Effectiveness, Feasibility, and Acceptability of Dynamic Elastomeric Fabric Orthoses (DEFO) for Managing Pain, Functional Capacity, and Quality of Life during Prenatal and Postnatal Care: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Identification of Studies
2.2. Screening and Selection Procedures
- Full text articles published in English or articles that could be translated into English.
- Published between January 2000 and April 2019.
- Constituted a report of a study with one of the following designs: randomized controlled trials, clinical controlled trials, prospective cohort studies, quasi-experimental studies, pilot studies, cross-sectional studies, single case studies.
- Study participants included women between the ages of 18–50 of any race or socioeconomic status in specified prenatal or postnatal periods as follows. Specifically, in prenatal studies, women were to be between 12–40 gestational weeks, and in postnatal studies, the study population needed to be immediately and/or up to 12 months postpartum.
- Investigated the effectiveness, the feasibility, or the acceptability of DEFO/compression garments for addressing physiological, psychological, and/or social outcomes including pain (pelvic, low back/lumbar or vulval regions), functional capacity, and quality of life.
- Compression garment location, style, and grade must include continuous contact with the torso and/or the pelvic region and the genital region, the perineum, and the thigh to be consistent with a DEFO.
- Studies investigating women in the prenatal phase who experienced: Rectus Diastasis ≥6 cm, complications or co-morbidities such as preeclampsia, eclampsia, venous thrombus/deep vein thrombosis, thrombophlebitis, bleeding of the varicose vein, pulmonary embolism, vaginal/rectal prolapse, or an intellectual or mental impairment.
- Studies investigating women in the postnatal phase who experienced: wound infection, severe haemorrhaging, infection, Rectus Diastasis ≥6 cm, complications or co-morbidities such as preeclampsia, eclampsia, venous thrombus/deep vein thrombosis, thrombophlebitis, bleeding of the varicose vein, pulmonary embolism, vaginal/rectal prolapse, or an intellectual or mental impairment.
- Studies investigating women who had surgical management other than caesarean section or episiotomy in prenatal or postnatal care.
2.3. Critical Appraisal of Methodological Quality
2.4. Data Extraction
2.5. Synthesis
3. Results
3.1. Included Studies and Participant Characteristics
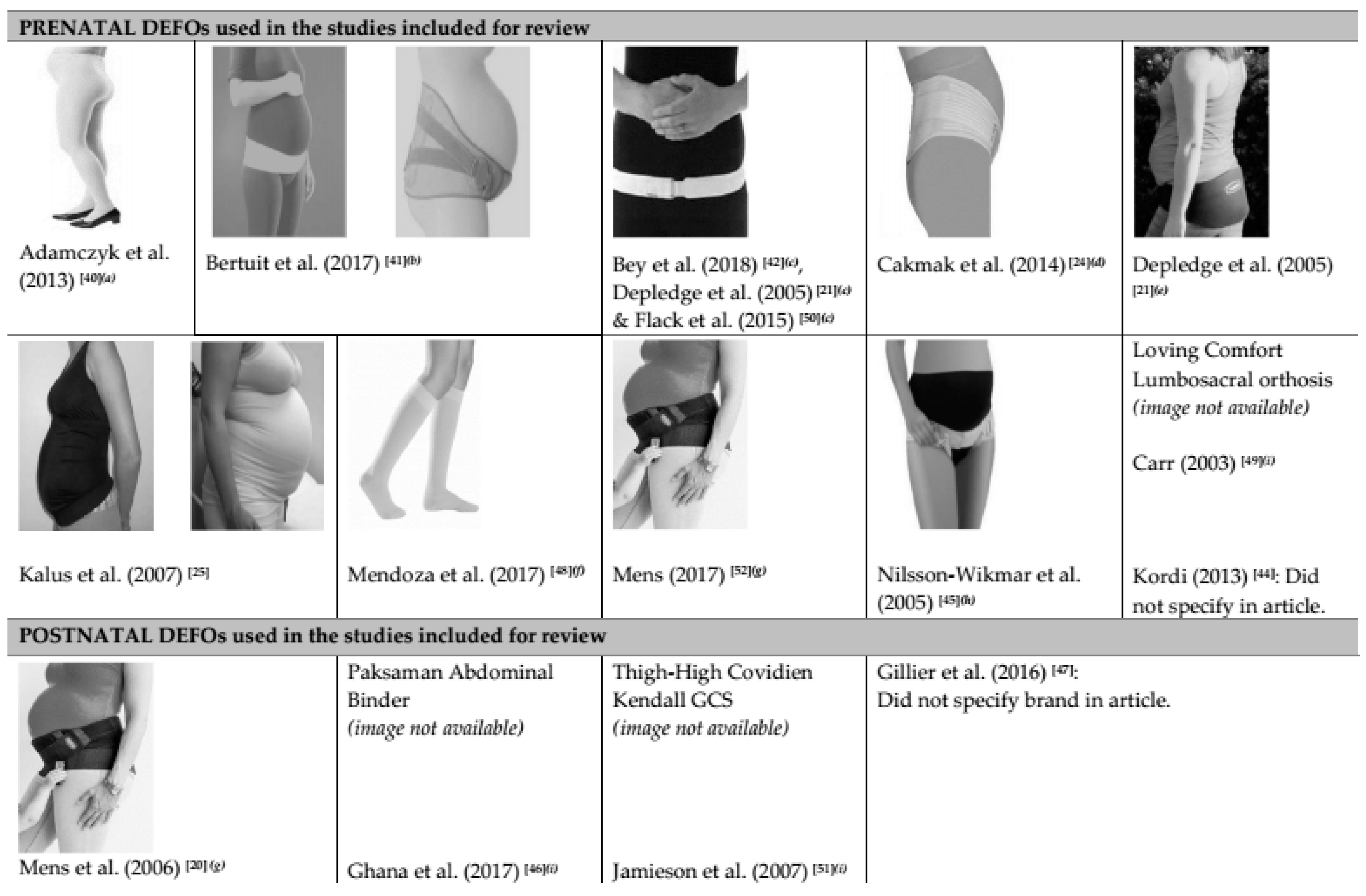
3.2. DEFO Investigated in the Included Studies
3.3. Ailments that DEFOs were Used to Treat during Prenatal and Postnatal Care
3.4. Methodological Quality of Included Studies
3.5. Aim 1 (Prenatal): Effectiveness of Using DEFO in Prenatal Care to Manage and/or Improve Pain, Functional Capacity, and Quality of Life
3.5.1. Effectiveness of Using DEFO in Prenatal Care to Manage and/or Improve Pain
3.5.2. Effectiveness of Using DEFO in Prenatal Care to Manage and/or Improve Functional Capacity
3.5.3. Effectiveness of Using DEFO in Prenatal Care to Manage and/or Improve Quality of Life
3.6. Aim 1 (Postnatal): Effectiveness of Using DEFO in Postnatal Care to Manage and/or Improve Pain, Functional Capacity, and Quality of Life
