Tailoring Tofacitinib Oral Therapy in Rheumatoid Arthritis: The TuTORApp—A Usability Study
Abstract
1. Introduction
2. Methods
2.1. Phase I: TuTOR Mobile App Design and Development
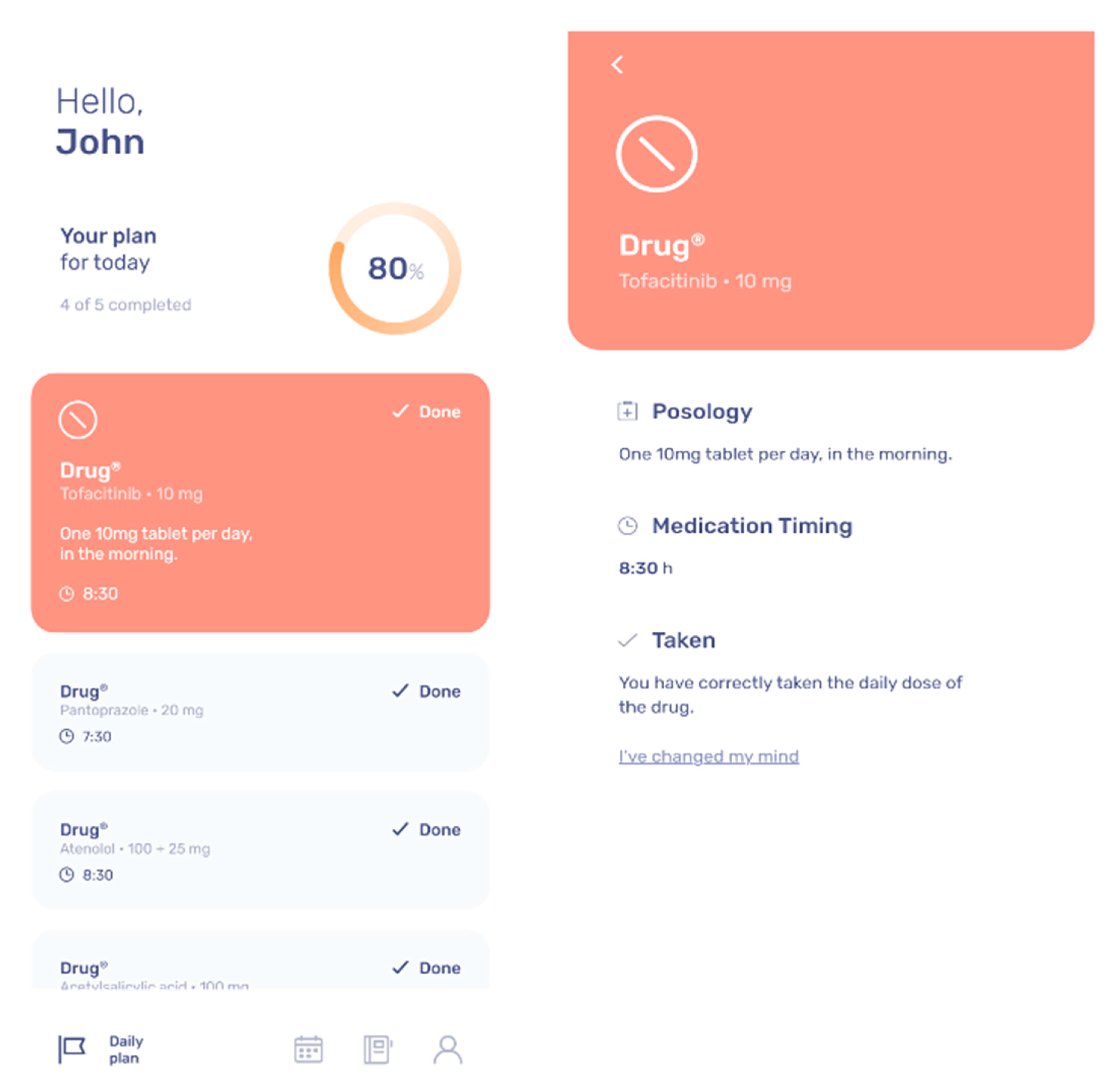
2.1.1. Not Just A Reminder: Smart Therapy Assistant
2.1.2. Medical Plan
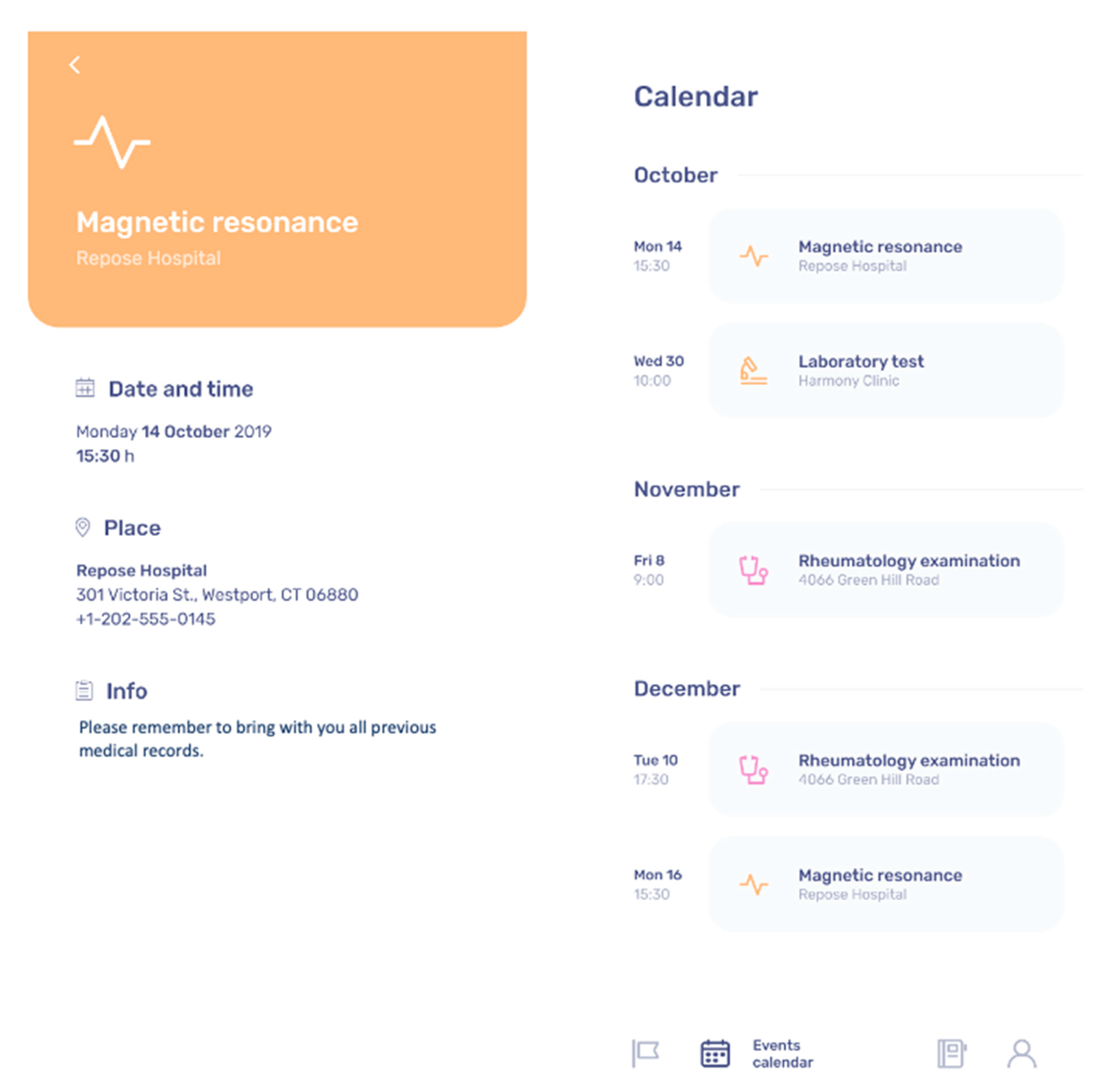
2.1.3. Clinical Follow-up
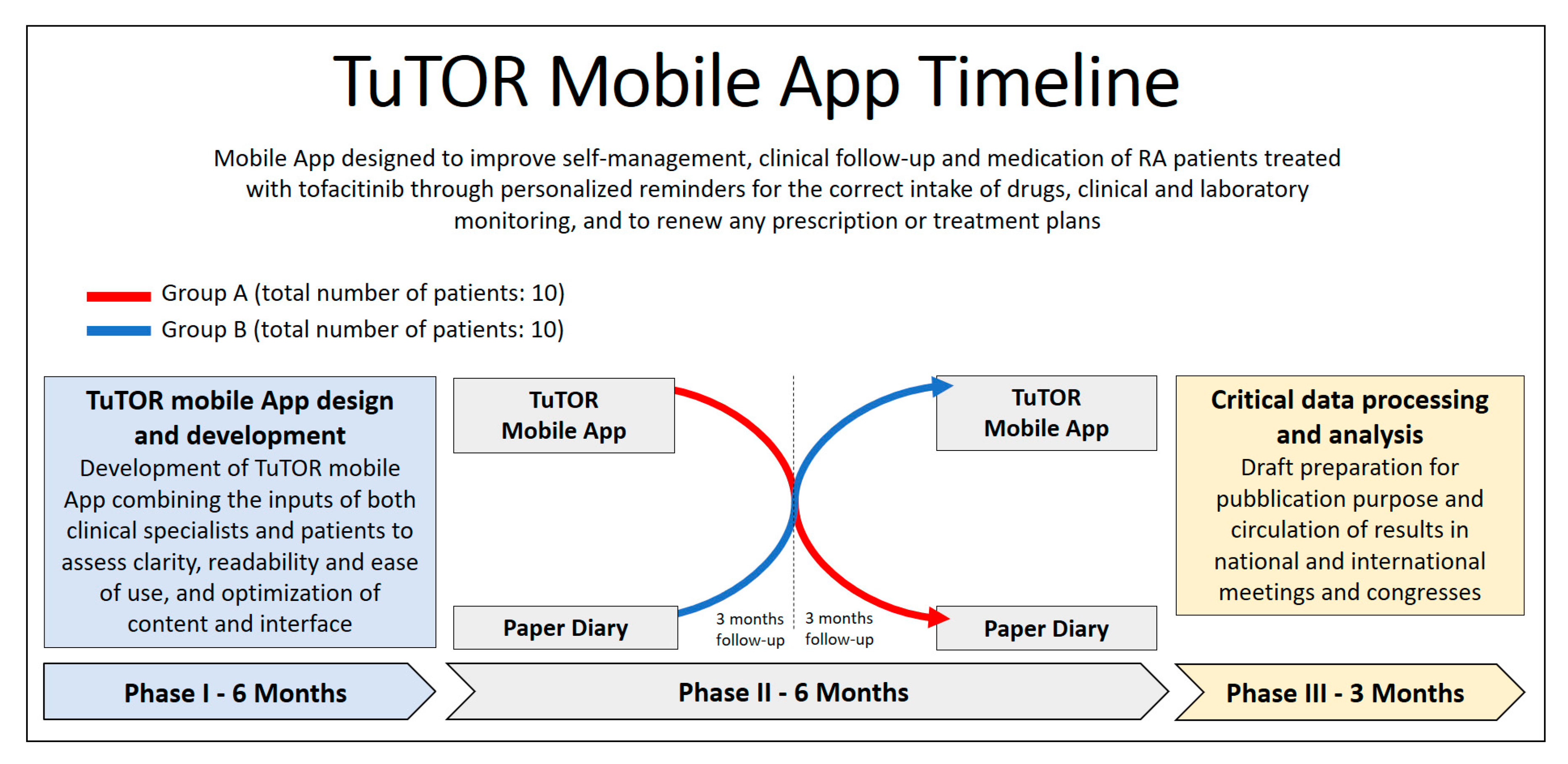
2.2. Phase II: Validation of the TuTOR App
2.2.1. Clinical Validation of TuTOR Mobile App Protocol
2.2.2. Patients Characteristics
Inclusion Criteria
Exclusion Criteria
2.3. Data Analysis
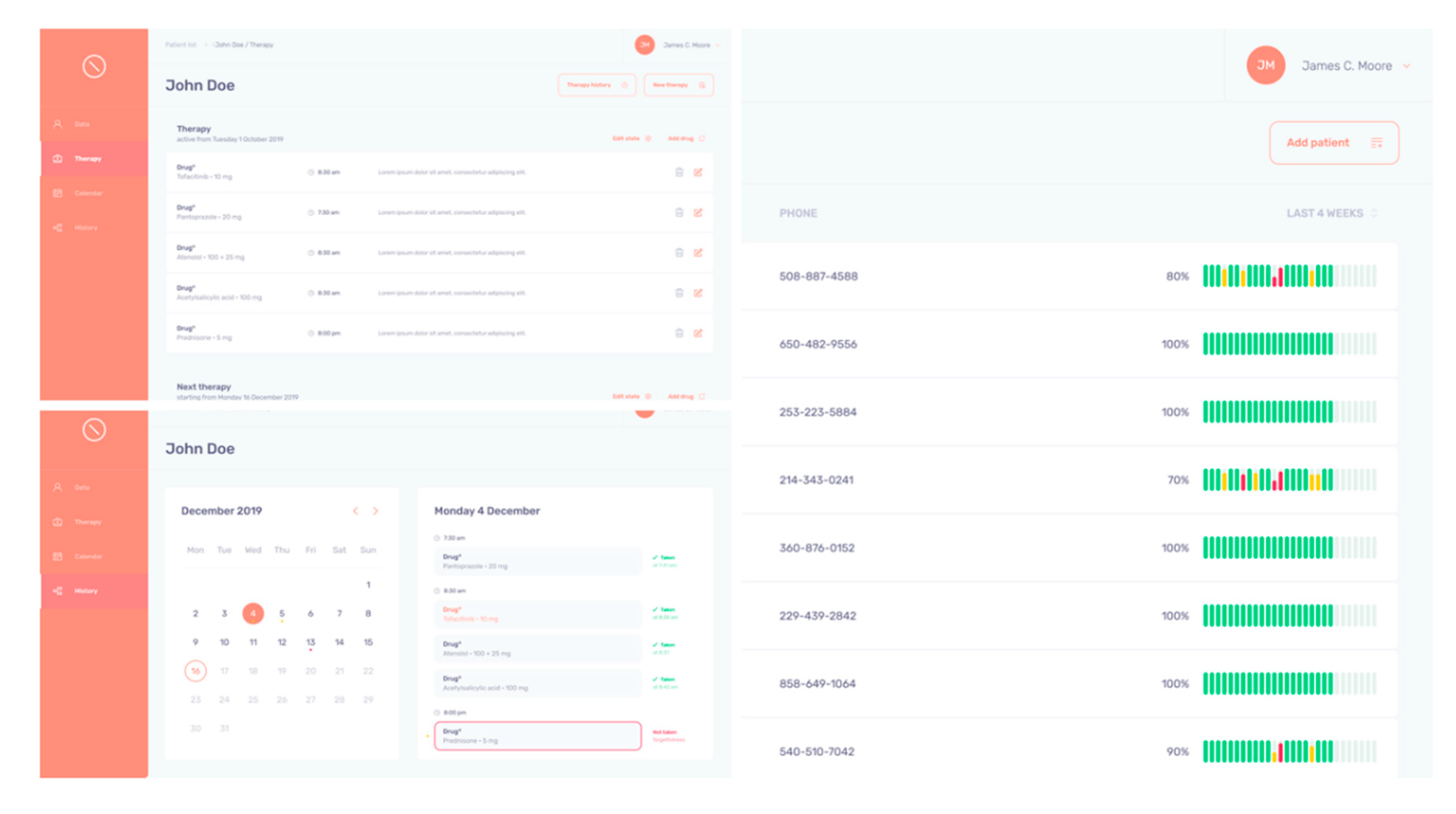
2.3.1. Objective Indicators for Therapy Adherence and Clinical Follow-up
2.3.2. Back-Office
2.3.3. Subjective Indicators for Therapy Adherence and Clinical Follow-up
2.3.4. Statistical Analysis Plan
3. Expected Results and Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wiens, A.; Venson, R.; Correr, C.J.; Otuki, M.F.; Pontarolo, R. Meta-analysis of the efficacy and safety of adalimumab, etanercept, and infliximab for the treatment of rheumatoid arthritis. Pharmacotherapy 2010, 30, 339–353. [Google Scholar] [CrossRef] [PubMed]
