Cost-Effectiveness of Dengue Vaccination in Indonesia: Considering Integrated Programs with Wolbachia-Infected Mosquitos and Health Education
Abstract
:1. Introduction
2. Methods
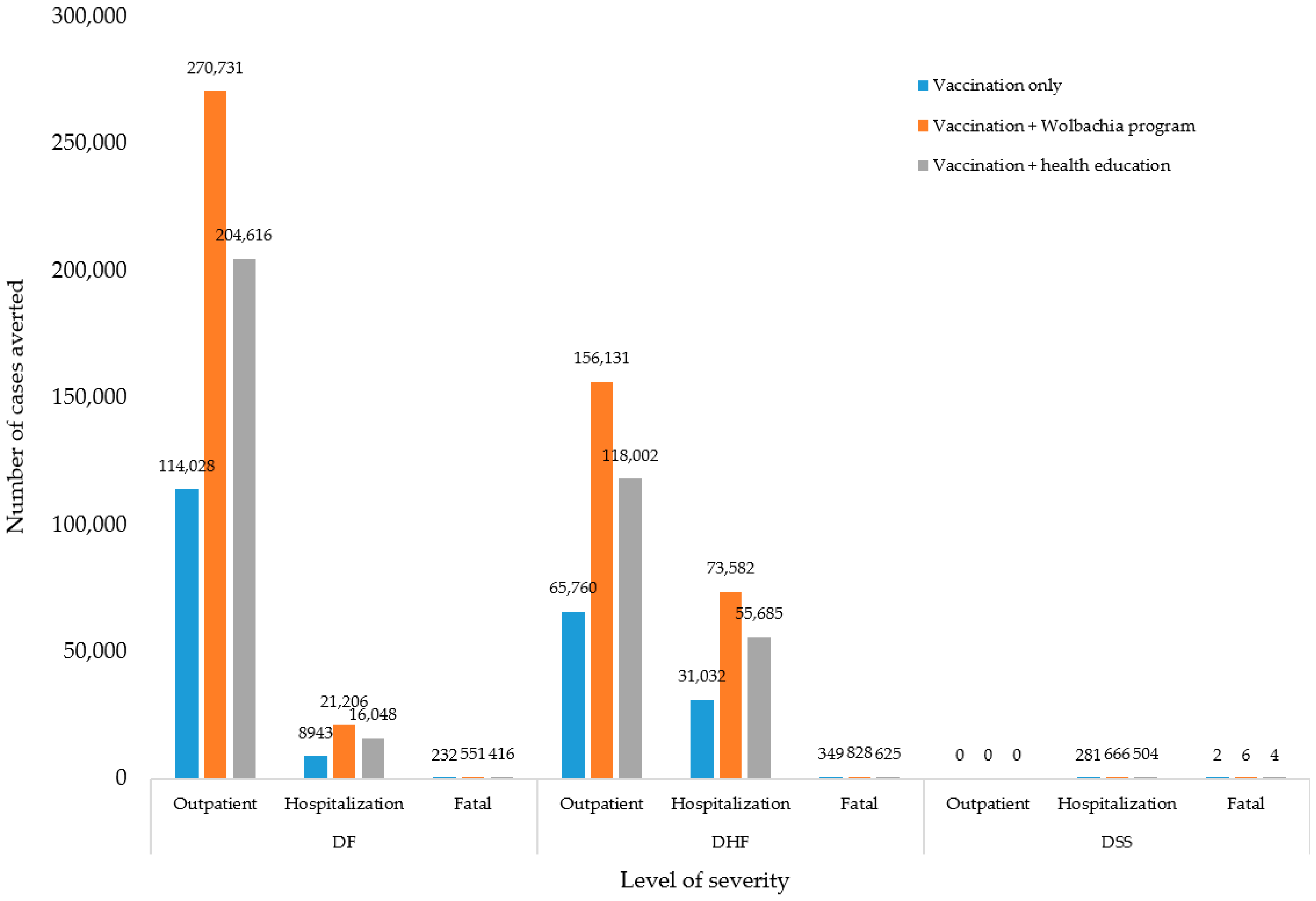
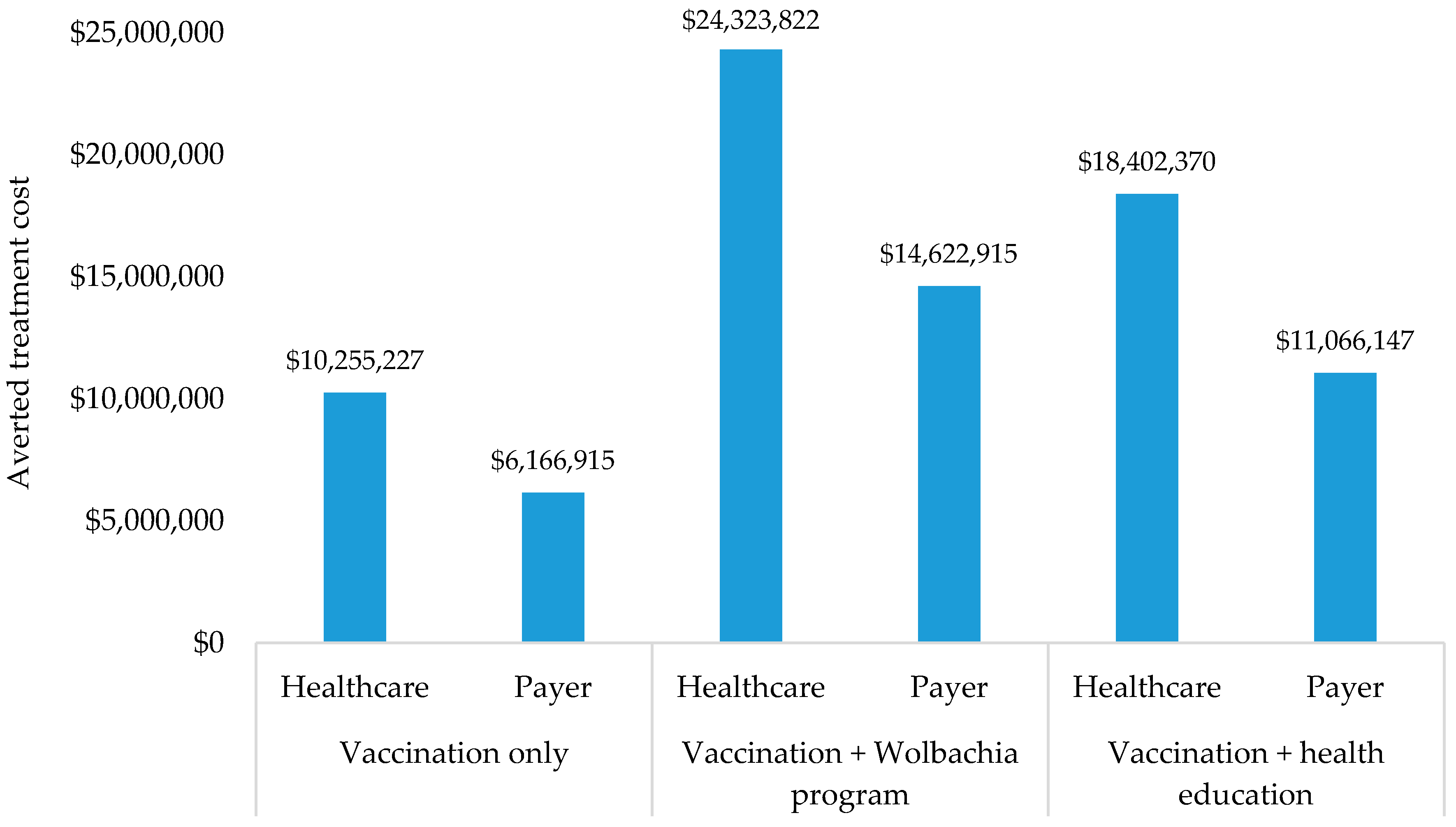
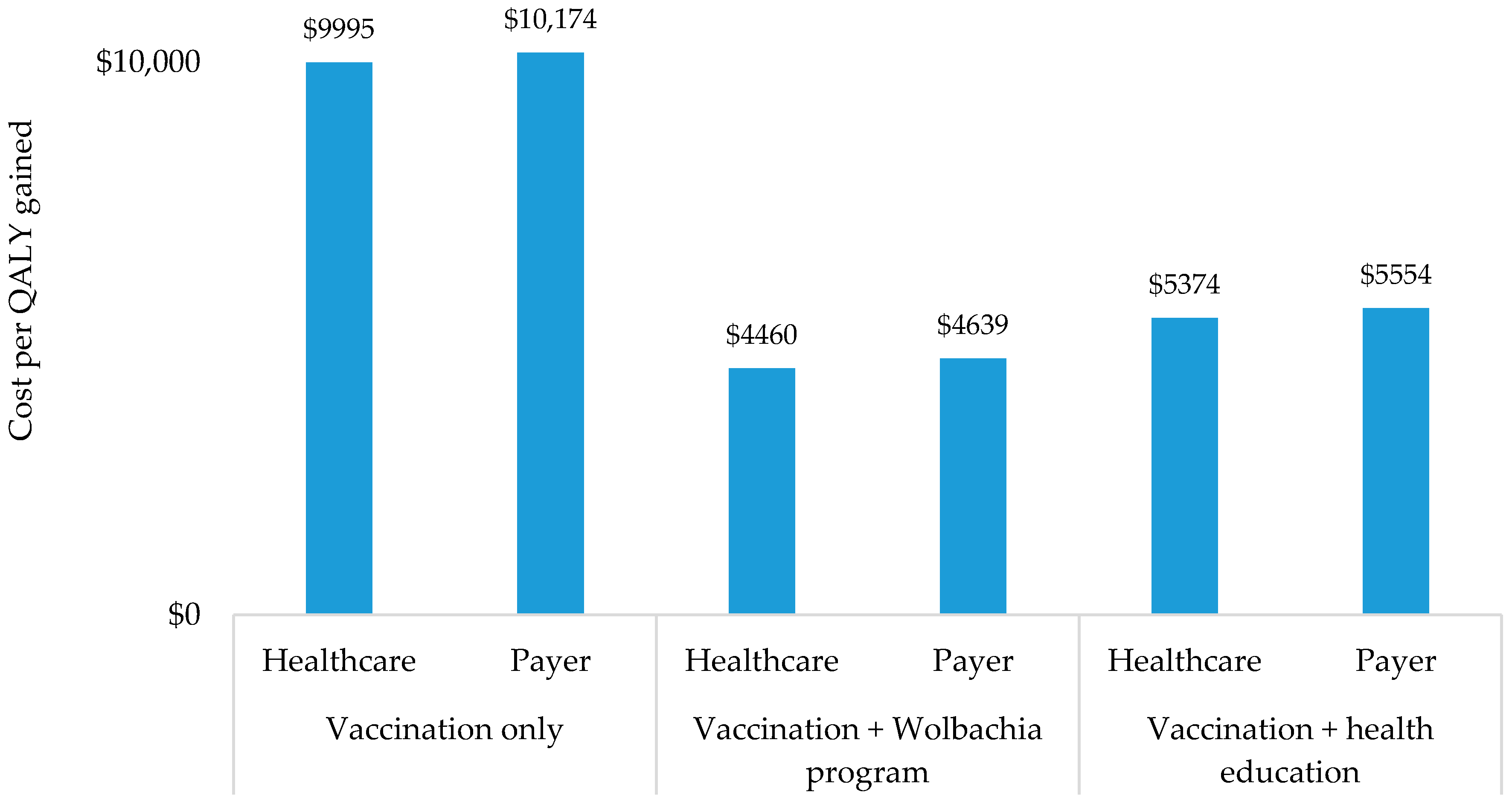
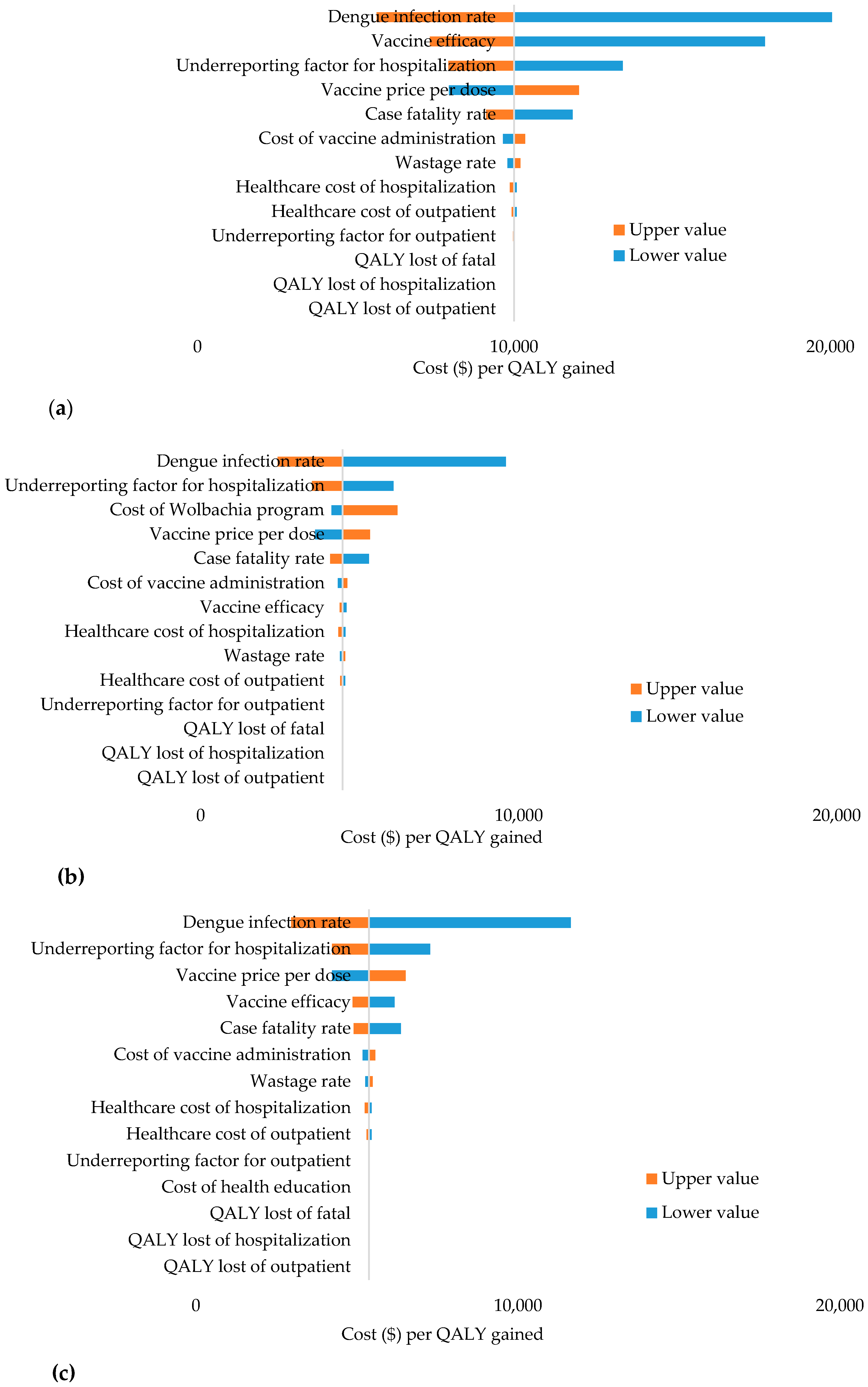
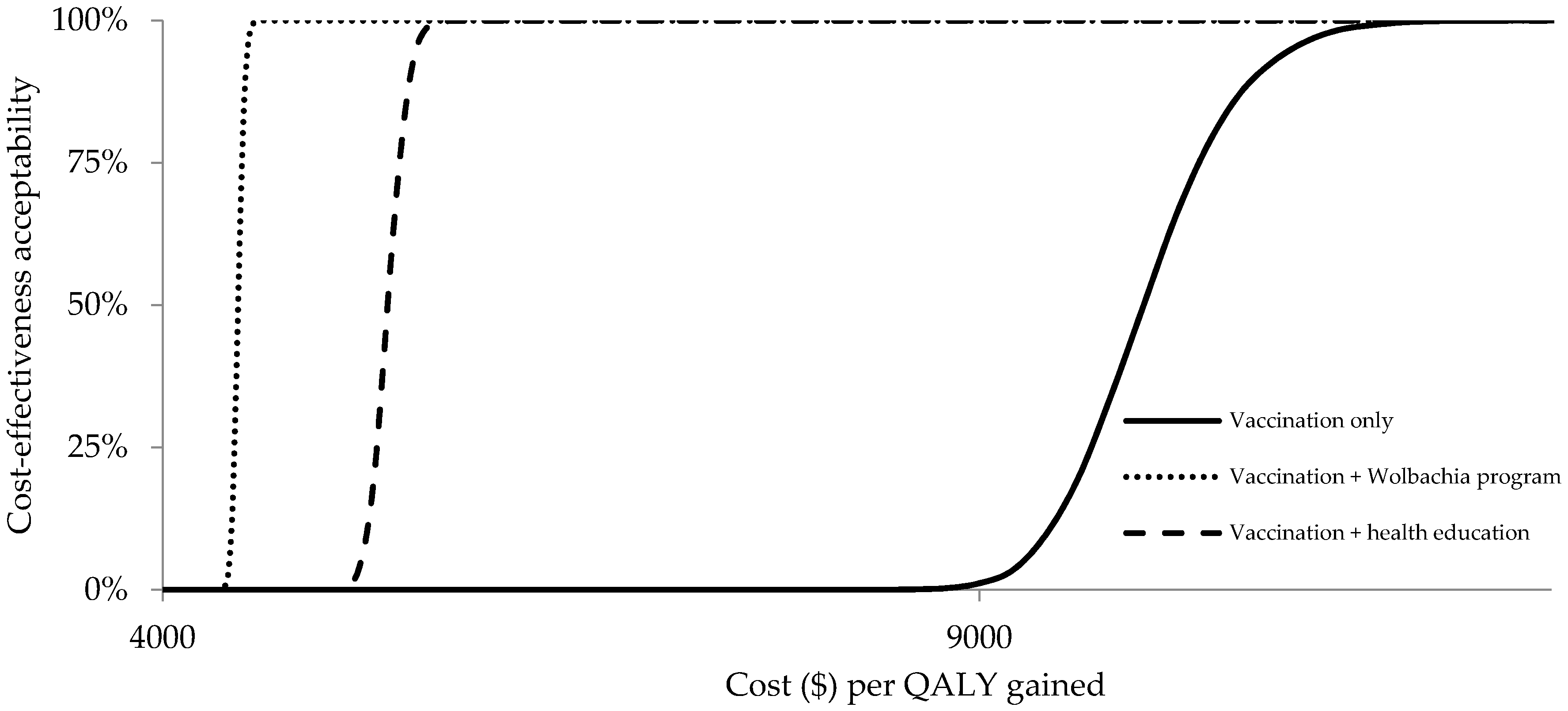
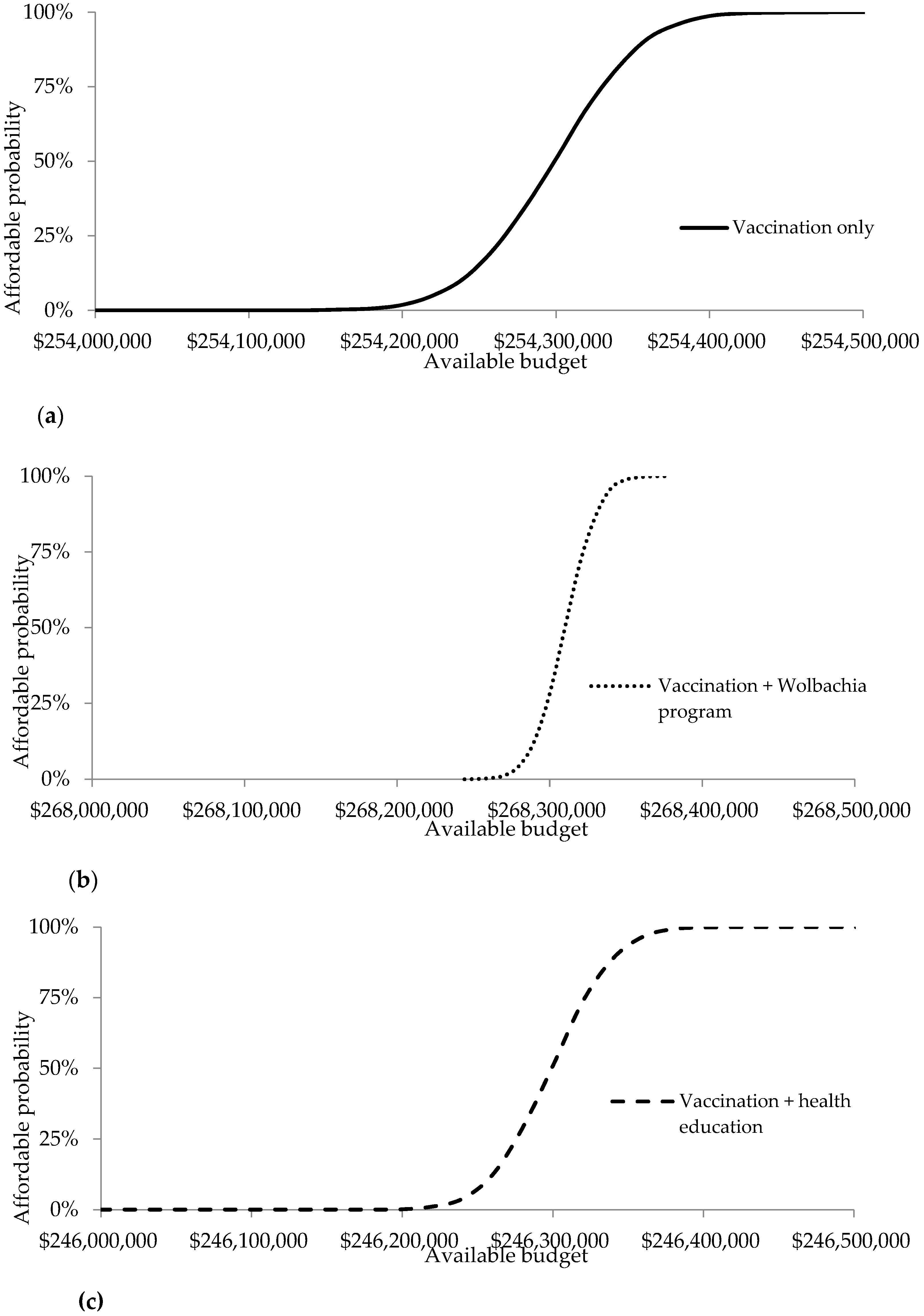
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Global Strategy for Dengue Prevention and Control; WHO Press: Geneva, Switzerland, 2012. [Google Scholar]
- Pan American Health Organization. Integrated Management Strategy for Dengue Prevention and Control in the Region of the Americas; PAHO: Washington, DC, USA, 2018. [Google Scholar]
- Martina, B.E.E.; Koraka, P.; Osterhaus, A.D.M.E. Dengue virus pathogenesis: An integrated view. Clin. Microbiol. Rev. 2009, 22, 564–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatt, S.; Gething, P.W.; Brady, O.J.; Messina, J.P.; Farlow, A.W.; Moyes, C.L.; Drake, J.M.; Brownstein, J.S.; Hoen, A.G.; Sankoh, O.; et al. The global distribution and burden of dengue. Nature 2013, 496, 504–507. [Google Scholar] [CrossRef] [PubMed]
