Prevalence of Burnout in Medical and Surgical Residents: A Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
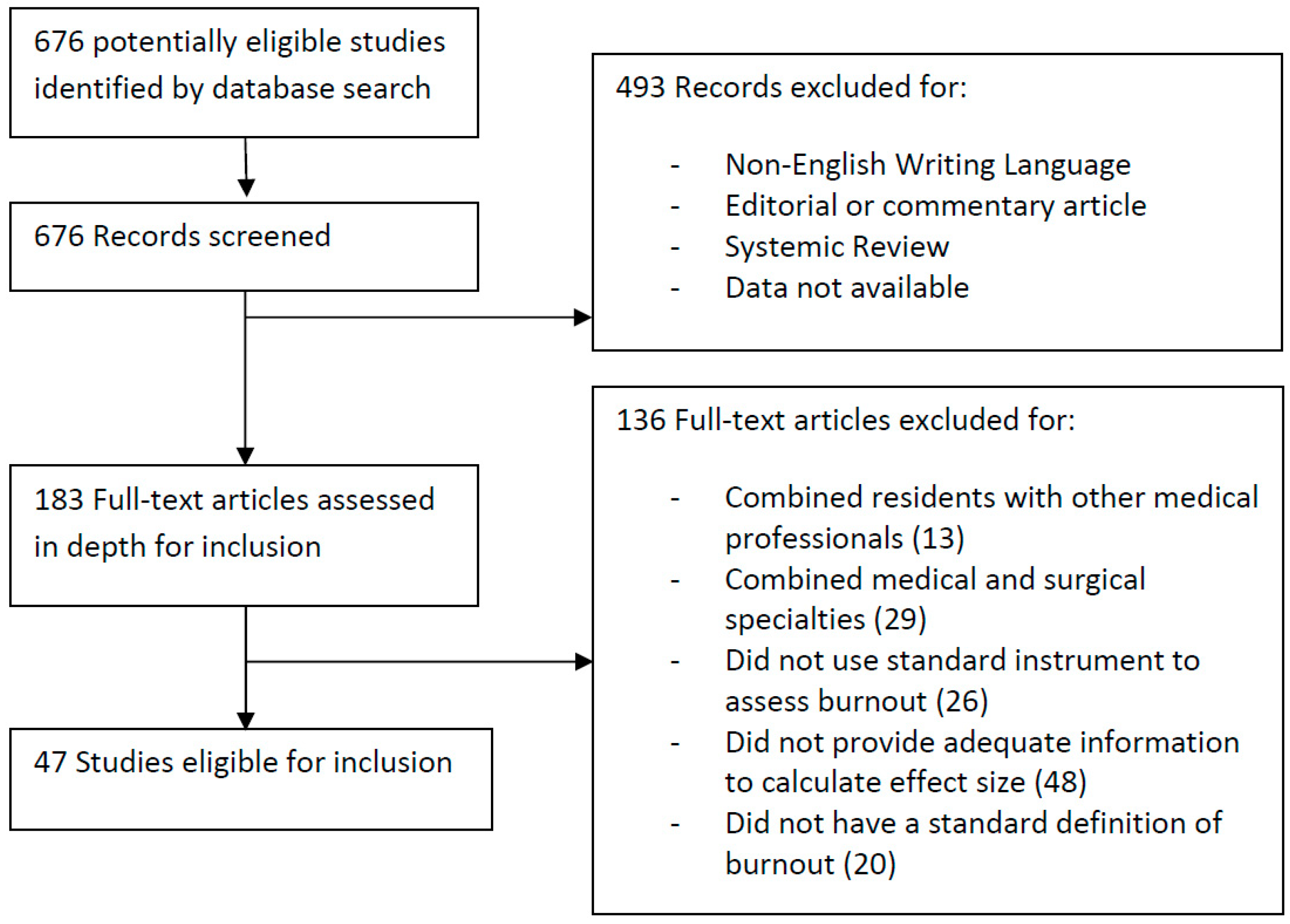
2.1. Search Strategy and Selection Criteria
2.2. Inclusion and Exclusion Criteria
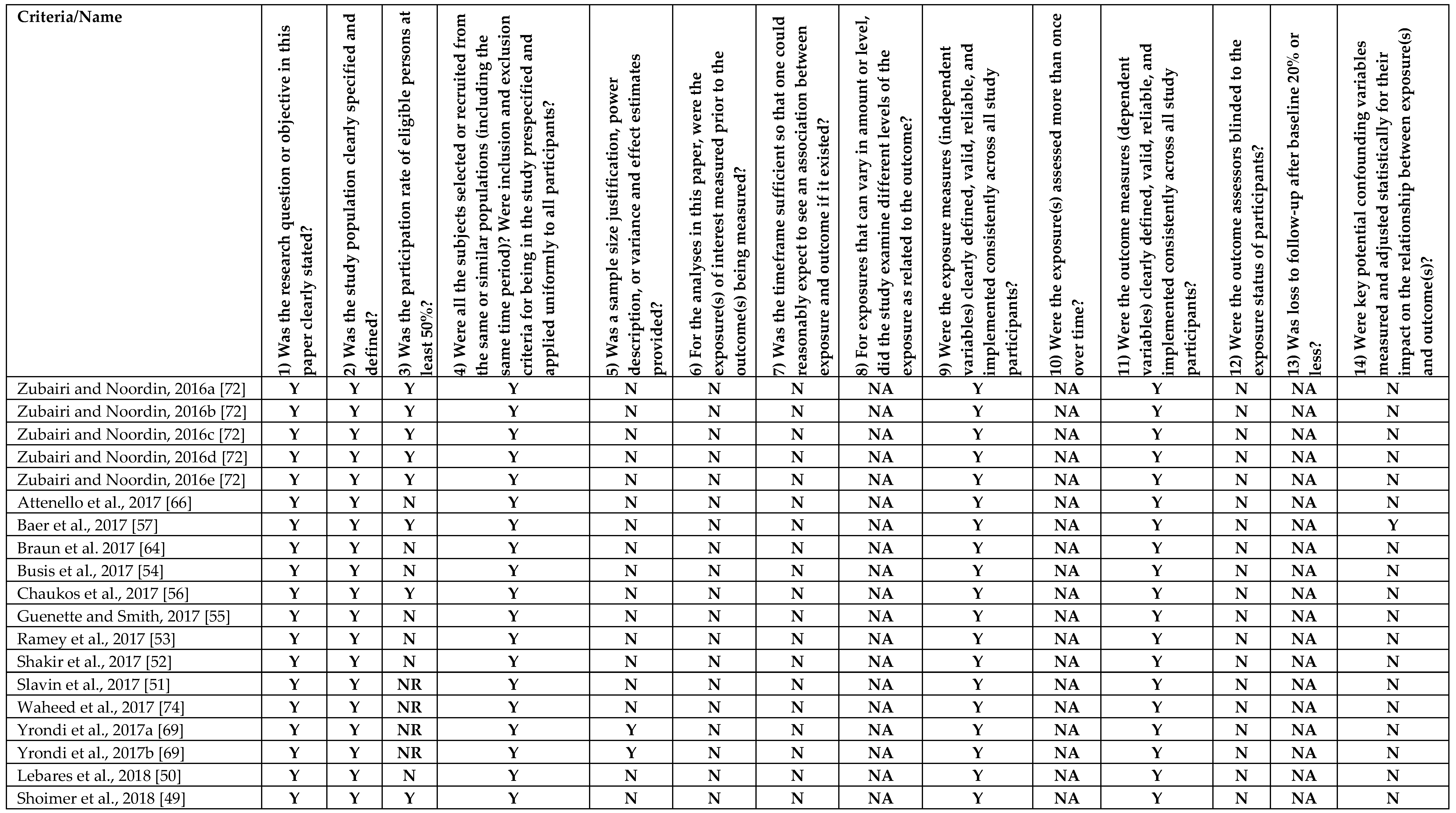
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analyses
3. Results
3.1. Characteristics of Studies
3.2. Aggregate Prevalence of Burnout
3.3. Subgroup Analysis
4. Discussion
4.1. Potential Reasons for High Prevalence of Burnout in Some Medical and Surgical Specialities
4.2. Extension of Burnout from Medical Schools into Residencies
4.3. Comparison with Other Healthcare Professions
4.4. Differences in Residency Burnout between the East and West
4.5. Future Research
4.6. Policy Implications
4.7. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A


References
- Freudenberger, H.J. Staff Burn-Out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Jackson, S.E.; Schwab, R.L.; Schuler, R.S. Toward an understanding of the burnout phenomenon. J. Appl. Psychol. 1986, 71, 630–640. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.; Leiter, M. The Maslach Burnout Inventory Manual; Consulting Psychologists Press: Palo Alto, CA, USA, 1997; Volume 3, pp. 191–218. [Google Scholar]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry Off. J. World Psychiatr. Assoc. (WPA) 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Golonka, K.; Mojsa-Kaja, J.; Gawlowska, M.; Popiel, K. Cognitive Impairments in Occupational Burnout—Error Processing and Its Indices of Reactive and Proactive Control. Front. Psychol. 2017, 8, 676. [Google Scholar] [CrossRef]
- Kang, E.K.; Lihm, H.S.; Kong, E.H. Association of intern and resident burnout with self-reported medical errors. Korean J. Fam. Med. 2013, 34, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Kluger, M.T.; Townend, K.; Laidlaw, T. Job satisfaction, stress and burnout in Australian specialist anaesthetists. Anaesthesia 2003, 58, 339–345. [Google Scholar] [CrossRef] [Green Version]
- Williams, E.S.; Konrad, T.R.; Scheckler, W.E.; Pathman, D.E.; Linzer, M.; McMurray, J.E.; Gerrity, M.; Schwartz, M. Understanding physicians’ intentions to withdraw from practice: The role of job satisfaction, job stress, mental and physical health. 2001. Health Care Manag. Rev. 2010, 35, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Dewa, C.S.; Loong, D.; Bonato, S.; Trojanowski, L.; Rea, M. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: A systematic literature review. BMC Med. Educ. 2017, 17, 195. [Google Scholar] [CrossRef]
- Williams, E.S.; Skinner, A.C. Outcomes of physician job satisfaction: A narrative review, implications, and directions for future research. Health Care Manag. Rev. 2003, 28, 119–139. [Google Scholar] [CrossRef]
