Adverse Childhood Experiences in Children with Intellectual Disabilities: An Exploratory Case-File Study in Dutch Residential Care
Abstract
:1. Introduction
1.1. The ACEs Framework
1.2. The Evolving ACEs Concept
1.3. Prevalence of ACEs
1.4. The Vulnerability of the Child with ID
1.5. The Influence of Parental ACEs
1.6. Impact on Children’s and Adolescents’ Health
1.7. The Present Study
2. Materials and Methods
2.1. Sample
2.2. Procedure
2.3. Measures
2.4. Statistical Analyses
3. Results
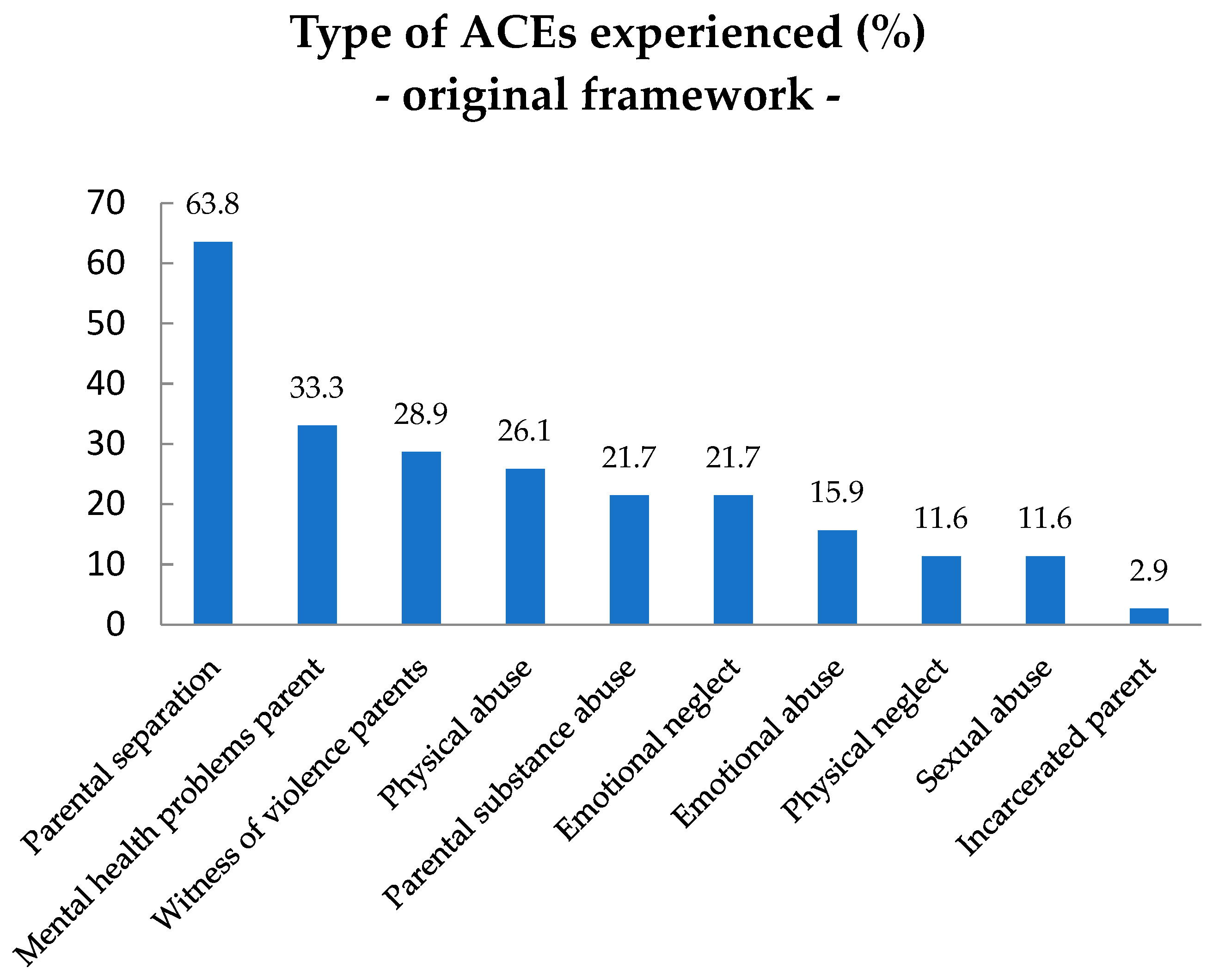
3.1. Prevalence of ACEs from the Original ACEs Framework in Children with ID and their Parents
3.2. Associations between Original ACEs and Problem Behavior, Youth Psychopathology and Physical Health Problems
3.3. Associations between ACEs from the Original and the Expanded ACEs Framework and Living Circumstances of the Child
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shonkoff, J.P.; Garner, A.S.; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care and Section on Developmental and Behavioral Pediatrics; Siegel, B.J.; Dobbins, M.I.; Earls, M.F.; Garner, A.S.; McGuinn, L.; Pascoe, J.; et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012, 129, e232–e246. [Google Scholar] [CrossRef] [PubMed]
- Bethell, C.D.; Carle, A.; Hudziak, J.; Gombojav, N.; Powers, K.; Wade, R.; Braveman, P. Methods to assess adverse childhood experiences of children and families: Toward approaches to promote child well-being in policy and practice. Acad. Pediatr. 2017, 17, S51–S69. [Google Scholar] [CrossRef] [PubMed]
- Bethell, C.D.; Solloway, M.R.; Guinosso, S.; Hassink, S.; Srivastav, A.; Ford, D.; Simpson, L.A. Prioritizing possibilities for child and family health: An agenda to address adverse childhood experiences and foster the social and emotional roots of well-being in pediatrics. Acad. Pediatr. 2017, 17, S36–S50. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Bellis, M.A.; Lowey, H.; Leckenby, N.; Hughes, K.; Harrison, D. Adverse childhood experiences: Retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J. Public Health 2013, 36, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef]
- McLaughlin, K.A. Future directions in childhood adversity and youth psychopathology. J. Clin. Child Adolesc. Psychol. 2016, 45, 361–382. [Google Scholar] [CrossRef] [PubMed]
- Nurius, P.S.; Green, S.; Logan-Green, P.; Borja, S. Life course pathways of adverse childhood experiences toward adult psychosocial well-being: A stress process analysis. Child Abus. Negl. 2015, 45, 143–153. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K.A. Science Brief: The Long Shadow of Adverse Childhood Experiences; American Psychological Association (APA): Washington, DC, USA, 2017. [Google Scholar]
- Oral, R.; Ramirez, M.; Coohey, C.; Nakada, S.; Walz, A.; Kuntz, A.; Benoit, J.; Peek-Asa, C. Adverse childhood experiences and trauma informed care: The future of health care. Pediatr. Res. 2016, 79, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Grimes, K.E. Lessons from ACEs: Pay now or pay (more) later. Acad. Pediatr. 2017, 17, S18–S19. [Google Scholar] [CrossRef] [PubMed]
- Zeanah, C.H.; Sonuga-Barke, E.J.S. The effects of early trauma and deprivation on human development—From measuring cumulative risk to characterizing specific mechanisms. J. Child Psychol. Psychiatry 2016, 57, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Northway, R. Laying the foundations for health. J. Intellect. Disabil. 2017, 21, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Sege, R.D.; Browne, C.H. Responding to ACEs with HOPE: Health outcomes from positive experiences. Acad. Pediatr. 2017, 17, S79–S85. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.; Costigan, T.; Schubert, K. Promoting lifelong health and well-being: Staying the course to promote health and prevent the effects of adverse childhood and community experiences. Acad. Pediatr. 2017, 17, S4–S6. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K.A.; Lambert, H.K. Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Curr. Opin. Psychol. 2017, 14, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Keesler, J.M. A call for the integration of trauma-informed care among intellectual and developmental disability organizations. J. Policy Pract. Intellect. Disabil. 2014, 11, 34–42. [Google Scholar] [CrossRef]
- Keesler, J.M. Trauma-informed day services for individuals with intellectual/developmental disabilities: Exploring staff understanding and perception within an innovative programme. J. Appl. Res. Intellect. Disabil. 2016, 29, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Emerson, E. The Determinants of Health Inequities Experienced by Children with Learning Disabilities; Public Health England: London, UK, 2015. [Google Scholar]
- Bouras, N.; Jacobson, J. Mental health care for people with mental retardation: A global perspective. World Psychiatry 2002, 1, 162–165. [Google Scholar] [PubMed]
- Nouwens, P.J.; Lucas, R.; Smulders, N.B.; Embregts, P.J. Identifying classes of persons with mild intellectual disability or borderline intellectual functioning: A latent class analysis. BMC Psychiatry 2017, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Nadarajah, J.; Roy, A.; Harris, T.O.; Corbett, J.A. Methodological aspects of live events research in people with learning disabilities: A review and initial findings. J. Intellect. Disabil. Res. 1995, 39, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.C.; Greenspan, S. Definition and nature of intellectual disability. In Handbook of Evidence-Based Practices in Intellectual and Developmental Disabilities; Singh, N.N., Ed.; Springer: Basel, Switzerland, 2016; pp. 11–39. ISBN 978-3-319-26581-0. [Google Scholar]
- Schalock, R.L. The evolving understanding of the construct of intellectual disability. J. Intellect. Dev. Disabil. 2011, 36, 223–233. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Association (APA). Handboek Voor de Classificatie van Psychische Stoornissen (DSM-5), 5th ed.; Nederlandse Vertaling van Diagnostic and Statistical Manual of Mental Disorders; APA: Arlington, TX, USA, 2014. [Google Scholar]
- De Bruijn, J.; Buntinx, W.H.; Twint, B. Verstandelijke Beperking: Definitie en Context; SWP: Amsterdam, The Netherlands, 2014; pp. 91–100. ISBN 9789088504396. [Google Scholar]
- Mason-Roberts, S.; Bradley, A.; Karatzias, T.; Brown, M.; Paterson, D.; Walley, R.; Truesdale, M.; Taggart, L.; Sirisena, C. Multiple traumatisation and subsequent psychopathology in people with intellectual disabilities and DSM-5 PTSD: A preliminary study. J. Intellect. Disabil. Res. 2018, 62, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Catani, C.; Sossalla, I.M. Child abuse predicts adult PTSD symptoms among individuals diagnosed with intellectual disabilities. Front. Psychol. 2015, 6, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hatton, C.; Emerson, E. The relationship between life events and psychopathology amongst children with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2004, 17, 109–117. [Google Scholar] [CrossRef]
- Marcal, S.; Trifoso, S. A Trauma-Informed Toolkit for Providers in the Field of Intellectual & Developmental Disabilities; Center for Disability Services: New York, NY, USA, 2017; Available online: https://www.acesconnection.com/blog/a-trauma-informed-toolkit-for-providers-in-the-field-of-intellectual-disabilities (accessed on 13 August 2017).
