Living in a Multi-Risk Chaotic Condition: Pandemic, Natural Hazards and Complex Emergencies
Abstract
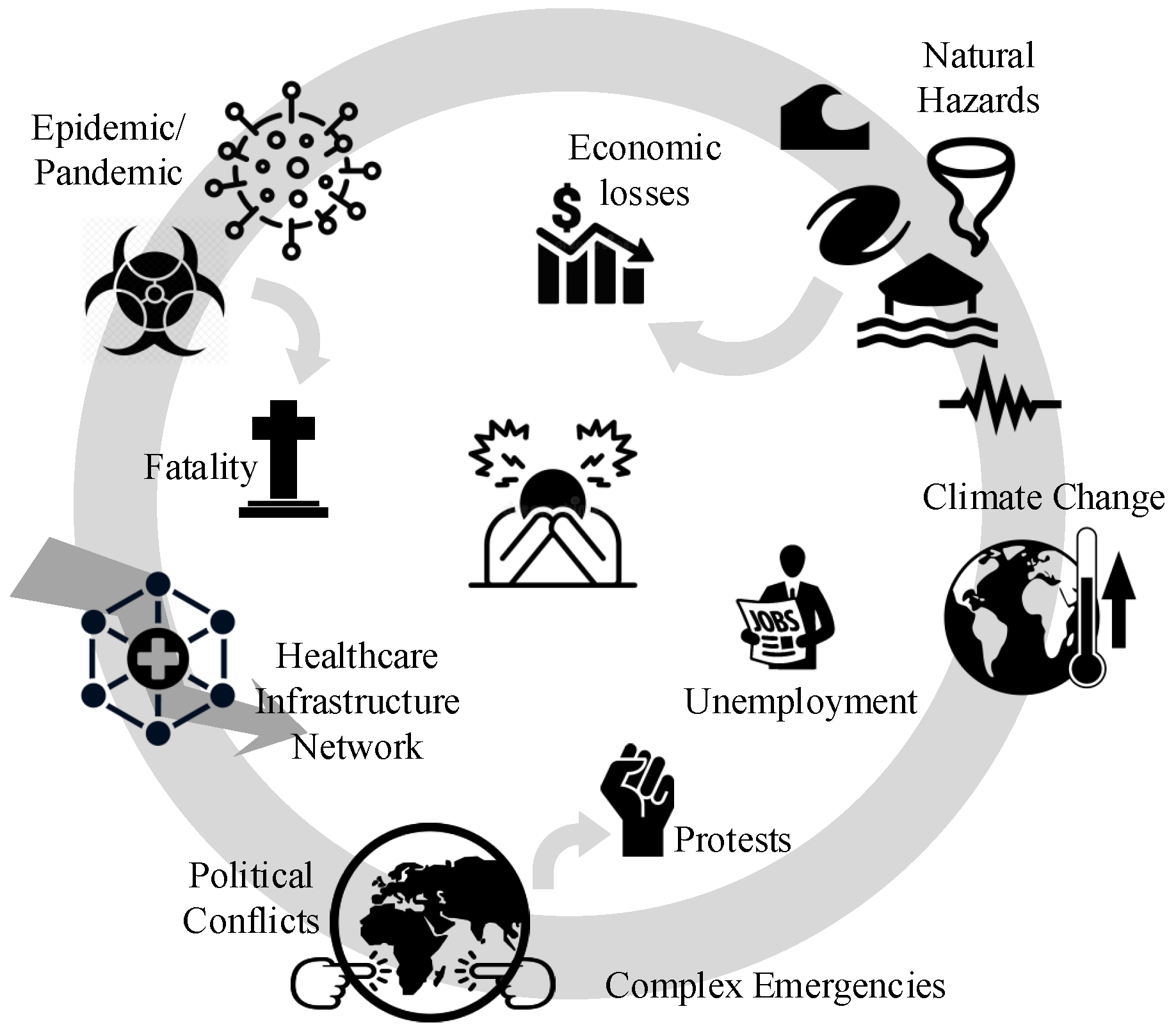
:1. Background
2. Single-Hazard Risk
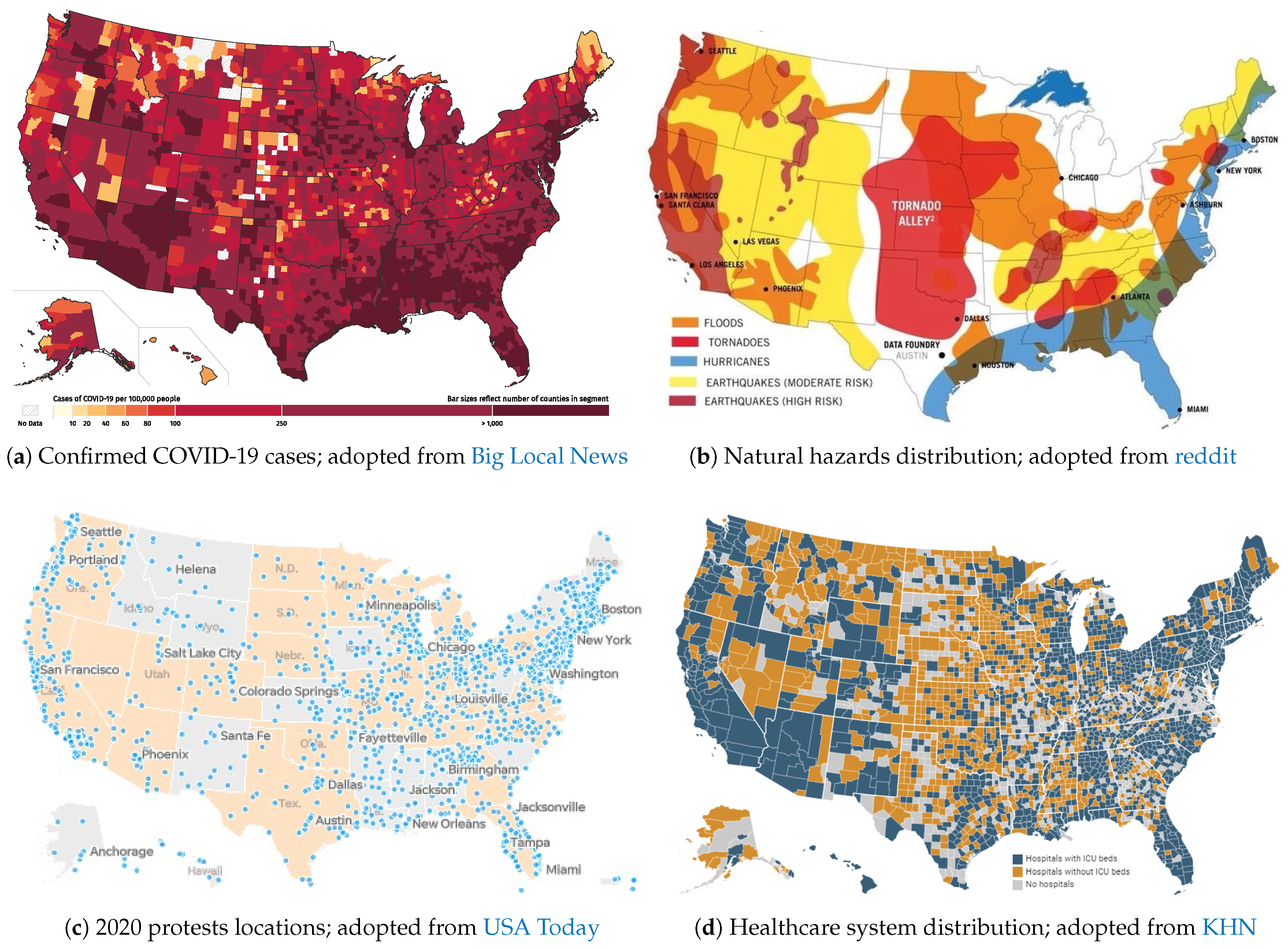
2.1. COVID-19 Pandemic
2.2. Natural Hazards
2.3. Complex Emergencies
2.4. Healthcare Availability
3. Multi-Hazard Risk
“to determine the probability of occurrence of different hazards either occurring at the same time or shortly following each other, because they are dependent from one another or because they are caused by the same triggering event or hazard, or merely threatening the same elements at risk without chronological coincidence.”
- Independent hazards threatening a given area: the main concern in this effort is harmonization of the hazard assessment, meaning that all should have a similar basis [31].
- Hazard interactions, triggering or cascade effects: in this effort, the occurrence of one event could affect the probability of occurrence in others (usually accelerates them). Once this concept is propagated into a chain of events, the Bayesian networks framework can be used [34]. For two events with occurrence of and , the probability of occurrence, , is:where the bar sign presents the non-occurrence condition. This equation can be generalized for N events.
