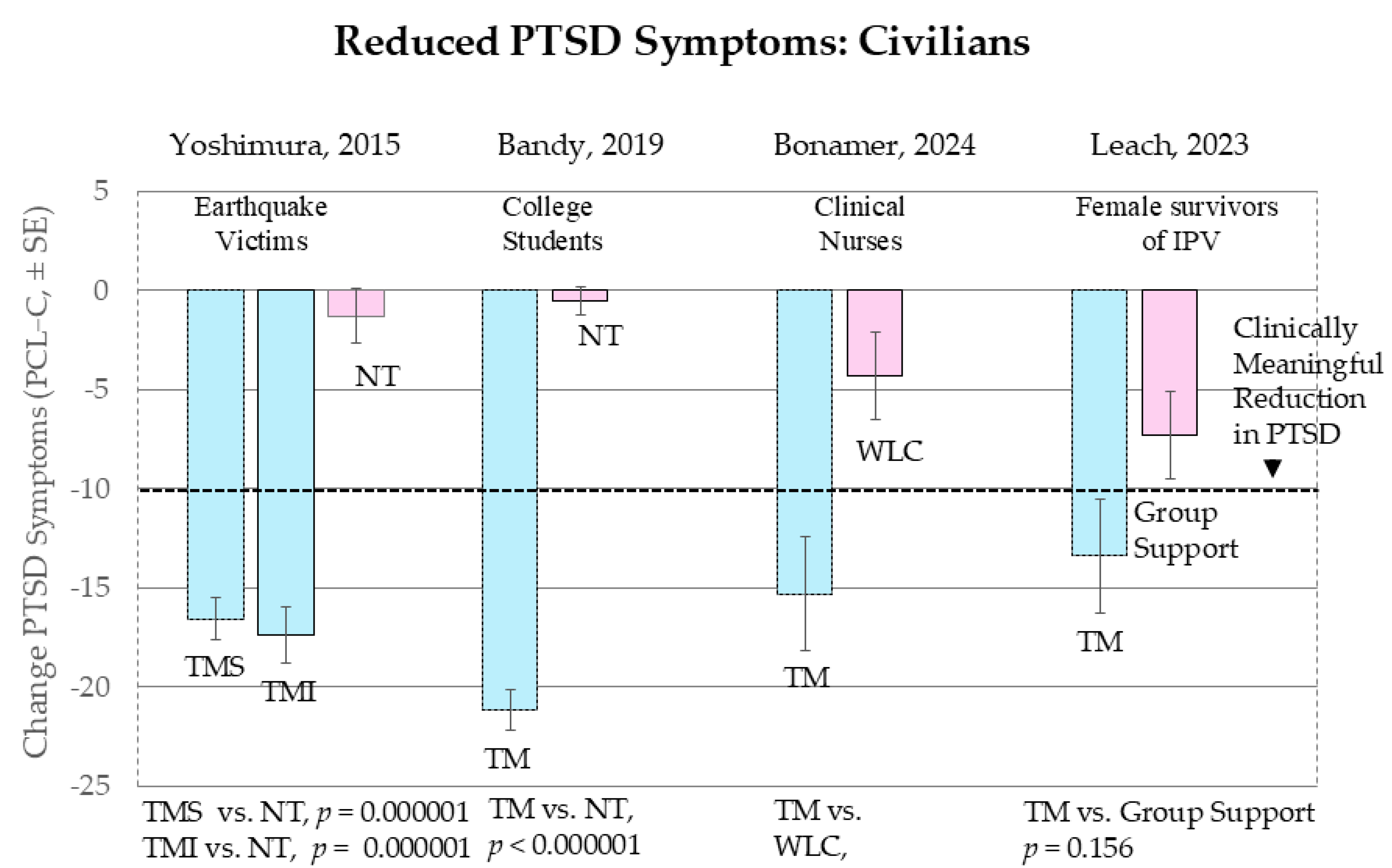
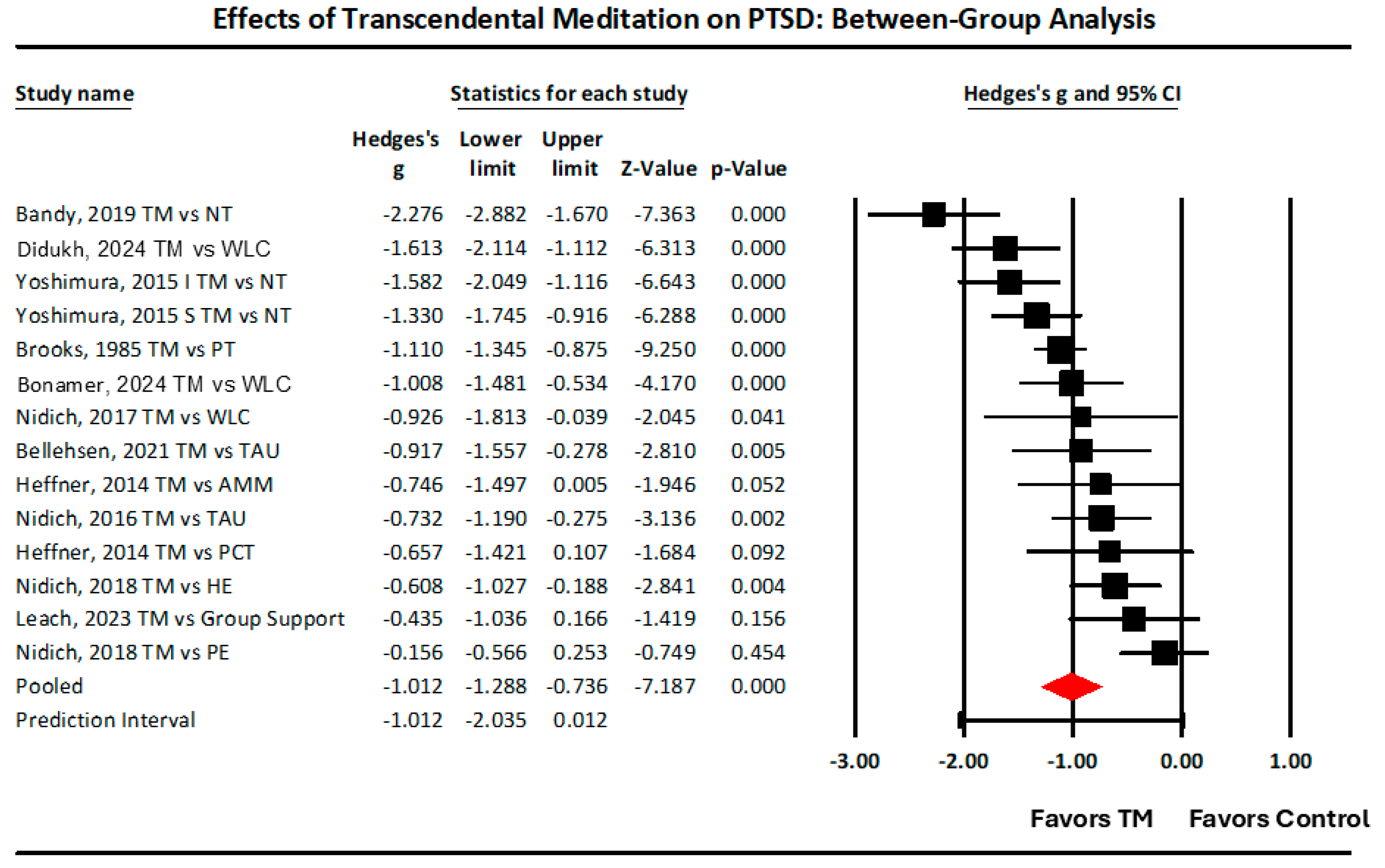
3.1. Part 1: Between Group Analyses Comparing TM with Various Controls
3.1.1. Individual Studies
3.1.2. Repeated Measures Studies on TM: The Rate of Decrease in PTSD Symptoms
3.2. Part 2: Meta-Analytic Synthesis of Between-Group Effects
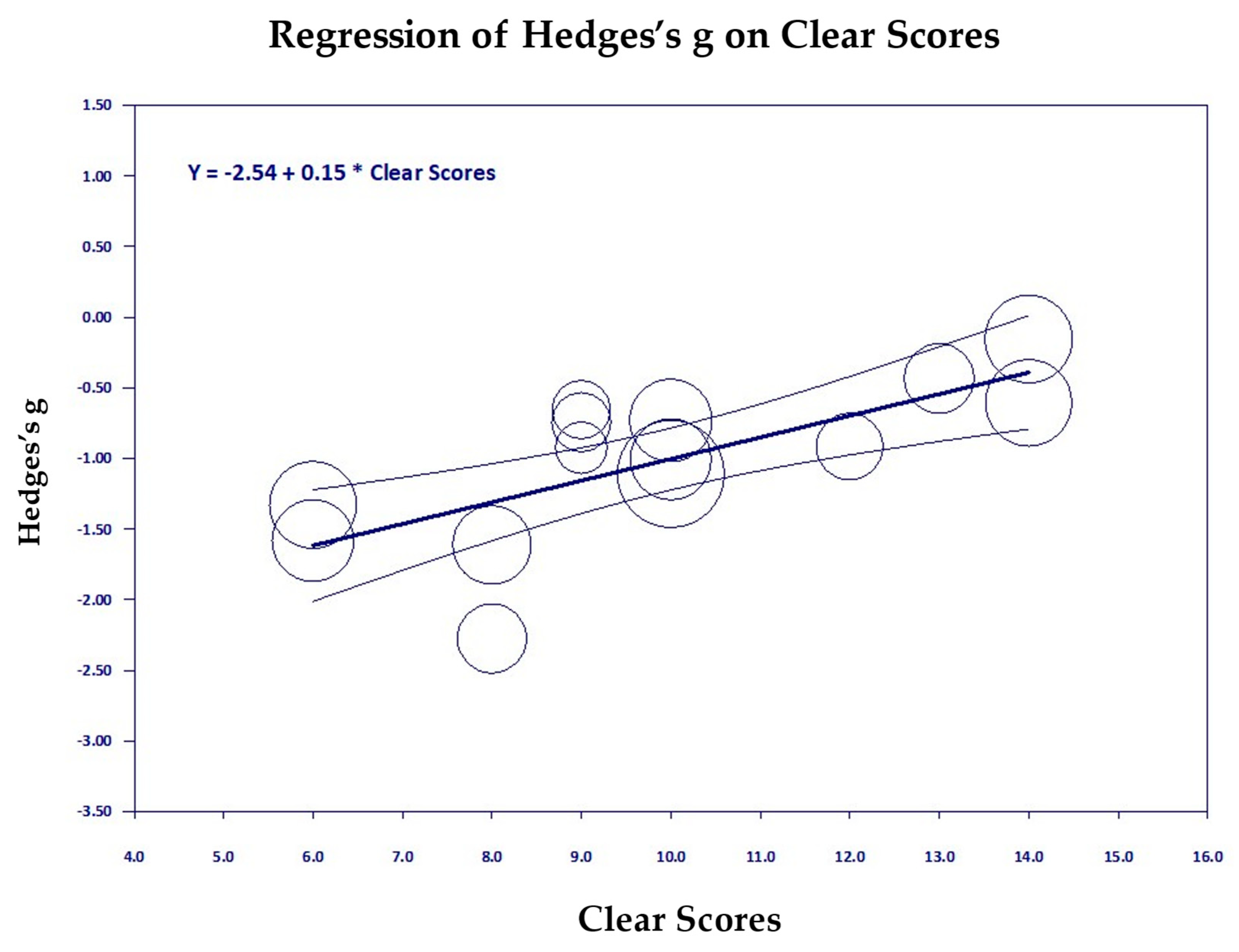
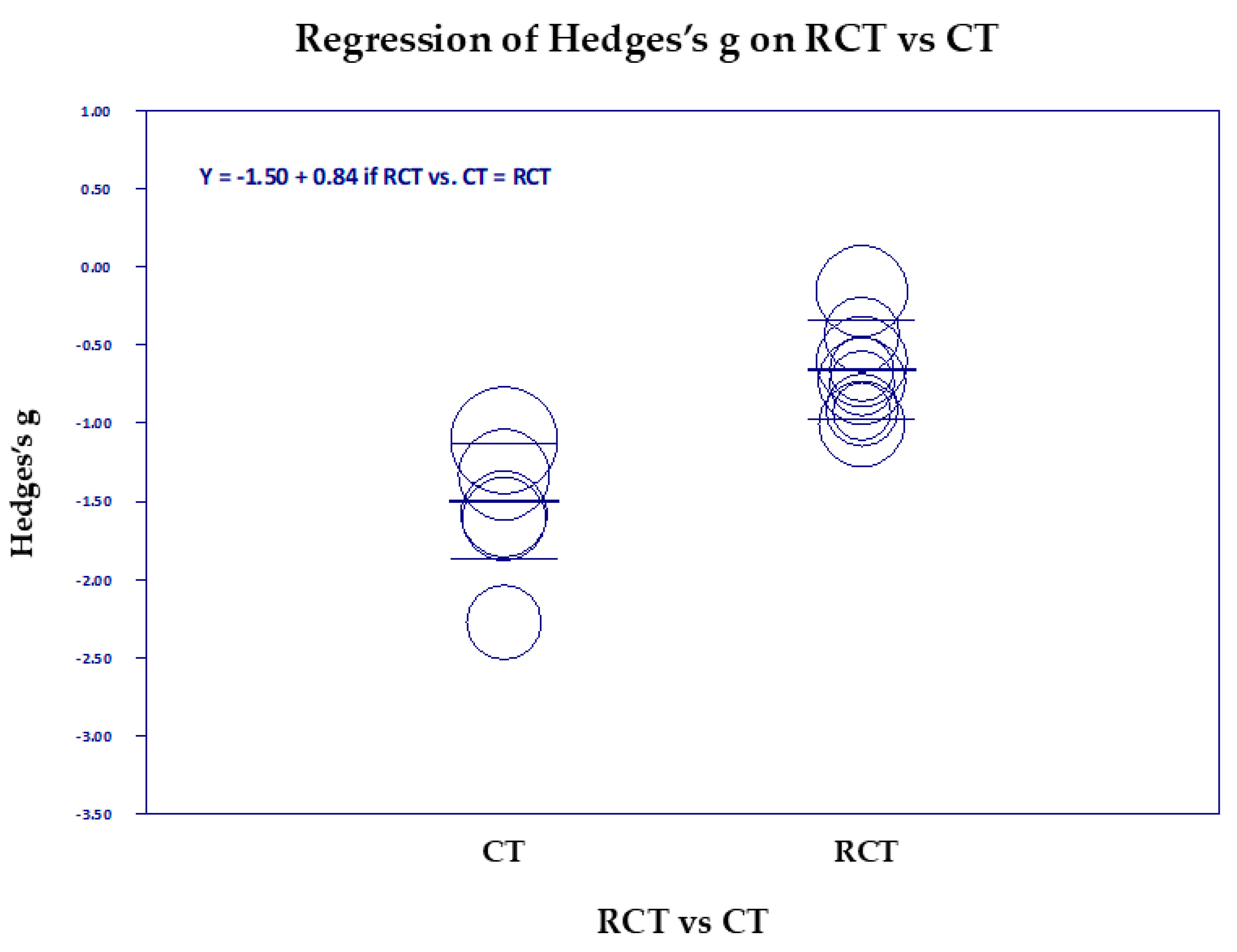
