Characterizing the Heart Rate Response to the 4 × 4 Interval Exercise Protocol
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Baseline Session
2.4. 4 × 4 Protocol
2.5. Assessment of Blood Lactate Concentration (BLa)
2.6. Statistical Analysis
3. Results
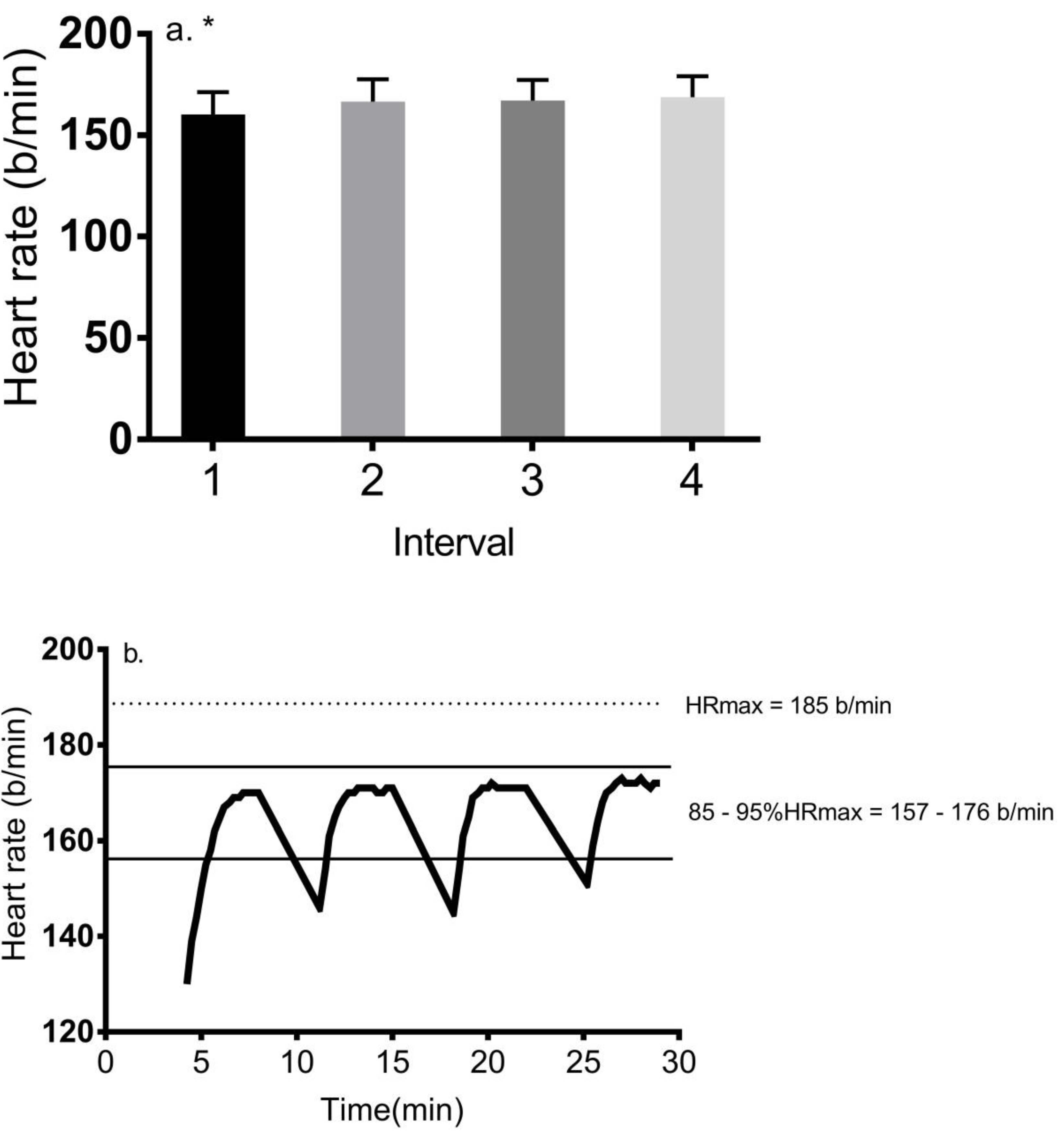
3.1. Change in HR during the 4 × 4 Protocol
3.2. Change in Power Output during the 4 × 4 Protocol
3.3. Change in Blood Lactate Concentration
3.4. Correlation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Weston, M.; Taylor, K.L.; Batterham, A.; Hopkins, W.G. Effects of low-volume high-intensity interval training (HIT) on fitness in adults: A meta-analysis of controlled and non-controlled trials. Sports Med. 2014, 44, 1005–1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milanović, Z.; Sporiš, G.; Weston, M. Effectiveness of high-intensity interval training (hit) and continuous endurance training for VO2 max improvements: A systematic review and meta-analysis of controlled trials. Sports Med. 2015, 45, 1469–1481. [Google Scholar] [CrossRef]
- Weston, K.S.; Wisløff, U.; Coombes, J.S. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: A systematic review and meta-analysis. Br. J. Sports Med. 2013, 48, 1227–1234. [Google Scholar] [CrossRef]
- Myers, J.; Prakash, M.; Froelicher, V.; Do, D.; Partington, S.; Atwood, J.E. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 2002, 346, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Nybo, L.; Sundstrup, E.; Jakobsen, M.D.; Mohr, M.; Hornstrup, T.; Simonsen, L.; Bülow, J.; Randers, M.B.; Nielsen, J.J.; Aagaard, P.; et al. High-intensity training versus traditional exercise interventions for promoting health. Med. Sci. Sports Exerc. 2010, 42, 1951–1958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, S.; Fedewa, M.V.; Hathaway, E.D.; Schmidt, M.D.; Evans, E.M. Sprint interval and moderate-intensity cycling training differentially affect adiposity and aerobic capacity in overweight young-adult women. Appl. Physiol. Nutr. Metab. 2016, 41, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Astorino, T.A.; Schubert, M.M.; Palumbo, E.; Stirling, D.; McMillan, D.; Cooper, C.; Godinez, J.; Martinez, D.; Gallant, R. Magnitude and time course of changes in maximal oxygen uptake in response to distinct regimens of chronic interval training in sedentary women. Eur. J. Appl. Physiol. 2013, 113, 2361–2369. [Google Scholar] [CrossRef]
- Hood, M.S.; Little, J.P.; Tarnopolsky, M.A.; Myslik, F.; Gibala, M.J. Low-volume interval training improves muscle oxidative capacity in sedentary adults. Med. Sci. Sports Exerc. 2011, 43, 1849–1856. [Google Scholar] [CrossRef] [PubMed]
- Astorino, T.A.; Edmunds, R.M.; Clark, A.; King, L.; Gallant, R.A.; Namm, S.; Fischer, A.; Wood, K.M. High-intensity interval training increases cardiac output and VO2 max. Med. Sci. Sports Exerc. 2017, 49, 265–273. [Google Scholar] [CrossRef]