- Stanaway, J.D.; Shepard, D.S.; Undurraga, E.A.; Halasa, Y.A.; Coffeng, L.E.; Brady, O.J.; Hay, S.I.; Bedi, N.; Bensenor, I.M.; Castaneda-Orjuela, C.A.; et al. The global burden of dengue: An analysis from the Global Burden of Disease Study 2013. Lancet Infect. Dis. 2016, 3099, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Shepard, D.S.; Undurraga, E.A.; Halasa, Y.A.; Stanaway, J.D. The global economic burden of dengue: A systematic analysis. Lancet Infect. Dis. 2016, 16, 935–941. [Google Scholar] [CrossRef]
- Nadjib, M.; Setiawan, E.; Putri, S.; Nealon, J.; Beucher, S.; Hadinegoro, S.R.; Permanasari, V.Y.; Sari, K.; Wahyono, T.Y.M.; Kristin, E.; et al. Economic burden of dengue in Indonesia. PLoS Negl. Trop. Dis. 2019, 13, e0007038. [Google Scholar] [CrossRef] [Green Version]
- Bowman, L.R.; Donegan, S.; McCall, P.J. Is dengue vector control deficient in effectiveness or evidence? Systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2016, 10, e0004551. [Google Scholar] [CrossRef] [Green Version]
- Shepard, D.S.; Halstead, S.B. Dengue (with notes on yellow fever and Japanese endephalitis). In Disease Control Priorities for Developing Countries; Jamison, D.T., Mosley, W.H., Measham, A.R., Bobadila, J., Eds.; Oxford University Press for the World Bank: New York, NY, USA, 1993; pp. 303–320. [Google Scholar]
- Zeng, W.; Halasa-Rappel, Y.A.; Baurin, N.; Coudeville, L.; Shepard, D.S. Cost-effectiveness of dengue vaccination in ten endemic countries. Vaccine 2018, 36, 413–420. [Google Scholar] [CrossRef]
