Lead Toxicity and Pollution in Poland
Abstract
:1. Introduction
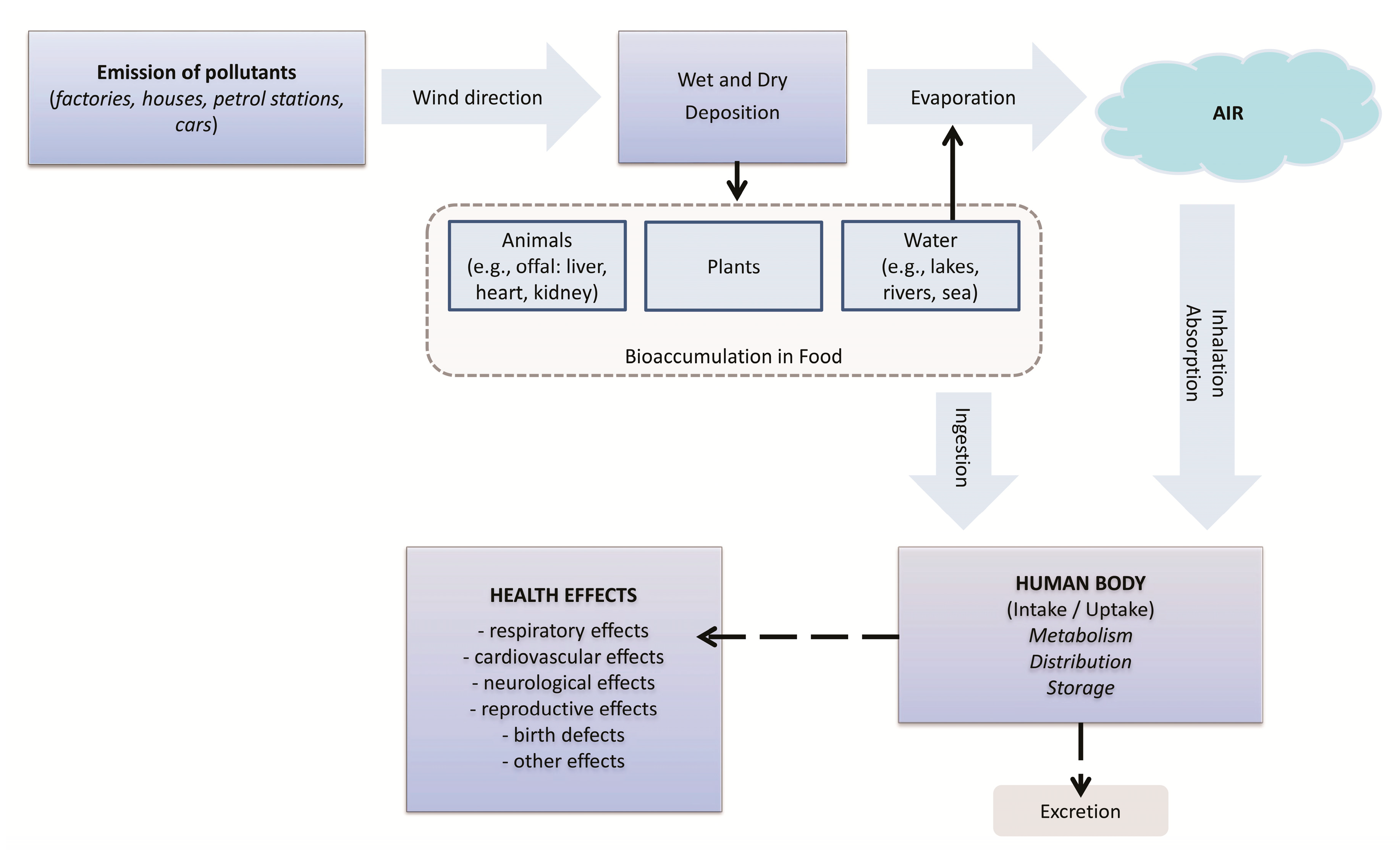
2. Lead Absorption
2.1. Lead Absorption, Excretion and Storage in Body
2.1.1. Ingestion
2.1.2. Lead in the Human Body
2.2. Lead’s Effects
2.2.1. Metabolic and Genetic Effects
2.2.2. Location of Lead in the Body
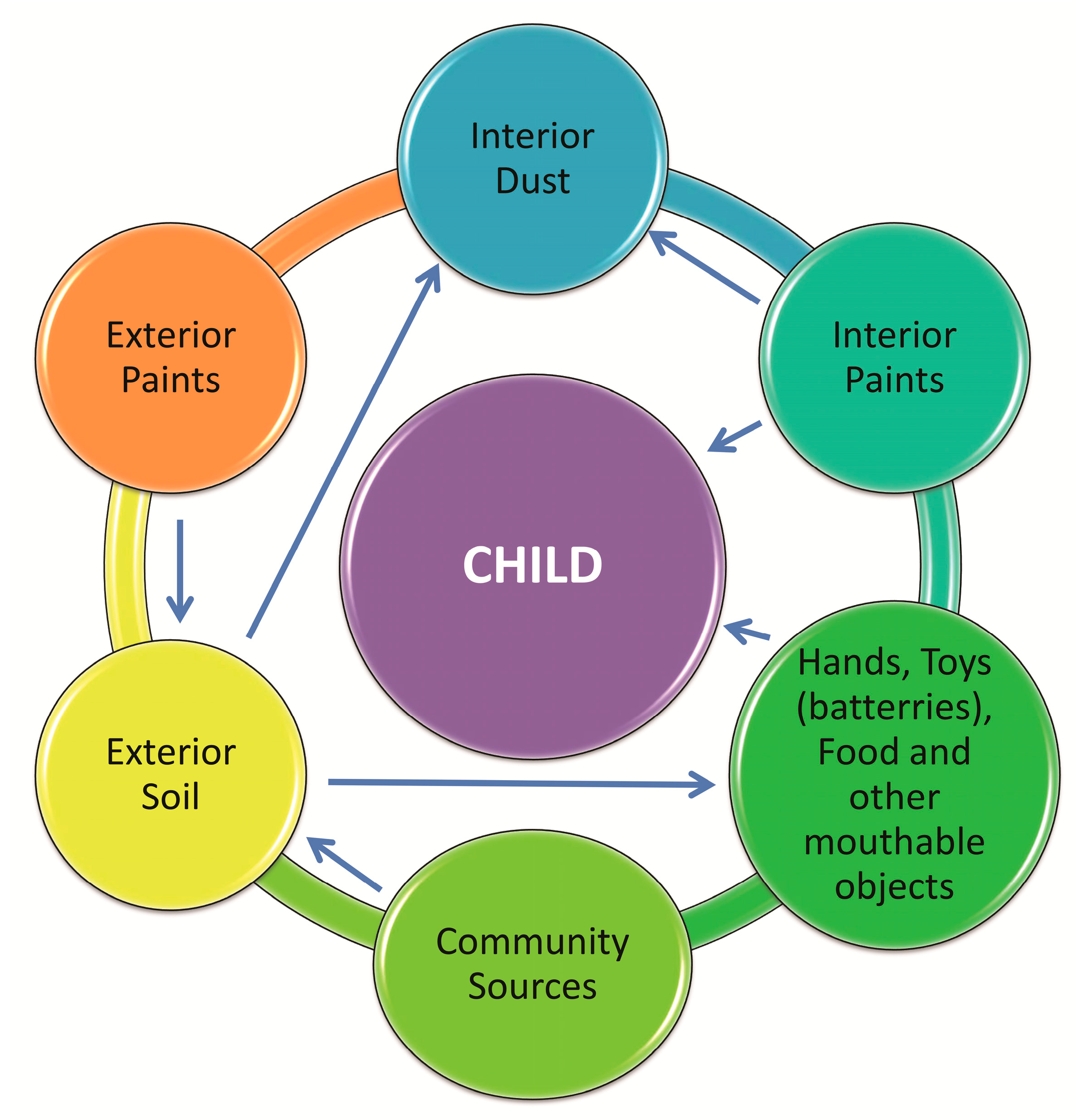
2.2.3. Children
2.2.4. Adults
2.3. Lead Exposure in Poland
2.3.1. In the Environment
2.3.2. In Paints
2.3.3. Lead in Food
2.4. Prevention and Monitoring of Lead Poisoning
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| Pb | lead |
| ALAD | aromatic l-amino acid decarboxylase |
| G6PD | glucose-6-phosphate dehydrogenase |
| δ-ALAD | δ-aminolevulinic acid dehydratase |
| δ-ALA | δ-aminolevulinic acid |
| GSH | glutathione |
| GSSG | glutathione disulfide |
| WHO | World Health Organization |
| IARC | International Agency for Research on Cancer |
References
- Krzywy, I.; Krzywy, E.; Pastuszak-Gabinowska, M.; Brodkiewicz, A. Lead—Is there something to be afraid of? Ann. Acad. Med. Stetin. 2010, 56, 118–128. [Google Scholar]
