Compensatory Health Beliefs on Breastfeeding Varying by Breastfeeding Status; A Scale Development
Abstract
:1. Introduction
The Present Study
2. Methods
2.1. Participants
2.2. Design and Procedure
3. Measures
3.1. Breastfeeding Status
3.2. Birth Experience
3.3. Compensatory Health Beliefs on Breastfeeding (CHB-BF)
3.4. Demographic Information
3.5. Data Analysis: Scale Development
3.6. Scale Analysis
4. Results
4.1. Participants’ Characteristics
4.2. Reliability and Structure of the CHB-BF Scale
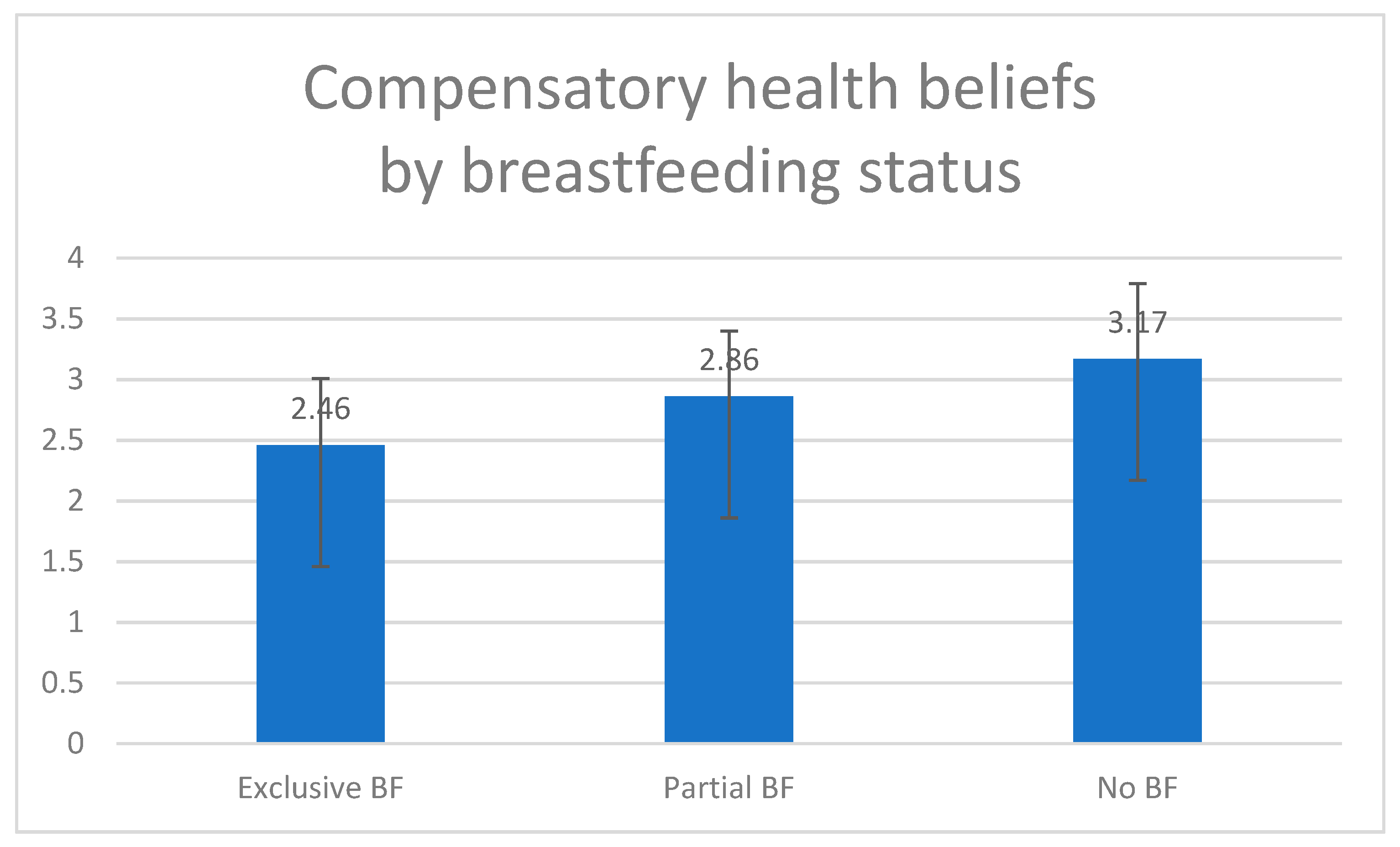
4.3. Comparing the CHB of the Breastfeeding Groups
5. Discussion
5.1. Summary
5.2. Comparison with Prior Work
5.3. Limitations and Strengths
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Availability of Data and Material
References
- World Health Organization. The Optimal Duration of Exclusive Breastfeeding: Report of an Expert Consultation; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Eidelman, A.I. Breastfeeding and the Use of Human Milk: An Analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeed. Med. 2012, 7, 323–324. [Google Scholar] [CrossRef]
- Grummer-Strawn, L.M.; Rollins, N. Summarising the health effects of breastfeeding. Acta Paediatr. Int. J. Paediatr. 2015, 104, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Victora, C.G.; Bahl, R.; Barros, A.J.D.; França, G.V.A.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C.; et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef] [Green Version]
- Heinig, M.J.; Dewey, K.G. Health Advantages of Breast Feeding for Infants: A Critical Review. Nutr. Res. Rev. 1996, 9, 89. [Google Scholar] [CrossRef]
- Heinig, M.J.; Dewey, K.G. Health effects of breast feeding for mothers: A critical review. Nutr. Res. Rev. 1997, 10, 35–56. [Google Scholar] [CrossRef]
- Rollins, N.C.; Bhandari, N.; Hajeebhoy, N.; Horton, S.; Lutter, C.K.; Martines, J.C.; Piwoz, E.G.; Richter, L.M.; Victora, C.G. Why invest, and what it will take to improve breastfeeding practices? Lancet 2016, 387, 491–504. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy for Infant and Young Child Feeding; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Abrahams, S.W. Milk and social media: Online communities and the international code of marketing of breast-milk substitutes. J. Hum. Lact. 2012, 28, 400–406. [Google Scholar] [CrossRef]