- West, C.P.; Shanafelt, T.D. Physician well-being and professionalism. Minn. Med. 2007, 90, 44–46. [Google Scholar]
- Wurm, W.; Vogel, K.; Holl, A.; Ebner, C.; Bayer, D.; Morkl, S.; Szilagyi, I.S.; Hotter, E.; Kapfhammer, H.P.; Hofmann, P. Depression-Burnout Overlap in Physicians. PLoS ONE 2016, 11, e0149913. [Google Scholar] [CrossRef]
- Rosenstein, A.H.; O’Daniel, M. Impact and implications of disruptive behavior in the perioperative arena. J. Am. Coll. Surg. 2006, 203, 96–105. [Google Scholar] [CrossRef]
- Ledikwe, J.H.; Kleinman, N.J.; Mpho, M.; Mothibedi, H.; Mawandia, S.; Semo, B.W.; O’Malley, G. Associations between healthcare worker participation in workplace wellness activities and job satisfaction, occupational stress and burnout: A cross-sectional study in Botswana. BMJ Open 2018, 8, e018492. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Thomas, M.R.; Massie, F.S.; Power, D.V.; Eacker, A.; Harper, W.; Durning, S.; Moutier, C.; Szydlo, D.W.; Novotny, P.J.; et al. Burnout and suicidal ideation among U.S. medical students. Ann. Intern. Med. 2008, 149, 334–341. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Balch, C.M.; Bechamps, G.J.; Russell, T.; Dyrbye, L.; Satele, D.; Collicott, P.; Novotny, P.J.; Sloan, J.; Freischlag, J.A. Burnout and career satisfaction among American surgeons. Ann. Surg. 2009, 250, 463–471. [Google Scholar] [CrossRef]
- Kumar, S. Burnout and doctors: Prevalence, prevention and intervention. Healthcare 2016, 4, 37. [Google Scholar] [CrossRef]
- Moradi, Y.; Baradaran, H.R.; Yazdandoost, M.; Atrak, S.; Kashanian, M. Prevalence of Burnout in residents of obstetrics and gynecology: A systematic review and meta-analysis. Med. J. Islamic Repub. Iran 2015, 29, 235. [Google Scholar]
- Sanfilippo, F.; Noto, A.; Foresta, G.; Santonocito, C.; Palumbo, G.J.; Arcadipane, A.; Maybauer, D.M.; Maybauer, M.O. Incidence and Factors Associated with Burnout in Anesthesiology: A Systematic Review. BioMed Res. Int. 2017, 2017, 8648925. [Google Scholar] [CrossRef]
- Ripp, J.; Babyatsky, M.; Fallar, R.; Bazari, H.; Bellini, L.; Kapadia, C.; Katz, J.T.; Pecker, M.; Korenstein, D. The incidence and predictors of job burnout in first-year internal medicine residents: A five-institution study. Acad. Med. 2011, 86, 1304–1310. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Schaufeli, W.B.; Schwab, R.L. Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1986; Volume 21. [Google Scholar]
- Agency for Healthcare Research and Quality. Physician Burnout. Available online: https://www.ahrq.gov/professionals/clinicians-providers/ahrq.../burnout/index.html (accessed on 17 April 2019).
