Basic Life-Support Learning in Undergraduate Students of Sports Sciences: Efficacy of 150 Minutes of Training and Retention after Eight Months
Abstract
:1. Introduction
2. Materials and Methods
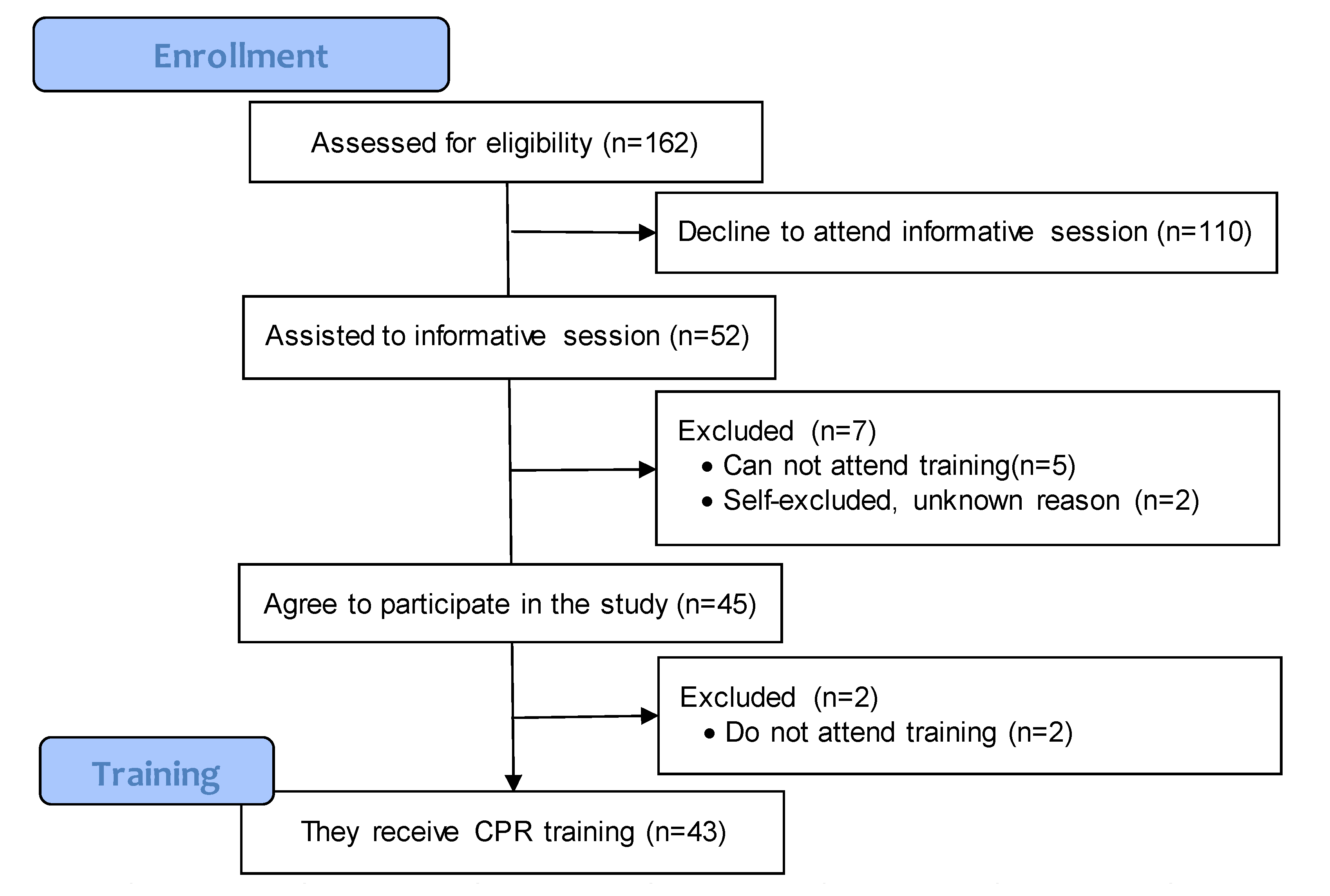
2.1. Participants
2.2. Study Design
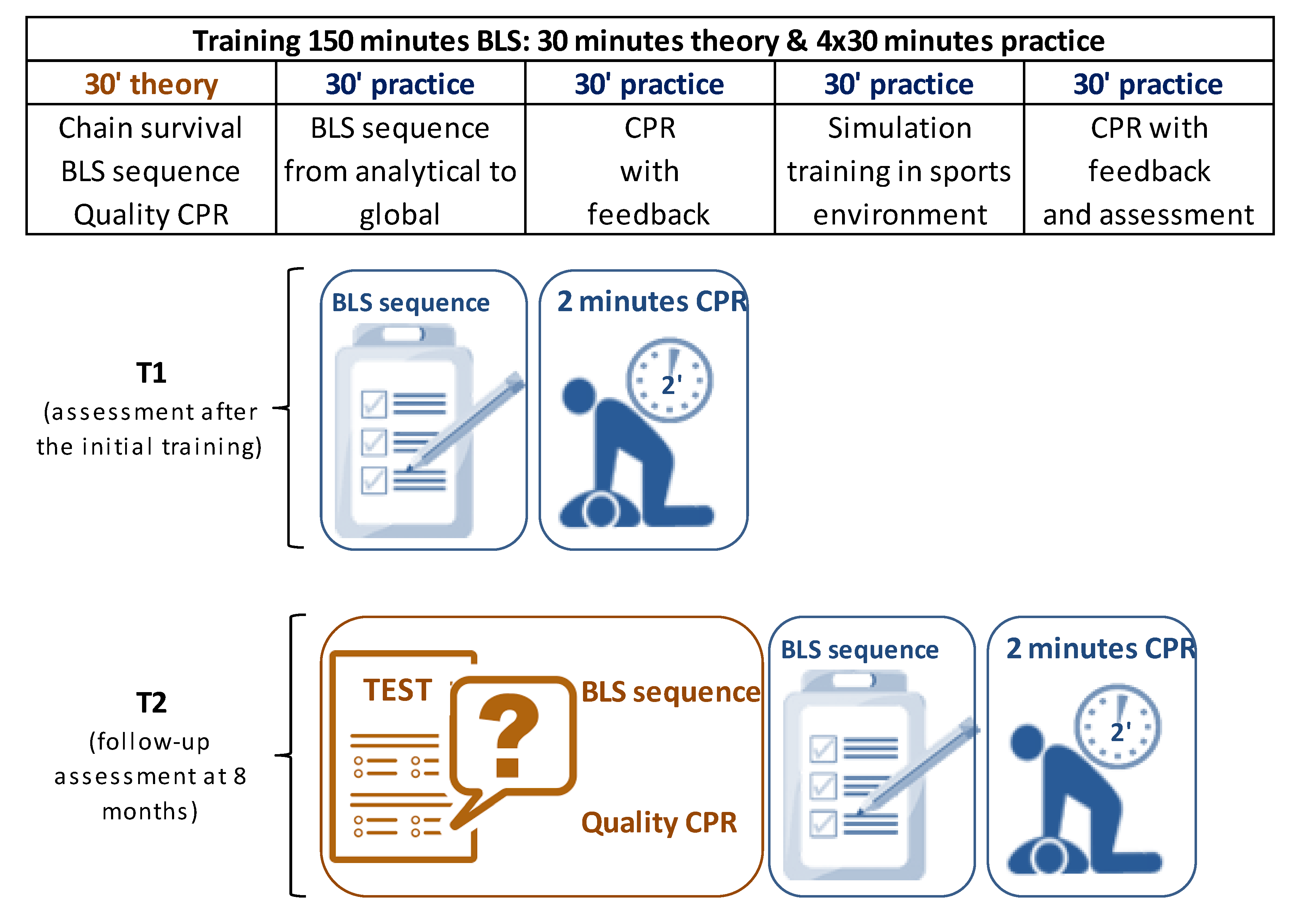
2.3. Training
2.4. Procedure, Assessments and Variables
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
3.1. Basic Life Support Learning
3.2. Basic Life-Support Retention
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gräsner, J.T.; Bossaert, L. Epidemiology and management of cardiac arrest: What registries are revealing. Best Pract. Res. Clin. Anaesthesiol. 2013, 27, 293–306. [Google Scholar] [CrossRef]
- Nolan, J.P.; Hazinski, M.F.; Aickin, R.; Bhanji, F.; Billi, J.E.; Callaway, C.W.; Gent, L.M. Part 1: Executive summary: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2015, 95, e1–e31. [Google Scholar] [CrossRef]
- Catalunya. Llei 3/2008, de 23 D’abril, de L’Exercici de les Professions de L’espor; DOGC, 02/05/2008, núm. 5123; Butlletí Oficial del Parlament de Catalunya: Barcelona Spain, 2008; pp. 34361–34378. [Google Scholar]
- Extremadura. Ley 15/2015, de 16 De Abril, Por la Que se Ordena el Ejercicio de las Profesiones del Deporte en Extremadura; BOE, 19/05/2015, núm. 119; Boletín Oficial de Extremadura: Extremadura, Spain, 2015; pp. 42417–42436. [Google Scholar]
- Papalexopoulou, K.; Chalkias, A.; Dontas, I.; Pliatsika, P.; Giannakakos, C.; Papapanagiotou, P.; Xanthos, T. Education and age affect skill acquisition and retention in lay rescuers after a European Resuscitation Council CPR/AED course. Heart Lung 2014, 43, 66–71. [Google Scholar] [CrossRef]
- Niles, D.E.; Nishisaki, A.; Sutton, R.M.; Elci, O.U.; Meaney, P.A.; O’Connor, K.A.; Nadkarni, V. Improved Retention of Chest Compression Psychomotor Skills with Brief “Rolling Refresher” Training. Simul. Healthc. 2017, 12, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Schexnayder, S.M. CPR Education. Curr. Pediatr. Rev. 2013, 9, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.Y.; Ko, Y.C.; Hsieh, M.J.; Chiang, W.C.; Ma, M.H.M. Interventions to improve the quality of bystander cardiopulmonary resuscitation: A systematic review. PLoS ONE 2019, 14, e0211792. [Google Scholar] [CrossRef] [PubMed]