3.6.1. Effectiveness of Using DEFO in Postnatal Care to Manage and/or Improve Pain
3.6.2. Effectiveness of Using DEFO in Postnatal Care to Manage and/or Improve Functional Capacity
3.6.3. Effectiveness of Using DEFO in Postnatal Care to Manage and/or Improve Quality of Life
3.7. Aim 2: Feasibility, and Acceptability of Using DEFO in Prenatal and Postnatal Care
3.7.1. Feasibility and Acceptability of Using DEFO in Prenatal Care
3.7.2. Feasibility and Acceptability of Using DEFO in Postnatal Care
4. Discussion
4.1. Overview of Findings
4.2. Aim 1: Effectiveness of Using DEFO’s in Prenatal and Postnatal Care to Manage and/or Improve Pain, Functional Capacity, and Quality of Life
4.3. Aim 2: Feasibility and Acceptability of Using DEFOs in Prenatal and Postnatal Care
4.4. Strengths and Limitations of the Review
5. Conclusions
Clinical and Research Implications
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Fitzgerald, C.M.; Mallinson, T. The association between pelvic girdle pain and pelvic floor muscle function in pregnancy. Int. Urogynecol. J. 2012, 23, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.S.M.; Yu, W.W.M.; Lao, T.T.; Chow, D.H.K.; Chung, J.W.Y.; Li, Y. Effectiveness of maternity support belts in reducing low back pain during pregnancy: A review. J. Clin. Nurs. 2009, 18, 1523–1532. [Google Scholar] [CrossRef] [PubMed]
- Ninia, J.G.; Goldberg, T.L. Treatment of vulvar varicosities by injection—Compression sclerotherapy and a pelvic supporter. Obstet. Gynaecol. 1996, 87, 786–788. [Google Scholar] [CrossRef]
- Liddle, S.D.; Pennick, V. Interventions for preventing and treating low-back and pelvic pain during pregnancy. Cochrane Database Syst. Rev. 2015, 10, CD001066. [Google Scholar] [CrossRef] [PubMed]
- Close, C.; Sinclair, M.; Liddle, D.; McCullough, J.; Hughes, C. Women’s experience of low back and/or pelvic pain (LBPP) during pregnancy. Midwifery 2016, 37, 1–8. [Google Scholar] [CrossRef]
- Howell, E.R. Pregnancy-related symphysis pubis dysfunction management and postpartum rehabilitation: Two case reports. J. Can. Chiropr. Assoc. 2012, 56, 102–111. [Google Scholar] [PubMed]
- Persson, M.; Winkvist, A.; Dahlgreen, L.; Mogren, I. Struggling with daily life and enduring pain: A qualitative study of the experience of pregnant women living with chronic pelvic pain. BMC Pregnancy Childbirth 2013, 13, 111. [Google Scholar] [CrossRef]
- Bjelland, E.; Stuge, B.; Vangen, S.; Stray-Pedersen, B.; Eberhard-Gran, M. Mode of delivery and persistence of pelvic girdle syndrome 6 months postpartum. Am. J. Obstet. Gynecol. 2013, 208, 298.e1–298.e7. [Google Scholar] [CrossRef]
- Brown, S.; Lumley, J. Maternal health after childbirth: Results of an Australian population-based survey. BJOG Int. J. Obstet. Gynaecol. 1998, 105, 156–161. [Google Scholar] [CrossRef]
- Leeman, L.; Fullilove, A.M.; Borders, N.; Rogers, R.G. Postpartum Perineal Pain in a Low Episiotomy Setting: Association with Severity of Genital Trauma, Labor Care and Birth Variables. Birth 2009, 36, 283–288. [Google Scholar] [CrossRef]