- National Heart, L.; Institute, B. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies; National Institutes of Health, Department of Health and Human Services: Bethesda, MD, USA, 2014.
- Cheung, M.W.L.; Ho, R.C.; Lim, Y.; Mak, A. Conducting a meta-analysis: Basics and good practices. Int. J. Rheum. Dis. 2012, 15, 129–135. [Google Scholar] [CrossRef]
- Lim, G.Y.; Tam, W.W.; Lu, Y.; Ho, C.S.; Zhang, M.W.; Ho, R.C. Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci. Rep. 2018, 8, 2861. [Google Scholar] [CrossRef]
- Quek, Y.H.; Tam, W.W.; Zhang, M.W.; Ho, R.C. The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. J. Am. Med. Dir. Assoc. 2017, 18, 111–116. [Google Scholar]
- Quek, Y.-H.; Tam, W.W.S.; Zhang, M.W.B.; Ho, R.C.M. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef]
- Tung, Y.-J.; Lo, K.K.; Ho, R.C.; Tam, W.S.W. Prevalence of depression among nursing students: A systematic review and meta-analysis. Nurse Educ. Today 2018, 63, 119–129. [Google Scholar] [CrossRef]
- Mak, A.; Cheung, M.W.; Fu, E.H.; Ho, R.C. Meta-analysis in medicine: An introduction. Int. J. Rheum. Dis. 2010, 13, 101–104. [Google Scholar] [CrossRef]
- Puthran, R.; Zhang, M.W.; Tam, W.W.; Ho, R.C. Prevalence of depression amongst medical students: A meta-analysis. Med. Educ. 2016, 50, 456–468. [Google Scholar] [CrossRef]
- Lu, D.W.; Dresden, S.; McCloskey, C.; Branzetti, J.; Gisondi, M.A. Impact of burnout on self-reported patient care among emergency physicians. West. J. Emerg. Med. 2015, 16, 996. [Google Scholar] [CrossRef]
- Pantaleoni, J.L.; Augustine, E.M.; Sourkes, B.M.; Bachrach, L.K. Burnout in pediatric residents over a 2-year period: A longitudinal study. Acad. Pediatr. 2014, 14, 167–172. [Google Scholar] [CrossRef]
- Lebensohn, P.; Dodds, S.; Benn, R.; Brooks, A.J.; Birch, M. Resident wellness behaviors. Fam. Med. 2013, 45, 541–549. [Google Scholar]
- Doolittle, B.R.; Windish, D.M.; Seelig, C.B. Burnout, coping, and spirituality among internal medicine resident physicians. J. Grad. Med. Educ. 2013, 5, 257–261. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Shanafelt, T.D.; Kolars, J.C. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA 2011, 306, 952–960. [Google Scholar] [CrossRef]
- Billings, M.E.; Lazarus, M.E.; Wenrich, M.; Curtis, J.R.; Engelberg, R.A. The effect of the hidden curriculum on resident burnout and cynicism. J. Grad. Med. Educ. 2011, 3, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Ripp, J.; Fallar, R.; Babyatsky, M.; David, R.; Reich, L.; Korenstein, D. Prevalence of resident burnout at the start of training. Teach. Learn. Med. 2010, 22, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Sargent, M.C.; Sotile, W.; Sotile, M.O.; Rubash, H.; Barrack, R.L. Quality of life during orthopaedic training and academic practice: Part 1: Orthopaedic surgery residents and faculty. JBJS 2009, 91, 2395–2405. [Google Scholar] [CrossRef] [PubMed]
- Ghetti, C.; Chang, J.; Gosman, G. Burnout, psychological skills, and empathy: Balint training in obstetrics and gynecology residents. J. Grad. Med. Educ. 2009, 1, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Landrigan, C.P.; Fahrenkopf, A.M.; Lewin, D.; Sharek, P.J.; Barger, L.K.; Eisner, M.; Edwards, S.; Chiang, V.W.; Wiedermann, B.L.; Sectish, T.C. Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics 2008, 122, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Gopal, R.; Glasheen, J.J.; Miyoshi, T.J.; Prochazka, A.V. Burnout and internal medicine resident work-hour restrictions. Arch. Intern. Med. 2005, 165, 2595–2600. [Google Scholar] [CrossRef] [PubMed]
- Goitein, L.; Shanafelt, T.D.; Wipf, J.E.; Slatore, C.G.; Back, A.L. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch. Intern. Med. 2005, 165, 2601–2606. [Google Scholar] [CrossRef]
- Martini, S.; Arfken, C.L.; Churchill, A.; Balon, R. Burnout comparison among residents in different medical specialties. Acad. Psychiatry 2004, 28, 240–242. [Google Scholar] [CrossRef]
- Garza, J.A.; Schneider, K.M.; Promecene, P.; Monga, M. Burnout in residency: A statewide study. South. Med. J. 2004, 97, 1171–1174. [Google Scholar] [CrossRef]
- Gelfand, D.V.; Podnos, Y.D.; Carmichael, J.C.; Saltzman, D.J.; Wilson, S.E.; Williams, R.A. Effect of the 80-hour workweek on resident burnout. Arch. Surg. 2004, 139, 933–940. [Google Scholar] [CrossRef]
- Campbell, J.; Prochazka, A.V.; Yamashita, T.; Gopal, R. Predictors of persistent burnout in internal medicine residents: A prospective cohort study. Acad. Med. 2010, 85, 1630–1634. [Google Scholar] [CrossRef]
- Hill, J.D.; Smith, R.J. Monitoring stress levels in postgraduate medical training. Laryngoscope 2009, 119, 75–78. [Google Scholar] [CrossRef]
