Investigation of the Environmental and Socio-Economic Characteristics of Counties with a High Asthma Burden to Focus Asthma Action in Utah
Abstract
:1. Introduction
1.1. Conceptual Model
1.1.1. Environmental Factors
1.1.2. Behavioral Health Factors
1.1.3. Socio-Economic Factors
2. Materials and Methods
2.1. Study Design
2.2. Study Location
2.3. Data Collection and Description
| Variable | Description | Years | Source |
|---|---|---|---|
| Health outcome variables | |||
| Adult asthma prevalence * (%) (AAP) | Current doctor-diagnosed adult asthma | 2012–2015 | BRFSS, UT Department of Health [65] |
| Asthma emergency room visits * (AER) | Rate of emergency department visits for asthma per 10,000 population | 2012 ** | Centers for Disease Control and Prevention [67] |
| Environmental variables | |||
| Estimated mine area | Ranks of mining area by county based on UT Mining Districts Map Image, from UGS publication OFR-695 | 2018 | UT geological survey Krahulec [74] |
| Median/Minimum aridity index (AI) | County-level AI derived from median pixel from high-resolution global AI map | 1950–2000 | Global Aridity and PET Database [73] |
| Median elevation (m) | Median elevation by county calculated from 30 m SRTM data | 2000 | USGS [72] |
| Particulate matter (PM2.5) (µg m3 −1) | County-level: Average daily density of fine particulate matter (PM2.5) Census tract: modelled Daily PM2.5 levels | 2011 ** 2011–2014 | County Health Rankings [25] https://healthdata.gov/dataset/daily-census-tract-level-pm25-concentrations-2011-2014. |
| Red air days per year | red air = daily average PM2.5 >35 µg m3 −1 (NAAQS standard) | 2011 | Health Indicators Warehouse (HIW) [66] |
| Total mines | All types of active mine | 2009 | Bon and Krahulec (2009) [16] |
| Wind erosion risk | Ranking of area of county with high erosion risk based on Figure 1e | 2019 | Dunway et al. (2019) [47] |
| Wind speed | Average wind speed (mph) | 2010–2014 | http://www.usa.com/rank/UT-state--average-wind-speed--city-rank.htm |
| Health behavior factors | |||
| Obesity (%) Smoking *(%) | Based on BRFSS height and weight questions (BMI) Current smoking — BRFSS | 2009 2011 | Health Indicators Warehouse (HIW) [66] County Health Rankings [25] |
| Socio-Economic factors | |||
| Health Improvement Index (HII) | Composite socio-economic index based on 9 indicators for USAD | 2018 | https://ruralhealth.health.UT.gov/portal/health-improvement-index/, UT Department of Health [55] |
| Median Household Income ($) (MHHI) | Median household income in dollars | 2010 | Health Indicators Warehouse (HIW) [66] |
| Native American Population | Percentage Native American population | 2000 | US Census data, HIW [66] |
| Population density | Number of people per square mile, <7 considered highly rural [49] | 2010/2011 | US Census data, HIW [66], County Health Rankings [25] |
| Poverty (%) | Estimated by Census Bureau based on data for the SAIPE program | 2007/2011 | Health Indicators Warehouse (HIW) [66] |
| Uninsured (%) | Percentage of the population under age 65 with no health insurance coverage | 2011 | County Health Rankings [25] |
| Unemployment 16+ (%) | LAUS data come from the CPS, the official measure of the labor force for the nation | 2008 | Health Indicators Warehouse (HIW) [66] |
2.4. Statistical Analysis
3. Results
3.1. Descriptive Statistics and Spatial Patterns of Variables
3.2. Adult Asthma Prevalence: Comparison Tests, Correlation, Regression and Spatial Analysis
3.3. Spatial Analysis to Investigate the Reasons for Some Unexpected Correlations with AAP at the County Level
3.4. Asthma ER Visits: Comparison Tests, Correlation and Regression Analysis
3.5. Spatial Analysis of AER Data
3.6. Summary of Results for AAP and AER
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- UT Department of Health UDOH. Asthma in UT Burden Report 2012. 2012. Available online: http://health.UT.gov/asthma/data/reports/burdenreport/burdenreport2012.pdf (accessed on 13 September 2016).
- Centers for Disease Control and Prevention CDC. Most Recent Asthma Data. National Health Interview Survey NHIS. Available online: https://www.cdc.gov/asthma/most_recent_data.htm (accessed on 11 January 2017).
- National Ambulatory Medical Care Survey NAMCS. National Ambulatory Medical Care Survey 2012. Available online: www.cdc.gov/nchs/data/ahcd/namcs_web_tables.pdf (accessed on 3 November 2016).
- Hasegawa, K.; Bittner, J.; Nonas, S.; Stoll, S.; Watase, T.; Gabriel, S.; Herrera, V.; Camargo, C. Children and adults with frequent hospitalizations for asthma exacerbation 2012–2013: A multicenter observational study. Am. Acad. Allergy Asthma Immunol. 2015, 5, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Asthma and Allergy Foundation of America. Cost of Asthma on Society. Available online: http://www.aafa.org/page/cost-of-asthma-on-society.aspx (accessed on 17 July 2016).