- Hahn, B.H.; McMahon, M.A.; Wilkinson, A.; Wallace, W.D.; Daikh, D.I.; Fitzgerald, J.D.; Karpouzas, G.A.; Merrill, J.T.; Wallace, D.J.; Yazdany, J.; et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res. (Hoboken) 2012, 64, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Smolen, J.S.; Landew, R.; Bijlsma, J.; Burmester, G.; Chatzidionysiou, K.; Dougados, M.; Nam, J.; Ramiro, S.; Voshaar, M.; van Vollenhoven, R.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann. Rheum. Dis. 2017, 76, 960–977. [Google Scholar] [CrossRef] [PubMed]
- Burmester, G.R.; Blanco, R.; Charles-Schoeman, C.; Wollenhaupt, J.; Zerbini, C.; Benda, B.; Gruben, D.; Wallenstein, G.; Krishnaswami, S.; Zwillich, S.H.; et al. Tofacitinib (CP-690,550) in combination with methotrexate in patients with active rheumatoid arthritis with an inadequate response to tumour necrosis factor inhibitors: A randomised phase 3 trial. Lancet 2013, 381, 451–460. [Google Scholar] [CrossRef]
- Fleischmann, R.; Kremer, J.; Cush, J.; Schulze-Koops, H.; Connell, C.A.; Bradley, J.D.; Gruben, J.D.; Wallenstein, G.V.; Zwillich, S.H. Placebo-Controlled Trial of TofacitinibMonotherapy in Rheumatoid Arthritis. N. Engl. J. Med. 2012, 367, 495–507. [Google Scholar] [CrossRef] [PubMed]