- Shoimer, I.; Patten, S.; Mydlarski, P. Burnout in dermatology residents: A Canadian perspective. Br. J. Dermatol. 2018, 178, 270–271. [Google Scholar] [CrossRef]
- Lebares, C.C.; Guvva, E.V.; Ascher, N.L.; O’Sullivan, P.S.; Harris, H.W.; Epel, E.S. Burnout and Stress among US Surgery Residents: Psychological Distress and Resilience. J. Am. Coll. Surg. 2018, 226, 80–90. [Google Scholar] [CrossRef]
- Slavin, S.; Shoss, M.; Broom, M.A. A Program to Prevent Burnout, Depression, and Anxiety in First-Year Pediatric Residents. Acad. Pediatr. 2017, 17, 456–458. [Google Scholar] [CrossRef]
- Shakir, H.J.; McPheeters, M.J.; Shallwani, H.; Pittari, J.E.; Reynolds, R.M. The Prevalence of Burnout Among US Neurosurgery Residents. Neurosurgery 2017, 83, 582–590. [Google Scholar] [CrossRef]
- Ramey, S.J.; Ahmed, A.A.; Takita, C.; Wilson, L.D.; Thomas, C.R.; Yechieli, R. Burnout Evaluation of Radiation Residents Nationwide: Results of a Survey of United States Residents. Int. J. Radiat. Oncol. Boil. Phys. 2017, 99, 530–538. [Google Scholar] [CrossRef]
- Busis, N.A.; Shanafelt, T.D.; Keran, C.M.; Levin, K.H.; Schwarz, H.B.; Molano, J.R.; Vidic, T.R.; Kass, J.S.; Miyasaki, J.M.; Sloan, J.A. Burnout, career satisfaction, and well-being among US neurologists in 2016. Neurology 2017, 88, 797–808. [Google Scholar] [CrossRef] [Green Version]
- Guenette, J.P.; Smith, S.E. Burnout: Prevalence and associated factors among radiology residents in New England with comparison against United States resident physicians in other specialties. Am. J. Roentgenol. 2017, 209, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Chaukos, D.; Chad-Friedman, E.; Mehta, D.H.; Byerly, L.; Celik, A.; McCoy, T.H.; Denninger, J.W. Risk and resilience factors associated with resident burnout. Acad. Psychiatry 2017, 41, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Baer, T.E.; Feraco, A.M.; Sagalowsky, S.T.; Williams, D.; Litman, H.J.; Vinci, R.J. Pediatric resident burnout and attitudes toward patients. Pediatrics 2017, 139, e20162163. [Google Scholar] [CrossRef]
- Shapiro, J.; Zhang, B.; Warm, E.J. Residency as a social network: Burnout, loneliness, and social network centrality. J. Grad. Med. Educ. 2015, 7, 617–623. [Google Scholar] [CrossRef]
- Winkel, A.F.; Feldman, N.; Moss, H.; Jakalow, H.; Simon, J.; Blank, S. Narrative medicine workshops for obstetrics and gynecology residents and association with burnout measures. Obstet. Gynecol. 2016, 128, 27S–33S. [Google Scholar] [CrossRef]
- Ripp, J.A.; Fallar, R.; Korenstein, D. A randomized controlled trial to decrease job burnout in first-year internal medicine residents using a facilitated discussion group intervention. J. Grad. Med. Educ. 2016, 8, 256–259. [Google Scholar] [CrossRef] [PubMed]
- Spataro, B.M.; Tilstra, S.A.; Rubio, D.M.; McNeil, M.A. The toxicity of self-blame: Sex differences in burnout and coping in internal medicine trainees. J. Womens Health 2016, 25, 1147–1152. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.T.; Liebert, C.A.; Tran, J.; Lau, J.N.; Salles, A. Emotional intelligence as a predictor of resident well-being. J. Am. Coll. Surg. 2016, 223, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Ripp, J.A.; Bellini, L.; Fallar, R.; Bazari, H.; Katz, J.T.; Korenstein, D. The impact of duty hours restrictions on job burnout in internal medicine residents: A three-institution comparison study. Acad. Med. 2015, 90, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Braun, S.E.; Auerbach, S.M.; Rybarczyk, B.; Lee, B.; Call, S. Mindfulness, burnout, and effects on performance evaluations in internal medicine residents. Adv. Med. Educ. Pract. 2017, 8, 591–597. [Google Scholar] [CrossRef] [Green Version]
- Rutherford, K.; Oda, J. Family medicine residency training and burnout: A qualitative study. Can. Med. Educ. J. 2014, 5, e13. [Google Scholar]
- Attenello, F.J.; Buchanan, I.A.; Wen, T.; Donoho, D.A.; McCartney, S.; Cen, S.Y.; Khalessi, A.A.; Cohen-Gadol, A.A.; Cheng, J.S.; Mack, W.J. Factors associated with burnout among US neurosurgery residents: A nationwide survey. J. Neurosurg. 2018, 129, 1349–1363. [Google Scholar] [CrossRef]
- Blanchard, P.; Truchot, D.; Albiges-Sauvin, L.; Dewas, S.; Pointreau, Y.; Rodrigues, M.; Xhaard, A.; Loriot, Y.; Giraud, P.; Soria, J. Prevalence and causes of burnout amongst oncology residents: A comprehensive nationwide cross-sectional study. Eur. J. Cancer 2010, 46, 2708–2715. [Google Scholar] [CrossRef]
- Castelo-Branco, C.; Figueras, F.; Eixarch, E.; Quereda, F.; Cancelo, M.; Gonzalez, S.; Balasch, J. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG Int. J. Obstet. Gynaecol. 2007, 114, 94–98. [Google Scholar] [CrossRef]