- Mogren, I. Does caesarean section negatively influence the post-partum prognosis of low back pain and pelvic pain during pregnancy? Eur. Spine J. 2007, 16, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Woolhouse, H.; Perlen, S.; Gartland, D.; Brown, S.J. Physical Health and Recovery in the First 18 Months Postpartum: Does Cesarean Section Reduce Long-Term Morbidity? Birth 2012, 39, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Ramelet, A. Compression Therapy. Dermatol. Surg. 2002, 28, 6–10. [Google Scholar] [PubMed]
- O’Meara, S.; Cullum, N.; Nelson, E.A.; Dumville, J.C. Compression for venous leg ulcers. Cochrane Database Syst. Rev. 2012, 11. [Google Scholar] [CrossRef]
- Dittmier, D.; Teasell, R. Complications of Immobilization and Part 1: Musculoskeletal and Cardiovascular Complications. Can. Fam. Physician 1993, 39, 1428–1437. [Google Scholar]
- Senthil, K.; Eva, C. Pregnancy-related low back pain or gestational back pain: Too complex to handle or too simple to ignore? Indian J. Obstet. Gynecol. 2013, 1, 87–89. [Google Scholar]
- Ho, S.S.; Yu, W.; Lao, T.T.; Chow, D.H.K.; Chung, J.W.; Li, Y. Comfort evaluation of maternity support garments in a wear trial. Ergonomics 2008, 51, 1376–1393. [Google Scholar] [CrossRef] [PubMed]
- Richards, E.; van Kessel, G.; Virgara, R.; Harris, P. Does antenatal physical therapy for pregnant women with low back pain or pelvic pain improve functional outcomes? A systematic review. ACTA Obstet. Gynecol. Scand. 2012, 91, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.S.M.; Yu, W.W.M.; Lao, T.T.; Chow, D.H.K.; Chung, J.W.Y.; Li, Y. Garment needs of pregnant women based on content analysis of in-depth interviews. J. Clin. Nurs. 2009, 18, 2426–2435. [Google Scholar] [CrossRef]
- Mens, J.M.A.; Damen, L.; Snijders, C.J.; Stam, H.J. The mechanical effect of a pelvic belt in patients with pregnancy-related pelvic pain. Clin. Biomech. 2006, 21, 122–127. [Google Scholar] [CrossRef]
- Depledge, J.; McNair, P.J.; Keal-Smith, C.; Williams, M. Management of Symphysis Pubis Dysfunction During Pregnancy Using Exercise and Pelvic Support Belts. Phys. Ther. 2005, 85, 1290–1300. [Google Scholar] [PubMed] [Green Version]
- Vleeming, A.; Albert, H.B.; Ostgaard, H.C.; Sturesson, B.; Stuge, B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. Spine J. 2008, 17, 794–819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, J.W.; Skaggs, C.D.; Thompson, P.A.; Nelson, M.; Gavard, J.A.; Gross, G.A. A randomized controlled trial comparing a multimodal intervention and standard obstetrics care for low back and pelvic pain in pregnancy. Am. J. Obstet. Gynecol. 2013, 208, 295.e1–295.e7. [Google Scholar] [CrossRef] [PubMed]
- Cakmak, B.; Inanir, A.; Nacar, M.C.; Filiz, B. The Effect of Maternity Support Belts on Postural Balance in Pregnancy. Am. Acad. Phys. Med. Rehabil. 2014, 6, 624–628. [Google Scholar] [CrossRef] [PubMed]
- Kalus, S.M.; Kornman, L.H.; Quinlivan, J.A. Managing back pain in pregnancy using a support garment: A randomised trial. Br. J. Obstet. Gynaecol. 2007, 115, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Sawle, L.; Freeman, J.; Marsden, J. The use of a dynamic elastomeric fabric orthosis (DEFO) in supporting the management of athletic pelvic and groin injury. J. Sport Rehabil. 2015, 25, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, T.; Anderson, G.S. Influence of moderate prophylactic compression on sport performance. J. Strength Cond. Res. 2005, 19, 292–297. [Google Scholar] [PubMed]