- Halldin, C.; Doney, B.; Hnizdo, E. Changes in prevalence of chronic obstructive pulmonary disease and asthma in the US population and associated risk factors. Chron. Resp. Dis. 2015, 12, 47–60. [Google Scholar] [CrossRef] [Green Version]
- American Lung Association ALA Trends in Asthma Morbidity and Mortality. 2012. Available online: www.lung.org/finding-cures/our-research/trend-reports/asthma-trend-report.pdf (accessed on 13 December 2014).
- UT Department of Health UDOH Asthma Fast Stats. 2016. Available online: http://health.UT.gov/asthma/fast/stats (accessed on 16 September 2016).
- Toskala, E.; Kennedy, D. Asthma risk factors. Int. Forum Allergy Rhinol. 2015, 1. [Google Scholar] [CrossRef]
- World Health Organization WHO. Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease. 2016. Available online: https://apps.who.int/iris/bitstream/handle/10665/250141/9789241511353-eng.pdf (accessed on 11 October 2016).
- United Nations UN Sustainable Development Goals. 2015. Available online: https://sustainabledevelopment.un.org/?menu=1300 (accessed on 27 January 2017).
- Burnett, R.; Chen, H.; Szyszkowicz, M.; Fann, N.; Hubbell, B.; Pope, C.A., III; Apte, J.S.; Brauer, M.; Cohen, A.; Weichenthal, S.; et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. USA 2018, 115, 9592–9597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Environmental Protection Agency EPA Criteria Air Pollutants. 2016. Available online: https://www.epa.gov/criteria-air-pollutants (accessed on 13 September 2016).
- Cox, L.; Popken, D. Has reducing fine particulate matter and ozone caused reduced mortality rates in the United States? Ann. Epidemiol. 2015, 25, 162–173. [Google Scholar] [CrossRef] [PubMed]
- University of Southern California USC. ‘Southern California’s reduction in smog linked to major improvement in children’s health: Bronchitic symptoms on the decline as pollution levels drop in Los Angeles region over the past two decades. Sci. News 2016. Available online: https://www.sciencedaily.com/releases/2016/04/160412160352.htm#.Vw56s6jxLMI.email (accessed on 16 April 2016).
- Bon, R.L.; Krahulec, K.A. Summary of Mineral Activity in UT. In Circular 111 UT Geological Survey; A Division of UT Department of Natural Resources: Salt Lake City, UT, USA, 2009. [Google Scholar]
- National Weather Service Forecasting Office. What are Temperature Inversions? 2016. Available online: http://www.wrh.noaa.gov/slc/climate/TemperatureInversions.php (accessed on 21 April 2016).
- American Lung Association. State of the Air Report 2016: Most Polluted Cities. 2016. Available online: www.lung.org/our-initiatives/healthy-air/sota/city-rankings/most-polluted-cities.html (accessed on 30 April 2016).
- American Lung Association. State of the Air 20th Anniversary Report 2019. 2019. Available online: https://www.lung.org/assets/documents/healthy-air/state-of-the-air/sota-2019-full.pdf (accessed on 15 August 2019).
- Whiteman, D.; Hoch, S.; Horel, J.; Charland, A. Relationship between particulate air pollution and meteorological variables in UT’s Salt Lake Valley. Atmo. Environ. 2014, 94, 742–753. [Google Scholar] [CrossRef]
- Malek, E.; Davis, T.; Martin, R.; Silva, P. Meteorological and environmental aspects of one of the worst national air pollution episodes (January 2004) in Logan, Cache Valley, UT, USA. Atmos. Res. 2006, 79, 108–122. [Google Scholar] [CrossRef]
- Johnson, R.; Graham, G. Fine particulate matter National Ambient Air Quality Standards: Public health impact on populations in the Northeastern United States. Environ. Health Perspect. 2005, 113, 1140–1147. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1280392/ (accessed on 23 January 2017). [CrossRef] [Green Version]
- Esworthy, R. Air Quality: EPA’s 2013 Changes to the Particulate Matter (PM) Standard. Congressional Research Service Report. 23 December 2015. Available online: https://www.fas.org/sgp/crs/misc/R42934.pdf (accessed on 1 May 2016).
- Di, Q.; Dai, L.; Wang, Y.; Zanobetti, A.; Choirat, C.; Schwartz, J.D.; Dominici, F. Association of Short-term exposure to air pollution with mortality in older adults. JAMA 2017, 318, 2445–2456. [Google Scholar] [CrossRef]
- Robert Wood Johnson Foundation RWJF. County Health Rankings. 2016. Available online: http://www.countyhealthrankings.org (accessed on 5 June 2020).