- Yrondi, A.; Fournier, C.; Fourcade, O.; Schmitt, L. Burnout compared between anaesthesiology and psychiatry residents in France: An observational study. Eur. J. Anaesthesiol. (EJA) 2017, 34, 480–482. [Google Scholar] [CrossRef]
- Yazgan Aksoy, D.; Durusu Tanriover, M.; Unal, S.; Dizdar, O.; Kalyoncu, U.; Karakaya, J.; Unal, S.; Kale, G. Burnout syndrome during residency in internal medicine and pediatrics in a country without working time directive. Int. J. Health Care Qual. Assur. 2014, 27, 223–230. [Google Scholar] [CrossRef]
- Aldrees, T.; Badri, M.; Islam, T.; Alqahtani, K. Burnout among otolaryngology residents in Saudi Arabia: A multicenter study. J. Surg. Educ. 2015, 72, 844–848. [Google Scholar] [CrossRef]
- Zubairi, A.J.; Noordin, S. Factors associated with burnout among residents in a developing country. Ann. Med. Surg. 2016, 6, 60–63. [Google Scholar] [CrossRef]
- Kwah, J.; Weintraub, J.; Fallar, R.; Ripp, J. The Effect of Burnout on Medical Errors and Professionalism in First-Year Internal Medicine Residents. J. Grad. Med. Educ. 2016, 8, 597–600. [Google Scholar] [CrossRef] [Green Version]
- Waheed, K.; Liaqat, N.; Ejaz, S.; Khanum, A.; Ijaz, S.; Butt, A.; Randhawa, F.A.; Naheed, I.; Javed, S. Burnout among gynaecological residents in Lahore, Pakistan: A cross-sectional survey. Age 2017, 27, 1–69. [Google Scholar]
- Shams, T.; El-Masry, R. Job stress and burnout among academic career anaesthesiologists at an Egyptian University Hospital. Sultan Qaboos Univ. Med. J. 2013, 13, 287. [Google Scholar] [CrossRef] [PubMed]
- Arora, M.; Diwan, A.D.; Harris, I.A. Prevalence and factors of burnout among Australian orthopaedic trainees: A cross-sectional study. J. Orthop. Surg. 2014, 22, 374–377. [Google Scholar] [CrossRef] [PubMed]
- Cubero, D.I.; Fumis, R.R.L.; de Sá, T.H.; Dettino, A.; Costa, F.O.; Van Eyll, B.M.A.; Beato, C.; Peria, F.M.; Mota, A.; Altino, J. Burnout in medical oncology fellows: A prospective multicenter cohort study in Brazilian institutions. J. Cancer Educ. 2016, 31, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Hughes, D.; Burke, D.; Hickie, I.; Wilson, A.; Tobin, M. Advanced training in adult psychiatry. Australas. Psychiatry 2002, 10, 6–10. [Google Scholar] [CrossRef]
- Momoh, P. Medical Ethics Manual; World Medical Association: Ferney-Voltaire, France, 2006. [Google Scholar]
- Myers, M.F. Physician impairment: Is it relevant to academic psychiatry? Acad. Psychiatry 2008, 32, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Hauer, A.; Waukau, H.J.; Welch, P. Physician Burnout in Wisconsin: An Alarming Trend Affecting Physician Wellness. WMJ Off. Publ. State Med. Soc. Wis. 2018, 117, 194–200. [Google Scholar]
- Liew, C. The future of radiology augmented with Artificial Intelligence: A strategy for success. Eur. J. Radiol. 2018, 102, 152–156. [Google Scholar] [CrossRef]
- Erschens, R.; Keifenheim, K.E.; Herrmann-Werner, A.; Loda, T.; Schwille-Kiuntke, J.; Bugaj, T.J.; Nikendei, C.; Huhn, D.; Zipfel, S.; Junne, F. Professional burnout among medical students: Systematic literature review and meta-analysis. Med. Teach. 2018, 41, 172–183. [Google Scholar] [CrossRef]
- Freischlag, J.A. Burnout and Depression Among General Surgery Residents: Image Is Everything—It Alters Perception. JAMA Surg. 2018, 153, 711. [Google Scholar] [CrossRef]
- Lee, Y.; Rosenblat, J.D.; Lee, J.; Carmona, N.E.; Subramaniapillai, M.; Shekotikhina, M.; Mansur, R.B.; Brietzke, E.; Lee, J.-H.; Ho, R.C. Efficacy of antidepressants on measures of workplace functioning in major depressive disorder: A systematic review. J. Affect. Disord. 2017, 227, 406–415. [Google Scholar] [CrossRef]
- Monsalve-Reyes, C.S.; San Luis-Costas, C.; Gómez-Urquiza, J.L.; Albendín-García, L.; Aguayo, R.; Cañadas-De la Fuente, G.A. Burnout syndrome and its prevalence in primary care nursing: A systematic review and meta-analysis. BMC Fam. Pract. 2018, 19, 59. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in Burnout and Satisfaction with Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef]
- Ogawa, R.; Seo, E.; Maeno, T.; Ito, M.; Sanuki, M.; Maeno, T. The relationship between long working hours and depression among first-year residents in Japan. BMC Med. Educ. 2018, 18, 50. [Google Scholar] [CrossRef]
- Ebrahimi, S.; Kargar, Z. Occupational stress among medical residents in educational hospitals. Ann. Occup. Environ. Med. 2018, 30, 51. [Google Scholar] [CrossRef]
- Temple, J. Resident duty hours around the globe: Where are we now? BMC Med. Educ. 2014, 14, S8. [Google Scholar] [CrossRef]
- Nasca, T.J. Summary of Changes to ACGME Common Program Requirements Section VI. Available online: http://www.acgme.org/Portals/0/PDFs/Nasca-Community/Section-VI-Memo-3-10-17.pdf (accessed on 9 May 2018).
