Redesigning Portable Health Clinic Platform as a Remote Healthcare System to Tackle COVID-19 Pandemic Situation in Unreached Communities
Abstract
:1. Introduction
- How to redesign RHS such as the PHC platform to achieve the goal more effectively in a pandemic situation like COVID-19?
- How to ensure coverage of underserved rural populations who have comparatively less access to healthcare facilities?
- How can the RHS platform like PHC be adapted to accommodate emergency response situations like COVID-19?
2. Evaluation of eHealth System During Emergency
3. Design Methodology
3.1. Primary Screening and Triage
3.2. Prevention and Control (Isolation and Quarantine)
3.3. Traceability and Privacy
4. Results
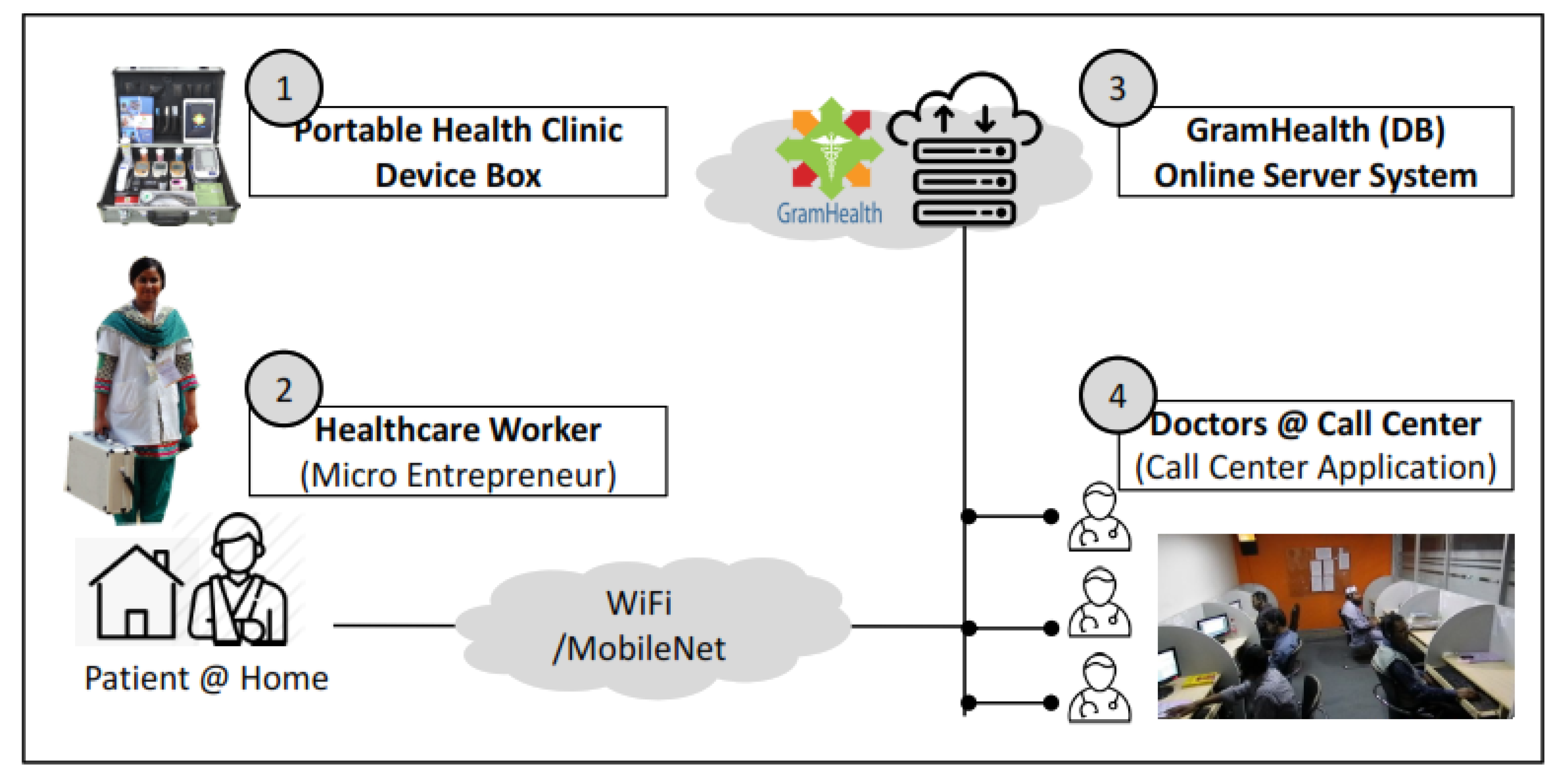
4.1. Redesigned PHC for COVID-19
4.2. Primary Screening and Triaging: Questionnaire and Measurement
4.3. Isolation and Quarantine
4.4. Traceability and Privacy
5. Discussion
- (1)
- a primary-level screening mechanism that can demonstrably reduce the burden of NCD-related complications among COVID-19 patients and that can directly contribute to the reduction of the incidence of NCDs by timely advice and treatment;
- (2)
- a primary healthcare service platform for underserved populations in remote regions of developing countries and now mature enough to be adapted to respond to large-scale public health emergencies such as COVID-19 to impact the reduction of associated mortality and morbidities;
- (3)
- a reliable platform for early detection of NCDs and associated comorbidities among target populations and for effectively contributing to a tangible reduction in the burden of disease;
- (4)
- a key ancillary mechanism for controlling patient-to-caregiver transmission of COVID-19 by creating physical distance between all except diagnosed cases and attending clinical staff;
- (5)
- evidence for health authorities to choose eHealth technologies, such as a PHC service, to provide primary healthcare services simultaneously for COVID-19 and NCDs, including video consultation with physicians, preventive health education, and awareness at the grassroots, and to encourage well-being behaviors;
- (6)
- an effective outreach tool for controlling NCDs and for decreasing the burden of disease on the target community;
- (7)
- a new approach to responding to large-scale public health emergencies like COVID-19 and to contributing directly to building adaptive resilience among populations at risk.
6. Limitations