- Little, J.P.; Safdar, A.; Wilkin, G.; Tarnopolsky, M.A.; Gibala, M.J. A practical model of low-volume high-intensity interval training induces mitochondrial biogenesis in human skeletal muscle: Potential mechanisms. J. Physiol. 2010, 588, 1011–1022. [Google Scholar] [CrossRef]
- Phillips, B.E.; Kelly, B.M.; Lilja, M.; Ponce-González, J.G.; Brogan, R.J.; Morris, D.L.; Gustafsson, T.; Kraus, W.E.; Atherton, P.J.; Vollaard, N.B.J.; et al. A practical and time-efficient high-intensity interval training program modifies cardio-metabolic risk factors in adults with risk factors for type II diabetes. Front. Endocrinol. 2017, 8. [Google Scholar] [CrossRef] [Green Version]
- Raleigh, J.P.; Giles, M.D.; Scribbans, T.D.; Edgett, B.A.; Sawula, L.J.; Bonafiglia, J.T.; Graham, R.B.; Gurd, B.J. The impact of work-matched interval training on VO2 peak and VO2 kinetics: Diminishing returns with increasing intensity. Appl. Physiol. Nutr. Metab. 2016, 41, 706–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helgerud, J.; Høydal, K.; Wang, E.; Karlsen, T.; Berg, P.; Bjerkaas, M.; Simonsen, T.; Helgesen, C.; Hjorth, N.; Bach, R.; et al. Aerobic high-intensity intervals improve vo2max more than moderate training. Med. Sci. Sports Exerc. 2007, 39, 665–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bækkerud, F.H.; Solberg, F.; Leinan, I.M.; Wisløff, U.; Karlsen, T.; Rognmo, Ø. Comparison of three popular exercise modalities on vo2max in overweight and obese. Med. Sci. Sports Exerc. 2016, 48, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Rognmo, Ø.; Hetland, E.; Helgerud, J.; Hoff, J.; Slørdahl, S.A. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur. J. Cardiovasc. Prev. Rehabil. 2004, 11, 216–222. [Google Scholar] [CrossRef]
- Tucker, W.J.; Sawyer, B.; Jarrett, C.L.; Bhammar, D.M.; Gaesser, G.A. Physiological responses to high-intensity interval exercise differing in interval duration. J. Strength Cond. Res. 2015, 29, 3326–3335. [Google Scholar] [CrossRef]
- Buchheit, M.; Laursen, P.B. High-intensity interval training, solutions to the programming puzzle: Part I: Cardiopulmonary emphasis. Sports Med. 2013, 43, 313–338. [Google Scholar] [CrossRef]
- Astorino, T.A. Alterations in VO2 max and the VO2 plateau with manipulation of sampling interval. Clin. Physiol. Funct. Imaging 2009, 29, 60–67. [Google Scholar] [CrossRef]
- Caiozzo, V.J.; Davis, J.A.; Ellis, J.F.; Azus, J.L.; Vandagriff, R.; Prietto, C.A.; McMaster, W.C. A comparison of gas exchange indices used to detect the anaerobic threshold. J. Appl. Physiol. 1982, 53, 1184–1189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falz, R.; Fikenzer, S.; Holzer, R.; Laufs, U.; Fikenzer, K.; Busse, M. Acute cardiopulmonary responses to strength training, high-intensity interval training, and moderate-intensity continuous training. Eur. J. Appl Physiol. 2019, 119, 1513–1523. [Google Scholar] [CrossRef] [PubMed]