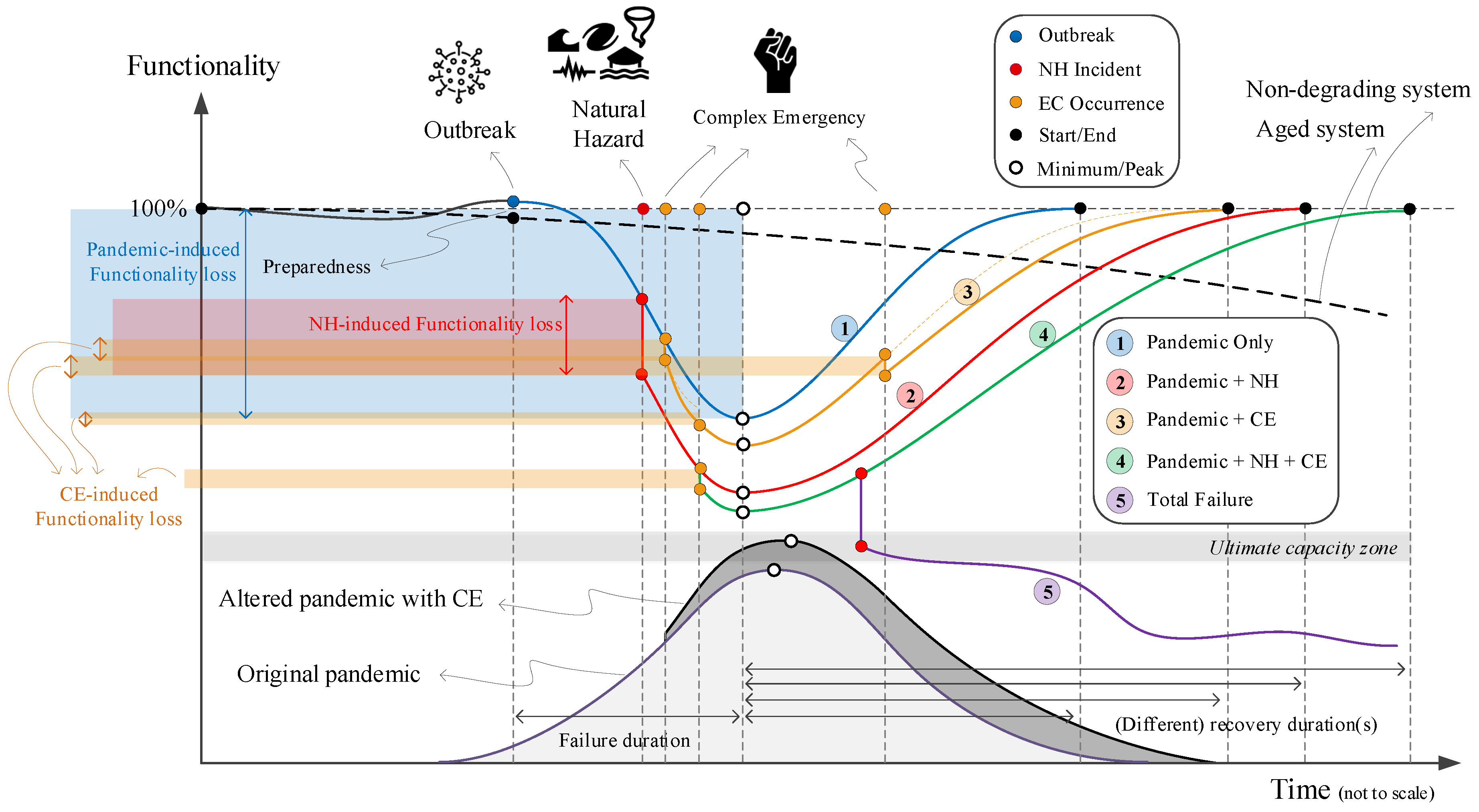
4. Multi-Hazard on Healthcare System
- Pandemic only: This is a single-hazard scenario and assumes no other concurrent hazard threatens the healthcare system. Based on this figure, the healthcare system is assumed to be initially in either full functionality (i.e., 100%), in a degraded mode (>100%), or in an upgraded mode (<100%). Degraded functionality could be caused by aging facilities or personnel and medical equipment shortages. Alternatively, upgraded functionality could be due to the preparedness of a system with prior knowledge about the possible occurrence and dimensions of such a pandemic [66].The performance, or functionality, of a system is reduced with increasing numbers of positive COVID-19 cases. The system has minimum functionality (more or less) when the pandemic is peaking. By reducing the number of infections and designating additional monetary and logistical recourses to the issue, the system recovers from this adverse effect. The transitioning from response to recovery, including consideration of assessment, management, and communication of risk and uncertainty over time was discussed by Menoni and Schwarze [67].
- Pandemic + Natural Hazard: This is a double-hazard situation that assumes a natural hazard (e.g., earthquake, flood) hits the community during a pandemic. Examples are provided in Section 2.2. The NH-induced functionality loss in this scenario is fairly rapid, compared to the slow reduction of functionality in the pandemic-only case. A natural disaster may impose extra pressure on the healthcare system by occupying a considerable amount of overall hospital capacity. It can also cause a large evacuation, which in turn increases the risk of viral infections among displaced people.Following the sudden functionality loss due to NH, the final compound loss of functionality in this scenario is more than in the pandemic-only one, assuming that the natural hazard can turn into a disaster. Recovery in this scenario is also longer because the natural disaster may cause some physical damage to the healthcare system, which would not occur in the pandemic-only scenario.
- Pandemic + CE: This is also a double-hazard situation in which multiple CEs (e.g., political conflict, protests) occur during a pandemic. Each of these events, depending on their severity, may or may not reduce the functionality of the healthcare system, including reductions in financial resources, global collaborations, and/or data sharing. Compared to the pandemic-only scenario, the recovery time is higher.On the other hand, the occurrence of such CEs may impact the original pandemic transmission curve by intensifying its peak and elongating its endurance time, see Figure 5 (transition from light gray to darker one).
- Pandemic + NH + CE: This is a very low-probability, high-consequence situation in which all three hazard sources occur in a relatively short timeframe, though not necessarily at the same time. Such a scenario might cause the largest functionality loss and longest recovery time. One may recognize some states within the U.S. exposed to such multi-risk by overlapping the three maps in Figure 2.
- The final scenario is an intense version of any of the previous four scenarios. The healthcare system in each county has a limited capacity (e.g., ICU rooms, ventilator machines), and may fail if the imposed demand becomes higher than the “ultimate capacity” of the system [68]. A potential solution is to flatten the transmission curve by imposing stronger stay-at-home orders.