- Wani, A.L.; Ara, A.; Usmani, J.A. Lead toxicity: A review. Int. Toxicol. 2015, 8, 55–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spivey, A. The Weight of Lead: Effects Add Up in Adults. Environ. Health Perspect. 2007, 115, 30–36. [Google Scholar] [CrossRef] [Green Version]
- Giel-Pietraszuk, M.; Hybza, K.; Chełchowska, M.; Barciszewski, J. Mechanisms of lead toxicity. Adv. Cell Biol. 2012, 39, 17–248. [Google Scholar]
- ATSDR. Lead Toxicity: What Is the biological Fate of Lead in the Body? Environmental Health and Medicine Education. 2017. Available online: https://www.atsdr.cdc.gov/csem/csem.asp?csem=34&po=9 (accessed on 12 June 2017).
- ATSDR. Lead Toxicity: Case Studies in Environmental Medicine (CSEM). Environmental Health and Medicine Education. 2017. Available online: https://www.atsdr.cdc.gov/csem/lead/docs/CSEM-Lead_toxicity_508.pdf (accessed on 12 June 2019).
- Drop, B.; Janiszewska, M.; Barańska, A.; Kanecki, K.; Nitsch-Osuch, A.; Bogdan, M. Satisfaction with Life and Adaptive Reactions in People Treated for Chronic Obstructive Pulmonary Disease. In Clinical Pulmonary Research. Advances in Experimental Medicine and Biology; Pokorski, M., Ed.; Springer International Publishing: Cham, Switzerland, 2018; Volume 1114, pp. 41–47. [Google Scholar]