- Achee, N.L.; Gould, F.; Perkins, T.A.; Reiner, R.C., Jr.; Morrison, A.C.; Ritchie, S.A.; Gubler, D.J.; Teyssou, R.; Scott, T.W. A critical assessment of vector control for dengue prevention. PLoS Negl. Trop. Dis. 2015, 9, e0003655. [Google Scholar] [CrossRef]
- Erlanger, T.E.; Keiser, J.; Utzinger, J. Effect of dengue vector control interventions on entomological parameters in developing countries: A systematic review and meta-analysis. Med. Vet. Entomol. 2008, 22, 203–221. [Google Scholar] [CrossRef]
- O’Reilly, K.M.; Hendrickx, E.; Kharisma, D.D.; Wilastonegoro, N.N.; Carrington, L.B.; Elyazar, I.R.F.; Kucharski, A.J.; Lowe, R.; Flasche, S.; Pigott, D.M.; et al. Estimating the burden of dengue and the impact of release of wMel Wolbachia-infected mosquitoes in Indonesia: A modelling study. BMC Med. 2019, 17, 172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anders, K.L.; Indriani, C.; Ahmad, R.A.; Tantowijoyo, W.; Arguni, E.; Andari, B.; Jewell, N.P.; Rances, E.; O’Neill, S.L.; Simmons, C.P.; et al. The AWED trial (applying Wolbachia to eliminate dengue) to assess the efficacy of Wolbachia-infected mosquito deployments to reduce dengue incidence in Yogyakarta, Indonesia: Study protocol for a cluster randomised controlled trial. Trials 2018, 19, 302. [Google Scholar] [CrossRef] [PubMed]