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Feng, Z.; Li, Q.; Zhang, Y.; Wu, Z.; Dong, X.; Ma, H.; Yin, D.; Lyu, K.; Wang, D.; Zhou, L.; et al. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19). China CDC Wkly. 2020, 2, 113–122. [Google Scholar]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cascella, M.; Rajnik, M.; Cuomo, A.; Dulebohn, S.C.; di Napoli, R. Features, Evaluation and Treatment Coronavirus (COVID-19); StatPearls Publishing: Treasure Island, FL, USA, 2020.
- Chan, J.F.; Yuan, S.; Kok, K.H.; To, K.K.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.; Poon, R.W.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Liao, X.; Qian, S.; Yuan, J.; Wang, F.; Liu, Y.; Wang, Z.; Wang, F.S.; Liu, L.; Zhang, Z. Community Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, Shenzhen, China. Emerg. Infect. 2020, 26. [Google Scholar] [CrossRef]
- Ong, S.W.; Tan, Y.K.; Chia, P.Y.; Lee, T.H.; Ng, O.T.; Wong, M.S.; Marimuthu, K. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) from a Symptomatic Patient. JAMA J. Am. Med Assoc. 2020, 323, 1610–1612. [Google Scholar] [CrossRef] [Green Version]
- WHO_Scientific_Brief. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. 2020. Available online: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed on 14 June 2020).
- Kamruzzaman, M.; Sakib, S.N. Bangladesh Imposes Total Lockdown over COVID-19. Anadolu Agency. 2020. Available online: https://www.aa.com.tr/en/asia-pacific/bangladesh-imposes-total-lockdown-over-covid-19/1778272 (accessed on 14 June 2020).
- WHO_Bangladesh. Global Health Workforce Alliance. 2020. Available online: https://www.who.int/workforcealliance/countries/bgd/en/ (accessed on 13 June 2020).
- WHO_Situation Report-144. Coronavirus Disease (COVID-19); WHO: Geneva, Switzerland, 2020.
- Hoque, A. Salute, the Heroes. Daily Prothom Alo. Available online: https://www.prothomalo.com/bangladesh/article/1663413/ (accessed on 18 June 2020).
- Kashem, A. Private Hospitals to Lose Licence for Refusing Emergency Patients or Anybody|The Business Standard. The Business Standard. 2020. Available online: https://tbsnews.net/bangladesh/health/private-hospitals-lose-licence-refusing-covid-19-patients-80218 (accessed on 13 June 2020).
- Mohiuddin, A.K. Covid-19 Situation in Bangladesh. Preprints 2020. [Google Scholar] [CrossRef]
- Corraya, S. Bangladesh COVID-19 is Spreading: 100 Deaths and 170 Infzected Doctors. 2020. Available online: http://www.asianews.it/news-en/COVID-19-is-spreading:-100-deaths-and-170-infected-doctors-49878.html (accessed on 23 April 2020).
- Worldometer_Coronavirus Age, Sex, Demographics (COVID-19). Age, Sex, Existing Conditions of COVID-19 Cases and Deaths. 2020. Available online: https://www.worldometers.info/coronavirus/coronavirus-age-sex-demographics/ (accessed on 26 March 2020).