- Alvarez, B.; Echeverria, S.; Alvarez, S.; Krupa, S. Air quality standards for particulate matter (PM) at high altitude cities. Environ. Pollut. 2013, 173, 255–256. Available online: www.ncbi.nlm.nih.gov/pubmed/23202983 (accessed on 30 April 2016). [CrossRef] [PubMed]
- Johnson, K. Quality of Air? That’s as Murky as Western Sky. New York Times, 11 December 2011. [Google Scholar]
- Goodman, M.M.; Carling, G.T.; Fernandez, D.P.; Rey, K.; Hale, C.; Bickmore, B.; Nelson, S.; Munroe, J. Trace element chemistry of atmospheric deposition along the Wasatch Front (UT, USA) reflects regional playa dust and local urban aerosols. Chem. Geol. 2019, 530, 119317. [Google Scholar] [CrossRef]
- Anto, J. Recent advances in the epidemiologic investigation of risk factors for asthma: A review of the 2011 literature. Curr. Allergy Asthma Rep. 2012, 12, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Mirabelli, M.; Vaidyanathan, A.; Flanders, W.; Qin, X.; Garbe, P. Outdoor PM2.5, Ambient Air Temperature, and Asthma Symptoms in the past 14 Days among Adults with Active Asthma. Environ. Health Perspect. 2016, 92. Available online: https://ehp.niehs.nih.gov/EHP92/ (accessed on 12 January 2017). [CrossRef] [PubMed] [Green Version]
- Akinbami, L.; Lynch, C.; Parker, J.; Woodruff, T. The association between childhood asthma prevalence and monitored air pollutants in metropolitan areas, United States 2001–2004. Environ. Res. 2010, 110, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Peel, J.; Tolbert, P.; Klein, M.; Metzger, K.; Flanders, W.; Todd, K.; Mulholland, J.; Ryan, P.; Frumkin, H. Ambient air pollution and respiratory emergency visits. Epidemiology 2005, 16, 164–174. [Google Scholar] [CrossRef]
- Gorai, A.; Tchounwou, P.; Tuluri, F. Association between ambient air pollution and asthma prevalence in different population groups residing in eastern Texas, USA. Int. J. Environ. Res. Public Health 2016, 13, 378. [Google Scholar] [CrossRef] [Green Version]
- Beard, J.; Beck, C.; Graham, R.; Packham, S.; Traphagan, M.; Giles, R.; Morgan, J. Winter temperature inversions and emergency department visits for asthma in Salt Lake County, UT, 2003—2008. Environ. Health Perspect. 2012, 120, 1385–1390. [Google Scholar] [CrossRef] [Green Version]
- Lauer, F.; Mitchell, L.; Bedrick, E.; McDonald, J.; Lee, W.; Li, W.; Olvera, H.; Amaya, M.; Berwick, M.; Gonzales, M.; et al. Temporal-spatial analysis of U.S.-Mexico border environmental fine and coarse PM air sample extract activity in human bronchial epithelial cells. Toxicol. Appl. Pharm. 2009, 238, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Wallace, J.; Nair, P.; Kanaroglou, P. Atmospheric remote sensing to detect effects of temperature inversions on sputum cell counts in airway diseases. Environ. Res. 2010, 110, 624–632. [Google Scholar] [CrossRef]
- Thalib, L.; Al-Taiar, A. Dust storms and the risk of asthma admissions to hospitals in Kuwait. Sci. Total Environ. 2012, 433, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Yamasaki, A.; Burioka, N.; Kurai, J.; Yoneda, K.; Yoshida, A.; Igishi, T.; Fukuoka, Y.; Nakamoto, M.; Takeuchi, H.; et al. Correlation between Asian Dust Storms worsening asthma in Western Japan. Allergol. Int. 2011, 60, 267–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strannegard, I.; Strannegard, O. Childhood bronchial asthma in a desert county. Allergy 1990, 45, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Akpinar-Elci, M.; Martin, F.; Behr, J.; Diaz, R. Saharan dust, climate variability, and asthma in Grenada, the Caribbean. Int. J. Biotechnol. 2015, 59, 1667–1671. [Google Scholar] [CrossRef]
- Kiechl-Kohlendorfer, U.; Horak, E.; Mueller, W.; Strobl, R.; Haberland, C.; Fink, F.; Schwaiger, M.; Gutenberger, K.; Reich, H.; Meraner, D.; et al. Living at high altitude and risk of hospitalisation for atopic asthma in children: Results from a large prospective birth-cohort study. Arch. Dis. Child. 2007, 92, 339–342. [Google Scholar] [CrossRef]
- Cogo, A.; Fiorenzano, G. Bronchial asthma: Advice for patients traveling to high altitude. High Alt. Med. Biol. 2009, 10, 117–121. [Google Scholar] [CrossRef]
- Vargas, M.H.; Becerril-Angeles, M.; Medina-Reyes, I.S.; Rascon-Pacheco, R.A. Altitude above 1500 m is a major determinant of asthma incidence: An ecological study. Respir. Med. 2018, 135, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayaaba, E.; Li, Y.; Yuan, J.L.; Ni, C.H. Occupational Respiratory Diseases of Miners from Two Gold Mines in Ghana. Int. J. Environ. Res. Public Health 2017, 14, 337. [Google Scholar] [CrossRef] [Green Version]
- Azad, S. Environmental Degradation due to Coal Mining in Baluchistan. Pol. J. Environ. Stud. 2015, 24, 1855–1861. [Google Scholar]
- Neophytou, A.M.; Costello, S.; Picciotto, S.; Noth, E.M.; Liu, S.; Lutzker, L.; Balmes, J.R.; Hammond, K.; Cullen, M.R.; Eisen, E.A. Accelerated lung function decline in an aluminium manufacturing industry cohort exposed to PM2.5: An application of the parametric g-formula. Occup. Environ. Med. 2019, 76, 888–894. [Google Scholar] [CrossRef]
- Dunway, M.C.; Pfennigwerth, A.A.; Fick, S.; Nauman, T.W.; Belnap, J.; Barger, N. Wind erosion and dust from US drylands: A review of causes, consequences, and solutions in a changing world. Ecosphere 2019, 10, 3. [Google Scholar] [CrossRef] [Green Version]
- Khokhawalla, S.; Rosenthal, S.; Pearlman, D.; Triche, E. Cigarette smoking and emergency care utilization among asthmatic adults in the 2011 Asthma Call-back Survey. J. Asthma Off. J. Assoc. Care Asthma 2015, 52, 732–739. [Google Scholar] [CrossRef]
- Cerveri, I.; Cazzoletti, L.; Corsico, A.; Marcon, A.; Niniano, R.; Grosso, A.; Ronzoni, V.; Accordini, S.; Janson, C.; Pin, I.; et al. The impact of cigarette smoking on asthma: A population-based international cohort study. Int. Arch. Allergy Immunol. 2012, 158, 175–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. Asthma and Obesity. 2010. Available online: https://www.cdc.gov/asthma/asthma_stats/asthma_obesity.htm (accessed on 30 December 2019).