- Martorell, A.; Tsakanikos, E. Traumatic experiences and life events in people with intellectual disability. Curr. Opin. Psychiatry 2008, 21, 445–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mevissen, L.; Didden, R.; de Jongh, A. EMDR voor trauma- en stressor-gerelateerde klachten bij patiënten met een verstandelijke beperking. Dir. Ther. 2016, 1, 5–25. [Google Scholar]
- Wigham, S.; Hatton, C.; Taylor, J.L. The Lancaster and Northgate Trauma Scales (LANTS): The development and psychometric properties of a measure of trauma for people with mild to moderate intellectual disabilities. Res. Dev. Disabil. 2011, 32, 2651–2659. [Google Scholar] [CrossRef] [PubMed]
- Dekker, M.C.; Koot, H.M. DSM-IV disorders in children with borderline to moderate intellectual disability. I: Prevelance and impact. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Emerson, E.; Hatton, C. Mental health of children and adolescents with intellectual disabilities in Britain. Br. J. Psychiatry 2007, 191, 493–499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Einfeld, S.; Ellis, L.A.; Emerson, E. Comorbidity of intellectual disability and mental disorder in children and adolescents: A systematic review. J. Intellect. Dev. Disabil. 2011, 36, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Emerson, E. Prevalence of psychiatric disorders in children and adolescents with and without intellectual disability. J. Intellect. Disabil. Res. 2003, 47, 51–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hastings, R.P.; Hatton, C.; Taylor, J.L.; Maddison, C. Life events and psychiatric symptoms in adults with intellectual disabilities. J. Intellect. Disabil. Res. 2004, 48, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Hulbert-Williams, L.; Hastings, R.; Owen, D.M.; Burns, L.; Day, J.; Mulligan, J.; Noone, S.J. Exposure to life events as an risk factor for psychological problems in adults with intellectual disabilities: A longitudinal design. J. Intellect. Disabil. Res. 2014, 58, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Hulbert-Williams, L.; Hastings, R.P.; Crowe, R.; Pemberton, J. Self-reported life events, social support and psychological problems in adults with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2011, 24, 427–436. [Google Scholar] [CrossRef]
- Hove, O.; Assmus, J.; Havik, O.E. Type and intensity of negative life events are associated with depression in adults with intellectual disabilities. Am. J. Iintellect. Dev. Disabil. 2016, 121, 419–431. [Google Scholar] [CrossRef] [PubMed]
- Martorell, A.; Tsakanikos, E.; Pereda, A.; Gutiérrez-Recacha, P.; Bouras, N.; Ayuso-Mateos, J.L. Mental health in adults with mild and moderate intellectual disabilities: The role of recent life events and traumatic experiences across the life span. J. Nerv. Ment. Dis. 2009, 197, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Wigham, S.; Taylor, J.L.; Hatton, C. A prospective study of the relationship between adverse life events and trauma in adults with mild to moderate intellectual disabilities. J. Intellect. Disabil. Res. 2014, 58, 1131–1140. [Google Scholar] [CrossRef] [PubMed]
- Tsakanikos, E.; Bouras, N.; Costello, H.; Holt, G. Multiple exposure to life events and clinical psychopathology in adults with intellectual disability. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Olofson, M.W. A new measurement of adverse childhood experiences drawn from the panel study of income dynamics child development supplement. Child. Indic. Res. 2018, 11, 629–647. [Google Scholar] [CrossRef]
- Ford, D. The community and public well-being model: A new framework and graduate curriculum for addressing adverse childhood experiences. Acad. Pediatr. 2017, 17, S9–S11. [Google Scholar] [CrossRef] [PubMed]