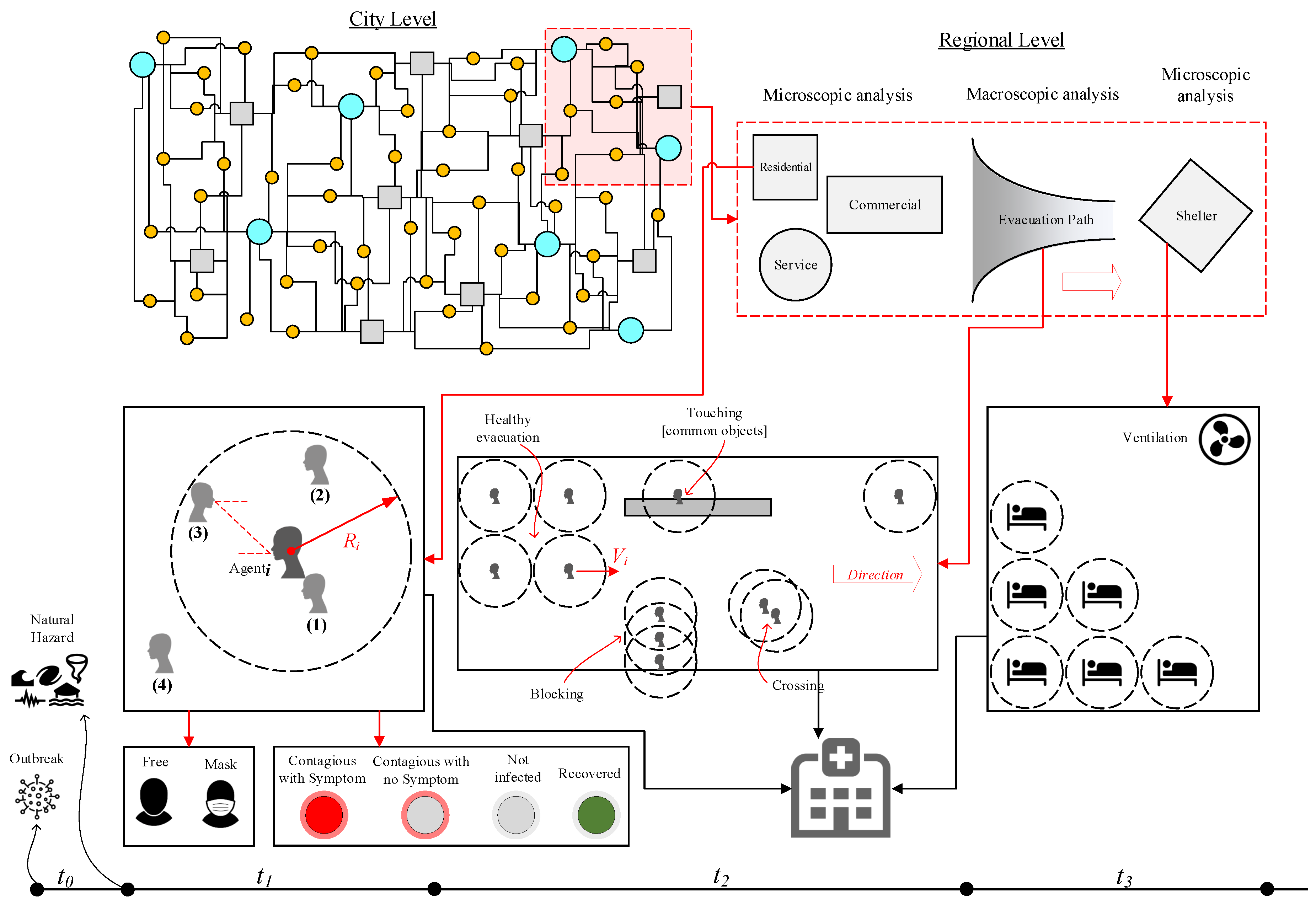
5. Multi-Hazard Evacuation Models
- Confined space crowd models investigate the occupants’ (or agents’) exposure inside a building during a pandemic and right before or after a natural hazard. In this model, various factors, such as the distance between individuals, the type of transmission contact (e.g., airborne, droplets), and time of exposure, should be considered. The uncertainty associated with the spread of disease can be addressed as one of four potential cases shown in Figure 6:
- Direct physical contact (e.g., touching).
- Within the social distance: the exposure might happen if the agent falls within the social distance (about 2.0 m) of agent.
- Being face-to-face within the social distance: the transmission of COVID-19 is higher when the individuals are facing each other or their faces are at a certain angle of each other. This is an important factor especially in commercial or service centers.
- Being in the same confined area.
One may add the following further details to each of four above-mentioned cases:- -
- All cases are time-dependent and should be analyzed in the transient mode.
- -
- All the interactions should be modeled between any two combination of agent and agent.
- -
- Various constraints should be applied to the simulations including but not limited to: using face covering, contagious with or without symptoms, etc.
- Evacuation models are divided into two parts: evacuating a building and heading towards a shelter. For the latter, factors such as duration, length of travel, difficulty of paths, speed of each individual, potential touching of common surfaces/objects, blocked paths by a group of individuals, and violations of social distancing should be considered.