- Akerman, M.J.; Calacanis, C.M.; Madsen, M.K. Relationship between asthma severity and obesity. J. Asthma 2004, 5, 521–526. [Google Scholar] [CrossRef]
- Jackson, E.; Doescher, M.; Hart, L. National Study of Lifetime Asthma Prevalence and Trends in Metro and Non-Metro Counties, 2000–2003; University of Washington Rural Health Research Center Study: Washington, DC, USA, 2007. [Google Scholar]
- UT Department of Environmental Quality UDEQ. UT Division of Air Quality 2014 Annual Report. 2014. Available online: http://www.airquality.UT.gov/docs/2015/02Feb/2014DAQAnnualReport_FINAL.pdf (accessed on 18 July 2020).
- Berkman, L.S. Social Epidemiology: Social Determinants of Health in the United States: Are We Losing Ground? Annu. Rev. Public Health 2009, 30, 27–41. [Google Scholar] [CrossRef] [Green Version]
- UT Department of Health. The UT Health Improvement Index. 2018. Available online: https://health.UT.gov/disparities/data/ohd/UTHII.pdf (accessed on 18 July 2020).
- Centers for Disease Control and Prevention. Adult Asthma Data: Prevalence Tables and Maps. 2012. Available online: https://www.cdc.gov/asthma/brfss/2012/tablel7.htm (accessed on 30 December 2019).
- Grineski, S.; Staniswalis, J.; Bulatgsinhala, P.; Peng, Y.; Gill, T. Hospital admissions for asthma and acute bronchitis in El Paso, Texas: Do age, sex, and insurance status modify the effects of dust and low wind events? Environ. Res. 2011, 111, 1148–1155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.; O’Neill, M.; Lee, J.; Cho, Y.; Kim, J.; Kim, H. Air pollution, socioeconomic position, and emergency hospital visits for asthma in Seoul, Korea. Int. Arch. Occup. Environ. Health 2007, 80, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Akinbami, L.J.; Moorman, J.E.; Bailey, C. Trends in Asthma Prevalence, Health Care Use, Mortality in the United States 2001–2010; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD, USA, 2012; p. 94.
- Forno, E.; Celedon, J.C. Asthma and ethnic minorities: Socioeconomic status and beyond. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 154–160. [Google Scholar] [CrossRef]
- Gorman, B.K.; Chu, M. Racial and ethnic differences in adult asthma prevalence, problems, and medical care. Ethn. Health 2009, 14, 527–552. [Google Scholar] [CrossRef] [PubMed]
- Coggon, D.; Rose, G.; Barker, D. Epidemiology for the Uninitiated, 3rd. ed.; BMJ Books: London, UK, 2003. [Google Scholar]
- Loney, T.; Nagelkerke, N. The individualistic fallacy, ecological studies and instrumental variables: A causal association. Emerg. Themes Epidemiol. 2014, 11, 18. [Google Scholar] [CrossRef] [Green Version]
- United States Census Bureau USCB. UT is nation’s fastest-growing state, Census Bureau reports. 2016. Available online: http://www.census.gov/newsroom/press-releases/2016/cb16-214.html (accessed on 2 February 2017).
- UT Department of Health UDOH. Health Indicator Report of Asthma: Adult Prevalence. 2016. Available online: https://ibis.health.UT.gov/indicator/view/AsthAdltPrev.SA.html (accessed on 15 December 2016).
- Health Indicators Warehouse HIW. 2016. Available online: http://www.healthindicators.gov (accessed on 18 July 2020).
- Centers for Disease Control and Prevention CDC. Emergency Department Visits for Asthma: Age-Adjusted Rate of Emergency Department Visits for Asthma per 10,000 Population. Natl. Environ. Public Health Track. Netw. Available online: Ephtracking.cdc.gov (accessed on 15 December 2016).