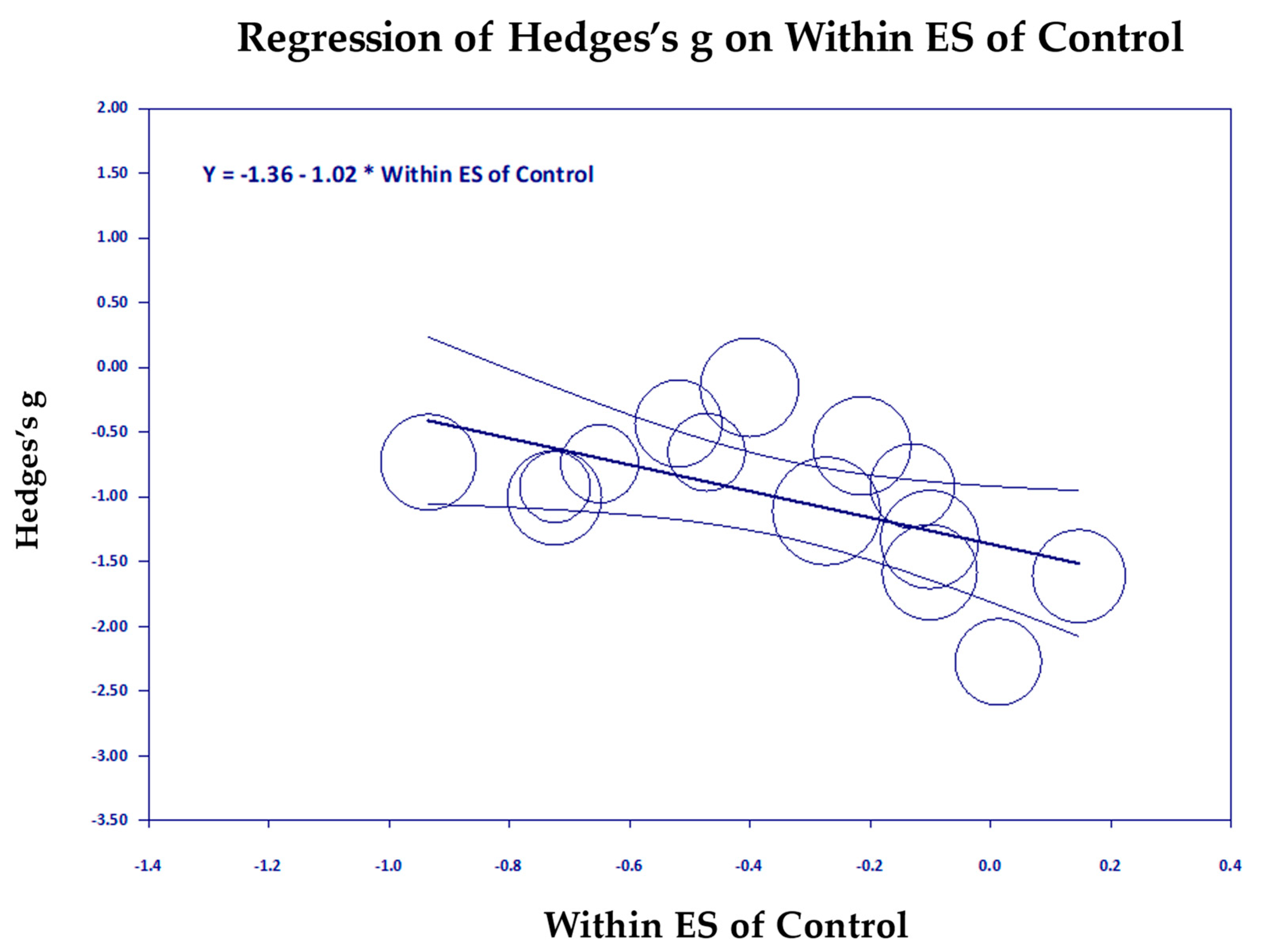
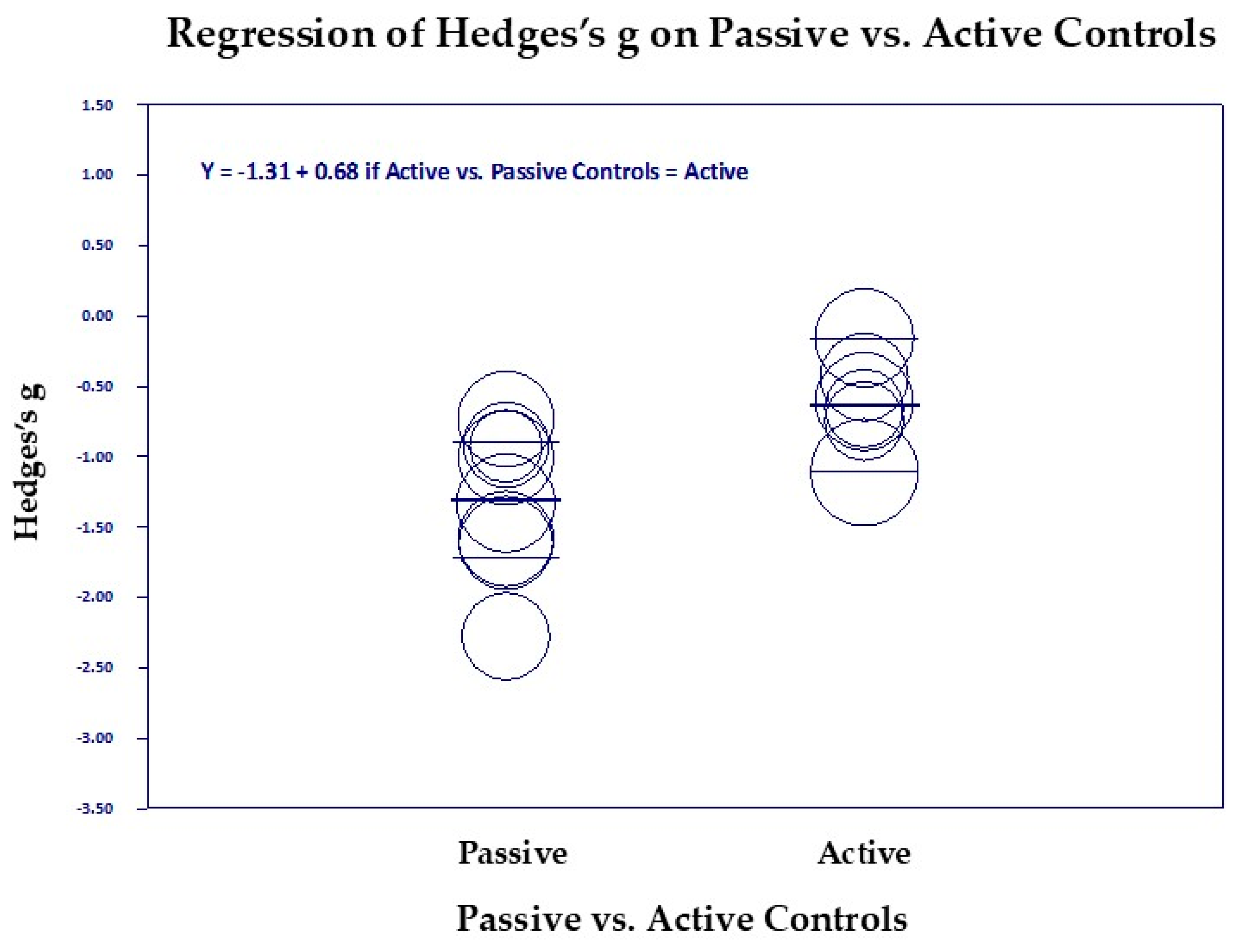
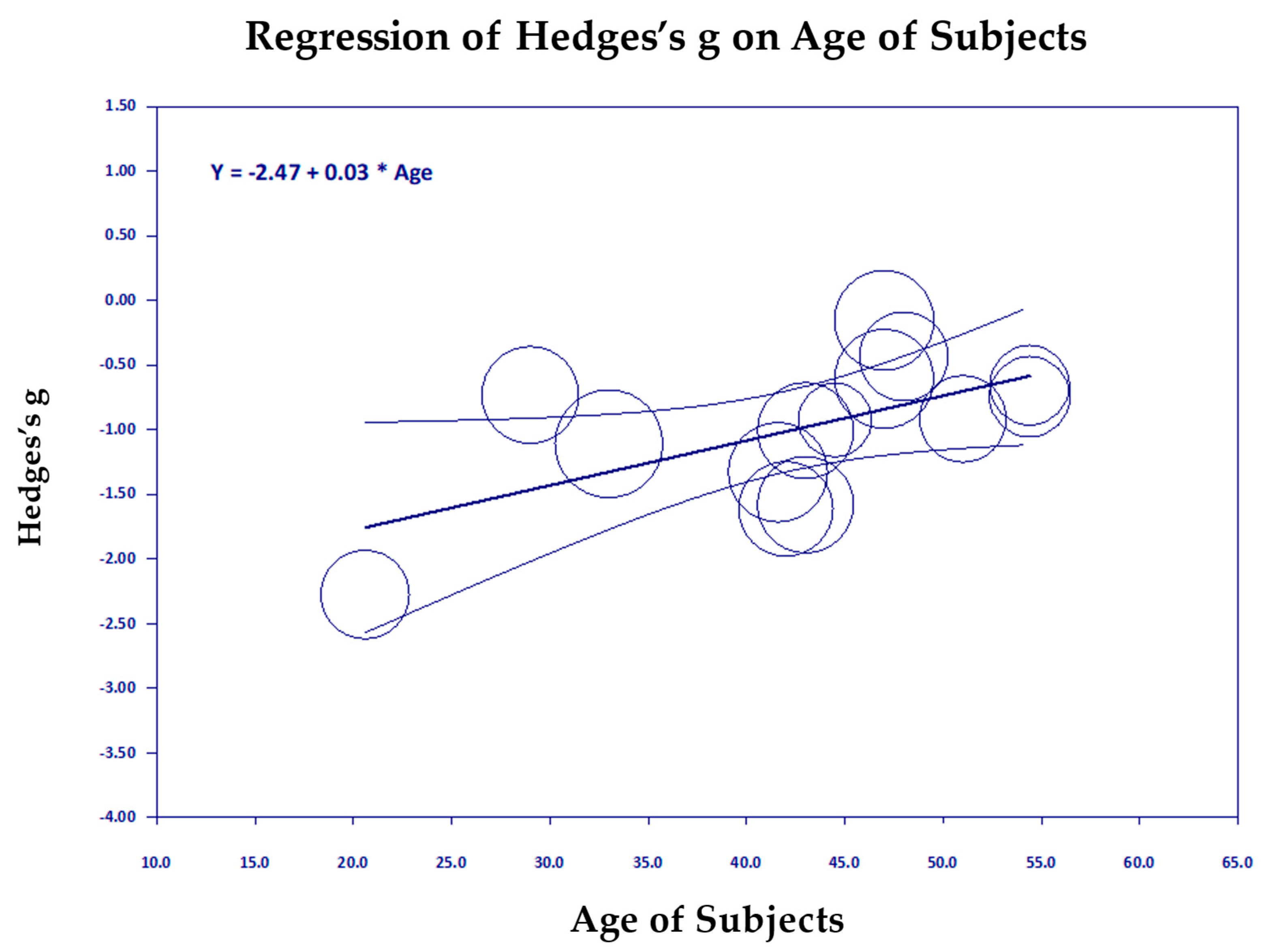
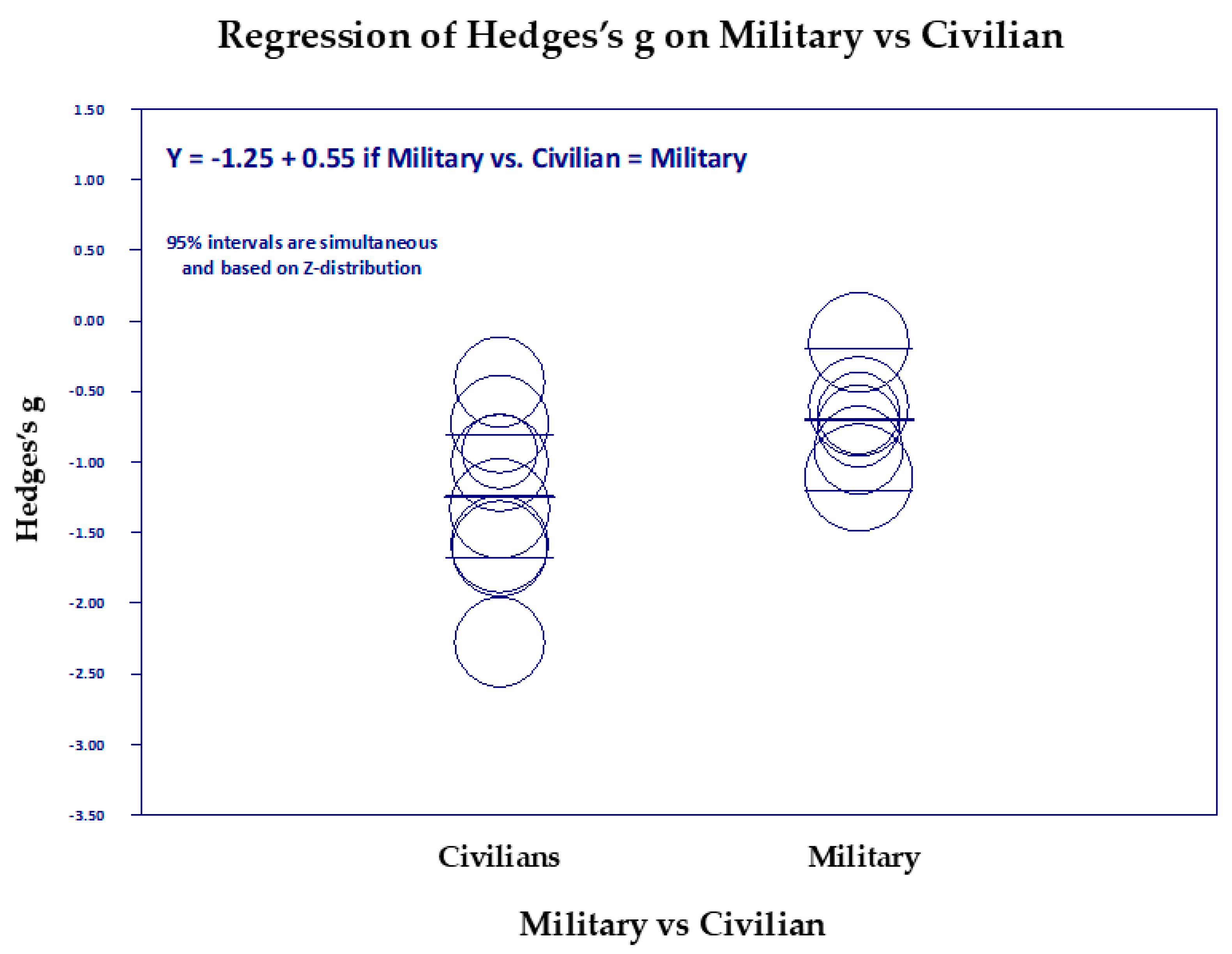
Scatter Diagrams
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mann, S.; Marwaha, R.; Torrico, T. Posttraumatic Stress Disorder; StatPearls Publishing: Treasure Island, FL, USA, 2025; Available online: https://www.statpearls.com/ (accessed on 12 March 2020).