- Lastly, sheltering is another major concern during a pandemic, and the capacity of shelters should be recalculated to account for safe distancing between individuals, as well as the length of time evacuees will remain there. Among other factors, the functionality of ventilation systems should be managed to avoid potential damage by a natural hazard.During all three models, a portion of evacuees might become injured, which should be accounted for in evacuation models and added to the resiliency of the healthcare system, Figure 5.
6. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Jonkman, S.; Van Gelder, P.; Vrijling, J. An overview of quantitative risk measures for loss of life and economic damage. J. Hazard. Mater. 2003, 99, 1–30. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease 2019 (COVID-19): Situation Report 80; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Wu, Y.C.; Chen, C.S.; Chan, Y.J. The outbreak of COVID-19: An overview. J. Chin. Med Assoc. 2020, 83, 217. [Google Scholar] [CrossRef] [PubMed]
- Hellewell, J.; Abbott, S.; Gimma, A.; Bosse, N.I.; Jarvis, C.I.; Russell, T.W.; Munday, J.D.; Kucharski, A.J.; Edmunds, W.J.; Sun, F.; et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. In The Lancet Global Health; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Johns Hopkins University of Medicine. Corovavirus Resource Center; Johns Hopkins University of Medicine: Baltimore, MD, USA, 2020. [Google Scholar]
- Wilson, N.; Kvalsvig, A.; Barnard, L.T.; Baker, M.G. Case-fatality risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg. Infect. Dis. 2020, 26, 1339–1441. [Google Scholar] [CrossRef] [PubMed]
- Boulos, M.N.K.; Geraghty, E.M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: How 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int. J. Health Geogr. 2020, 19, 8. [Google Scholar]
- Petropoulos, F.; Makridakis, S. Forecasting the novel coronavirus COVID-19. PLoS ONE 2020, 15, e0231236. [Google Scholar] [CrossRef]
- Fanelli, D.; Piazza, F. Analysis and forecast of COVID-19 spreading in China, Italy and France. Chaos Solitons Fractals 2020, 134, 109761. [Google Scholar] [CrossRef]
- Anastassopoulou, C.; Russo, L.; Tsakris, A.; Siettos, C. Data-based analysis, modelling and forecasting of the COVID-19 outbreak. PLoS ONE 2020, 15, e0230405. [Google Scholar] [CrossRef] [Green Version]
- Grasselli, G.; Pesenti, A.; Cecconi, M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA 2020, 323, 1545–1546. [Google Scholar] [CrossRef] [Green Version]
- Yamana, T.; Pei, S.; Shaman, J. Projection of COVID-19 Cases and Deaths in the US as Individual States Re-open May 4, 2020. medRxiv 2020. [Google Scholar] [CrossRef]
- Der-Kiureghian, A.; Ditlevsen, O. Aleatory or epistemic? Does it matter? Struct. Saf. 2009, 31, 105–112. [Google Scholar] [CrossRef]
- Nelson, S. Natural Hazards and Natural Disasters; Natural Disaster & Assessing Hazards and Risk, Tulane University: New Orleans, LA, USA, 2018; Last Viewed May 2020. [Google Scholar]
- Hariri-Ardebili, M. Risk, Reliability, Resilience (R3) and beyond in dam engineering: A state-of-the-art review. Int. J. Disaster Risk Reduct. 2018, 31, 806–831. [Google Scholar] [CrossRef]
- McCloskey, B.; Zumla, A.; Ippolito, G.; Blumberg, L.; Arbon, P.; Cicero, A.; Endericks, T.; Lim, P.L.; Borodina, M. Mass gathering events and reducing further global spread of COVID-19: A political and public health dilemma. Lancet 2020, 395, 1096–1099. [Google Scholar] [CrossRef]
- Memish, Z.A.; Steffen, R.; White, P.; Dar, O.; Azhar, E.I.; Sharma, A.; Zumla, A. Mass gatherings medicine: Public health issues arising from mass gathering religious and sporting events. Lancet 2019, 393, 2073–2084. [Google Scholar] [CrossRef]
- Barrios, J.M.; Hochberg, Y. Risk Perception Through the Lens of Politics in the Time of the Covid-19 Pandemic; Technical Report; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Painter, M.; Qiu, T. Political Beliefs Affect Compliance with COVID-19 Social Distancing Orders. SSRN 3569098. Available online: https://ssrn.com/abstract=3569098 (accessed on 6 July 2020).
- Grossman, G.; Kim, S.; Rexer, J.; Thirumurthy, H. Political Partisanship Influences Behavioral Responses to Governors’ Recommendations for COVID-19 Prevention in the United States. SSRN 3578695. Available online: https://ssrn.com/abstract=3578695 (accessed on 6 July 2020).