- Fargen, K.M.; Rosen, C.L. Are Duty Hour Regulations Promoting a Culture of Dishonesty Among Resident Physicians? J. Grad. Med. Educ. 2013, 5, 553–555. [Google Scholar] [CrossRef] [Green Version]
- Siu, C.; Yuen, S.K.; Cheung, A. Burnout among public doctors in Hong Kong: Cross-sectional survey. Hong Kong Med. J. = Xianggang Yi Xue Za Zhi 2012, 18, 186–192. [Google Scholar]
- Choo, C.C.; Harris, K.M.; Ho, R.C. Prediction of lethality in suicide attempts: Gender matters. OMEGA-J. Death Dying 2017. [Google Scholar] [CrossRef]
- Williford, M.L.; Scarlet, S.; Meyers, M.O.; Luckett, D.J.; Fine, J.P.; Goettler, C.E.; Green, J.M.; Clancy, T.V.; Hildreth, A.N.; Meltzer-Brody, S.E. Multiple-institution comparison of resident and faculty perceptions of burnout and depression during surgical training. JAMA Surg. 2018, 153, 705–711. [Google Scholar] [CrossRef]
- Rodrigues, H.; Cobucci, R.; Oliveira, A.; Cabral, J.V.; Medeiros, L.; Gurgel, K.; Souza, T.; Goncalves, A.K. Burnout syndrome among medical residents: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0206840. [Google Scholar] [CrossRef]
- Eckleberry-Hunt, J.; Kirkpatrick, H.; Barbera, T. The Problems With Burnout Research. Acad. Med. 2018, 93, 367–370. [Google Scholar] [CrossRef]
- Ho, C.S.; Zhang, M.W.; Ho, R.C. Optical Topography in Psychiatry: A Chip Off the Old Block or a New Look Beyond the Mind-Brain Frontiers? Front. Psychiatry 2016, 7, 74. [Google Scholar] [CrossRef]
- Lai, C.Y.Y.; Ho, C.S.H.; Lim, C.R.; Ho, R.C.M. Functional near-infrared spectroscopy in psychiatry. BJPsych Adv. 2017, 23, 324–330. [Google Scholar] [CrossRef] [Green Version]
- Ho, R.C.; Cheung, M.W.; Fu, E.; Win, H.H.; Zaw, M.H.; Ng, A.; Mak, A. Is high homocysteine level a risk factor for cognitive decline in elderly? A systematic review, meta-analysis, and meta-regression. Am. J. Geriatr. Psychiatry 2011, 19, 607–617. [Google Scholar] [CrossRef]
- Lancet. Violence against doctors: Why China? Why now? What next? Lancet 2014, 383, 1013. [Google Scholar] [CrossRef] [Green Version]
- Lo, D.; Wu, F.; Chan, M.; Chu, R.; Li, D. A systematic review of burnout among doctors in China: A cultural perspective. Asia Pac. Fam. Med. 2018, 17, 3. [Google Scholar] [CrossRef]


| Study | Study Demographics | Study Results | MBI/Abbrev. MBI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Country | Region | Mean Age | Proportion of Males | Specialty | Medical/Surgical | Response Rate | Sample Size | Number of Residents Who Reported Burnout | ||
| Garza et al., 2004 [45] | USA | N. America | NR | 0.29 | Obstetrics and Gynecology | Surgical | 37% | 136 | 52 | MBI |
| Gelfand et al., 2004 [46] | USA | N. America | NR | NR | General Surgery | Surgical | 69% | 37 | 21 | MBI |
| Martini et al., 2004a [44] | USA | N. America | NR | NR | Obstetrics and Gynecology | Surgical | 35% | 36 | 12 | MBI |
| Martini et al., 2004b [44] | USA | N. America | NR | NR | Internal Medicine | Medical | 35% | 114 | 24 | MBI |
| Martini et al., 2004c [44] | USA | N. America | NR | NR | Neurology | Medical | 35% | 16 | 8 | MBI |
| Martini et al., 2004d [44] | USA | N. America | NR | NR | Ophthalmology | Surgical | 35% | 21 | 5 | MBI |
| Martini et al., 2004e [44] | USA | N. America | NR | NR | Dermatology | Medical | 35% | 10 | 6 | MBI |
| Martini et al., 2004f [44] | USA | N. America | NR | NR | General Surgery | Surgical | 35% | 59 | 25 | MBI |
| Martini et al., 2004g [44] | USA | N. America | NR | NR | Psychiatry | Medical | 35% | 29 | 15 | MBI |
| Martini et al., 2004h [44] | USA | N. America | NR | NR | Family Medicine | Medical | 35% | 36 | 15 | MBI |
| Goitein et al., 2005 [43] | USA | N. America | NR | 0.47 | Internal Medicine | Medical | 73% | 118 | 80 | MBI |
| Gopal et al., 2005 [42] | USA | N. America | 29.9 | 0.58 | Internal Medicine | Medical | 87% | 121 | 74 | MBI |
| Castelo-Branco et al., 2007 [68] | Spain | Europe | 27.0 | 0.14 | Obstetrics and Gynecology | Surgical | 67% | 109 | 63 | MBI |
| Landrigan et al., 2008 [41] | USA | N. America | 30.2 | 0.29 | Pediatrics | Medical | 59% | 220 | 141 | MBI |