- Werren, J.H.; Baldo, L.; Clark, M.E. Wolbachia: Master manipulators of invertebrate biology. Nat. Rev. Microbiol. 2008, 6, 741–751. [Google Scholar] [CrossRef]
- Van den Hurk, A.F.; Hall-Mendelin, S.; Pyke, A.T.; Frentiu, F.D.; McElroy, K.; Day, A.; Higgs, S.; O’Neill, S.L. Impact of Wolbachia on infection with chikungunya and yellow fever viruses in the mosquito vector Aedes aegypti. PLoS Negl. Trop. Dis. 2012, 6, e1892. [Google Scholar] [CrossRef] [Green Version]
- Dutra, H.L.C.; Rocha, M.N.; Dias, F.B.S.; Mansur, S.B.; Caragata, E.P.; Moreira, L.A. Wolbachia blocks currently circulating Zika virus isolates in Brazilian Aedes aegypti mosquitoes. Cell Host Microbe 2016, 19, 771–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffmann, A.A.; Montgomery, B.L.; Popovici, J.; Iturbe-Ormaetxe, I.; Johnson, P.H.; Muzzi, F.; Greenfield, M.; Durkan, M.; Leong, Y.S.; Dong, Y.; et al. Successful establishment of Wolbachia in Aedes populations to suppress dengue transmission. Nature 2011, 476, 454–457. [Google Scholar] [CrossRef]
- Sulistyawati, S.; Astuti, F.D.; Umniyati, S.R.; Satoto, T.B.T.; Lazuardi, L.; Nilsson, M.; Rocklov, J.; Andersson, C.; Holmner, A. Dengue vector control through community empowerment: Lessons learned from a community-based study in Yogyakarta, Indonesia. Int. J. Environ. Res. Public Health 2019, 16, 1013. [Google Scholar] [CrossRef] [Green Version]