- MacRae, B.A.; Laing, R.M.; Niven, B.E.; Cotter, J.D. Pressure and coverage effects of sporting compression garments on cardiovascular function, thermoregulatory function, and exercise performance. Eur. J. Appl. Physiol. 2012, 112, 1783–1795. [Google Scholar] [CrossRef]
- Candlier, C.; Bird, A.; Woodcock, D. An audit into the management of pregnancy-related pelvic girdle pain. J. Assoc. Chart. Physiother. Women’s Health 2011, 108, 18–19. [Google Scholar]
- Pierce, H.; Homer, C.S.E.; Dahlen, H.G.; King, J. Pregnancy-related lumbopelvic pain: Listening to Australian women. Nurs. Res. Pract. 2012, 387428. [Google Scholar] [CrossRef]
- Centre for Reviews and Dissemination (CRD). Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care; York Publishing Services Limited: York, UK, 2009. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyse: The PRISMA statement. BMJ 2009, 339, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Clarivate Analytics. EndNote (Version X8) (Reference Management Software). 2018. Available online: https://endnote.com (accessed on 10 May 2019).
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality of both randomized and non-randomized studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Armijo Olivo, S.; Macedo, L.G.; Gadotti, I.C.; Fuentes, J.; Stanton, T.; Magee, D.J. Scales to Assess the Quality of Randomized Controlled Trials: A Systematic Review. Phys. Ther. 2008, 88, 156–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jäkel, A.; von Haunschild, P. Therapeutic effects of cranial osteopathic manipulative medicine: A systematic review. J. Am. Osteopath. Assoc. 2011, 111, 685–693. [Google Scholar] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Leary, H.; Walker, A. Meta-analysis and meta-synthesis methodologies: Rigorously piecing together research. TechTrends 2018, 62, 525–534. [Google Scholar] [CrossRef]
- Cliff, D.P.; Hesketh, K.D.; Vella, S.A.; Hinkley, T.; Tsiros, M.D.; Ridgers, N.D.; Carver, A.; Veitch, J.; Parrish, A.M.; Hardy, L.L.; et al. Objectively measured sedentary behaviour and health development in children and adolescents: Systematic review and meta-analysis. Obes. Rev. 2016, 17, 330–344. [Google Scholar] [CrossRef]
- Adamczyk, A.; Krug, M.; Schnabl, S.; Häfner, H.M. Compression therapy during pregnancy: Bane or boom? Phlebologie 2013, 42, 301–307. [Google Scholar] [CrossRef]
- Bertuit, J.; Van Lint, C.E.; Rooze, M.; Feipel, V. Pregnancy and pelvic girdle pain: Analysis of pelvic belt on pain. J. Clin. Nurs. 2018, 27, e129–e137. [Google Scholar] [CrossRef]
- Bey, M.E.; Arampatzis, A.; Legerlotz, K. The effect of a maternity support belt on static stability and posture in pregnant and non-pregnant women. J. Biomech. 2018, 75, 123–128. [Google Scholar] [CrossRef]
- Cameron, L.; Marsden, J.; Watkins, K.; Freeman, J. Management of antenatal pelvic girdle pain study (MAPS): A double blinded randomised trial evaluating the effectiveness of two pelvic orthoses. Int. J. Women’s Health Care 2018, 3, 1–9. [Google Scholar]