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. e-Health 2020, 26, 377–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, A.; Rebeiro-Hargrave, A.; Nohara, Y.; Kai, E.; Ripon, Z.H.; Nakashima, N. Targeting Morbidity in Unreached Communities Using Portable Health Clinic System. IEICE Trans. Commun. 2014, 97, 540–545. [Google Scholar] [CrossRef] [Green Version]
- Islam, R.; Nohara, Y.; Rahman, M.J.; Sultana, N.; Ahmed, A.; Nakashima, N. Portable health clinic: An advanced tele-healthcare system for unreached communities. Stud. Health Technol. Inform. 2019, 264, 616–619. [Google Scholar] [PubMed]
- Sampa, M.B.; Hossain, M.N.; Hoque, M.R.; Islam, R.; Yokota, F.; Nishikitani, M.; Fukuda, A.; Ahmed, A. Influence of Factors on the Adoption and Use of ICT-Based eHealth Technology by Urban Corporate People. J. Serv. Sci. Manag. 2020, 13, 1–19. [Google Scholar]
- Hollander, J.E.; Brendan, G.C. Virtually Perfect? Telemedicine for Covid-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Sugimoto, M.; Rebeiro-Hargrave, A.; Nohara, Y.; Moriyama, M.; Ahmed, A.; Shimizu, S.; Nakashima, N. Mobile Healthcare System for Health Checkups and Telemedicine in Post-Disaster Situations. Stud. Health Technol. Inform. 2015, 216, 79–83. [Google Scholar] [PubMed]
- Yokota, F.; Ahmed, A.; Islam, R.; Nishikitani, M.; Kikuchi, K.; Nohara, Y.; Okajima, H.; Kitaoka, H.; Nakashima, N. Relationships among hypertension, diabetes, and proteinuria and their risk factors in rural adults from Bheramara Upazila, Bangladesh -Findings from portable health clinic data. Int. J. Med. Res. Health Sci. 2018, 7, 1–12. [Google Scholar]
- Huang, S.; Zhang, D.; Zhang, X. Integrative Administration System of Preventive and Health Care Information in Hospital Based on HIS. J. Prev. Med. Inf. 2007. Available online: http://en.cnki.com.cn/Article_en/CJFDTOTAL-YFYX200704020.htm (accessed on 29 June 2020).
- Zhong, C.; Tao, Y.; Zhang, Z. Administrative Information System for Epidemic Situation Report of Infectious Diseases. Chin. J. Nosoconmiol. 2005, 12. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-ZHYY200512033.htm (accessed on 29 June 2020).
- Farias, D.R.; Raffo, L.; Bacigalupo, S.; Cremaschi, M.; Vence, L.; Ramos, S.; Salguero, A.; Claudio, M.; Meites, E.; Cubito, A. Data for decision making: Strategic information tools for hospital management during a pandemic. Disaster Med. Public Health Prep. 2010, 4, 207–212. [Google Scholar] [CrossRef]
- Timpka, T.; Olvander, C.; Hallberg, N. Information system needs in health promotion: A case study of the Safe Community programme using requirements engineering methods. Health Inform. J. 2008, 14, 183–193. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Zhou, L.; Yang, Y.; Peng, W.; Wang, W.; Chen, X. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir. Med. 2020, 8, e11–e12. [Google Scholar] [CrossRef] [Green Version]
- Pappot, N.; Taarnhøj, G.A.; Pappot, H. Telemedicine and e-Health Solutions for COVID-19: Patients’ Perspective. Telemed. e-Health 2020, 26, 10–12. [Google Scholar] [CrossRef]
- Ting, D.S.W.; Carin, L.; Dzau, V.; Wong, T.Y. Digital Technology and COVID-19. Nat. Med. 2020, 26, 459–461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omboni, S. Telemedicine During The COVID-19 in Italy: A Missed Opportunity? Telemed. e-Health 2020, 19–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MBS Online. 2020. Available online: http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Home (accessed on 22 April 2020).
- CARES_Act. Coronavirus Aid, Relief, and Economic Security; CARES_Act: Washington, DC, USA, 2020.