- Liu, A.; Dai, Y.; Xie, X.; Chen, L. Implementation of International Code of Marketing Breast-Milk Substitutes in China. Breastfeed. Med. 2014, 9, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Hsia, J.; Fridinger, F.; Hussain, A.; Benton-Davis, S.; Grummer-Strawn, L. Public beliefs about breastfeeding policies in various settings. J. Am. Diet. Assoc. 2004, 104, 1162–1168. [Google Scholar] [CrossRef] [PubMed]
- BouDiab, S.; Werle, C. What motivates women to breastfeed in Lebanon: An exploratory qualitative analysis. Appetite 2018, 123, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Niela-Vilén, H.; Axelin, A.; Melender, H.L.; Salanterä, S. Aiming to be a breastfeeding mother in a neonatal intensive care unit and at home: A thematic analysis of peer-support group discussion in social media. Matern. Child Nutr. 2015, 11, 712–726. [Google Scholar] [CrossRef] [PubMed]
- Wolynn, T. Using Social Media to Promote and Support Breastfeeding. Breastfeed. Med. 2012, 7, 364–365. [Google Scholar] [CrossRef] [PubMed]
- Bahkali, S.; Alkharjy, N.; Alowairdy, M.; Househ, M.; Da’ar, O.; Alsurimi, K. A Social Media Campaign to Promote Breastfeeding among Saudi Women: A Web-based Survey Study. Stud. Health Technol. Inform. 2015, 213, 247–250. [Google Scholar] [PubMed]
- Giles, M.; Connor, S.; McClenahan, C.; Mallett, J.; Stewart-Knox, B.; Wright, M. Measuring young people’s attitudes to breastfeeding using the Theory of Planned Behaviour. J. Public Health 2007, 29, 17–26. [Google Scholar] [CrossRef] [Green Version]
- Doulougeri, K.; Panagopoulou, E.; Montgomery, A. The impact of maternal stress on initiation andestablishment of breastfeeding. J. Neonatal Nurs. 2013, 19, 162–167. [Google Scholar] [CrossRef]
- Neter, E.; Goren, S. Infertility Centrality in the Woman’s Identity and Goal Adjustment Predict Psychological Adjustment Among Women in Ongoing Fertility Treatments. Int. J. Behav. Med. 2017, 24, 880–892. [Google Scholar] [CrossRef]
- Israel Center for Disease Control. Infant Health and Nutrition Survey Israel, 2009–2012; Israel Center for Disease Control: Ramat Gan, Isearl, 2012.