- Del Rincón, I.D.; Williams, K.; Stern, M.P.; Freeman, G.L.; Escalante, A. High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001, 44, 2737–2745. [Google Scholar] [CrossRef]
- Vrijens, B.; Vincze, G.; Kristanto, P.; Urquhart, J.; Burnier, M. Adherence to prescribed antihypertensive drug treatments: Longitudinal study of electronically compiled dosing histories. BMJ 2008, 336, 1114–1117. [Google Scholar] [CrossRef] [PubMed]
- Melnikow, J.; Kiefe, C. Patient compliance and medical research: Issues in methodology. J. Gen. Intern. Med. 1994, 9, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Cramer, J.A.; Benedict, A.; Muszbek, N.; Keskinaslan, A.; Khan, Z.M. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: A review. Int. J. Clin. Pract. 2008, 62, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Hamood, H.; Hamood, R.; Green, M.S.; Among, R. Determinants of adherence to evidence-based therapy after acute myocardial infarction. Eur. J. Prev. Cardiol. 2016, 23, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Grindrod, K.A.; Li, M.; Gates, A. Evaluating user perceptions of mobile medication management applications with older adults: A usability study. JMIR mHealth uHealth 2014, 2, e11. [Google Scholar] [CrossRef] [PubMed]
- Mertens, A.; Brandl, C.; Miron-Shatz, T.; Schlick, C.; Neumann, T.; Kribben, A.; Meister, S.; Diamantidis, C.J.; Albrecht, U.-V.; Horn, P.; et al. A mobile application improves therapy-adherence rates in elderly patients undergoing rehabilitation. Medicine 2016, 95, e4446. [Google Scholar] [CrossRef] [PubMed]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, M.C.; Chang, R.W.; Dwosh, I.; Lindsey, S.; Pincus, T.; Wolfe, F. The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum. 1992, 35, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Steele, R.; Lo, A.; Secombe, C.; Wong, Y.K. Elderly persons’ perception and acceptance of using wireless sensor networks to assist healthcare. Int. J. Med. Inform. 2009, 78, 788–801. [Google Scholar] [CrossRef] [PubMed]
- Jank, S.; Bertsche, T.; Schellberg, D.; Herzog, W.; Haefeli, W.E. The A14-scale: Development and evaluation of a questionnaire for assessment of adherence and individual barriers. Pharm. World Sci. 2009, 31, 426–431. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sciascia, S.; Radin, M.; Cecchi, I.; Di Nunzio, P.; Buccarano, N.; Di Gregorio, F.; Valeria, M.; Osella, S.; Crosasso, P.; Favuzzi, M.D.; et al. Tailoring Tofacitinib Oral Therapy in Rheumatoid Arthritis: The TuTORApp—A Usability Study. Int. J. Environ. Res. Public Health 2020, 17, 3469. https://doi.org/10.3390/ijerph17103469