- Dunn, V.J.; Abbott, R.A.; Croudace, T.J.; Wilkinson, P.; Jones, P.B.; Herbert, J.; Goodyer, I.M. Profiles of family-focused adverse experiences through childhood and early adolescence: The ROOTS project a community investigation of adolescent mental health. BMC Psychiatry 2011, 11, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kessler, R.C.; Aguilar-Gaxiola, S.; Alonso, J.; Benjet, C.; Bromet, E.J.; Cardoso, G.; Degenhardt, L.; de Girolamo, G.; Dinolova, R.V.; Ferry, F.; et al. Trauma and PTSD in the WHO world mental health surveys. Eur. J. Psychotraumatol. 2017, 8, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Kalmakis, K.A.; Chandler, G.E. Health consequences of adverse childhood experiences: A systematic review. J. Med. Assoc. Nurse Pract. 2015, 27, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Finkelhor, D. Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abus. Negl. 2017. [Google Scholar] [CrossRef] [PubMed]
- Finkelhor, D.; Shattuck, A.; Turner, H.; Hamby, S. Improving the adverse childhood experiences study scale. JAMA Pediatr. 2013, 167, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Kalmakis, K.A.; Chandler, G.E. Adverse childhood experiences: Towards a clear conceptual meaning. J. Adv. Nurs. 2014, 70, 1489–1501. [Google Scholar] [CrossRef] [PubMed]
- Cronholm, P.F.; Forke, C.M.; Wade, R.; Bair-Merrit, M.H.; Davis, M.; Markins-Schwarz, M.; Pachter, L.M.; Fein, J.A. Adverse childhood experiences, expanding the concept of adversity. Am. J. Prev. Med. 2015, 49, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Finkelhor, D.; Shattuck, A.; Turner, H.; Hamby, S. A revised inventory of adverse childhood experiences. Child Abus. Negl. 2015, 48, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Soleimanpour, S.; Geierstanger, S.; Brindis, C.D. Adverse childhood experiences and resilience: Addressing the unique needs of adolescents. Acad. Pediatr. 2017, 17, S108–S114. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Tucker, W. Invited commentary: Poverty as an adverse childhood experience. N. C. Med. J. 2018, 79, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Bruner, C. ACE, place, race, and poverty: Building hope for children. Acad. Pediatr. 2017, 17, S123–S129. [Google Scholar] [CrossRef] [PubMed]
- Woodman, A.C.; Mailick, M.R.; Anderson, K.A.; Esbensen, A.J. Residential transitions among adults with intellectual disability across 20 years. Am. J. Intellect. Dev. Disabil. 2014, 119, 496–515. [Google Scholar] [CrossRef] [PubMed]
- Schermerhorn, A.C. Associations of child emotion recognition with interparental conflict and shy child temperament traits. J. Soc. Pers. Relatsh. 2018, 1–24. [Google Scholar] [CrossRef]
- Merrick, M.T.; Ports, K.A.; Ford, D.C.; Afifi, T.O.; Gershoff, E.T.; Grogan-Kaylor, A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abus. Negl. 2017, 69, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Afifi, T.O.; Ford, D.; Gershoff, E.T.; Merrick, M.; Grogan-Kaylor, A.; Ports, K.A.; MacMillan, H.L.; Holden, G.W.; Taylor, C.A.; Lee, S.J.; et al. Spanking and adult mental health impairment: The case for the designation of spanking as an adverse childhood experience. Child Abus. Negl. 2017, 71, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Shonkoff, J.; Levitt, P.; Bunge, S.; Cameron, J.; Duncan, G.; Fisher, P.; Nox, N. Supportive Relationships and Active Skill-Building Strengthen the Foundations of Resilience: Working Paper 13; National Scientific Council on the Developing Child: Cambridge, UK, 2015; Available online: https://developingchild.harvard.edu/resources/supportive-relationships-and-active-skill-building-strengthen-the-foundations-of-resilience/ (accessed on 14 September 2017).
- Copeland, W.E.; Keeler, G.; Angold, A.; Costello, E.J. Traumatic events and posttraumatic stress in childhood. Arch. Gen. Psychiatry 2007, 64, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Perez, N.M.; Jennings, W.G.; Baglivio, M.T. A path to serious, violent, chronic delinquency: The harmful aftermath of adverse childhood experiences. Crime Delinq. 2018, 64, 3–25. [Google Scholar] [CrossRef]
- Alisic, E. Teachers ’perspectives on providing support to children after trauma: A qualitative study. Sch. Psychol. Q. 2012, 27, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Vink, R.; Pal, S.; Eekhout, I.; Pannebakker, F.; Mulder, T. Report: Ik Heb al veel Meegemaakt: Ingrijpende Jeugdervaringen (ACE) bij Leerlingen in Groep 7/8 van het REGULIER Basisonderwijs; TNO: Leiden, The Netherlands, 2016; Available online: https://repository.tudelft.nl/view/tno/uuid:641d3e67-38e3-45f5-ad8e-47894d82a4be/ (accessed on 12 August 2017).