- Yeung, J.; Meeks, R.; Edelson, D.; Gao, F.; Soar, J.; Perkins, G.D. The use of CPR feedback/prompt devices during training and CPR performance: A systematic review. Resuscitation 2009, 80, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, R. Nurses’ knowledge and skill retention following cardiopulmonary resuscitation training: A review of the literature. J. Adv. Nurs. 2005, 51, 288–297. [Google Scholar] [CrossRef]
- Perkins, G.D. Simulation in resuscitation training. Resuscitation 2007, 73, 202–311. [Google Scholar] [CrossRef]
- Anderson, R.; Sebaldt, A.; Lin, Y.; Cheng, A. Optimal training frequency for acquisition and retention of high-quality CPR skills: A randomized trial. Resuscitation 2019, 135, 153–161. [Google Scholar] [CrossRef]
- Hsieh, M.-J.; Chiang, W.-C.; Jan, C.-F.; Lin, H.-Y.; Yang, C.-W.; Ma, M.H.-M. The effect of different retraining intervals on the skill performance of cardiopulmonary resuscitation in laypeople-A three-armed randomized control study. Resuscitation 2018, 128, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Roppolo, L.P.; Pepe, P.E.; Campbell, L.; Ohman, K.; Kulkarni, H.; Miller, R.; Idris, A.H. Prospective, randomized trial of the effectiveness and retention of 30-min layperson training for cardiopulmonary resuscitation and automated external defibrillators: The American Airlines Study. Resuscitation 2007, 74, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.K.; Gilcreast, D.; Pierce, K. Evaluation of staff’s retention of ACLS and BLS skills. Resuscitation 2008, 78, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Woollard, M.; Whitfield, R.; Newcombe, R.G.; Colquhoun, M.; Vetter, N.; Chamberlain, D. Optimal refresher training intervals for AED and CPR skills: A randomised controlled trial. Resuscitation 2006, 71, 237–247. [Google Scholar] [CrossRef]
- Woollard, M.; Whitfield, R.; Smith, A.; Colquhoun, M.; Newcombe, R.G.; Vetter, N.; Chamberlain, D. Skill acquisition and retention in automated external defibrillator (AED) use and CPR by lay responders: A prospective study. Resuscitation 2004, 60, 17–28. [Google Scholar] [CrossRef]