- PTSD: National Center for PTSD. PTSD Checklist for DSM-5 (PCL-5). Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed on 12 March 2020).
- NIH PTSD: National Center for PTSD. Available online: https://www.ptsd.va.gov/understand/common/common_adults.asp (accessed on 12 March 2020).
- Radow, B.; Anderson, N.; Richmond, B. Post-Traumatic Stress Disorder (PTSD) in Trauma Patients. Am. Surg. 2024, 91, 292–299. [Google Scholar] [CrossRef]
- Tanielian, T.; Jaycox, L. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery; RAND Corporation: Santa Monica, CA, USA, 2008. [Google Scholar]
- Davidson, J. Pharmacologic treatment of acute and chronic stress following trauma. J. Clin. Psychiatry 2006, 67 (Suppl. S2), 34–39. [Google Scholar]
- Steenkamp, M.; Litz, B.; Hoge, C.; Marmar, C. Psychotherapy for military-related PTSD: A review of randomized clinical trials. JAMA 2015, 314, 489–500. [Google Scholar] [CrossRef]
- National Center for PTSD: How Common Is PTSD in Veterans? Available online: https://www.ptsd.va.gov/understand/common/common_veterans.asp (accessed on 15 March 2020).
- United Nations Authors. PTSD Statistics. Available online: http://www.ptsdunited.org/ptsd-statistics-2/ (accessed on 7 October 2024).