- Ziv, Y.; Sofri, I.; Capps Umphlet, K.L.; Olarte, S.; Venza, J. Children and caregivers’ exposure to adverse childhood experiences (ACES): Association with children’s and caregivers’ psychological outcomes in a therapeutic preschool program. Int. J. Environ. Res. Public Health 2018, 15, 646. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, M.; Halfon, N. Pediatric adverse childhood experiences: Implications for life course health trajectories. Acad. Pediatr. 2015, 15, 467–468. [Google Scholar] [CrossRef] [PubMed]
- Reichman, N.E.; Corman, H.; Noonan, K.; Jimenez, M.E. Infant health and future childhood adversity. Matern. Child Health J. 2018, 22, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Lanier, P.; Maguire-Jack, K.; Lombardi, B.; Frey, J.; Rose, R.A. Adverse childhood experiences and child health outcomes: Comparing cumulative risk and latent class approaches. Matern. Child Health J. 2018, 22, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Moonen, X. (H)erkennen en Waarderen; Universiteit van Amsterdam faculteit der Maatschappij-en Gedragswetenschappen: Amsterdam, The Netherlands, 2017. (In Dutch) [Google Scholar]
- Beckmann, K.A. Mitigating adverse childhood experiences through investments in early childhood programs. Acad. Pediatr. 2017, 17, S28–S29. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W.; Li, D.; Whipple, S.S. Cumulative risk and child development. Psychol. Bull. 2013, 139, 1342–1396. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, J. Post-traumatic stress disorder in people with learning disability. Adv. Psychiatr. Treat. 2001, 7, 163–169. [Google Scholar] [CrossRef] [Green Version]
- Lindblad, I.; Billstedt, E.; Gillberg, C.; Fernell, E. A register study of life events in young adults born to mothers with mild intellectual disability. J. Intellect. Disabil. 2014, 18, 351–363. [Google Scholar] [CrossRef] [PubMed]
- Wyman, J.D.; Lavoie, J.; Talwar, V. Best practices for interviewing children with intellectual disabilities in maltreatment cases. Exceptionality 2018, 1–18. [Google Scholar] [CrossRef]
- Horner-Johnson, W.; Drum, C.E. Prevalence of maltreatment of people with intellectual disabilities: A review of recently published research. Ment. Retard. Dev. Disabil. Res. Rev. 2006, 12, 57–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sullivan, P.M.; Knutson, J.F. Maltreatment and disabilities: A population-based epidemiological study. Child Abus. Negl. 2000, 24, 1257–1273. [Google Scholar] [CrossRef]
- Hassall, R.; Rose, J.; McDonald, J. Parenting stress in mothers of children with an intellectual disability: The effects of parental cognitions in relation to child characteristics and family support. J. Intellect. Disabil. Res. 2005, 49, 405–418. [Google Scholar] [CrossRef] [PubMed]
- Küffer, A.L.; Thoma, M.V.; Maercker, A. Transgenerational aspects of former Swiss child laborers: Do second generations suffer from their parents’ adverse early-life experiences? Eur. J. Psychotraumatol. 2016, 7, 30804. [Google Scholar] [CrossRef] [PubMed]
- Schickedanz, A.; Halfon, N.; Sastry, N.; Chung, P.J. Parents’ adverse childhood experiences and their children’s behavioral health problems. Pediatrics 2018, 142, e20180023. [Google Scholar] [CrossRef] [PubMed]
- Folger, A.T.; Eismann, E.A.; Stephenson, N.B.; Shapiro, R.A.; Macaluso, M.; Brownrigg, M.E.; Gillespie, R.J. Parental adverse childhood experiences and offspring development at 2 years of age. Pediatrics 2018, e20172826. [Google Scholar] [CrossRef] [PubMed]
- Lê-Scherban, F.; Wang, X.; Boyle-Steed, K.H.; Pachter, L.M. Intergenerational associations of parent adverse childhood experiences and child health outcomes. Pediatrics 2018, 141, e20174274. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.N.; Beck, A.F.; Sucharew, H.J.; Litman, S.; Pfefferman, C.; Haney, J.; Samir, S.; Simmons, M.; Auger, A. Parental adverse childhood experiences and resilience on coping after discharge. Pediatrics 2018, e20172127. [Google Scholar] [CrossRef] [PubMed]
- Bouvette-Turcot, A.A.; Bernier, A.; Meaney, M. Intergenerational transmission of psychosocial risk: Maternal childhood adversity, mother-child attachment, and child temperament. Psychol. Belg. 2013, 53, 65–83. [Google Scholar] [CrossRef]
- Racine, N.; Plamondon, A.; Madigan, S.; McDonald, S.; Tough, S. Maternal adverse childhood experiences and infant development. Pediatrics 2018, e20172495. [Google Scholar] [CrossRef] [PubMed]
- Plant, D.T.; Jones, F.W.; Pariante, C.M.; Pawlby, S. Association between maternal childhood trauma and offspring childhood psychopathology: Mediation analysis form the ALSPAC cohort. Br. J. Psychiatry 2017, 211, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Patel, F.; Rose-Jacobs, R.; Frank, D.A.; Black, M.M.; Chilton, M. Mothers’ adverse childhood experiences and their young children’s development. Am. J. Prev. Med. 2017, 53, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Murphy, A.; Steele, M.; Dube, S.R.; Bate, J.; Bonuck, K.; Meissner, P.; Goldman, H.; Steele, H. Adverse childhood experiences (ACEs) questionnaire and adult attachment interview (AAI): Implications for parent child relationships. Child Abuse Negl. 2014, 38, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Murphy, A.; Steele, H.; Steele, M.; Allman, B.; Kastner, T.; Dube, S.R. The clinical Adverse Childhood Experiences (ACEs) questionnaire: Implications for trauma-informed behavioral healthcare. In Integrated Early Childhood Behavioral Health in Primary Care; Briggs, R.D., Ed.; Springer: Basel, Switzerland, 2016; pp. 7–16. ISBN 9783319318134. [Google Scholar]
- Corcoran, M.; McNulty, M. Examining the role of attachment in the relationship between childhood adversity, psychological distress and subject well-being. Child Abus. Negl. 2018, 76, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Granqvist, P.; Forslund, T.; Fransson, M.; Springer, L.; Lindberg, L. Mothers with intellectual disability, their experiences of maltreatment, and their children’s attachment representations: A small-group matched comparison study. Attach. Hum. Dev. 2014, 16, 417–436. [Google Scholar] [CrossRef] [PubMed]
- Bethell, C.D.; Davis, M.B.; Gombojav, N.; Stumbo, S.; Powers, K. Issue Brief: A National and Across-State Profile on Adverse Childhood Experiences among U.S. Children and Possibilities to Heal and Thrive; Johns Hopkins Bloomberg School of Public Health: Baltimore, MD, USA, 2017; Available online: https://pcal.org/wp-content/uploads/2017/11/Aces_Brief_Final_USChildren.pdf (accessed on 18 March 2018).