- McCrimmon, D.R.; Cunningham, D.A.; Rechnitzer, P.A.; Griffiths, J. Effect of training on plasma catecholamines in post myocardial infarction patients. Med. Sci. Sports Exerc. 1976, 8, 152–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coyle, E.F.; Gonzalez-Alonso, J. Cardiovascular drift during prolonged exercise: New perspectives. Exerc. Sport Sci. Rev. 2001, 29, 88–92. [Google Scholar] [PubMed]
- Brooks, G.A. The lactate shuttle during exercise and recovery. Med. Sci. Sports Exerc. 1986, 18, 360–368. [Google Scholar] [CrossRef] [Green Version]
- Capostagno, B.; Bosch, A. Higher fat oxidation during running versus cycling at the same exercise intensities. Int. J. Sports Nutr. Exerc. Metab. 2010, 20, 44–55. [Google Scholar] [CrossRef] [PubMed]
- King, L.; Sillers, W.; McCarthy, K.; Louis, P.; Astorino, T.A. Higher fat oxidation during treadmill walking versus cycle ergometry in active women at equal RPE: A pilot study. J. Sports Med. Phys. Fit. 2015, 56, 1298–1303. [Google Scholar]
- Davies, C.T.M.; Few, J.; Foster, K.G.; Sargeant, A.J. Plasma catecholamine concentration during dynamic exercise involving different muscle groups. Eur. J. Appl. Physiol. Occup. Physiol. 1974, 32, 195–206. [Google Scholar] [CrossRef]

| Variable | Total |
|---|---|
| Number (M/F) | 20/19 |
| Age (year) | 26.0 ± 6.1 |
| Mass (kg) | 72.1 ± 10.8 |
| BMI (kg/m2) | 24.2 ± 2.9 |
| VO2 max (mL/kg/min) | 37.0 ± 5.4 |
| VO2 max (L/min) | 2.7 ±0.6 |
| VCO2 max (L/min) | 3.3 ± 0.6 |
| RER max | 1.30 ± 0.09 |
| VE max (L/min) | 112.5 ± 24.5 |
| HR max (b/min) | 184.9 ± 8.6 |
| PPO (W) | 260.1 ± 41.5 |
| Physical activity (h/week) | 5.4 ± 2.4 |
| Interval Number | Time Spent between 85 and 95% HR Max (min) | 95% CI |
|---|---|---|
| 1 | 2.7 ± 0.6 * | 2.5–2.8 |
| 2 | 3.4 ± 0.4 | 3.2–3.6 |
| 3 | 3.4 ± 0.5 | 3.2–3.6 |
| 4 | 3.5 ± 0.3 | 3.2–3.6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Acala, J.J.; Roche-Willis, D.; Astorino, T.A. Characterizing the Heart Rate Response to the 4 × 4 Interval Exercise Protocol. Int. J. Environ. Res. Public Health 2020, 17, 5103. https://doi.org/10.3390/ijerph17145103
Acala JJ, Roche-Willis D, Astorino TA. Characterizing the Heart Rate Response to the 4 × 4 Interval Exercise Protocol. International Journal of Environmental Research and Public Health. 2020; 17(14):5103. https://doi.org/10.3390/ijerph17145103
Chicago/Turabian StyleAcala, Justin J., Devyn Roche-Willis, and Todd A. Astorino. 2020. "Characterizing the Heart Rate Response to the 4 × 4 Interval Exercise Protocol" International Journal of Environmental Research and Public Health 17, no. 14: 5103. https://doi.org/10.3390/ijerph17145103
APA StyleAcala, J. J., Roche-Willis, D., & Astorino, T. A. (2020). Characterizing the Heart Rate Response to the 4 × 4 Interval Exercise Protocol. International Journal of Environmental Research and Public Health, 17(14), 5103. https://doi.org/10.3390/ijerph17145103