- Tamayo y Ortiz, M.; Téllez-Rojo, M.M.; Hu, H.; Hernandez-Avila, M.; Wright, R.; Amarasiriwardena, C.; Lupoli, N.; Mercado-Garcia, A.; Pantic, I.; Lamadrid-Figueroa, H. Lead in candy consumed and blood lead levels of children living in Mexico City. Environ. Res. 2016, 147, 497–502. [Google Scholar] [CrossRef]
- Staniak, S. Sources and levels of lead in food. Pol. J. Agron. 2014, 19, 36–45. [Google Scholar]
- Rehman, K.; Fatima, F.; Waheed, I. Prevalence of exposure of heavy metals and their impact on health consequences. J. Cell. Biochem. 2018, 119, 157–184. [Google Scholar] [CrossRef]
- Wieczorek, J.; Baran, A.; Urbański, K.; Mazurek, R.; Klimowicz-Pawlas, A. Assessment of the pollution and ecological risk of lead and cadmium in soils. Environ. Geochem. Health 2018, 40, 2325–2342. [Google Scholar] [CrossRef]
- Commission Regulation NR 1881/2006 from 19.12.2006 Setting Maximum Levels for Certain Contaminants in Foodstuffs. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32006R1881&from=EN (accessed on 20 December 2006).
- EFSA. Scientific Opinion of the Panel on Contaminants in the Food Chain. Lead in Food. Available online: https://efsa.onlinelibrary.wiley.com/doi/epdf/10.2903/j.efsa.2010.1570 (accessed on 22 March 2013).