- Arneliwati; Agrina; Dewi, A.P. The effectiveness of health education using audiovisual media on increasing family behavior in preventing dengue hemorrhagic fever (DHF). Enfermeria Clinica 2019, 29, 30–33. [Google Scholar]
- Statistics Indonesia. Indonesia Population Projection 2010–2035; Statistics Indonesia: Jakarta, Indonesia, 2013. [Google Scholar]
- Prayitno, A.; Taurel, A.F.; Nealon, J.; Satari, H.I.; Karyanti, M.R.; Sekartini, R.; Soedjatmiko, S.; Gunardi, H.; Medise, B.E.; Sasmono, R.T.; et al. Dengue seroprevalence and force of primary infection in a representative population of urban dwelling Indonesian children. PLoS Negl. Trop. Dis. 2018, 12, e0006467. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Republic of Indonesia. Profil Kesehatan Indonesia 2009–2018; Ministry of Health: Jakarta, Indonesia, 2009–2018.
- Kosasih, H.; Alisjahbana, B.; Nurhayati, Q.d.M.; Rudiman, I.F.; Widjaja, S.; Antonjaya, U.; Novriani, H.; Susanto, N.H.; Jusuf, H.; Susanto, N.H.; et al. The Epidemiology, Virology and Clinical Findings of Dengue Virus Infections in a Cohort of Indonesian Adults in Western Java. PLoS Negl. Trop. Dis. 2016, 10, e0004390. [Google Scholar] [CrossRef]