- Schwartz, J.; King, C.-C.; Yen, M.-Y. Protecting Health Care Workers during the COVID-19 Coronavirus Outbreak-Lessons from Taiwan’s SARS response. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [Green Version]
- Chang, D.; Xu, H.; Rebaza, A.; Sharma, L.; Cruz, C.S.D. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir. Med. 2020, 8, e13. [Google Scholar] [CrossRef] [Green Version]
- Handel, A.A.; Miller, J.C.; Ge, Y.; Fung, I.C. If long-term suppression is not possible, how do we minimize mortality for COVID-19 and other emerging infectious disease outbreaks? Preprint 2020. [Google Scholar] [CrossRef] [Green Version]
- WHO. Clinical Management of Severe Acute Respiratory Infection when COVID-19 is Suspected (v1.2); WHO: Geneva, Switzerland, 2020. [Google Scholar]
- WHO. Considerations in the Investigation of Cases and Clusters of COVID-19: Interim Guidance; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- WHO. Infection Prevention and Control during Halth Care when Novel Coronavirus (nCOV) Infection is Suspected; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Baskerville, R.; Baiyere, A.; Gregor, S.; Hevner, A.; Rossi, M. Design Science Research Contributions: Finding a Balance between Artifact and Theory. J. Assoc. Inf. Syst. 2018, 19, 358–376. [Google Scholar] [CrossRef] [Green Version]
- Gregor, S. Building Theory in the Sciences of the Artificial. In Proceedings of the 4th International DESRIST Conference, Philadelphia, PA, USA, 7 May 2009. [Google Scholar]
- Ahmed, A.; Rebeiro-Hargrave, A.; Nohara, Y.; Maruf, R.I.; Ghosh, P.P.; Nakashima, N.; Yasuura, H. Portable health clinic: A telehealthcare system for unreached communities. In Smart Sensors and Systems; Springer International Publishing: Cham, Switzerland, 2015; pp. 447–467. [Google Scholar]
- Sampa, M.B.; Hoque, R.; Hossain, N. Impacts of Anthropometric, Biochemical, Socio- Demographic, and Dietary Habits Factors on the Health Status of Urban Corporate People in a Developing Country. Healthcare 2020, 8, 188. [Google Scholar] [CrossRef]
- Warkentin, M.; Johnston, A.C.; Shropshire, J. The influence of the informal social learning environment on information privacy policy compliance efficacy and intention. Eur. J. Inf. Syst. 2011, 20, 267–284. [Google Scholar] [CrossRef]
- Crestani, C.C. Emotional stress and cardiovascular complications in animal models: A review of the influence of stress type. Front. Physiol. 2016, 7, 251. [Google Scholar] [CrossRef] [Green Version]
- Kivimäki, M.; Virtanen, M.; Elovainio, M.; Kouvonen, A.; Väänänen, A.; Vahtera, J. Work stress in the etiology of coronary heart disease—A meta-analysis. Scand. J. Work. Environ. Heal. 2006, 32, 431–442. [Google Scholar] [CrossRef]
- Barouki, R.; Gluckman, P.D.; Grandjean, P.; Hanson, M.; Heindel, J.J. Developmental origins of non-communicable disease: Implications for research and public health. Environ. Heal. A Glob. Access Sci. Source 2012, 11, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Grippo, A.J.; Moffitt, J.A.; Johnson, A.K. Cardiovascular alterations and autonomic imbalance in an experimental model of depression. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002, 282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sgoifo, A.; Carnevali, L.; Grippo, A.J. The socially stressed heart. Insights from studies in rodents. Neurosci. Biobehav. Rev. 2014, 39, 51–60. [Google Scholar] [CrossRef] [PubMed]
- MedicalEconomics. Coronavirus: Study finds Psychological Burden in Frontline Medical Workers. 2020. Available online: https://www.medicaleconomics.com/news/coronavirus-study-finds-psychological-burden-frontline-medical-workers (accessed on 22 April 2020).
- Time. Medical Workers Face Coronavirus Mental Health Crisis. 2020. Available online: https://time.com/5817435/covid-19-mental-health-coronavirus/?fbclid=IwAR0OqzF2fIMliU2NbNgl4XuJYhoIfA6inLjFwEdG2HfOaLKBc4sJucwvwNg (accessed on 25 April 2020).
- JapanTimes. From fine to Flailing: Rapid Health Declines in COVID-19 Patients jar Doctors and Nurses. The Japan Times. 2020. Available online: https://www.japantimes.co.jp/news/2020/04/09/world/science-health-world/rapid-health-declines-covid-19/#.XqKV-Wj7Qb4 (accessed on 24 April 2020).
- CDC. Criteria to Guide Evaluation and Laboratory Testing for COVID-19. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html (accessed on 22 April 2020).
- Kelly, M.; Tink, W.; Nixon, L. Keeping the human touch in medical practice. Lippincott Williams and Wilkins. Acad. Med. 2014, 89, 1314. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus preparedness and response supplemental appropriations act. In Public Law 116–123—Mar. 6, 2020; Congressional Record: Washington, DC, USA, 2020. Available online: https://www.congress.gov/116/plaws/publ123/PLAW-116publ123.pdf (accessed on 29 June 2020).