- González-Salvado, V.; Abelairas-Gómez, C.; Peña-Gil, C.; Neiro-Rey, C.; Barcala-Furelos, R.; González-Juanatey, J.R.; Rodríguez-Núñez, A. Basic life support training into cardiac rehabilitation programs: A chance to give back. A community intervention controlled manikin study. Resuscitation 2018, 127, 14–20. [Google Scholar]
- Méndez-Martínez, C.; Martínez-Isasi, S.; García-Suárez, M.; Peña-Rodríguez, M.A.D.; Gómez-Salgado, J.; Fernández-García, D. Acquisition of Knowledge and Practical Skills after a Brief Course of BLS-AED in First-Year Students in Nursing and Physiotherapy at a Spanish University. Int. J. Environ. Res. Public Health 2019, 16, 766. [Google Scholar] [CrossRef]
- Bjørnshave, K.; Krogh, L.Q.; Hansen, S.B.; Nebsbjerg, M.A.; Thim, T.; Løfgren, B. Teaching basic life support with an automated external defibrillator using the two-stage or the four-stage teaching technique. Eur. J. Emerg. Med. 2018, 25, 18–24. [Google Scholar] [CrossRef]
- Perkins, G.; Colquhoun, M.; Simons, R. Training manikins. In ABC of Resuscitation, 5th ed.; Colquhoun, M., Handley, A., Evans, T., Eds.; BMJ Books: London, UK, 2004; pp. 97–101. [Google Scholar]
- Mpotos, N.; De Wever, B.; Cleymans, N.; Raemaekers, J.; Loeys, T.; Herregods, L.; Monsieurs, K.G. Repetitive sessions of formative self-testing to refresh CPR skills: A randomised non-inferiority trial. Resuscitation 2014, 85, 1282–1286. [Google Scholar] [CrossRef]
- Castillo, J.; Gallart, A.; Rodríguez, E.; Castillo, J.; Gomar, C. Basic life support and external defibrillation competences after instruction and at 6 months comparing face-to-face and blended training. Randomised trial. Nurse Educ. Today 2018, 65, 232–238. [Google Scholar] [CrossRef]
- Saraç, L.; Ok, A. The effects of different instructional methods on students’ acquisition and retention of cardiopulmonary resuscitation skills. Resuscitation 2010, 81, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Cha, K.C.; Kim, H.J.; Shin, H.J.; Kim, H.; Lee, K.H.; Hwang, S.O. Hemodynamic effect of external chest compressions at the lower end of the sternum in cardiac arrest patients. J. Emerg. Med. 2013, 44, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Hellevuo, H.; Sainio, M.; Nevalainen, R.; Huhtala, H.; Olkkola, K.T.; Tenhunen, J.; Hoppu, S. Deeper chest compression—More complications for cardiac arrest patients? Resuscitation 2013, 84, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Stiell, I.G.; Brown, S.P.; Christenson, J.; Cheskes, S.; Nichol, G.; Powell, J.; Vaillancourt, C. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit. Care Med. 2012, 40, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Idris, A.H.; Guffey, D.; Pepe, P.E.; Brown, S.P.; Brooks, S.C.; Callaway, C.W.; Kudenchuk, P.J. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit. Care Med. 2015, 43, 840–848. [Google Scholar] [CrossRef]
- Ko, R.J.M.; Lim, S.H.; Wu, V.X.; Leong, T.Y.; Liaw, S.Y. Easy-to-learn cardiopulmonary resuscitation training programme: A randomised controlled trial on laypeople’s resuscitation performance. Singapore Med. J. 2018, 59, 217–223. [Google Scholar] [CrossRef]
- Allen, J.A.; Currey, J.; Considine, J. Annual resuscitation competency assessments: A review of the evidence. Aust. Crit. Care 2013, 26, 12–17. [Google Scholar] [CrossRef]
- Magill, R.; Anderson, D.I. Motor Learning and Control: Concepts and Applications, 10th ed.; McGraw-Hill: New York, NY, USA, 2014. [Google Scholar]
- Seidler, R.D. Multiple motor learning experiences enhance motor adaptability. J. Cogn. Neurosci. 2004, 16, 65–73. [Google Scholar] [CrossRef]
- Yaprak, P.; Güçlü, M.; Ayyildiz Durhan, T. The Happiness, Hardiness, and Humor Styles of Students with a Bachelor’s Degree in Sport Sciences. Behav. Sci. 2018, 8, 82. [Google Scholar] [CrossRef]
- Boet, S.; Bould, M.D.; Pigford, A.A.; Rössler, B.; Nambyiah, P.; Li, Q.; Schebesta, K. Retention of Basic Life Support in Laypeople: Mastery Learning vs. Time-based Education. Prehosp. Emerg. Care 2017, 21, 362–377. [Google Scholar] [CrossRef]

| CPR | BLS Checklist |
| Global CPR performance (%) | Checking for consciousness |
| Compression performance (%) | Opening the airway |
| Ventilation performance (%) | Checking for breathing |
| Compression depth (mm) | Calling 112 (emergency phone) for help |
| Compression: too shallow (%) | Starting CPR |
| Compression: adequate depth (%) | |
| Compression: too deep (%) | Resulting from the Questionnaire |
| Compression rate (compression/min) | Correct position of hands |
| Compression rate: too slow (%) | Correct depth of chest compression |
| Compression rate: adequate (%) | Correct frequency of chest compressions |