- Thompson, R.A. Issue Brief: Social-Emotional Development in the First Three Years: Establishing the Foundations; Edna Bennett Pierce Prevention Research Center: University Park, PA, USA, 2018; Available online: https://www.rwjf.org/content/dam/farm/reports/issue_briefs/2018/rwjf444708 (accessed on 16 April 2018).
- Korotona, L.M.; Dobson, K.S.; Pusch, D.; Josephson, T. A review of primary care interventions to improve health outcomes in adult survivors of adverse childhood experiences. Clin. Psychol. Rev. 2016, 46, 59–90. [Google Scholar] [CrossRef] [PubMed]
- Biglan, A.; Van Ryzin, M.J.; Hawkins, J.D. Evolving a more nurturing society to prevent adverse childhood experiences. Acad. Pediatr. 2017, 17, S150–S157. [Google Scholar] [CrossRef] [PubMed]
- Heleniak, C.; Jenness, J.L.; Vander Stoep, A.; McCauley, E.; McLaughlin, K.A. Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognit. Ther. Res. 2016, 40, 394–415. [Google Scholar] [CrossRef] [PubMed]
- Schilling, E.A.; Aseltine, R.H.; Gore, S. Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health 2007, 7. [Google Scholar] [CrossRef] [PubMed]
- Hunt, T.K.A.; Slack, K.S.; Berger, L.M. Adverse childhood experiences and behavioral problems in middle childhood. Child Abus. Negl. 2016, 67, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Peshevska, D.J.; Raleva, M.; Filov, I.; Sethi, D.; Jordanova, T.; Hamza, K.H.; Tozija, F.; Ilievska, V.D. Association between physical abuse, physical neglect and health risk behaviours among young adolescents: Results from the national study. Maced. J. Med. Sci. 2014, 7, 386–391. [Google Scholar] [CrossRef]
- Stempel, H.; Cox-Martin, M.; Bronsert, M.; Dickinson, L.; Allison, M.A. Chronic school absenteeism and the role of adverse childhood experiences. Acad. Pediatr. 2017, 17, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Dunn, E.C.; Wang, Y.; Tse, J.; McLaughlin, K.A.; Fitzmaurice, G.; Gilman, S.E.; Susser, E.S. Sensitive periods for the effect of childhood interpersonal violence on psychiatric disorder onset among adolescents. Br. J. Psychiatry 2017, 211, 365–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Björkenstam, E.; Hjern, A.; Mittendorfer-Rutz, E.; Vinnerljung, B.; Hallqvist, J. Multi-Exposure and Clustering of Adverse Childhood Experiences. PLoS ONE 2013, 8, e53551. [Google Scholar] [CrossRef] [PubMed]
- Yurdakök, K. Neonatal maltreatment and brain development. J. Pediatr. Neonatal Individ. Med. 2014, 3, e030228. [Google Scholar]
- Kerker, B.D.; Zhang, J.; Nadeem, E.; Stein, R.E.; Hurlburt, M.S.; Heneghan, A.; Landsverk, J.; McCue Horwitz, S. Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Acad. Pediatr. 2015, 15, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.; Flaherty, E.G.; English, D.J.; Litrownik, A.J.; Dubowitz, H.; Kotch, J.B.; Runyan, D.K. Trajectories of adverse childhood experiences and self-reported health at age 18. Acad. Pediatr. 2015, 15, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Lackner, C.L.; Santesso, D.L.; Dywan, J.; O’Leary, D.; Wade, T.J.; Segalowitz, S.J. Adverse childhood experiences are associated with self-regulation and the magnitude of the error-related negativity difference. Boil. Psychol. 2018, 132, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Burke Harris, N.; Silvéro Marques, S.; Oh, D.; Bucci, M.; Cloutier, M. Prevent, screen, heal: Collective action to fight the toxic effects of early life adversity. Acad. Pediatr. 2017, 17, S14–S15. [Google Scholar] [CrossRef] [PubMed]
- Drury, S.S.; Howell, B.R.; Jones, C.; Esteves, K.; Morin, E.; Schlesinger, R.; Meyer, J.S.; Baker, K.; Sanchez, M.M. Shaping long-term primate development: Telomere length trajectory as an indicator of early maternal maltreatment and predictor of future physiologic regulation. Dev. Psychopathol. 2017, 29, 1539–1551. [Google Scholar] [CrossRef] [PubMed]