| Ghetti et al., 2009 [40] | USA | N. America | 28.0 | NR | Obstetrics and Gynecology | Surgical | 47% | 17 | 13 | MBI |
| Hill and Smith, 2009 [48] | USA | N. America | NR | NR | Otolaryngology | Surgical | 76% | 22 | 7 | MBI |
| Sargent et al., 2009 [39] | USA | N. America | NR | 0.88 | Orthopedics | Surgical | NR | 384 | 215 | MBI |
| Blanchard et al., 2010 [67] | France | Europe | 28.0 | 0.40 | Oncology | Medical | 60% | 204 | 89 | MBI |
| Campbell et al., 2010 [47] | USA | N. America | 30.0 | 0.51 | Internal Medicine | Medical | 48% | 86 | 58 | MBI |
| Ripp et al., 2010 [38] | USA | N. America | NR | 0.50 | Internal Medicine | Medical | 94% | 145 | 50 | MBI |
| Billings et al., 2011 [37] | USA | N. America | NR | NR | Internal Medicine | Medical | 43% | 284 | 128 | Abbrev. MBI |
| Ripp et al., 2011 [20] | USA | N. America | NR | 0.48 | Internal Medicine | Surgical | 73% | 191 | 154 | MBI |
| West et al., 2011 [36] | USA | N. America | NR | 0.57 | General Surgery | Surgical | 77% | 16,394 | 8343 | Abbrev. MBI |
| Doolittle et al., 2013 [35] | USA | N. America | 30.0 | 0.50 | Internal Medicine | Medical | 63% | 108 | 94 | MBI |
| Lebensohn et al., 2013 [34] | USA | N. America | 29.0 | 0.40 | Family Medicine | Medical | 77% | 167 | 23 | MBI |
| Shams and El-Masry, 2013 [75] | Egypt | Africa | NR | NR | Anesthesia | Medical | 73% | 30 | 21 | MBI |
| Aksoy et al., 2014a [70] | Turkey | Asia | 25.9 | 0.45 | Pediatrics | Medical | 66% | 22 | 6 | MBI |
| Aksoy et al., 2014b [70] | Turkey | Asia | 26.6 | 0.48 | Internal Medicine | Medical | 66% | 33 | 11 | MBI |
| Arora et al., 2014 [76] | Australia | Oceania | NR | 0.88 | Orthopedics | Surgical | 22% | 51 | 27 | MBI |
| Pantaleoni et al., 2014 [33] | USA | N. America | NR | NR | Pediatrics | Medical | 100% | 54 | 9 | MBI |
| Rutherford and Oda, 2014 [65] | Canada | N. America | 29.5 | 0.10 | Family Medicine | Medical | 4% | 10 | 7 | MBI |
| Aldrees et al., 2015 [71] | Saudi Arabia | Asia | 29.0 | 0.67 | Otolaryngology | Surgical | 69% | 85 | 38 | MBI |
| Lu et al., 2015 [32] | USA | N. America | NR | NR | Emergency Medicine | Medical | 50% | 27 | 17 | MBI |
| Shapiro et al., 2015 [58] | USA | N. America | NR | 0.51 | Internal Medicine | Medical | 77% | 95 | 43 | MBI |
| Ripp et al., 2015a [63] | USA | N. America | NR | 0.44 | Internal Medicine | Medical | 62% | 108 | 91 | MBI |
| Ripp et al., 2015b [63] | USA | N. America | NR | 0.58 | Internal Medicine | Medical | 71% | 123 | 92 | MBI |
| Cubero et al., 2016 [77] | Brazil | S. America | 28.4 | 0.54 | Oncology | Medical | 31% | 54 | 15 | MBI |
| Lin et al., 2016 [62] | USA | N. America | 30.8 | 0.58 | General Surgery | Surgical | 63% | 73 | 60 | MBI |
| Spataro et al., 2016 [61] | USA | N. America | 29.9 | 0.51 | Internal Medicine | Medical | 69% | 198 | 45 | MBI |
| Kwah et al., 2016 [73] | Pakistan | Asia | NR | NR | Internal Medicine | Medical | 59% | 32 | 24 | MBI |
| Ripp et al., 2016 [60] | USA | N. America | NR | NR | Internal Medicine | Medical | 76% | 39 | 17 | MBI |
| Winkel et al., 2016 [59] | USA | N. America | NR | NR | Obstetrics and Gynecology | Surgical | 64% | 42 | 28 | MBI |
| Zubairi and Noordin, 2016a [72] | Pakistan | Asia | NR | 0.54 | General Surgery | Surgical | 54% | 24 | 19 | MBI |
| Zubairi and Noordin, 2016b [72] | Pakistan | Asia | NR | 0.54 | Internal Medicine | Medical | 54% | 32 | 25 | MBI |
| Zubairi and Noordin, 2016c [72] | Pakistan | Asia | NR | 0.54 | Pediatrics | Medical | 54% | 11 | 5 | MBI |
| Zubairi and Noordin, 2016d [72] | Pakistan | Asia | NR | 0.54 | Radiology | Medical | 54% | 5 | 5 | MBI |
| Zubairi and Noordin, 2016e [72] | Pakistan | Asia | NR | 0.54 | Anesthesia | Medical | 54% | 10 | 7 | MBI |
| Attenello et al., 2017 [66] | USA | N. America | 30.9 | 0.78 | Neurosurgery | Surgical | 21% | 346 | 232 | Abbrev. MBI |
| Baer et al., 2017 [57] | USA | N. America | 29.4 | 0.21 | Pediatrics | Medical | 53% | 258 | 101 | Abbrev. MBI |
| Braun et al. 2017 [64] | USA | N. America | 28.6 | 0.79 | Internal Medicine | Medical | 30% | 38 | 19 | MBI |
| Busis et al., 2017 [54] | USA | N. America | 32.0 | 0.51 | Neurology | Medical | 38% | 212 | 156 | MBI |