- Vaidyanathan, A.; Dimmick, W.D.; Kegler, S.R.; Qualters, J.R. Statistical Air Quality Predictions for Public Health Surveillance: Evaluation and Generation of County-level Metrics of PM2.5 for the Environmental Public Health Tracking Network. Int. J. Health Geogr. 2013, 12, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berrocal, V.; Gelfand, A.E.; Holland, D.M. Space-time fusion under error in computer model. Biometrics 2011, 68, 837–848. [Google Scholar] [CrossRef] [Green Version]
- Output: An application to modeling air quality. Biometrics 2011, 68, 837–848. [CrossRef]
- Berrocal, V.; Gelfand, A.E.; Holland, D.M. A bivariate space-time downscaler under space and time misalignment. Ann. Appl. Stat. 2010, 4, 1942–1975. [Google Scholar] [CrossRef] [PubMed]
- Berrocal, V.; Gelfand, A.E.; Holland, D.M. A spatio-temporal downscaler for output from numerical models. J. Agric. Biol. Environ. Stat. 2010, 15, 176–197. [Google Scholar] [CrossRef]
- United States Geological Survey USGS. 2005. Available online: http://egsc.usgs.gov/lsb/pubs/booklets/elvadlst.html (accessed on 18 July 2020).
- Global Aridity and PET Database. Available online: www.cgjar-csi.org/data/global-aridity-and-pet-database (accessed on 18 July 2020).
- Krahulec, K. UT Mining Districts; Open File Report ofr-695; UT Geological Survey: Salt Lake City, UT, USA, 2008.
- Jacquez, G.M.; Goovaerts, P.; Kaufmann, A.; Rommel, R. SpaceStat 4.0 User Manual: Software for the Space-Time Analysis of Dynamic Complex Systems, 04/2014, 4th ed.; BioMedware: Ann Arbor, MI, USA, 2014. [Google Scholar]
- Hengl, T.; Heuvelink, G.B.; Rossiter, D.G. About regression-kriging: From equations. Comput. Geosci. 2007, 33, 1301–1315. [Google Scholar] [CrossRef]
- Aneslin, L. Local Indicators of Spatial Association--LISA. Geog. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Goovaerts, P.; Jacquez, G.M. Detection of temporal changes in the spatial distribution of cancer rates using local Maran’s I and geostatistically simulated spatial neutral models. J. Geog. Syst. 2005, 7, 137–159. [Google Scholar] [CrossRef] [Green Version]
- Belnap, J.; Walker, B.; Munson, S.; Gill, R. Controls on sediment production in two U.S. deserts. Aeolian Res. 2014, 14, 15–24. [Google Scholar] [CrossRef]
- Wilhelm, M.; Ritz, B. Local Variations in CO and Particulate Air Pollution and Adverse Birth Outcomes in Los Angeles County, California, USA. Environ. Health. Perspect. 2005, 113, 1212–1221. [Google Scholar] [CrossRef] [Green Version]
- Merrill, R. Descriptive Findings Life Expectancy among LDS and Non-LDS in UT. Demogr. Res. 2004, 10, 61–62. [Google Scholar] [CrossRef]
- Schultze-Weminghause, G. Effects of high altitude on bronchial asthma. Pneumologie 2008, 62, 170–176. [Google Scholar]
- Simeonov, K.; Himmelstein, D. Lung cancer incidence decreases with elevation: Evidence for oxygen as an inhaled carcinogen. Peer J. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Social Determinants of Health, 2nd ed.; Wilkinson, R., Marmot, M., Eds.; Available online: https://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf?ua=1 (accessed on 19 July 2020).
- Novilla, L.; Barnes, M.; Hanson, C.; West, J.; Edwards, E. How Can We Get the Social Determinants of Health Message on the Public Policy and Public Health Agenda? 2011. Available online: www.who.int/sdhconference/resources/draft_background_paper2_usa.pdf (accessed on 19 July 2020).