- Mott, J.; Hundt, N.; Sansgiry, S.; Mignogna, J.; Cully, J.A. Changes in psychotherapy utilization among veterans with depression, anxiety, and PTSD. Psychiatr. Serv. 2014, 65, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Seal, K.; Maguen, S.; Cohen, B.; Gima, K.; Metzler, T.; Ren, L.; Bertenthal, D.; Marmar, C. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J. Trauma Stress 2010, 23, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Gallegos, A.M.; Crean, H.F.; Pigeon, W.R.; Heffner, K.L. Meditation and yoga for posttraumatic stress disorder: A meta-analytic review of randomized controlled trials. Clin. Psychol. Rev. 2017, 58, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Heffner, K.L.; Caine, E.D.; Crean, H.; Franus, N.; Moynihan, J.A.; Talbot, N. Meditation for PTSD Demonstration Project: Final Report to Mental Health Services, Department of Veteran Affairs; Department of Psychiatry at the University of Rochester: Rochester, NY, USA, 2014. [Google Scholar]
- Heffner, K.L.; Crean, H.F.; Kemp, J.E. Meditation programs for veterans with posttraumatic stress disorder: Aggregate findings from a multi-site evaluation. Psychol. Trauma Theory. Res. Pract. Policy 2016, 8, 365–374. [Google Scholar] [CrossRef]
- Hilton, L.; Maher, A.R.; Colaiaco, B.; Apaydin, E.; Sorbero, M.E.; Booth, M.; Shanman, R.M.; Hempel, S. Meditation for posttraumatic stress: Systematic review and meta-analysis. Psychol. Trauma Theory Res. Pract. Policy 2017, 9, 453–460. [Google Scholar] [CrossRef]
- Steenkamp, M.; Litz, B.; Marmar, C. First-line Psychotherapies for Military-Related PTSD. JAMA 2020, 323, 656–657. [Google Scholar] [CrossRef]
- Orme-Johnson, D.W.; Barnes, V.A.; Rees, B.; Tobin, J. A Systematic Review and Meta-Analysis of the Effects of Mindfulness-Based Stress Reduction and the Transcendental Meditation Technique on PTSD.PROSPERO 2019 CRD42019148498 PROSPERO: International Prospective Register of Systematic Reviews: National Institute of Health Research 2020. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42018105225 (accessed on 17 January 2025).
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis, version 4; Biostat: Englewood, NJ, USA, 2022. [Google Scholar]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD Checklist for diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in Veterans. Psychol. Assess. 2016, 28, 1379–1391. [Google Scholar] [CrossRef]
- National Center for PTSD. Using the PTSD Checklist for DSM-IV (PCL) PCL Handouts M4; Affairs, V., Ed.; Department of Veterans Affairs: Washington, DC, USA, 2024; pp. 1–3.
- Hedges, L. Distribution theory for Glass’s estimator of effect size and related estimators. J. Educ. Stat. 1981, 6, 107–128. [Google Scholar]
- Weathers, F.; Keane, T.; Davidson, J. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depress. Anxiety 2001, 13, 132–156. [Google Scholar]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Introduction to Meta-Analysis, 2nd ed.; John Wiley & Sons, Ltd.: Chichester, UK, 2021. [Google Scholar]
- Bandy, C.L.; Dillbeck, M.C.; Sezibera, V.; Taljaard, L.; Wilks, M.; Shapiro, D.; de Reuck, J.; Peycke, R. Reduction of PTSD in South African university students using Transcendental Meditation practice. Psychol. Rep. 2019, 123, 725–740. [Google Scholar] [PubMed]
- Rees, B.; Travis, F.; Shapiro, D.; Chant, R. Reduction in post traumatic stress symptoms in Congolese refugees practicing Transcendental Meditation. J. Trauma Stress 2013, 26, 295–298. [Google Scholar]
- Bonamer, J.; Kutash, M.; Hartranft, S.; Aquino-Russell, C.; Bugajski, A.; Johnson, A. Clinical nurse well-being improved through Transcendental Meditation. J. Nurs. Adm. 2024, 54, 16–24. [Google Scholar]
- Leach, M.; Lorenzon, H. Transcendental Meditation for women affected by domestic violence: A pilot randomised, controlled trial. J. Fam. Violence 2023, 39, 1437–1446. [Google Scholar]
- Nidich, S.; Mills, P.J.; Rainforth, M.; Heppner, P.; Schneider, R.H.; Rosenthal, N.E.; Salerno, J.; Gaylord-King, C.; Rutledge, T. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: A randomised controlled trial. Lancet Psychiatry 2018, 5, 975–986. [Google Scholar]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [PubMed]
- Rosenthal, R. Meta-Analytic Procedures for Social Research; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Orme-Johnson, D.W.; Barnes, V.A.; Rees, B.; Tobin, J.; Walton, K.G. Effectiveness of Meditation Techniques in Treating PTSD: A Systematic Review and Meta-Analysis. Medicina 2024, 60, 2050. [Google Scholar]
- Brooks, J.S.; Scarano, T. Transcendental Meditation and the treatment of post-Vietnam adjustment. J. Couns. Dev. 1985, 64, 212–215. [Google Scholar]
- Bellehsen, M.; Stoycheva, V.; Cohen, B.; Nidich, S. A pilot randomized controlled trial of Transcendental Meditation as treatment for posttraumatic stress disorder in veterans. J. Trauma Stress 2021, 35, 22–31. [Google Scholar]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, Version 6.4; John Wiley & Sons: Chichester, UK, 2023; Available online: https://www.cochrane.org/ (accessed on 6 July 2024).
- Orme-Johnson, D.W. Autonomic stability and Transcendental Meditation. Psychosom. Med. 1973, 35, 341–349. [Google Scholar] [PubMed]
- Schnurr, P.; Friedman, M.; Lavori, P.; Hsieh, F. Design of Department of Veterans Affairs Cooperative Study no. 420: Group treatment of posttraumatic stress disorder. Control. Clin. Trials 2001, 22, 74–88. [Google Scholar]
- Shea, M.T. Present-Centered Therapy for PTSD. U.S. Department of Veterans Affairs, Ed.; PTSD: National Center for PTSD: White River Junction, VT, USA, 2021. Available online: https://www.ptsd.va.gov/professional/treat/txessentials/present_centered_therapy.asp (accessed on 23 November 2023).
- Yoshimura, M.; Etsuko, K.; Noda, T.; Hineno, K.; Tanaka, Y.; Kawai, Y.; Dillbeck, M.C. Disaster relief for the Japanese earthquake-tsunami of 2011: Stress reduction through the Transcendental Meditation technique. Psychol. Rep. Ment. Phys. Health 2015, 117, 206–216. [Google Scholar]
- Ferris, E.; Solis, M. Earthquake, Tsunami, Meltdown—The Triple Disaster’s Impact on Japan, Impact on the World. Available online: https://www.brookings.edu/articles/earthquake-tsunami-meltdown-the-triple-disasters-impact-on-japan-impact-on-the-world/ (accessed on 22 March 2025).