| Compression rate: too fast (%) | Correct proportion of compressions-ventilations |
| Ventilation volume (mL) | |
| Ventilation: too little volume (%) | Subjective perception (0–10) |
| Ventilation: adequate volume (%) | Competence performing CRP |
| Ventilation: too much volume (%) | Confidence performing CPR in a real OHCA |
| Hands-off time (s) | |
| Correct hand position (%) | |
| 30:2 cycles in 2 min (#) |
| Variables CPR | T1: Initial | T2: Follow-up | p Value a | t or Z b | Change | |||
|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | |||||
| Quality of CPR components | ||||||||
| Global CPR performance (%) | 72.5 | (20.1) | 64.3 | (29.1) | 0.323 | ↓ | 11.3% | |
| Compression performance (%) | 78.6 | (25.9) | 65.6 | (38.2) | 0.168 | ↓ | 16.5% | |
| Ventilation performance (%) | 69.9 | (30.1) | 60.1 | (35.2) | 0.399 | ↓ | 14.0% | |
| Compression depth | ||||||||
| Compression depth (mm) | 51.4 | (7.9) | 56.0 | (5.7) | 0.007 | −2.700 | ↑ | 8.1% |
| Too shallow (%) | 33.9 | (39.1) | 16.3 | (29.5) | 0.010 | −2.576 | ↓ | 51.9% |
| Adequate depth (%) | 66.1 | (39.1) | 83.7 | (29.5) | 0.010 | −2.576 | ↑ | 21.0% |
| Too deep (%) | 0.0 | (0.0) | 0.0 | (0.0) | 1.000 | 0.0% | ||
| Compression rate | ||||||||
| Compression rate (comp/min) c | 115.3 | (11.5) | 101.1 | (11.3) | <0.001 | 5.909 | ↓ | 12.3% |
| Too slow (%) | 12.7 | (27.0) | 49.4 | (43.5) | 0.001 | −3.219 | ↑ | 74.2% |
| Adequate rate (%) | 50.4 | (40.7) | 43.2 | (40.5) | 0.584 | ↓ | 14.3% | |
| Too fast (%) | 36.9 | (43.5) | 7.4 | (21.9) | 0.001 | −3.254 | ↓ | 79.8% |
| Ventilations | ||||||||
| Ventilation volume (ml) c | 663.7 | (319.0) | 657.1 | (364.7) | 0.934 | ↓ | 1.0% | |
| Too little volume (%) | 26.0 | (31.8) | 11.2 | (23.6) | 0.064 | ↓ | 56.9% | |
| Adequate volume (%) | 38.2 | (30.1) | 30.4 | (35.3) | 0.334 | ↓ | 20.5% | |
| Too much volume (%) | 35.8 | (38.6) | 45.4 | (41.6) | 0.379 | ↑ | 21.1% | |
| Others | ||||||||
| Hands-off time (seconds) | 7.5 | (2.1) | 6.0 | (1.7) | 0.001 | −3.216 | ↓ | 20.2% |
| Correct hand position (%) | 98.2 | (8.8) | 77.2 | (39.7) | 0.028 | −2.197 | ↓ | 21.3% |
| 30:2 cycles in 2 min (#) | 4.5 | (1.3) | 4.1 | (2.2) | 0.348 | ↓ | 9.6% | |
| CPR Variables in Participants with Global CPR Performance Scores <70% | T1: Initial Training | |
|---|---|---|