- World Health Organization WHO. The WHO Health Systems Framework. Available online: https://www.who.int/healthsystems/strategy/everybodys_business.pdf (accessed on 17 May 2017).









| Mann-Whitney U Test | Kruskal-Wallis H Test | Pearson Correlation with AAP | p-Value (2 dp) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Rank | p-Value | Mean Rank | p-Value (2 dp) | ||||||
| Risk Factor Variables | Low AAP | High AAP | Low AAP | Medium AAP | High AAP | ||||
| Environmental variables | |||||||||
| Estimated Mine Area | 12.86 | 20.63 | 0.03 * | 7.50 | 14.53 | 20.63 | 0.02 * | 0.45 | 0.01 ** |
| Median Aridity Index | 17.43 | 8.63 | 0.01 ** | 20.80 | 16.38 | 8.63 | 0.03 * | −0.48 | 0.01 ** |
| Minimum Aridity Index | 16.90 | 10.00 | 0.05 * | 19.00 | 16.25 | 10.00 | 0.12 | −0.35 | 0.06 § |
| Median Elevation (m) | 14.86 | 15.38 | 0.88 | 21.80 | 12.69 | 15.38 | 0.11 | −0.30 | 0.12 |
| CL PM2.5 | 15.86 | 12.75 | 0.40 | 19.40 | 14.75 | 12.75 | 0.38 | −0.06 | 0.77 |
| Red Air Days | 17.02 | 9.69 | 0.03 * | 18.20 | 16.66 | 9.69 | 0.09 § | −0.24 | 0.22 |
| Total Mines | 12.95 | 20.38 | 0.02 * | 8.00 | 14.50 | 20.38 | 0.02 * | 0.33 | 0.08 § |
| Wind Erosion Risk | 12.83 | 20.69 | 0.02 * | 7.00 | 14.72 | 20.56 | 0.02 * | 0.45 | 0.01 ** |
| Health behavior variables | |||||||||
| Obesity (%) | 13.36 | 19.31 | 0.09 § | 13.90 | 13.19 | 19.31 | 0.24 | 0.49 | 0.01 ** |
| Smoking (%) | 13.48 | 19.00 | 0.11 | 9.10 | 14.84 | 19.00 | 0.12 | 0.42 | 0.02 * |
| Socio-economic variables | |||||||||
| Health Improvement Index | 13.76 | 18.25 | 0.21 | 3.8 | 16.88 | 18.25 | 0.005 ** | 0.49 | 0.01 ** |
| Median Household Income | 16.90 | 10.00 | 0.05 * | 20.60 | 15.75 | 10.00 | 0.08 § | −0.30 | 0.11 |
| Native American Pop. | 14.24 | 17.00 | 0.37 | 12.90 | 14.66 | 17.00 | 0.60 | 0.14 | 0.47 |
| Population Density | 17.02 | 9.69 | 0.04 * | 15.40 | 7.53 | 9.69 | 0.10 | −0.11 | 0.56 |
| Poverty (%) | 12.43 | 21.75 | 0.01 ** | 7.60 | 13.94 | 21.75 | 0.01 ** | 0.35 | 0.06 § |
| Unemployment (%) | 13.38 | 19.25 | 0.10 § | 14.80 | 12.94 | 19.25 | 0.23 | 0.14 | 0.47 |
| Uninsured (%) | 13.64 | 18.56 | 0.16 | 11.50 | 14.31 | 18.56 | 0.30 | 0.09 | 0.66 |
| Term | Parameter Estimates | Standard Error | p-Value |
|---|---|---|---|
| Intercept | 7.03237 | 2.30619 | 0.006 * |
| Median AI | −0.00042 | 0.00022 | 0.066 |
| Total Mines | 0.14935 | 0.09469 | 0.128 |
| Smoking | 0.32907 | 0.20596 | 0.123 |
| Native Am. Pop. | −0.00009 | 0.00004 | 0.028 * |
| Pearson Correlations with RK AAP | ||||||
|---|---|---|---|---|---|---|
| Variable | All Small Areas | p-Value (n = 588) | Metro Small Areas | p-Value (n = 519) | Non-Metro Small Areas | p-Value (n = 69) |
| CT PM2.5 Summer 2011 max | 0.273 | <0.01 ** | 0.396 | <0.01 ** | 0.211 | 0.08 § |
| CT PM2.5 Summer 2014 max | 0.022 | 0.59 | 0.378 | <0.01 ** | −0.161 | 0.19 |
| CT PM2.5 Winter 2011–2014 mean | 0.090 | 0.03 * | 0.428 | <0.01 ** | −0.06 | 0.62 |
| Mann-Whitney U Test | Kruskal-Wallis H Test | Pearson Correlation with AER Visits | p-Value (2 dp) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Rank | p-Value | Mean Rank | p-Value (2 dp) | ||||||
| Low AER | High AER | Low AER | Medium AER | High AER | |||||
| Environmental variables | |||||||||
| Estimated Mine Area | 14.35 | 15.53 | 0.71 | 14.58 | 12.38 | 21.36 | 0.06 § | 0.25 | 0.19 |