Sciascia S, Radin M, Cecchi I, Di Nunzio P, Buccarano N, Di Gregorio F, Valeria M, Osella S, Crosasso P, Favuzzi MD, et al. Tailoring Tofacitinib Oral Therapy in Rheumatoid Arthritis: The TuTORApp—A Usability Study. International Journal of Environmental Research and Public Health. 2020; 17(10):3469. https://doi.org/10.3390/ijerph17103469
Chicago/Turabian StyleSciascia, Savino, Massimo Radin, Irene Cecchi, Pierluigi Di Nunzio, Nicola Buccarano, Federico Di Gregorio, Milone Valeria, Sara Osella, Paola Crosasso, Marika Denise Favuzzi, and et al. 2020. "Tailoring Tofacitinib Oral Therapy in Rheumatoid Arthritis: The TuTORApp—A Usability Study" International Journal of Environmental Research and Public Health 17, no. 10: 3469. https://doi.org/10.3390/ijerph17103469
APA StyleSciascia, S., Radin, M., Cecchi, I., Di Nunzio, P., Buccarano, N., Di Gregorio, F., Valeria, M., Osella, S., Crosasso, P., Favuzzi, M. D., Rubini, E., Foddai, S. G., Baldovino, S., Roccatello, D., & Rossi, D. (2020). Tailoring Tofacitinib Oral Therapy in Rheumatoid Arthritis: The TuTORApp—A Usability Study. International Journal of Environmental Research and Public Health, 17(10), 3469. https://doi.org/10.3390/ijerph17103469