- Elbers, J.; Rovnaghi, C.R.; Golianu, B.; Anand, K.J. Clinical profile associated with adverse childhood experiences: The advent of nervous system dysregulation. Children 2017, 4, 98. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; McLaughlin, K.A.; Green, J.G.; Gruber, M.J.; Sampson, N.A.; Zaslavsky, A.M.; Aguilar-Gaxiola, S.; Alhamzawi, A.O.; Alonso, J.; Angermeyer, M.; et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br. J. Psychiatry 2010, 197, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Sara, G.; Lappin, J. Comment: Childhood trauma: Psychiatry’s greatest public health challenge? Lancet Public Health 2017, 2, e300–e301. [Google Scholar] [CrossRef]
- Jones, T.M.; Nurius, P.; Song, C.; Fleming, C.M. Modeling life course pathways from adverse childhood experiences to adult mental health. Child Abuse Negl. 2018, 80, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA School-Age Forms & Profiles; University of Vermont, Research Center for Children, Youth & Families: Burlinton, VT, USA, 2001. [Google Scholar]
- Nederlands Jeugdinstituut. Available online: https://www.nji.nl/nl/Databank/Classificatie-Jeugdproblemen/Classificeren-met-CAP-J (accessed on 15 April 2018).
- Turk, J.; Robbins, I.; Woodhead, M. Post-traumatic stress disorder in young people with intellectual disability. J. Intellect. Disabil. Res. 2005, 49, 872–875. [Google Scholar] [CrossRef] [PubMed]



| Variable | Percentage (n) |
|---|---|
| Child Characteristics | |
| Gender, % male | 66.7% (46) |
| Age, mean (SD) | 11.3 (SD = 3.1) |
| Nationality, % Dutch | 92.8% (64) |
| Mean years of social-emotional developmental delay | 6.3 (SD = 3.2) |
| Attachment problems (DSM-IV) | 33.3% (23) |
| Trauma and stressor- related problems (DSM-IV) | 32.9% (23) |
| Coping problems | 17.4% (12) |
| Emotion regulation problems | 62.3% (43) |
| Suicidal ideation | 11.6% (8) |
| Sexual rule-breaking behavior | 17.1% (12) |
| Sexual risk taking behavior | 10% (7) |
| Average number of attended schools | 2.9 (SD = 1.4) |
| Physical health characteristics of the child | |
| Experienced clinical hospitalization | 34.3% (24) |
| Sleeping problems | 27.5% (19) |
| Obstipation | 13% (9) |
| Overweight or obese | 30.4% (21) |
| Eczema | 15.5% (10) |
| Headaches and/or stomach pains | 12.9% (9) |
| Allergies | 7.1% (5) |
| Respiratory symptoms (asthma, bronchitis) | 5.7% (4) |
| Use of psychotropic medication | 55.7% (39) |
| Sleep medication and tranquillizers | 32.9% (23) |
| Antipsychotic medications | 30% (21) |
| Stimulants | 18.6% (13) |
| Anti-depressants | 4.3% (3) |
| Family characteristics | |
| Biological parent(s) with ACEs | 28.6% (20) |
| Biological parent(s) with an ID | 27.1% (19) |
| Physical health problems parent(s) * | 31.9% (22) |
| Parent(s) involved with justice (incarceration excluded) | 8.6% (6) |
| Divorced or separated biological parents | 63.8% (44) |
| New composed family | 37.7% (26) |
| One parent household | 34.8% (24) |
| Average number of primary caregivers | 2.4 (SD = 0.8) |
| Average number of (step)siblings grown up with | 2.8 (SD = 1.4) |
| Child protection/welfare involved | 33.3% (23) |
| Parent(s) in debt | 23.2% (16) |
| Parent(s) with housing problems | 7.2% (5) |
| Unemployment father | 15.9% (11) |
| Unemployment mother | 36.2% (25) |
| Limited social network | 30% (21) |
| Problematic caregiver burden | 70% (49) |
| Limited parenting competence | 24.3% (17) |
| Problematic caregiver-child relationship | 37.1% (26) |
| Residence before admission to De Hondsberg | |
| Living with parent(s) | 66.6% (46) |
| Residential youth care | 14.3% (10) |
| Crisis intervention residence | 11.6% (8) |
| Foster care | 4.3% (3) |
| Family | 1.4% (1) |
| ACEs | Definition |
|---|---|
| Physical abuse | Being pushed, beaten, grabbed, slapped, kicked or being hit so hard resulting in marks or injury |
| Emotional abuse | Being sworn at, insulted, threatened, put down |
| Physical neglect | Parent’s or primary caregiver’s behavior interfered with the child’s care, wearing dirty clothes, bad hygiene, not enough personal living space, no safe living space, not enough to eat, not taken to a doctor when sick, forced to take care for themselves |