- Utama, I.M.S.; Lukman, N.; Sukmawati, D.D.; Alisjahbana, B.; Anggraini, A.; Murniati, D.; Utama, I.M.G.D.L.; Puspitasari, D.; Kosasih, H.; Laksono, I.; et al. Dengue viral infection in Indonesia: Epidemiology, diagnostic challenges, and mutations from an observational cohort study. PLoS Negl. Trop. Dis. 2019, 13, e0007785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Silveira, L.T.C.; Tura, B.; Santos, M. Systematic review of dengue vaccine efficacy. BMC Infect. 2019, 19, 750. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Dengue Vaccine: WHO Position Paper—September 2018. Available online: https://apps.who.int/iris/bitstream/handle/10665/274315/WER9336.pdf?ua=1 (accessed on 3 August 2019).
- Carrasco, L.R.; Lee, L.K.; Lee, V.J.; Ooi, E.E.; Shepard, D.S.; Thein, T.L.; Gan, V.; Cook, A.R.; Lye, D.; Ng, L.C.; et al. Economic impact of dengue illness and the cost-effectiveness of future vaccination programs in Singapore. PLoS Negl. Trop. Dis. 2011, 5, e1426. [Google Scholar] [CrossRef] [PubMed]
- Shim, E. Dengue dynamics and vaccine cost-effectiveness analysis in the Philippines. Am. J. Trop. Med. Hyg. 2016, 95, 1137–1147. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Republic of Indonesia. Standar Tarif Pelayanan Kesehatan Dalam Penyelenggaraan Program Jaminan Kesehatan. Available online: https://www.depkes.go.id/resources/download/peraturan/pmk-59-thn-2014-ttg-standar-tarif-jkn.pdf (accessed on 3 August 2019).