| Preexisting Conditions | Confirmed Death Rates | All Cases (Suspected and Asymptomatic) of COVID-19 |
|---|---|---|
| Cardiovascular disease | 13.2% | 10.5% |
| Diabetes | 9.2% | 7.3% |
| Chronic respiratory disease | 8.0% | 6.3% |
| Hypertension | 8.4% | 6.0% |
| Cancer | 7.6% | 5.6% |
| No preexisting conditions | 0.9% |
| No. | Symptoms | Healthy | Suspicious | Affected | Emergent |
|---|---|---|---|---|---|
| Green | Yellow | Orange (Consultation) | Red (Emergency) | ||
| 1 | Fever | <37.5 °C | ≥37.5 °C, Continue ≤3 days * | ≥37.5 °C, Continue ≥4 days ** | |
| 2 | muscle or joint pain | No | Continue ≤3 days * | Continue ≥4 days ** | |
| 3 | Sore throat | No | Continue ≤3 days * | Continue ≥4 days ** | |
| 4 | Dyspnea | No | Light to Moderate, Continue ≤3 days * | Light to Moderate, Continue ≥4 days ** | |
| or Severe | |||||
| 5 | Shortness of Breath | ≤15/min | ≤20/min | ≤25/min | ≥26/min |
| 6 | Cough | No | Continue ≤3 days * | Continue ≥4 days ** | |
| 7 | Chillness | No | Continue ≤3 days * | Continue ≥4 days ** | |
| 8 | SpO2 (%) | ≥96% | ≤95%, With no Symptom | ≤95%, With Light to Moderate Dyspnea | ≤95%, With severe Dyspnea |
| 9 | Fatigue | No | Light to Moderate, Continue ≤3 days * | Light to Moderate, Continue ≥4 days ** | |
| or Severe | |||||
| 10 | Loss of appetite | No | Continue ≤3 days * | Continue ≥4 days ** | |
| 11 | Diarrhea | No | Continue ≤3 days* | Continue ≥4 days ** | |
| 12 | Loss of taste | No | Yes | ||
| 13 | Loss of smell sense | No | Yes |
| Activity | General Mode | Emergency Mode |
|---|---|---|
| Symptom Collection | Health Worker | Mobile Phone or App |
| Clinical Measurements | Health Worker | Patients Self-Test or Health Worker |
| Medical Consultancy | Remote Doctor | Remote Doctor |
| ePrescription | GramHealth Application, printed by eHealth worker | GramHealth Application or Medical Facilities |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sampa, M.B.; Hoque, M.R.; Islam, R.; Nishikitani, M.; Nakashima, N.; Yokota, F.; Kikuchi, K.; Rahman, M.M.; Shah, F.; Ahmed, A. Redesigning Portable Health Clinic Platform as a Remote Healthcare System to Tackle COVID-19 Pandemic Situation in Unreached Communities. Int. J. Environ. Res. Public Health 2020, 17, 4709. https://doi.org/10.3390/ijerph17134709
Sampa MB, Hoque MR, Islam R, Nishikitani M, Nakashima N, Yokota F, Kikuchi K, Rahman MM, Shah F, Ahmed A. Redesigning Portable Health Clinic Platform as a Remote Healthcare System to Tackle COVID-19 Pandemic Situation in Unreached Communities. International Journal of Environmental Research and Public Health. 2020; 17(13):4709. https://doi.org/10.3390/ijerph17134709
Chicago/Turabian StyleSampa, Masuda Begum, Md. Rakibul Hoque, Rafiqul Islam, Mariko Nishikitani, Naoki Nakashima, Fumihiko Yokota, Kimiyo Kikuchi, Md Moshiur Rahman, Faiz Shah, and Ashir Ahmed. 2020. "Redesigning Portable Health Clinic Platform as a Remote Healthcare System to Tackle COVID-19 Pandemic Situation in Unreached Communities" International Journal of Environmental Research and Public Health 17, no. 13: 4709. https://doi.org/10.3390/ijerph17134709
APA StyleSampa, M. B., Hoque, M. R., Islam, R., Nishikitani, M., Nakashima, N., Yokota, F., Kikuchi, K., Rahman, M. M., Shah, F., & Ahmed, A. (2020). Redesigning Portable Health Clinic Platform as a Remote Healthcare System to Tackle COVID-19 Pandemic Situation in Unreached Communities. International Journal of Environmental Research and Public Health, 17(13), 4709. https://doi.org/10.3390/ijerph17134709