- Adolph, C.; Amano, K.; Bang-Jensen, B.; Fullman, N.; Wilkerson, J. Pandemic Politics: Timing State-Level Social Distancing Responses to COVID-19; American Political Science Association: Washington, DC, USA, 2020. [Google Scholar]
- Kavanagh, N.M.; Goel, R.R.; Venkataramani, A.S. Association of County-Level Socioeconomic and Political Characteristics with Engagement in Social Distancing for COVID-19. medRxiv 2020, 4, 2020. [Google Scholar]
- Dincer, O.C.; Gillanders, R. Shelter in Place? Depends on the Place: Corruption and Social Distancing in American States; SSRN: Rochester, NY, USA, 2020. [Google Scholar]
- Seddighi, H. Trust in Humanitarian Aid From the Earthquake in 2017 to COVID-19 in Iran: A Policy Analysis. In Disaster Medicine and Public Health Preparedness; Cambridge University Press: Cambridge, UK, 2020; pp. 1–4. [Google Scholar]
- Ferretti, L.; Wymant, C.; Kendall, M.; Zhao, L.; Nurtay, A.; Abeler-Dörner, L.; Parker, M.; Bonsall, D.; Fraser, C. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science 2020, 368, eabb6936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- VanEgeren, J. 72 COVID Positive After Attending Large Event; WMTV: Madison, WI, USA, 2020. [Google Scholar]
- Resnick, B. What Public Health Experts Want Critics to Know About Why They Support the Protests. 2020. Available online: https://www.vox.com/science-and-health/2020/6/6/21279592/protest-pandemic-covid-19-risk-second-wave-systemic-racism (accessed on 6 June 2020).
- Devakumar, D.; Shannon, G.; Bhopal, S.S.; Abubakar, I. Racism and discrimination in COVID-19 responses. Lancet 2020, 395, 1194. [Google Scholar] [CrossRef]
- Bedford, J.; Farrar, J.; Ihekweazu, C.; Kang, G.; Koopmans, M.; Nkengasong, J. A new twenty-first century science for effective epidemic response. Nature 2019, 575, 130–136. [Google Scholar] [CrossRef]
- Schmidt, J.; Matcham, I.; Reese, S.; King, A.; Bell, R.; Henderson, R.; Smart, G.; Cousins, J.; Smith, W.; Heron, D. Quantitative multi-risk analysis for natural hazards: A framework for multi-risk modelling. Nat. Hazards 2011, 58, 1169–1192. [Google Scholar] [CrossRef]
- Marzocchi, W.; Garcia-Aristizabal, A.; Gasparini, P.; Mastellone, M.L.; Di Ruocco, A. Basic principles of multi-risk assessment: A case study in Italy. Nat. Hazards 2012, 62, 551–573. [Google Scholar] [CrossRef]
- European Commission. Risk Assessment and Mapping Guidelines for Disaster Management; Technical Report, Commission Staff Working Paper, SEC (2010) 1626 Final, Brussels; European Commission: Brussels, Belgium, 2010. [Google Scholar]
- Liu, Z.; Nadim, F.; Garcia-Aristizabal, A.; Mignan, A.; Fleming, K.; Luna, B.Q. A three-level framework for multi-risk assessment. Georisk Assess. Manag. Risk Eng. Syst. Geohazards 2015, 9, 59–74. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Nadim, F.; Vangelsten, B.V.; Eidsvig, U.; Kalsnes, B. Quantitative multi-risk modelling and management using Bayesian networks. In Landslide Science for a Safer Geoenvironment; Springer: Berlin/Heidelberg, Germany, 2014; pp. 773–779. [Google Scholar]
- Ni, H.; Chen, A.; Chen, N. Some extensions on risk matrix approach. Saf. Sci. 2010, 48, 1269–1278. [Google Scholar] [CrossRef]
- Komendantova, N.; Mrzyglocki, R.; Mignan, A.; Khazai, B.; Wenzel, F.; Patt, A.; Fleming, K. Multi-hazard and multi-risk decision-support tools as a part of participatory risk governance: Feedback from civil protection stakeholders. Int. J. Disaster Risk Reduct. 2014, 8, 50–67. [Google Scholar] [CrossRef] [Green Version]
- Waller, M.A. Resilience in ecosystemic context: Evolution of the concept. Am. J. Orthopsychiatry 2001, 71, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Bruneau, M.; Chang, S.E.; Eguchi, R.T.; Lee, G.C.; O’Rourke, T.D.; Reinhorn, A.M.; Shinozuka, M.; Tierney, K.; Wallace, W.A.; Von Winterfeldt, D. A framework to quantitatively assess and enhance the seismic resilience of communities. Earthq. Spectra 2003, 19, 733–752. [Google Scholar] [CrossRef] [Green Version]
- Johnson, J.L.; Wiechelt, S.A. Introduction to the special issue on resilience. Subst. Use Misuse 2004, 39, 657–670. [Google Scholar] [CrossRef]
- Van der Leeuw, S.E.; Aschan-Leygonie, C. A long-term perspective on resilience in socio-natural systems. In Micro-Meso-Macro: Addressing Complex Systems Couplings; World Scientific: London, UK, 2005; pp. 227–264. [Google Scholar]
- Magis, K. Community resilience: An indicator of social sustainability. Soc. Nat. Resour. 2010, 23, 401–416. [Google Scholar] [CrossRef]