| Median Aridity Index | 17.62 | 12.88 | 0.14 | 16.00 | 17.38 | 8.71 | 0.08 § | −0.38 | 0.04* |
| Minimum Aridity Index | 17.27 | 13.16 | 0.20 | 14.00 | 18.69 | 7.43 | 0.01 ** | −0.38 | 0.04 * |
| Median Elevation (m) | 15.77 | 14.38 | 0.66 | 19.33 | 14.31 | 12.86 | 0.35 | −0.23 | 0.23 |
| CL PM2.5 | 16.46 | 13.81 | 0.40 | 15.75 | 17.56 | 8.51 | 0.06 § | −0.33 | 0.08 § |
| Red Air Days | 18.12 | 12.47 | 0.07 § | 14.25 | 18.28 | 8.14 | 0.02 * | −0.31 | 0.11 |
| Total Mines | 14.73 | 15.22 | 0.87 | 16.83 | 12.31 | 19.57 | 0.10 § | 0.25 | 0.19 |
| Wind Erosion Risk | 12.75 | 11.03 | 0.59 | 16.25 | 11.91 | 21.00 | 0.05 * | 0.51 | 0.01 ** |
| Health behavior variables | |||||||||
| Obesity (%) | 15.96 | 14.22 | 0.58 | 18.25 | 13.59 | 15.43 | 0.51 | 0.16 | 0.42 |
| Smoking (%) | 16.23 | 14.00 | 0.48 | 20.17 | 11.31 | 19.00 | 0.03 * | 0.02 | 0.93 |
| Socio-economic variables | |||||||||
| Health Improvement Index | 15.14 | 14.87 | 0.95 | 15.00 | 13.88 | 17.57 | 0.63 | 0.13 | 0.50 |
| Median Household Income | 16.38 | 13.88 | 0.43 | 13.17 | 18.06 | 9.57 | 0.08 § | −0.17 | 0.38 |
| Native American Pop. | 13.69 | 16.06 | 0.39 | 14.92 | 13.22 | 19.14 | 0.21 | 0.37 | 0.05 * |
| Population Density | 17.23 | 13.19 | 0.20 | 12.33 | 17.97 | 10.50 | 0.11 | −0.21 | 0.28 |
| Poverty (%) | 15.81 | 14.34 | 0.65 | 17.92 | 12.09 | 19.14 | 0.12 | 0.15 | 0.43 |
| Unemployment (%) | 14.54 | 15.38 | 0.79 | 18.50 | 12.69 | 17.29 | 0.26 | 0.15 | 0.45 |
| Uninsured (%) | 12.65 | 16.91 | 0.18 | 13.92 | 12.81 | 20.93 | 0.10 § | 0.37 | 0.05 * |
| Term | Parameter Estimates | Standard Error | p-Value |
|---|---|---|---|
| Intercept | 15.7536 | 6.0839 | 0.0155 * |
| Wind Erosion Risk | 1.0798 | 0.4307 | 0.0187 * |
| Uninsured | 0.4142 | 0.3088 | 0.1914 |
| AAP (County Level) | Expected Association | Mann Whitney U | Kruskal Wallis H | Pearson Correlation | Regression |
|---|---|---|---|---|---|
| Risk Factor Variables | Positive or Negative | Ranks Associated with High AAP (HL) | Ranks Associated with High AAP (and Low AAP) (HML) | Positive or Negative | Positive or Negative |
| Environmental variables | |||||
| Estimated Mine Area | pos. | H * | H(L) * | pos. ** | - |
| Median Aridity Index | neg. | L ** | L(H) * | neg.** | neg. § |
| Minimum Aridity Index | neg. | L * | L(H) | neg. § | - |
| Median Elevation (m) | neg. | H | M(H) | neg. | - |
| CL PM2.5 | pos. | L | L(H) | neg. | - |
| Red Air Days | pos. | L * | L(H) § | neg. | - |
| Total Mines | pos. | H * | H(L) * | pos. § | pos. § |
| Wind Erosion Risk | pos. | H * | H(L) * | pos. ** | - |
| Health behavior variables | |||||
| Obesity (%) | pos. | H § | H(M) | pos. ** | - |
| Smoking (%) | pos. | H | H(L). | pos. * | pos. § |
| Socio-economic variables | |||||
| Health Improvement Index | pos. | H | H(L) ** | pos. ** | - |
| Median Household Income | neg. | L * | L(H) § | neg. | - |
| Native American Pop. | pos. | H | H(L) | pos. | neg * |
| Population Density | pos. | L * | M(H) | neg. | - |
| Poverty (%) | pos. | H * | H(L) ** | pos. § | - |
| Unemployment (%) | pos. | H § | H(M) | pos. | - |
| Uninsured (%) | pos. | H | H(L). | pos. | - |
| Correlations for Metro vs. Non-Metro | |||||
| RK AAP (USAD) | Expected Association | All | Metro | Non-Metro | |
| CT PM2.5 Summer 2011 max. | pos. | pos. ** | pos. ** | pos. § | |
| CT PM2.5 Summer 2014 max. | pos. | pos. | pos. ** | neg. | |