| Emotional neglect | Parents didn’t make the child feel special and loved, the family not being a source of strength, protection and support, the child receiving little attention |
| Sexual abuse | Being involuntarily touched in a sexual way, forced into any form of sexual contact, forced into watching sexual content |
| Parental incarceration | A parent or primary caregiver being incarcerated |
| Parental separation/divorce | Separation or divorce of biological parents |
| Witness of violence against a parent | The child being a witness of verbal or physical violence (abuse) against the parent or primary caregiver |
| Parental substance abuse | Excessive alcohol use or drug use of the parent or primary caregiver |
| Parental mental health problems | Biological parent(s) having mental health problems (anxiety, depression, bipolar disorder or other mental issues/illnesses) interfering with the child’s care or having a parent ever attempted suicide |
| ACEs Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Emotional neglect M = 0.22; SD = 0.415 | 1 | - | - | - | - | - | - | - | - | - |
| 2. Emotional abuse M = 0.16; SD = 0.6 | 0.346 ** | 1 | - | - | - | - | - | - | - | - |
| 3. Physical neglect M = 0.12; SD = 0.323 | 0.577 ** | 0.213 | 1 | - | - | - | - | - | - | - |
| 4. Physical abuse M = 0.26; SD = 0.442 | 0.327 ** | 0.463 ** | 0.300 * | 1 | - | - | - | - | - | - |
| 5. Sexual abuse M = 0.12; SD = 0.32 | 0.136 | 0.211 | 0.008 | −0.012 | 1 | - | - | - | - | - |
| 6. Substance abuse M = 0.22; SD = 0.41 | 0.319 ** | 0.154 | 0.138 | 0.087 | 0.266 * | 1 | - | - | - | - |
| 7. Mental health pr. M = 0.33; SD = 0.47 | 0.075 | 0.112 | 0.032 | 0.070 | 0.040 | 0.298 * | 1 | - | - | - |
| 8. Witness violence M = 0.2; SD = 0.46 | 0.059 | 0.213 | 0.145 | 0.435 ** | −0.150 | 0.199 | −0.054 | 1 | - | - |
| 9. Incarceration M = 0.03; SD = 0.169 | 0.328 ** | 0.397 ** | 0.477 ** | 0.094 | 0.207 | 0.118 | 0.244 * | 0.126 | 1 | - |
| 10. Divorce M = 0.64 SD = 0.484 | 0.251 * | 0.164 | 0.179 | 0.242 * | −0.006 | 0.178 | 0.021 | 0.049 | −0.049 | 1 |
| Significant Living Characteristics | Significant Child Characteristics |
|---|---|
| Parents in debt | Attachment related problems/disorders |
| ACEs in parents | Trauma- and stressor- related disorders |
| Mother with ID | Number of placements in residential care or foster care homes |
| Parent experiencing limited parenting competence | Sexual risk taking behavior |
| A parent in contact with justice (incarceration | Rule-breaking behavior (CBCL) |
| excluded) | Thought problems (CBCL) |
| Problematic caregiver-child relationship | Somatic complaints (CBCL) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vervoort-Schel, J.; Mercera, G.; Wissink, I.; Mink, E.; Van der Helm, P.; Lindauer, R.; Moonen, X. Adverse Childhood Experiences in Children with Intellectual Disabilities: An Exploratory Case-File Study in Dutch Residential Care. Int. J. Environ. Res. Public Health 2018, 15, 2136. https://doi.org/10.3390/ijerph15102136
Vervoort-Schel J, Mercera G, Wissink I, Mink E, Van der Helm P, Lindauer R, Moonen X. Adverse Childhood Experiences in Children with Intellectual Disabilities: An Exploratory Case-File Study in Dutch Residential Care. International Journal of Environmental Research and Public Health. 2018; 15(10):2136. https://doi.org/10.3390/ijerph15102136
Chicago/Turabian StyleVervoort-Schel, Jessica, Gabriëlle Mercera, Inge Wissink, Emmelie Mink, Peer Van der Helm, Ramón Lindauer, and Xavier Moonen. 2018. "Adverse Childhood Experiences in Children with Intellectual Disabilities: An Exploratory Case-File Study in Dutch Residential Care" International Journal of Environmental Research and Public Health 15, no. 10: 2136. https://doi.org/10.3390/ijerph15102136
APA StyleVervoort-Schel, J., Mercera, G., Wissink, I., Mink, E., Van der Helm, P., Lindauer, R., & Moonen, X. (2018). Adverse Childhood Experiences in Children with Intellectual Disabilities: An Exploratory Case-File Study in Dutch Residential Care. International Journal of Environmental Research and Public Health, 15(10), 2136. https://doi.org/10.3390/ijerph15102136