- Vallejo, L.; Mullan, M. Climate-Resilient Infrastructure; OECD: Paris, France, 2017. [Google Scholar]
- Nikolaou, S.; Kourkoulis, R.; Diaz-Fanas, G. Earthquake-Resilient Infrastructure: The Missing Link. In Proceedings of the Geotechnical Earthquake Engineering and Soil Dynamics V, Austin, TX, USA, 10–13 June 2018; pp. 79–90. [Google Scholar] [CrossRef]
- Lhomme, S.; Serre, D.; Diab, Y.; Laganier, R. Analyzing resilience of urban networks: A preliminary step towards more flood resilient cities. Nat. Hazards Earth Syst. Sci. 2013, 13, 221. [Google Scholar] [CrossRef] [Green Version]
- Litman, T. Pandemic-Resilient Community Planning: Practical Ways to Help Communities Prepare for, Respond to, and Recover from Pandemics and Other Economic, Social and Environmental Shocks; Victoria Transport Policy Institute: Victoria, BC, Canada, 2020. [Google Scholar]
- Takian, A.; Raoofi, A.; Kazempour-Ardebili, S. COVID-19 battle during the toughest sanctions against Iran. Lancet 2020, 395, 1035. [Google Scholar] [CrossRef]
- Legido-Quigley, H.; Asgari, N.; Teo, Y.Y.; Leung, G.M.; Oshitani, H.; Fukuda, K.; Cook, A.R.; Hsu, L.Y.; Shibuya, K.; Heymann, D. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet 2020, 395, 848–850. [Google Scholar] [CrossRef] [Green Version]
- Legido-Quigley, H.; Mateos-García, J.T.; Campos, V.R.; Gea-Sánchez, M.; Muntaner, C.; McKee, M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health 2020, 5, e251–e252. [Google Scholar] [CrossRef] [Green Version]
- Santarone, K.; McKenney, M.; Elkbuli, A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am. J. Emerg. Med. 2020, 38, 1530–1531. [Google Scholar] [CrossRef] [PubMed]
- Plomecka, M.B.; Gobbi, S.; Neckels, R.; Radziński, P.; Skórko, B.; Lazerri, S.; Almazidou, K.; Dedić, A.; Bakalović, A.; Hrustić, L.; et al. Mental Health Impact of COVID-19: A global study of risk and resilience factors. medRxiv 2020. [Google Scholar] [CrossRef]
- Rahman, M.; Chowdhury, M.; Garcia-Ballestas, E.; Florez, W.; Agrawal, A.; Moscote-Salazar, L.R. COVID 19 and Resilience: Neurosurgical perspectives. World Neurosurg. 2020, 426. [Google Scholar] [CrossRef]
- D’Orazio, M.; Bernardini, G.; Quagliarini, E. Sustainable and resilient strategies for touristic cities against COVID-19: An agent-based approach. arXiv 2020, arXiv:2005.12547. [Google Scholar]
- Worstell, J. Ecological resilience of food systems in response to the COVID-19 crisis. J. Agric. Food Syst. Community Dev. 2020, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Golan, M.S.; Jernegan, L.H.; Linkov, I. Trends and applications of resilience analytics in supply chain modeling: Systematic literature review in the context of the COVID-19 pandemic. In Environment Systems & Decisions; Springer: Berlin/Heidelberg, Germany, 2020; pp. 222–243. [Google Scholar]
- Hart, C.; Nash, F. Teacher Resilience during COVID: Burnout and Trauma; RTI Press: Research Triangle Park, NC, USA, 2020. [Google Scholar]
- Baldwin, R.; Evenett, S. COVID-19 and Trade Policy: Why Turning Inward Won’t Work; VoxEU: London, UK, 2020. [Google Scholar]
- Amekudzi-Kennedy, A.; Labi, S.; Woodall, B.; Marsden, G.; Grubert, E. Role of Socially-Equitable Economic Development in Creating Resilient and Sustainable Systems: COVID-19-Related Reflections. Engineering 2020. [Google Scholar] [CrossRef]
- Bostrom, A.; Bohm, G.; OConnor, R.E.; Hanss, D.; Bodi-Fernandez, O.; Halder, P. Comparative risk science for the coronavirus pandemic. J. Risk Res. 2020, 1–10. [Google Scholar] [CrossRef]
- Bryce, C.; Ring, P.; Ashby, S.; Wardman, J. Resilience in the face of uncertainty: Early lessons from the COVID-19 pandemic. J. Risk Res. 2020, 1–8. [Google Scholar] [CrossRef]
- Barton, M.A.; Christianson, M.; Myers, C.G.; Sutcliffe, K. Resilience in action: Leading for resilience in response to COVID-19. BMJ Lead. 2020. [Google Scholar] [CrossRef]
- Sadati, A.K.; MH, B.L.; Bagheri Lankarani, K. Risk Society, Global Vulnerability and Fragile Resilience; Sociological View on the Coronavirus Outbreak. Shiraz E-Med. J. 2020, 21, e102263. [Google Scholar] [CrossRef] [Green Version]
- Collins, A.; Florin, M.V.; Renn, O. COVID-19 risk governance: Drivers, responses and lessons to be learned. J. Risk Res. 2020, 1–10. [Google Scholar] [CrossRef]
- Aven, T.; Bouder, F. The COVID-19 pandemic: How can risk science help? J. Risk Res. 2020, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Dryhurst, S.; Schneider, C.R.; Kerr, J.; Freeman, A.L.; Recchia, G.; Van Der Bles, A.M.; Spiegelhalter, D.; van der Linden, S. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020, 1–13. [Google Scholar] [CrossRef]