- Sirivarasai, J.; Kaojarern, S.; Chanprasertyothin, S.; Panpunuan, P.; Petchpoung, K.; Tatsaneeyapant, A.; Yoovathaworn, K.; Sura, T.; Kaojarern, S.; Sritara, P. Environmental lead exposure, catalase gene, and markers of antioxidant and oxidative stress relation to hypertension: An analysis based on the EGAT study. Biomed. Res. Int. 2015. [Google Scholar] [CrossRef]
- Jakubowski, M. Lead and its inorganic compounds, other than lead arsenate and lead chromate as Pb, inhalable fraction. Documentation of suggested occupational exposure limits (OELs). Princ. Meth. Assess. Work. Environ. 2014, 2, 111–144. [Google Scholar]
- WHO. Preventing disease through healthy environments. Exposure to Lead: A Major Public Health Concern World Health Organization Geneva, Switzerland 2010. Available online: https://apps.who.int/iris/bitstream/handle/10665/204585/9789241565196_eng.pdf;jsessionid=42B78C18C48C9D442D642C8714FED921?sequence=1 (accessed on 11 May 2016).
- Zawadzki, M.; Poręba, R.; Gać, P. Mechanisms and toxic effects of lead on the cardiovascular system. Med. Pr. 2006, 57, 543–549. [Google Scholar] [PubMed]
- Omeljaniuk, W.; Socha, K.; Soroczyńska, J.; Charkiewicz, A.E.; Laudański, T.; Kulikowski, M.; Kobylec, E.; Szpak, A.; Borawska, M.H. Cadmium and lead in women who miscarried. Clin. Lab. 2018, 64, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Choi, H.; Hwank, U.K.; Kang, J.C.; Kang, Y.J.; Kim, K.I.; Kim, J.H. Toxic effects of lead exposure on bioaccumulation, oxidative stress, neurotoxicity, and immune responses in fish: A review. Environ. Toxicol. Pharmacol. 2019, 68, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Pinon-Lataillade, G.; Thoreux-Manlay, A.; Coffigny, H.; Monchaux, G.; Masse, R.; Soufir, J.C. Effect of ingestion and inhalation of lead on the reproductive system and fertility of adult male rats and their progeny. Hum. Exp. Toxicol. 1993, 12, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Zhushan, F.; Shuhua, X. The effects of heavy metals on human metabolism. Toxicol. Mech. Meth. 2020, 30, 167–176. [Google Scholar] [CrossRef]
- Fernando, B., Jr.; Tanus-Santos, J.E.; Gerlach, R.F.; Parsons, P.J. A Critical Review of Biomarkers Used for Monitoring Human Exposure to Lead: Advantages, Limitations, and Future Needs. Environ. Health Perspec. 2005, 113, 1669–1674. [Google Scholar] [CrossRef] [Green Version]
- Freire, C.; Vrhovnik, P.; Fiket, Ž.; Alcedo-Bellido, I.; Echeverría, R.; Martín-Olmedo, P.; Kniewald, G.; Fernández, M.F.; Arrebola, J.P. Adipose tissue concentrations of arsenic, nickel, lead, tin, and titanium in adults from GraMo cohort in Southern Spain: An exploratory study. Sci. Total Environ. 2020, 137458. [Google Scholar] [CrossRef]
- WHO. Expert Consultation. Available Evidence for the Future Update of the WHO Global Air Quality Guidelines (AQGs) (2016). Available online: https://www.euro.who.int/__data/assets/pdf_file/0013/301720/Evidence-future-update-AQGs-mtg-report-Bonn-sept-oct-15.pdf (accessed on 1 December 2015).
- Centers for Disease Control and Prevention (CDC). Guidelines for the Identification and Management of Lead Exposure in Pregnant and Lactating Women. Atlanta. 2010. Available online: https://www.cdc.gov/nceh/lead/publications/leadandpregnancy2010.pdf (accessed on 27 July 2012).