| Mean | (SD) | |
| Quality of CPR components | ||
| Global CPR performance (%) | 52.1 | (6.1) |
| Compression performance (%) | 54.7 | (9.0) |
| Ventilation performance (%) | 73.3 | (11.6) |
| Compression depth | ||
| Compression depth (mm) | 44.7 | (2.4) |
| Too shallow (%) | 67.4 | (12.6) |
| Adequate depth (%) | 32.6 | (12.6) |
| Too deep (%) | 0.0 | (0.0) |
| Compression rate | ||
| Compression rate (compression/min) | 115.7 | (4.6) |
| Too slow (%) | 13.6 | (10.8) |
| Adequate rate (%) | 52.1 | (15.8) |
| Too fast (%) | 34.3 | (15.8) |
| Ventilations | ||
| Ventilation volume (mL) | 537.0 | (95.0) |
| Too little volume (%) | 32.4 | (12.6) |
| Adequate volume (%) | 47.9 | (11.3) |
| Too much volume (%) | 19.7 | (11.2) |
| Others | ||
| Hands-off time (s) | 8.7 | (0.8) |
| Correct hand position (%) | 95.3 | (4.7) |
| 30:2 cycles in 2 min (#) | 4.1 | (0.5) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aranda-García, S.; Herrera-Pedroviejo, E.; Abelairas-Gómez, C. Basic Life-Support Learning in Undergraduate Students of Sports Sciences: Efficacy of 150 Minutes of Training and Retention after Eight Months. Int. J. Environ. Res. Public Health 2019, 16, 4771. https://doi.org/10.3390/ijerph16234771
Aranda-García S, Herrera-Pedroviejo E, Abelairas-Gómez C. Basic Life-Support Learning in Undergraduate Students of Sports Sciences: Efficacy of 150 Minutes of Training and Retention after Eight Months. International Journal of Environmental Research and Public Health. 2019; 16(23):4771. https://doi.org/10.3390/ijerph16234771
Chicago/Turabian StyleAranda-García, Silvia, Ernesto Herrera-Pedroviejo, and Cristian Abelairas-Gómez. 2019. "Basic Life-Support Learning in Undergraduate Students of Sports Sciences: Efficacy of 150 Minutes of Training and Retention after Eight Months" International Journal of Environmental Research and Public Health 16, no. 23: 4771. https://doi.org/10.3390/ijerph16234771
APA StyleAranda-García, S., Herrera-Pedroviejo, E., & Abelairas-Gómez, C. (2019). Basic Life-Support Learning in Undergraduate Students of Sports Sciences: Efficacy of 150 Minutes of Training and Retention after Eight Months. International Journal of Environmental Research and Public Health, 16(23), 4771. https://doi.org/10.3390/ijerph16234771