- Trump, B.D.; Linkov, I. Risk and resilience in the time of the COVID-19 crisis. In Environment Systems and Decisions; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Fakhruddin, B.; Blanchard, K.; Ragupathy, D. Are we there yet? The transition from response to recovery for the COVID-19 pandemic. In Progress in Disaster Science; Elsevier: Amsterdam, The Netherlands, 2020; p. 100102. [Google Scholar]
- Menoni, S.; Schwarze, R. Recovery during a crisis: Facing the challenges of risk assessment and resilience management of COVID-19. Environ. Syst. Decis. 2020, 40, 1–10. [Google Scholar] [CrossRef]
- Jovanovic, A.; Klimek, P.; Renn, O.; Schneider, R.; Chakravarty, S.; Brown, J.; DiGennaro, M.; Liu, Y.; Pfau, V.; Jelic, M.; et al. Assessing resilience of healthcare infrastructure exposed to COVID-19: Emerging risks, resilience indicators, interdependencies and international standards. Environ. Syst. Decis. 2020. [Google Scholar] [CrossRef]
- Pelechano, N.; Malkawi, A. Evacuation simulation models: Challenges in modeling high rise building evacuation with cellular automata approaches. Autom. Constr. 2008, 17, 377–385. [Google Scholar] [CrossRef]
- Kuligowski, E.D.; Peacock, R.D.; Hoskins, B.L. A Review of Building Evacuation Models; US Department of Commerce, National Institute of Standards and Technology: Washington, DC, USA, 2005. [Google Scholar]
- Pelechano, N.; Badler, N.I. Modeling crowd and trained leader behavior during building evacuation. IEEE Comput. Graph. Appl. 2006, 26, 80–86. [Google Scholar] [CrossRef] [Green Version]
- Shen, T.S. ESM: A building evacuation simulation model. Build. Environ. 2005, 40, 671–680. [Google Scholar] [CrossRef]
- Shi, J.; Ren, A.; Chen, C. Agent-based evacuation model of large public buildings under fire conditions. Autom. Constr. 2009, 18, 338–347. [Google Scholar] [CrossRef]
- Bernardini, G.; D’Orazio, M.; Quagliarini, E.; Spalazzi, L. An agent-based model for earthquake pedestrians’ evacuation simulation in urban scenarios. Transp. Res. Procedia 2014, 2, 255–263. [Google Scholar] [CrossRef] [Green Version]
- Goto, Y.; Affan, M.; Nurdin, Y.; Yuliana, D.K.; Ardiansyah. Tsunami evacuation simulation for disaster education and city planning. J. Disaster Res. 2012, 7, 92–101. [Google Scholar] [CrossRef]
- King, M.A.; Niven, A.S.; Beninati, W.; Fang, R.; Einav, S.; Rubinson, L.; Kissoon, N.; Devereaux, A.V.; Christian, M.D.; Grissom, C.K. Evacuation of the ICU: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014, 146, e44S–e60S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Čivljak, R.; Markotić, A.; Capak, K. Earthquake in the time of COVID-19: The story from Croatia (CroVID-20). J. Glob. Health 2020, 10, e010349. [Google Scholar] [CrossRef] [PubMed]
- Putz, C. 70,000 Evacuated After Breach in Uzbek Dam, Investigation Into Failure Launched; The Diplomat: Tokyo, Japan, 2020. [Google Scholar]
- World Meteorological Organization. Tropical Cyclone Harold Challenges Disaster and Public Health Management; World Meteorological Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Keenan, J.M. COVID, resilience, and the built environment. In Environment Systems and Decisions; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1–6. [Google Scholar]
- Haas, C. Coronavirus and risk analysis. Risk Anal. 2020, 40, 660. [Google Scholar] [CrossRef] [PubMed] [Green Version]


© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hariri-Ardebili, M.A. Living in a Multi-Risk Chaotic Condition: Pandemic, Natural Hazards and Complex Emergencies. Int. J. Environ. Res. Public Health 2020, 17, 5635. https://doi.org/10.3390/ijerph17165635
Hariri-Ardebili MA. Living in a Multi-Risk Chaotic Condition: Pandemic, Natural Hazards and Complex Emergencies. International Journal of Environmental Research and Public Health. 2020; 17(16):5635. https://doi.org/10.3390/ijerph17165635
Chicago/Turabian StyleHariri-Ardebili, Mohammad Amin. 2020. "Living in a Multi-Risk Chaotic Condition: Pandemic, Natural Hazards and Complex Emergencies" International Journal of Environmental Research and Public Health 17, no. 16: 5635. https://doi.org/10.3390/ijerph17165635
APA StyleHariri-Ardebili, M. A. (2020). Living in a Multi-Risk Chaotic Condition: Pandemic, Natural Hazards and Complex Emergencies. International Journal of Environmental Research and Public Health, 17(16), 5635. https://doi.org/10.3390/ijerph17165635