- Forbes. Mosquito Wars—A Big Win in Australia Brings Hopeful News for Southern US. Available online: https://www.forbes.com/sites/judystone/2018/08/03/mosquito-wars-a-big-win-in-australia-brings-hopeful-news-to-florida-and-southern-us/#3f7078fa3069 (accessed on 1 March 2020).
- Stahl, H.C.; Butenschoen, V.M.; Tran, H.T.; Gozzer, E.; Skewes, R.; Mahendradhata, Y.; Runge-Ranziger, S.; Kroeger, A.; Farlow, A. Cost of dengue outbreaks: Literature review and country case studies. BMC Public Health 2013, 13, 1048. [Google Scholar] [CrossRef] [Green Version]
- World Bank. PPP Conversion Factor. Available online: https://data.worldbank.org/indicator/PA.NUS.PPP (accessed on 15 August 2019).
- World Bank. GDP Per Capita—Indonesia. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=ID (accessed on 25 August 2019).
- World Health Organization. WHO Guide for Standardization of Economic Evaluations of Immunization Programmes. Available online: https://apps.who.int/iris/bitstream/handle/10665/69981/WHO_IVB_08.14_eng.pdf?sequence=1 (accessed on 15 August 2019).
- Yakob, L.; Walker, T. Zika virus outbreak in the Americas: The need for novel mosquito control methods. Lancet Glob. Health 2016, 4, e148–e149. [Google Scholar] [CrossRef] [Green Version]
- Von Seidlein, L.; Kekulé, A.S.; Strickman, D. Novel vector control approaches: The future for prevention of Zika virus transmission? PLoS Med. 2017, 14, e1002219. [Google Scholar] [CrossRef] [Green Version]
- Walker, T.; Johnson, P.H.; Moreira, L.A.; Iturbe-Ormaetxe, I.; Frentiu, F.D.; McMeniman, C.J.; Leong, Y.S.; Axford, J.; Kriesner, P.; Lloyd, A.L.; et al. The wMel Wolbachia strain blocks dengue and invades caged Aedes aegypti populations. Nature 2011, 476, 450–453. [Google Scholar] [CrossRef]
- Harapan, H.; Rajamoorthy, Y.; Anwar, S.; Bustamam, A.; Radiansyah, A.; Angraini, P.; Fasli, R.; Salwiyadi, S.; Bastian, R.A.; Oktiviyari, A.; et al. Knowledge, attitude, and practice regarding dengue virus infection among inhabitants of Aceh, Indonesia: A cross-sectional study. BMC Infect. Dis. 2018, 18, 96. [Google Scholar] [CrossRef] [Green Version]
- Dhimal, M.; Aryal, K.K.; Dhimal, M.L.; Gautam, I.; Singh, S.P.; Bhusal, C.L.; Kuch, U. Knowledge, Attitude and Practice Regarding Dengue Fever among the Healthy Population of Highland and Lowland Communities in Central Nepal. PLoS ONE 2014, 9, e102028. [Google Scholar] [CrossRef] [Green Version]
- Supadmi, W.; Suwantika, A.A.; Perwitasari, D.A.; Abdulah, R. Economic Evaluations of Dengue Vaccination in the Southeast Asia Region: Evidence from a Systematic Review. Value Health Reg. Issues 2019, 18, 132–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suwantika, A.A.; Zakiyah, N.; Lestari, K.; Postma, M.J. Accelerating the introduction of rotavirus immunization in Indonesia. Expert Rev. Vaccines 2014, 13, 463–472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suwantika, A.A.; Beutels, P.; Postma, M.J. Cost-effectiveness of hepatitis A vaccination in Indonesia. Hum. Vaccines Immunother. 2014, 10, 2342–2349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suwantika, A.A.; Postma, M.J. Effect of breastfeeding promotion interventions on cost-effectiveness of rotavirus immunization in Indonesia. BMC Public Health 2013, 13, 1106. [Google Scholar] [CrossRef] [Green Version]
- Setiawan, D.; Dolk, F.C.; Suwantika, A.A.; Westra, T.A.; Wilschut, J.C.; Postma, M.J. Cost-Utility Analysis of Human Papillomavirus Vaccination and Cervical Screening on Cervical Cancer Patient in Indonesia. Value Health Reg. Issues 2016, 9, 84–92. [Google Scholar] [CrossRef]
- Brady, O.J.; Kharisma, D.D.; Wilastonegoro, N.N.; O’Reilly, K.M.; Hendricx, E.; Bastos, L.S.; Yakob, L.; Shepard, D.S. The potential cost-effectiveness of controlling dengue in Indonesia using wMel Wolbachia released at scale: A modelling study. medRxiv 2020. Available online: https://www.medrxiv.org/content/10.1101/2020.01.11.20017186v1.full.pdf (accessed on 25 August 2019). [CrossRef]
- Lee, B.Y.; Cannor, D.L.; Kitchen, S.B.; Bacon, K.M.; Shah, M.; Brown, S.T.; Bailey, R.R.; Laosiritaworn, Y.; Burke, D.S.; Cummings, D.A.T. Economic value of dengue vaccine in Thailand. Am. J. Trop. Med. Hyg. 2011, 84, 764–772. [Google Scholar] [CrossRef] [Green Version]