- American Nurses Association. COVID-19. Impact Assessment Survey—The Second Year; ANA Enterprise: COVID-19 Resource Center: Silver Spring, MD, USA, 2022. [Google Scholar]
- Bonamer, J.R.; Aquino-Russell, C. Self-care strategies for professional development: Transcendental Meditation reduces compassion fatigue and improves resilience for nurses. J. Nurses Prof. Dev. 2019, 35, 93–97. [Google Scholar] [PubMed]
- Bonamer, J.; Ruff, A.; Kutash, M.; Hartranft, S.; Aquino-Russell, C.; Johnson, A. Transcendental Meditation® for Clinical Nurses’ Well-Being. In National Magnet Conference; American Nurses Credentialing Center (ANCC): Philadelphia, PA, USA, 2022. [Google Scholar]
- United Nations. What Is Domestic Abuse? Available online: https://www.un.org/en/coronavirus/what-is-domestic-abuse (accessed on 4 April 2023).
- World Health Organization. Violence Against Women Prevalence Estimates, 2018: Global, Regional and National Prevalence Estimates for Intimate Partner Violence Against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence Against Women. Available online: https://www.who.int/publications/i/item/9789240022256 (accessed on 12 March 2023).
- Nidich, S.; O’Connor, T.; Rutledge, T.; Duncan, J.; Compton, B.; Seng, A.; Nidich, R. Reduced trauma symptoms and perceived stress in male prison Inmates through the Transcendental Meditation program: A randomized controlled trial. Perm. J. 2016, 20, 16-007. [Google Scholar]
- Nidich, S.; Seng, A.; Compton, B.; O’Connor, T.; Salerno, J.W.; Nidich, R. Transcendental Meditation and Reduced Trauma Symptoms in Female Inmates: A Randomized Controlled Study. Perm. J. 2017, 21, 39–43. [Google Scholar]
- Didukh, M.L.; Freytag, K.S. Reduction in symptoms of posttraumatic stress disorder and depression in Ukrainian refugees practicing Transcendental Meditation. Perspect. Behav. Sci. 2024; submitted. [Google Scholar]
- Freytag, K.S.; Didukh, M. Vedic meditation as a treatment for trauma-related mental disorders. Sci. Educ. 2023, 4, 63–69. [Google Scholar]
- Operation Data Portal Refugees from Ukraine recorded in Europe by the UN Refugee Agency (UNHCR). Available online: https://data.unhcr.org/en/situations/ukraine (accessed on 15 June 2023).
- Wikipedia Authors. Second Congo War. Available online: https://en.wikipedia.org/wiki/Second_Congo_War (accessed on 15 June 2023).
- Center for Preventive Action Conflict in the Democratic Republic of Congo. Available online: https://www.cfr.org/global-conflict-tracker/conflict/violence-democratic-republic-congo (accessed on 15 June 2023).
- Rees, B.; Travis, F.; Shapiro, D.; Chant, R. Significant Reductions in Posttraumatic Stress Symptoms in Congolese Refugees after 10 days Transcendental Meditation Practice. J. Trauma Stress 2014, 27, 112–115. [Google Scholar]
- Vancampfort, D.; Stubbs, B.; Van Damme, T.; Smith, L.; Hallgren, M.; Schuch, F.; Deenik, J.; Rosenbaum, S.; Ashdown-Franks, G.; Mugisha, J. The efficacy of meditation-based mind-body interventions for mental disorders: A meta-review of 17 meta-analyses of randomized controlled trials. J. Psychiatr. Res. 2021, 134, 181–191. [Google Scholar] [PubMed]
- Sun, L.; Gu, J.; Huang, L.; Shang, Z.; Wu, L.; Jia, Y.; Liu, N.; Liu, W. Military-related posttraumatic stress disorder and mindfulness meditation: A systematic review and meta-analysis. Chin. J. Traumatol. 2021, 24, 221–230. [Google Scholar]
- Orme-Johnson, D.W. Transcendental Meditation in the Treatment of Mental and Physical Conditions. In The Oxford Handbook of Meditation; Farias, M., Brazier, D., Lalljee, M., Eds.; Oxford University Press: Oxford, UK, 2021. [Google Scholar]
- Maharishi Mahesh Yogi on the Bhagavad-Gita: A New Translation And Commentary, Chapters 1–6; Penguin Books Inc.: Baltimore, MD, USA, 1969.
- Dillbeck, M.C.; Orme-Johnson, D.W. Physiological differences between Transcendental Meditation and rest. Am. Psychol. 1987, 42, 879–881. [Google Scholar]
- MacLean, C.R.K.; Walton, K.G.; Wenneberg, S.R.; Levitsky, D.K.; Schneider, R.H. Apparent serum dehydroepiandrosterone response to acute laboratory stress. Soc. Neurosci. Abstr. 1993, 19, 169. [Google Scholar]
- Barnes, V.A.; Orme-Johnson, D.W. Prevention and treatment of cardiovascular disease in adolescents and adults through the Transcendental Meditation program®: A research review update. Curr. Hypertens. Rev. 2012, 8, 227–242. [Google Scholar]
- Barnes, V.A.; Treiber, F.A.; Davis, H. Impact of Transcendental Meditation on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. J. Psychosom. Res. 2001, 51, 597–605. [Google Scholar]
- Walton, K.G.; Levitsky, D.K. Stress-induced neuroendocrine abnormalities in aggression and crime—Apparent reversal by the Transcendental Meditation program. J. Offender Rehabil. 2003, 36, 67–87. [Google Scholar]
- Goldmann, E.; Aiello, A.; Uddin, M.; Delva, J.; Koenen, K.; Gant, L.M.; Galea, S. Pervasive Exposure to Violence and Posttraumatic Stress Disorder in a Predominantly African American Urban Community: The Detroit Neighborhood Health Study. J. Trauma Stress 2011, 24, 747–751. [Google Scholar]
- Haratani, T.; Hemmi, T. Effects of Transcendental Meditation on health behavior of industrial workers. Jpn. J. Public Health 1990, 37 (Suppl. S10), 729. [Google Scholar]
- So, K.T.; Orme-Johnson, D.W. Three randomized experiments on the holistic longitudinal effects of the Transcendental Meditation technique on cognition. Intelligence 2001, 29, 419–440. [Google Scholar]
- Alexander, C.N.; Langer, E.J.; Newman, R.I.; Chandler, H.M.; Davies, J.L. Transcendental Meditation, mindfulness, and longevity: An experimental study with the elderly. J. Personal. Soc. Psychol. 1989, 57, 950–964. [Google Scholar]