| Chaukos et al., 2017 [56] | USA | N. America | 28.3 | 0.40 | Psychiatry | Medical | 80% | 68 | 19 | MBI |
| Guenette and Smith, 2017 [55] | USA | N. America | NR | 0.63 | Radiology | Medical | 20% | 94 | 35 | MBI |
| Ramey et al., 2017 [53] | USA | N. America | NR | 0.69 | Oncology | Medical | 32% | 232 | 86 | MBI |
| Shakir et al., 2017 [52] | USA | N. America | NR | 0.80 | Neurosurgery | Surgical | 21% | 255 | 93 | Abbrev. MBI |
| Slavin et al., 2017 [51] | USA | N. America | NR | NR | Pediatrics | Medical | NR | 18 | 14 | MBI |
| Waheed et al., 2017 [74] | Pakistan | Asia | 27.5 | NR | Obstetrics and Gynecology | Surgical | NR | 102 | 54 | MBI |
| Yrondi et al., 2017a [69] | France | Europe | 28.8 | 0.55 | Anesthesia | Medical | NR | 123 | 11 | MBI |
| Yrondi et al., 2017b [69] | France | Europe | 27.7 | 0.33 | Psychiatry | Medical | NR | 148 | 20 | MBI |
| Lebares et al., 2018 [50] | USA | N. America | NR | 0.49 | General Surgery | Surgical | 10% | 566 | 322 | MBI |
| Shoimer et al., 2018 [49] | Canada | N. America | NR | NR | Dermatology | Medical | 59% | 96 | 49 | MBI |
| Medical Specialty/Region | Number of Residents (pct.) | Burnout Prevalence pct. and 95% CI | I2 |
|---|---|---|---|
| All residents | 22,778 (100%) | 51.0% (45.0–57.0) | 97.0% |
| Surgical vs. medical: p (subgroup difference) = 0.337 | |||
| Surgical residents | 18,759 (82.36%) | 53.27% (46.27–60.15) | 94.8% |
| Medical residents | 4019 (17.64%) | 50.13% (42.12–58.13) | 95.0% |
| * Specialty: p (subgroup difference) = 0.533 | |||
| Radiology | 99 (0.43%) | 77.16% (5.99–99.45) | 77.8% |
| Neurology | 228 (1%) | 71.93% (65.78–77.39) | 0% |
| General Surgery | 17,153 (75.31%) | 58.39% (45.72–70.04) | 96.0% |
| Internal Medicine | 1865 (8.19%) | 57.11% (45.11–68.33) | 95.3% |
| Orthopedics | 435 (1.91%) | 55.63% (50.93–60.28) | 96.3% |
| Dermatology | 106 (0.47%) | 51.89% (42.42–61.21) | 0% |
| Obstetrics and Gynecology | 442 (1.94%) | 52.84% (41.77–63.63) | 78.0% |
| Neurosurgery | 601 (2.63%) | 52.02% (31.02–72.33) | 96.3% |
| Pediatrics | 583 (2.6%) | 43.74% (26.70–62.39) | 92.3% |
| Anesthesia | 163 (0.71%) | 43.71% (11.15–82.29) | 92.3% |
| Otolaryngology | 107 (0.47%) | 42.06% (33.09–51.58) | 0.0% |
| Psychiatry | 245 (1.08%) | 42.05% (33.09–51.58) | 89.6% |
| Oncology | 490 (2.15%) | 38.36% (32.69–44.37) | 27.6% |
| Family Medicine | 213 (0.94%) | 35.97% (13.89–66.18) | 88.4% |
| † Region: p (subgroup difference) = 0.093 | |||
| Several Asian countries (Pakistan, Saudi Arabia, and Turkey) | 356 (1.56%) | 57.18% (45.80–67.85) | 80.9% |
| Several European countries (France, Spain) | 584 (2.56%) | 27.72% (17.40–41.11) | 96.4% |
| North America | 21,757(95.52%) | 51.64% (46.96–56.28) | 97.1% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Low, Z.X.; Yeo, K.A.; Sharma, V.K.; Leung, G.K.; McIntyre, R.S.; Guerrero, A.; Lu, B.; Sin Fai Lam, C.C.; Tran, B.X.; Nguyen, L.H.; et al. Prevalence of Burnout in Medical and Surgical Residents: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 1479. https://doi.org/10.3390/ijerph16091479
Low ZX, Yeo KA, Sharma VK, Leung GK, McIntyre RS, Guerrero A, Lu B, Sin Fai Lam CC, Tran BX, Nguyen LH, et al. Prevalence of Burnout in Medical and Surgical Residents: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2019; 16(9):1479. https://doi.org/10.3390/ijerph16091479
Chicago/Turabian StyleLow, Zhi Xuan, Keith A. Yeo, Vijay K. Sharma, Gilberto K. Leung, Roger S. McIntyre, Anthony Guerrero, Brett Lu, Chun Chiang Sin Fai Lam, Bach X. Tran, Long H. Nguyen, and et al. 2019. "Prevalence of Burnout in Medical and Surgical Residents: A Meta-Analysis" International Journal of Environmental Research and Public Health 16, no. 9: 1479. https://doi.org/10.3390/ijerph16091479
APA StyleLow, Z. X., Yeo, K. A., Sharma, V. K., Leung, G. K., McIntyre, R. S., Guerrero, A., Lu, B., Sin Fai Lam, C. C., Tran, B. X., Nguyen, L. H., Ho, C. S., Tam, W. W., & Ho, R. C. (2019). Prevalence of Burnout in Medical and Surgical Residents: A Meta-Analysis. International Journal of Environmental Research and Public Health, 16(9), 1479. https://doi.org/10.3390/ijerph16091479