- Shepard, D.S.; Suaya, J.A.; Halstead, S.B.; Nathan, M.B.; Gubler, D.J.; Mahoney, R.T.; Wang, D.N.C.; Meltzer, M.I. Cost-effectiveness of a pediatric dengue vaccine. Vaccine 2004, 22, 1275–1280. [Google Scholar] [CrossRef]
- Shafie, A.A.; Yeo, H.Y.; Coudeville, L.; Steinberg, L.; Gill, B.S.; Jahis, R.; Amar-Singh, H.S.S. The potential cost-effectiveness of different dengue vaccination programmes in Malaysia: A value-based pricing assessment using dynamic transmission mathematical modelling. Pharmacoeconomics 2017, 35, 575–589. [Google Scholar] [CrossRef]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The Levels of Evidence and their role in Evidence-Based Medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef] [Green Version]
- Jiang, V.; Jiang, B.; Tate, J.; Parashar, U.D.; Patel, M.M. Performance of rotavirus vaccines in developed and developing countries. Hum. Vaccines 2010, 6, 532–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Parameters | Value | Distribution | Reference |
|---|---|---|---|
| Epidemiology | |||
| Dengue infection rate | 0.05% | Dirichlet | [24] |
| Case fatality rate | 0.83% | Dirichlet | [24] |
| Probability of DF | 39.80% | Dirichlet | [25,26] |
| Probability of DHF | 59.80% | Dirichlet | [25,26] |
| Probability of DSS | 0.40% | Dirichlet | [25] |
| Probability of outpatient (DF) | 68% | Dirichlet | [8] |
| Probability of hospitalization (DF) | 32% | Dirichlet | [8] |
| Probability of outpatient (DHF) | 26.10% | Dirichlet | [8] |
| Probability of hospitalization (DHF) | 73.90% | Dirichlet | [8] |
| Probability of outpatient (DSS) | 0% | Dirichlet | [8] |
| Probability of hospitalization (DSS) | 100.00% | Dirichlet | [8] |
| Expansion factor for outpatient | 45.90 | Dirichlet | [8] |
| Expansion factor for hospitalization | 7.65 | Dirichlet | [8] |
| Costs | |||
| Healthcare cost of outpatient | $19,22 | Gamma | [8] |
| Healthcare cost of hospitalization | $297,79 | Gamma | [8] |
| Payer cost of outpatient | $0,62 | Gamma | [32] |
| Payer cost of hospitalization | $227,94 | Gamma | [31] |
| Vaccine price per dose | $20,00 | Gamma | [11] |
| Cost of vaccine administration | $3,42 | Gamma | [11] |
| Cost of Wolbachia program | $3,00 | Alternative scenario | [33] |
| Cost of health education | $0,02 | Alternative scenario | [34] |
| Vaccine characteristics | |||
| Vaccine efficacy | 44.00% | Alternative scenario | [27] |
| Vaccine coverage | 87.56% | Alternative scenario | [24] |
| Schedule (3-dose for >9 years old) | 6-month interval | [30] | |
| Wastage rate | 10% | Alternative scenario | [11] |
| Utilities | |||
| QALY loss of outpatient | 0.00009 | Beta | [8,11] |
| QALY loss of hospitalization | 0.00038 | Beta | [8,11] |
| QALY loss of fatal | 1 | Beta | [8,11] |
| Others | |||
| Targeted population | 4,701,100 | Unvaried | [22] |
| Discount rate | 3.00% | Unvaried | [35] |
| Time horizon | 10 years | Unvaried |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suwantika, A.A.; Kautsar, A.P.; Supadmi, W.; Zakiyah, N.; Abdulah, R.; Ali, M.; Postma, M.J. Cost-Effectiveness of Dengue Vaccination in Indonesia: Considering Integrated Programs with Wolbachia-Infected Mosquitos and Health Education. Int. J. Environ. Res. Public Health 2020, 17, 4217. https://doi.org/10.3390/ijerph17124217
Suwantika AA, Kautsar AP, Supadmi W, Zakiyah N, Abdulah R, Ali M, Postma MJ. Cost-Effectiveness of Dengue Vaccination in Indonesia: Considering Integrated Programs with Wolbachia-Infected Mosquitos and Health Education. International Journal of Environmental Research and Public Health. 2020; 17(12):4217. https://doi.org/10.3390/ijerph17124217
Chicago/Turabian StyleSuwantika, Auliya A., Angga P. Kautsar, Woro Supadmi, Neily Zakiyah, Rizky Abdulah, Mohammad Ali, and Maarten J. Postma. 2020. "Cost-Effectiveness of Dengue Vaccination in Indonesia: Considering Integrated Programs with Wolbachia-Infected Mosquitos and Health Education" International Journal of Environmental Research and Public Health 17, no. 12: 4217. https://doi.org/10.3390/ijerph17124217
APA StyleSuwantika, A. A., Kautsar, A. P., Supadmi, W., Zakiyah, N., Abdulah, R., Ali, M., & Postma, M. J. (2020). Cost-Effectiveness of Dengue Vaccination in Indonesia: Considering Integrated Programs with Wolbachia-Infected Mosquitos and Health Education. International Journal of Environmental Research and Public Health, 17(12), 4217. https://doi.org/10.3390/ijerph17124217