- Bellinger, D.C. Prenatal exposures to environmental chemicals and children’s Neurodevelopment: An update. Saf. Health Work 2013, 4, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Zhang, A.; Hu, H.; Sánchez, B.N.; Ettinger, A.S.; Park, S.K.; Cantonwine, D.; Schnaas, L.; Wright, R.O.; Lamadrid-Figueroa, H.; Tallez-Rojo, M.M. Association between prenatal lead exposure and blood pressure in children. Environ. Health Perspect. 2012, 120, 445–450. [Google Scholar] [CrossRef]
- Poręba, R.; Gać, P.; Poręba, M.; Derkacz, A.; Pilecki, W.; Antonowicz-Juchniewicz, J.; Andrzejak, R. Relationship between chronic exposure to lead, cadmium and manganese, blood pressure values and incidence of arterial hypertension. Med. Pr. 2010, 61, 5–14. [Google Scholar]
- Lanphear, B.P.; Rauch, S.; Auinger, P.; Allen, R.W.; Hornung, R.W. Low-level lead exposure and mortality in US adults: A population-based cohort study. Lancet Public Health 2018, 3, 177–184. [Google Scholar] [CrossRef]
- Gump, B.B.; Stewart, P.; Reihman, J.; Lonky, E.; Darvill, T.; Matthews, K.A.; Parsons, P.J. Prenatal and early childhood blood lead levels and cardiovascular functioning in 9½ year old children. Neurotoxicol. Teratol. 2005, 27, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Navas-Acien, A.; Guallar, E.; Silbergeld, E.K.; Rothenberg, S.J. Lead Exposure and Cardiovascular Disease—A Systematic Review. Environ. Health Perspect. 2007, 115, 472–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahn, J.; Park, M.Y.; Kang, M.-Y.; Shin, I.-S.; An, S.; Kim, H.-R. Occupational Lead Exposure and Brain Tumors: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 3975. [Google Scholar] [CrossRef]
- Steenland, K.; Barry, V.; Anttila, A.; Sallmen, M.; Mueller, W.; Ritchie, P.; McElvenny, M.D.; Straif, K. Cancer incidence among workers with blood lead measurements in two countries. Occup. Environ. Med. 2019, 76, 603–610. [Google Scholar] [CrossRef]
- Feng, W.; Cui, X.; Liu, B.; Liu, C.; Xiao, Y.; Lu, W.; Guo, H.; He, M.; Zhang, X.; Yuan, J.; et al. Association of urinary metal profiles with altered glucose levels and diabetes risk: A population-based study in China. PLoS ONE 2015, 10, e0123742. [Google Scholar] [CrossRef]
- Szyczewski, P.; Siepak, J.; Niedzielski, P.; Sobczyński, T. Research on Heavy Metals in Poland. Pol. J. Environ. Stud. 2009, 18, 755–768. [Google Scholar]
- Domańska, W. Environment 2018, Statistics Poland, Spatial and Environmental Surveys Department, Warsaw, Poland 2018. Available online: https://stat.gov.pl/obszary-tematyczne/srodowisko-energia/srodowisko/ochrona-srodowiska-2018,1,19.html (accessed on 29 November 2019).
- Staszewski, T.; Łukasik, W.; Kubiesa, P. Contamination of Polish national parks with heavy metals. Environ. Monit. Assess. 2012, 184, 4597–4608. [Google Scholar] [CrossRef]
- Charkiewicz, A.E.; Omeljaniuk, W.J.; Orywal, K.; Czygier, M.; Szmitkowski, M.; Mroczko, B.; Maślach, D.; Szpak, A. Concentration of selected elements and antioxidative potential in a group of males working in the metal industry. Am. J. Men Health 2019, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Commission Regulation (EC) No 420/2011 of 29.04.2011 amending Regulation (EC) No 1881/2006 Establishing Maximum Levels for Certain Contaminants in Foodstuffs. Available online: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2011:111:0003:0006:EN:PDF (accessed on 29 April 2011).