- Kordi, R.; Abolhasani, M.; Rostami, M.; Hantoushzadeh, S.; Mansournia, M.A.; Vasheghani-Farahani, F. Comparison between the effect of lumbopelvic belt and home-based pelvic stabilizing exercise on pregnant women with pelvic girdle pain; a randomized controlled trial. J. Back Musculoskelet. Rehabil. 2013, 26, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Nilsson-Wikmar, L.; Holm, K.; Öijerstedt, R.; Harms-Ringdahl, K. Effect of three different physical therapy treatments on pain and activity in pregnant women with pelvic girdle pain: A randomized clinical trial with 3, 6, and 12 months follow-up postpartum. Spine 2005, 30, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Ghana, S.; Hakimi, S.; Mirghasfourvand, M.; Abbasalizadeh, F.; Behnampour, N. Randomised controlled trial of abdominal binders for postoperative pain, distress, and blood loss after caesarean delivery. Int. J. Gynecol. Obstet. 2017, 137, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Gillier, C.M.; Sparks, J.R.; Kriner, R.; Anasti, J.N. A randomised controlled trial of abdominal binders for the management of postoperative pain and distress after caesarean delivery. Int. J. Gynecol. Obstet. 2016, 133, 188–191. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, E.; Amsler, F. A randomized crossover trial on the effect of compression stockings on nausea and vomiting in early pregnancy. Int. J. Women’s Health 2017, 9, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Carr, C.A. Use of a Maternity Support Binder for Relief of Pregnancy-Related Back Pain. J. Obstet. Gynecol. Neonatal Nurs. 2003, 32, 495–502. [Google Scholar] [CrossRef]
- Flack, N.A.M.S.; Hay-Smith, E.J.C.; Stringer, M.D.; Gray, A.R.; Woodley, S.J. Adherence, tolerance and effectiveness of two different pelvic support belts as a treatment for pregnancy-related symphyseal pain—A pilot randomized trial. BMC Pregnancy Childbirth 2015, 15, 36. [Google Scholar] [CrossRef]
- Jamieson, R.; Calderwood, C.H.; Greer, I.A. The effect of graduated compression stockings on blood velcoty in the deep venous system of the lower limb in the postnatal period. BJOG Int. J. Obstet. Gynecol. 2007, 114, 1292–1294. [Google Scholar] [CrossRef]
- Mens, J. Does a pelvic belt reduce hip adduction weakness in pregnancy-related posterior pelvic girdle pain? A case-control study. Eur. J. Phys. Rehabil. Med. 2017, 53, 575–581. [Google Scholar] [CrossRef]
- Gutke, A.; Betten, C.; Degerskär, K.; Pousette, S.; Olsén, M.F. Treatments for pregnancy-related lumbopelvic pain: A systematic review of physiotherapy modalities. Acta Obstet. Gynecol. Scand. 2015, 94, 1156–1168. [Google Scholar] [CrossRef] [PubMed]
- Noren, L.; Ostgaard, S.; Johansson, G.; Ostgaard, H.C. Lumbar back and posterior pelvic pain during pregnancy: A 3-year follow-up. Eur. Spine J. 2002, 11, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.M.; DeZinno, P.; Fermo, L.; William, K.; Caldwell-Andrews, A.A.; Bravemen, F. Complementary and Alternative Medicine for Low-Back Pain in Pregnancy: A Cross-Sectional Survey. J. Altern. Complement. Med. 2005, 11, 459–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| All Studies Included | ||||
|---|---|---|---|---|
| Variable | Significant Effect n | Non-Significant Effect n | Summary of Coding | |
| n/Na (%) for Variable | DEFO b Effect (+/−,0,?) c | |||