| CT PM2.5 Winter 2011-2014 mean | pos. | pos. * | pos. ** | neg. | |
| Moving Correlations with RK AAP | |||||
| RK AAP (USAD) | Northern UT | Southern UT | |||
| Population Density | pos. | pos. | neg. | ||
| CT PM2.5 Summer 2011 max. | pos. | pos. | neg. | ||
| CT PM2.5 Winter 2011-2014 mean | pos. | pos. | neg. | ||
| AER (County Level) | Expected Association | Mann Whitney U | Kruskal Wallis H | Pearson Correlation | Regression | ||
|---|---|---|---|---|---|---|---|
| Risk Factor Variables | Positive or Negative | Ranks Associated with High AER (HL) | Ranks Associated with High AER (HML) | Positive or Negative | Positive or Negative | ||
| Environmental variables | |||||||
| Estimated Mine Area | pos. | H | H(M) § | pos. | - | ||
| Median Aridity Index | neg. | L | L(M) § | neg. * | - | ||
| Minimum Aridity Index | neg. | L | L(M) ** | neg. * | - | ||
| Median Elevation (m) | neg. | L | L(H) | neg. | - | ||
| CL PM2.5 | pos. | L | L(M) § | neg. § | - | ||
| Red Air Days | pos. | L § | L(M) * | neg. | - | ||
| Total Mines | pos. | H. | H(M) * | pos. | - | ||
| Wind Erosion Risk | pos. | L | H(M) * | pos. ** | pos. * | ||
| Health behavior variables | |||||||
| Obesity (%) | pos. | L | M(H) | pos. | - | ||
| Smoking (%) | pos. | L | M(H) * | pos. | - | ||
| Socio-economic variables | |||||||
| Health Improvement Index | pos. | L | H(M) | pos. | - | ||
| Median Household Income | neg. | L | L(M) § | neg. | - | ||
| Native American Pop. | pos. | H. | H(M) | pos. * | - | ||
| Population Density | pos. | L | L(M) | neg. | - | ||
| Poverty (%) | pos. | L | H(M) | pos. | - | ||
| Unemployment (%) | pos. | H. | M(H) | pos. | - | ||
| Uninsured (%) | pos. | H. | H(M) § | pos. * | pos. | ||
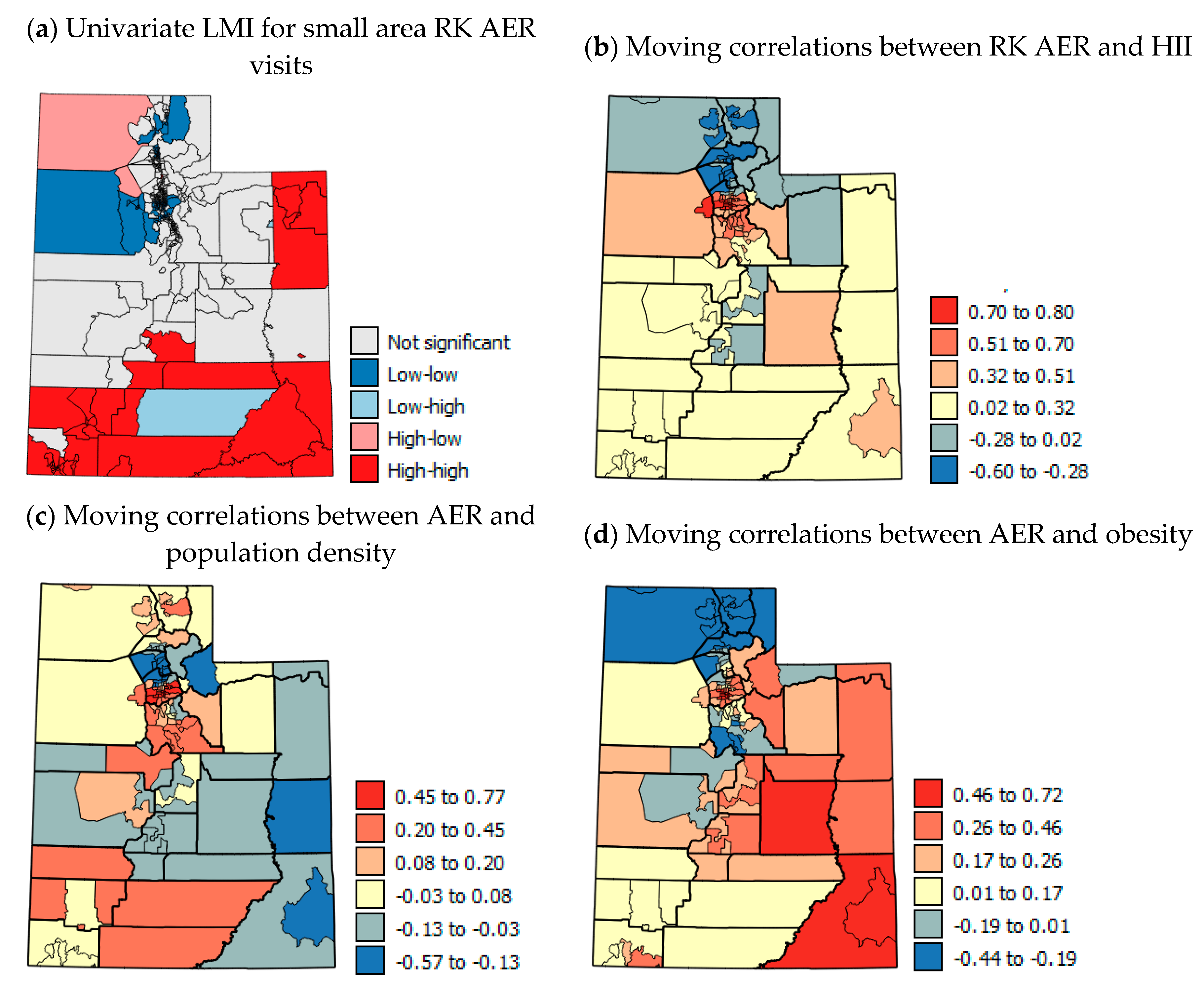
| Moving Correlations with RK AER | |||||||
| RK AER (USAD) | Expected Association | Northern UT | Southern UT | ||||
| HII | pos. | pos. | neg. | pos. | neg. | ||
| Population Density | pos. | pos. | neg. | pos. | neg. | ||
| Obesity | pos. | pos. | neg. | pos. | neg. | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vowles, M.; Kerry, R.; Ingram, B.; Mason, L. Investigation of the Environmental and Socio-Economic Characteristics of Counties with a High Asthma Burden to Focus Asthma Action in Utah. Int. J. Environ. Res. Public Health 2020, 17, 5251. https://doi.org/10.3390/ijerph17145251
Vowles M, Kerry R, Ingram B, Mason L. Investigation of the Environmental and Socio-Economic Characteristics of Counties with a High Asthma Burden to Focus Asthma Action in Utah. International Journal of Environmental Research and Public Health. 2020; 17(14):5251. https://doi.org/10.3390/ijerph17145251
Chicago/Turabian StyleVowles, Maureen, Ruth Kerry, Ben Ingram, and Linda Mason. 2020. "Investigation of the Environmental and Socio-Economic Characteristics of Counties with a High Asthma Burden to Focus Asthma Action in Utah" International Journal of Environmental Research and Public Health 17, no. 14: 5251. https://doi.org/10.3390/ijerph17145251
APA StyleVowles, M., Kerry, R., Ingram, B., & Mason, L. (2020). Investigation of the Environmental and Socio-Economic Characteristics of Counties with a High Asthma Burden to Focus Asthma Action in Utah. International Journal of Environmental Research and Public Health, 17(14), 5251. https://doi.org/10.3390/ijerph17145251