- Gajewska, M.; Czajkowska-Mysłek, A. The estimation of content of cadmium and lead in culinary herbs and spices available in retail sale. Brom. Chem. Toksykol. 2016, 2, 203–209. [Google Scholar]
- Kot, A.; Zaręba, S.; Wyszogrodzka-Koma, L. Assessment of lead contamination in cereals, cereal products and potatoes from Lublin Region. Food Sci. Technol. Qual. 2009, 4, 86–91. [Google Scholar]
- Fiłon, J.; Karwowska, A.; Karczewski, J.; Kmiecik, G. Lead content in cereal products from the area of Podlasie province. Brom. Chem. Toksykol. 2011, 3, 748–753. [Google Scholar]
- Duma, P.; Zin, M.; Znamirowska, A.; Woźnica, A. Analysis of lead content in the animal products in sub-carpathian province. PNiTPRS 2011, 66, 144–162. [Google Scholar]
- Pietrzak-Fiećko, R.; Bakuła, S.; Jakubowska, D.; Smoczyński, S.S. Cadmium and lead contents in drinking milk from selected regions of Poland. Environ. Med. 2013, 16, 15–19. [Google Scholar]
- Żurek, N.; Szwerc, W.; Bilek, M.; Kocjan, R. Heavy metals content in the well water from the agricultural area. Brom. Chem. Toksykol. 2017, 2, 140–148. [Google Scholar]
- Charkiewicz, A.E.; Jamiołkowski, J.; Pędziński, B.; Krzyżak, M.; Maślach, D.; Szpak, A.; Omeljaniuk, W.J. Changes in dietary patterns and the nutritional status in men in the metallurgical industry in Poland over a 21-year period. Ann. Nutr. Metab. 2018, 72, 161–171. [Google Scholar] [CrossRef]
- Piotrowska, D.E.; Pędziński, B.; Jankowska, D.; Huzarska, D.; Charkiewicz, A.E.; Szpak, A.S. Socio-economic inequalities in the use of dental care in urban and rural areas in Poland. Ann. Agric. Environ. Med. 2018, 25, 512–516. [Google Scholar] [CrossRef] [Green Version]
- Trzcinka-Ochocka, M.; Jakubowski, M.; Nowak, U. Effectiveness of preventive actions for lead exposed workers: An assessment based on biological monitoring. Med. Pr. 2006, 57, 537–542. [Google Scholar]
- Nieć, J.; Marchwińska-Wyrwał, E. Review of researches and prevention activities related to exposure to heavy metals of Silesian children. Pol. Rev. Health Sci. 2017, 1, 141–142. [Google Scholar] [CrossRef]

| Blood Lead Level (µg/L) | Degrees of Lead Poisoning | Symptoms | |
|---|---|---|---|
| Adults | Children | ||
| <10 | low | passing through the placenta into the fetal bloodstream | IQ reduction, learning and memory disabilities, growth disorders, reduced development, motor coordination, hearing, speech and verbal skills, symptoms of hyperactivity |
| 10–40 | mild | elevated blood pressure, slowed nerve conduction | deceleration of nerve conduction and vitamin D metabolism, impaired hemoglobin synthesis, sporadic intestinal discomfort, muscle pain, irritability, fatigue, apathy |
| 40–70 | moderate | drowsiness, fatigue, mood swings, reduced mental abilities, impaired fertility, chronic hypertension, impaired hemoglobin synthesis | difficulty concentrating, trembling, fatigue, muscular weakness, headache, vomiting, constipation, weight loss |
| 70–100 | serious | metallic taste in the mouth, constipation, headaches, abdominal pain, insomnia, memory loss, decreased sex drive, nephropathy | colic (severe intestinal musculoskeletal contractions), lead limbs (dark teeth and/or gums), anemia, nephropathy, encephalopathy, paralysis |
| >100 | acute poisoning | encephalopathy, anemia, death (> 150 µg/L) | convulsions, death (usually below 150 µg/L) |
| Lead’s Effects | Summary | |
|---|---|---|
| Metabolic and Genetic Effects | Impairs multiple biochemical processes | |
| Interacts with biological molecules | ||
| Reduces the activity of various enzymes | ||
| Causes oxidative stress | ||
| Causes gene expression alterations | ||
| Inhibits the enzyme ferrochelatase | ||
| Can causes rapid depletion of antioxidants in the body | ||
| Can increase the production of reactive oxygen, as well as reactive forms of nitrogen | ||
| Location of Lead in the Body | Most lead is stored in the bones | |
| Bone-to-blood lead mobilization increases during advanced age | ||