| Prenatal Studies | ||||
| Pain | 9 [21,25,41,43,44,45,49,50,52] | 0 | 9/9 (100.0) | + |
| Functional Capacity | 15 [21,24,25,40,41,42,43,44,45,49,50,52] | 3 [24,42,43] | 15/18 (83.3) | + |
| Quality of Life | 7 [40,43,44,48] | 1 [25] | 7/8 (87.5) | + |
| Postnatal Studies | ||||
| Pain | 2 [46,47] | 0 | 2/2 (100.0) | ? |
| Functional Capacity | 5 [20,46,51] | 1 [46] | 5/6 (83.3) | + |
| Quality of Life | 2 [46,47] | 0 | 2/2 (100.0) | ? |
| Studies of Moderate to Strong Quality Included Only d | ||||
| Variable | Significant Effect n | Non-Significant Effect n | Summary of Coding | |
| n/Na (%) for Variable | DEFO b Effect (+/−,0,?) c | |||
| Prenatal Studies | ||||
| Pain | 9 [21,25,41,43,44,45,49,50,52] | 0 | 9/9 (100.0) | + |
| Functional Capacity | 11 [21,25,41,42,43,44,45,49,50,52] | 2 [42,43] | 11/13 (84.6) | + |
| Quality of Life | 6 [43,44,48] | 1 [25] | 6/7 (85.7) | + |
| Postnatal Studies | ||||
| Pain | 2 [46,47] | 0 | 2/2 (100.0) | ? |
| Functional Capacity | 2 [46,51] | 1 [46] | 2/3 (66.7) | ? |
| Quality of Life | 2 [46,47] | 0 | 2/2 (100.0) | ? |
| Randomised Control Trials Included Only | ||||
| Significant Effect n | Non-Significant Effect n | Summary of Coding | ||
| n/Na (%) for Variable | DEFO b Effect (+/−,0,?) c | |||
| Prenatal Studies | ||||
| Pain | 6 [21,25,41,43,44,45] | 0 | 4/6 (66.7) | + |
| Functional Capacity | 7 [21,25,41,42,43,44,45] | 2 [21,43] | 7/9 (77.7) | + |
| Quality of Life | 3 [40,43,44] | 1 [25] | 3/4 (75.0) | ? |
| Postnatal Studies | ||||
| Pain | 2 [46,47] | 0 | 2/2 (100.0) | ? |
| Functional Capacity | 1 [46] | 1 [46] | 1/2 (50.0) | ? |
| Quality of Life | 2 [46,47] | 0 | 2/2 (100.0) | ? |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szkwara, J.M.; Milne, N.; Hing, W.; Pope, R. Effectiveness, Feasibility, and Acceptability of Dynamic Elastomeric Fabric Orthoses (DEFO) for Managing Pain, Functional Capacity, and Quality of Life during Prenatal and Postnatal Care: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 2408. https://doi.org/10.3390/ijerph16132408
Szkwara JM, Milne N, Hing W, Pope R. Effectiveness, Feasibility, and Acceptability of Dynamic Elastomeric Fabric Orthoses (DEFO) for Managing Pain, Functional Capacity, and Quality of Life during Prenatal and Postnatal Care: A Systematic Review. International Journal of Environmental Research and Public Health. 2019; 16(13):2408. https://doi.org/10.3390/ijerph16132408
Chicago/Turabian StyleSzkwara, Jaclyn M., Nikki Milne, Wayne Hing, and Rodney Pope. 2019. "Effectiveness, Feasibility, and Acceptability of Dynamic Elastomeric Fabric Orthoses (DEFO) for Managing Pain, Functional Capacity, and Quality of Life during Prenatal and Postnatal Care: A Systematic Review" International Journal of Environmental Research and Public Health 16, no. 13: 2408. https://doi.org/10.3390/ijerph16132408
APA StyleSzkwara, J. M., Milne, N., Hing, W., & Pope, R. (2019). Effectiveness, Feasibility, and Acceptability of Dynamic Elastomeric Fabric Orthoses (DEFO) for Managing Pain, Functional Capacity, and Quality of Life during Prenatal and Postnatal Care: A Systematic Review. International Journal of Environmental Research and Public Health, 16(13), 2408. https://doi.org/10.3390/ijerph16132408