- Alexander, C.N.; Rainforth, M.V.; Gelderloos, P. Transcendental Meditation, Self-Actualization and Psychological Health: A Conceptual Overview and Statistical Meta-Analysis. J. Soc. Behav. Personal. 1991, 6, 189–247. [Google Scholar]
- Chandler, H.; Alexander, C.; Heaton, D.; Grant, J. Transcendental Meditation and postconventional self-development: A 10-year longitudinal study. J. Soc. Behav. Personal. 2005, 17, 93–122. [Google Scholar]
- Goldstein, L.; Nidich, S.; Goodman, R.; Goodman, D.H. The effect of Transcendental Meditation on self-efficacy, perceived stress, and quality of life of mothers in Uganda. Health Care Women Int. 2018, 39, 734–754. Available online: https://www.tandfonline.com/eprint/pm88crSrBmtfsbRgG75F/full (accessed on 19 March 2022). [PubMed]
- Travis, F.T.; Arenander, A. Cross-sectional and longitudinal study of effects of Transcendental Meditation practice on interhemispheric frontal asymmetry and frontal coherence. Int. J. Neurosci. 2006, 116, 1519–1538. [Google Scholar]
- Avvenuti, G.; Leo, A.; Cecchetti, L.; Fatima, M.; Frederick, F.; Travis, F.; Caramella, D.; Bernardi, G.; Ricciardi, E.; Pietrini, P. Reductions in perceived stress following Transcendental Meditation practice are associated with increased brain regional connectivity at rest. Brain Cogn. 2020, 139, 105517. [Google Scholar]
| Study ID | Location | Population/Trauma Type | Research Design | Cont. Group | Baseline PTSD TM, C | Research Quality | Mean Age TM, C | Sample Total | % Males TM | Study Duration (Week) |
|---|---|---|---|---|---|---|---|---|---|---|
| Heffner, 2014 Saginaw TM [13] | Saginaw MI VA | Military/Combat-trauma | RCT | AMM, PCT | TM, AMM, PCT 66, 61, 60 | 7 | 54, 55 | 65 | 74 | 8 |
| Nidich, 2016 TM [45] | Oregon | Civilian/Male Prison Inmates/Interpersonal violence, | RCT | TAU | 35, 31 | 10 | 29, 30 | 181 | 100 | 16 |
| State Penitentiary | ||||||||||
| Nidich, 2017 TM [46] | Coffee Creek Correctional Facility, Wilsonville, OR | Civilian/Female Prison Inmates/Interpersonal violence | RCT | WLC | 53, 52 | 9 | 45, 45 | 20 | 0 | 16 |
| Nidich, 2018 TM [28] | San Diego VA | Military/Combat trauma | RCT | PE, HE | TM, PE, HE 61, 61, 59 | 14 | TM, PE, HE 46, 46, 46 | 202 | 82 | 13 |
| Bellehsen, 2021 TM [33] | Veterans Administration Medical Center Long Island, NY | Military/Combat trauma | RCT | TAU | 53, 54 | 12 | 53, 50 | 40 | 80 | 12 |
| Leach, 2023 TM [27] | University of South Australia, Adelaide | Civilian/Abused Women, Domestic Violence | RCT | Facilitated Group Support | 33, 30 | 13 | 48, 47 | 42 | 0 | 16 |
| Bonamer, 2024 TM [26] | Sarasota Memorial Health Care System. Moffitt Cancer Center, Tampa General Hospital | Civilian/Nurses Caregiver Stress | RCT | WLC | 29, 25 | 10 | 42, 44 | 104 | 0 | 12 |
| Brooks, 1985 TM [32] | VA Denver Colorado, US | Military/Combat-trauma | CT | PT | 60, 60 | 9 | 33, 33 | 18 | 100 | 12 |
| Rees, 2013 TM [25] | Kampala, Uganda | Civilian/War Refugees, Combat Trauma, | CT | WLC | 65, 68 | 9 | 33, 31 | 42 | 65 | 19 |
| Yoshimura, 2015 Ishinomaki TM [38] | Sendai, Ishinomaki, | Civilian/Earthquake–Tsunami, Disaster Trauma | CT | NT | I, S, T 33, 34, 23 | 6 | 43, 42, 40 | 239 | 19 | 1 |
| Tokyo, Japan | ||||||||||
| Bandy, 2019 TM [24] | Johannesburg, South Africa | Civilian/College Students, sexual and criminal victimization, combat | CT | NT | 53, 57 | 8 | 21, 21 | 68 | 21 | 15 |
| Didukh, 2024 TM [47] | Lubeck, Germany | Civilian/War Refugees in Ukraine/ Interpersonal violence | CT | WCL | 32, 25 | 8 | 40, 37 | 80 | 23 | 8 |
| Age of the Subjects | Sample Size N | % Males in the Study | Study Duration (Weeks) | |
|---|---|---|---|---|
| Mean | 40.5 | 91.8 | 46.9 | 12.3 |
| SD | 2.4 | 10.1 | 74.8 | 40.1 |
| Range | 20.6 to 54.4 | 18 to 239 | 0% to 100% | 1 to 19 |
| Covariate | p-Value | R2 | I2 | Type of Covariate |
|---|---|---|---|---|
| Clear Score | 0.000007 | 0.78 | 42.97, p = 0.05 | Research Design |
| RCT vs. CT: CT | 0.00002 | 0.68 | 51.00, p = 0.02 | Research Design |
| Within-Group ES of Controls | 0.01 | 0.34 | 69.44, p = 0.0001 | Research Design |
| Active vs. Passive | 0.008 | 0.26 | 70.62, p = 0.00005 | Research Design |
| Age | 0.015 | 0.24 | 71.71, p = 00003 | Subject Variable |
| Military vs. Civilian | 0.04 | 0.13 | 73.84, p = 0.000007 | Subject Variable |
| Study Duration | 0.18 | 0.13 | 74.82, p = 0.000004 | Research Design |
| Five Trauma Groups | 0.2 | 0.04 | 76.76, p = 0.00003 | Subject Variable |
| % Males | 0.18 | 0 | 76.63, p = 0.0000008 | Subject Variable |
| Baseline PTSD | 0.6 | 0 | 78.75, p = 0.0000001 | Subject Variable |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orme-Johnson, D.W.; Barnes, V.A.; Rees, B.; Tobin, J. Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder. Medicina 2025, 61, 659. https://doi.org/10.3390/medicina61040659
Orme-Johnson DW, Barnes VA, Rees B, Tobin J. Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder. Medicina. 2025; 61(4):659. https://doi.org/10.3390/medicina61040659
Chicago/Turabian StyleOrme-Johnson, David W., Vernon A. Barnes, Brian Rees, and Jean Tobin. 2025. "Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder" Medicina 61, no. 4: 659. https://doi.org/10.3390/medicina61040659
APA StyleOrme-Johnson, D. W., Barnes, V. A., Rees, B., & Tobin, J. (2025). Systematic Review and Meta-Analysis of Transcendental Meditation for Post-Traumatic Stress Disorder. Medicina, 61(4), 659. https://doi.org/10.3390/medicina61040659