| Calcium deficiency is exacerbated, bone-to-blood lead mobilization | ||
| Children | Adversely affects the central nervous system and development of children | |
| Can interfere with the ability to learn, impair memory, lower IQ and interfere with growth and development | ||
| Can affect speech and hearing, cause hyperactivity, nerve conduction, intestinal discomfort, constipation | ||
| Vomiting, weight loss muscle aches | ||
| Can lead to anemia, nephropathy, paralysis, convulsions or death | ||
| Damage can begin as early as pregnancy | ||
| Increases the risk of miscarriage, stillbirth, low birth weight and underdeveloped children | ||
| Children are lead exposed via inhalation and ingestion | ||
| Increased risk occurs in families where one parent works in an environment where high levels of lead are present | ||
| Adults | Can result in serious morphological and functional changes in some organs | |
| Can cause changes in the nervous system, the circulatory system, the gastrointestinal system | ||
| Hormonal, astringency of the mouth, metallic taste in the mouth, and thirst or death | ||
| Affects myocytes of the muscular layer of blood vessels | ||
| Can result in an increase in blood pressure (not firmly established) | ||
| Can adversely affect blood and the metabolism of blood cells | ||
| Can have adverse effects on the nervous system, fertility, miscarriages |
| Food Product | Threshold Content (mg/kg Fresh Matter) |
|---|---|
| Milk | 0.02 |
| Meat (bovine animals, sheep, pig, poultry) | 0.1 |
| Offal (bovine animals, sheep, pig, poultry) | 0.5 |
| Fish | 0.3 |
| Cereal | 0.2 |
| Vegetable (leaf, fresh herbs, fungi, seaweed) | 0.1–0.3 |
| Potatoes | 0.1 |
| Fruits | 0.1–0.2 |
| Fat and oil | 0.1 |
| Honey | 0.1 |
| Drinking water | 0.1* |
| Lead’s Exposure | Summary |
|---|---|
| In the environment | Poland has the richest Pb deposits in Europe |
| Pb has been widely used since the 12th Century | |
| Lead in gasoline was a major pollutant for much of the 20th Century | |
| The south-west regions of the country are the most polluted, caused by higher levels of industrial activity and transboundary transport | |
| The most polluted air occurs in the vicinity of mines and metalworks | |
| Pb generally ranks first as a pollutant in waste management, second in industries burning coal, and third in road transport | |
| The work environment is a significant source of Pb exposure | |
| In paints | Present in paints manufactured before 1978 |
| Can still be found on many painted surfaces in older homes | |
| Repainting and renovations can create a serious problem with lead dust | |
| Old lead paint can contaminate the soil | |
| In food | Nearly all agricultural soils are characterized by some natural Pb |
| Lead absorption by plants depends on the properties of the soil, the characteristic features of the species and the physiological state of the plant | |
| An important source of contamination of food products can be technological processes and devices used in food production | |
| Pb contamination depends on the infrastructure of the area and industry |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charkiewicz, A.E.; Backstrand, J.R. Lead Toxicity and Pollution in Poland. Int. J. Environ. Res. Public Health 2020, 17, 4385. https://doi.org/10.3390/ijerph17124385
Charkiewicz AE, Backstrand JR. Lead Toxicity and Pollution in Poland. International Journal of Environmental Research and Public Health. 2020; 17(12):4385. https://doi.org/10.3390/ijerph17124385
Chicago/Turabian StyleCharkiewicz, Angelika Edyta, and Jeffrey R. Backstrand. 2020. "Lead Toxicity and Pollution in Poland" International Journal of Environmental Research and Public Health 17, no. 12: 4385. https://doi.org/10.3390/ijerph17124385
APA StyleCharkiewicz, A. E., & Backstrand, J. R. (2020). Lead Toxicity and Pollution in Poland. International Journal of Environmental Research and Public Health, 17(12), 4385. https://doi.org/10.3390/ijerph17124385