- Knäuper, B.; Rabiau, M.; Cohen, O.; Patriciu, N. Compensatory health beliefs: Scale development and psychometric properties. Psychol. Heal. 2004, 19, 607–624. [Google Scholar] [CrossRef]
- Kronick, I.; Knäuper, B. Temptations elicit compensatory intentions. Appetite 2010, 54, 398–401. [Google Scholar] [CrossRef]
- Dijkstra, A. Disengagement beliefs in smokers: Do they influence the effects of a tailored persuasive message advocating smoking cessation? Psychol. Health 2009, 24, 791–804. [Google Scholar] [CrossRef]
- Kleinjan, M.; Van den Eijnden, R.J.J.M.; Dijkstra, A.; Brug, J.; Engels, R.C.M.E. Excuses to continue smoking: The role of disengagement beliefs in smoking cessation. Addict. Behav. 2006, 31, 2223–2237. [Google Scholar] [CrossRef] [Green Version]
- Radtke, T.; Scholz, U.; Keller, R.; Hornung, R. Smoking is ok as long as I eat healthily: Compensatory Health Beliefs and their role for intentions and smoking within the Health Action Process Approach. Psychol. Health 2012, 27, 91–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleig, L.; Ngo, J.; Roman, B.; Ntzani, E.; Satta, P.; Warner, L.M.; Schwarzer, R.; Brandi, M.L. Beyond single behaviour theory: Adding cross-behaviour cognitions to the health action process approach. Br. J. Health Psychol. 2015. [Google Scholar] [CrossRef] [PubMed]
- Matley, F.A.I.; Davies, E.L. Resisting temptation: Alcohol specific self-efficacy mediates the impacts of compensatory health beliefs and behaviours on alcohol consumption. Psychol. Health. Med. 2017, 8506, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ernsting, A.; Schwarzer, R.; Lippke, S.; Schneider, M. “I do not need a flu shot because I lead a healthy lifestyle”: Compensatory health beliefs make vaccination less likely. J. Health Psychol. 2013, 18, 825–836. [Google Scholar] [CrossRef]
- Neter, E.; Levi, B. My child doesn’t Need to be vaccinated because we lead a healthy lifestyle: Compensatory health beliefs predicting intentions and reported child vaccination. Arch. Community Med. Public Health 2015, 1, 22–25. [Google Scholar]
- Schmied, V.; Lupton, D. Blurring the boundaries: Breastfeeding and maternal subjectivity. Sociol. Health Illn. 2001, 23, 234–250. [Google Scholar] [CrossRef]
- Forster, D.A.; McLachlan, H.L. Women’s views and experiences of breast feeding: Positive, negative or just good for the baby? Midwifery 2010, 26, 116–125. [Google Scholar] [CrossRef]
- French, D.P.; Cooke, R.; Mclean, N.; Williams, M.; Sutton, S. What do people think about when they answer theory of planned behaviour questionnaires? A “think aloud” study. J. Health Psychol. 2007, 12, 672–687. [Google Scholar] [CrossRef] [Green Version]
- Sutton, S.; French, D.P. Planning research: Design, sample, measures. In Health Psychology in Practice; Michie, S., Abrahams, C., Eds.; BPS Blackwell: Oxford, UK, 2004; pp. 83–103. ISBN 9780470694008. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 23.0, 2015; IBM Corp: Chicago, IL, USA, 2015. [Google Scholar]
- Murphy, E. “Breast is best”: Infant feeding decisions and maternal deviance. Sociol. Health Illn. 1999, 21, 187–208. [Google Scholar] [CrossRef]
- West, J.; Guelfi, K.J.; Dimmock, J.A.; Jackson, B. “I deserve a treat”: Exercise motivation as a predictor of post-exercise dietary licensing beliefs and implicit associations toward unhealthy snacks. Psychol. Sport Exerc. 2017, 32, 93–101. [Google Scholar] [CrossRef]
- Kaplan, K.J. On the ambivalence-indifference problem in attitude theory and measurement: A suggested modification of the semantic differential technique. Psychol. Bull. 1972, 77, 361–372. [Google Scholar] [CrossRef]
| Items | Item-Total Correlation | Loading on Factor (a, b, c) |
|---|---|---|
| 0.59 | 0.68 a |
| 0.47 | 0.56 a |
| 0.47 | 0.55 b |
| 0.42 | 0.49 a |
| 0.38 | 0.47 a |
| 0.27 | 0.73 c |
| 0.54 | 0.63 a |
| 0.66 | 0.74 a |
| 0.67 | 0.77 a |
| 0.58 | 0.54 a |
| 0.56 | 0.47 a |
| 0.65 | 0.74 a |
| 0.66 | 0.77 a |
| 0.39 | 0.61 b |
| 0.57 | 0.64 a |
| Variable | N (%) | Mean (SD) |
|---|---|---|
| Age, in years | ||
| Range; Interquartile Range | 18–49; 30–36 | |
| Mean (SD) | 32.86 (4.52) | |
| Education | N (%) | |
| Secondary | 65 (8.4) | |
| Post-secondary | 114 (14.7) | |
| Tertiary | 594 (76.9) | |
| Income | N (%) | |
| Average and above | 593 (76.7) | |
| Marital Status | N (%) | |
| Married/cohabitating | 757 (97.9) | |
| Divorced/widowed/Separated | 6 (0.8) | |
| Single | 10 (1.3) | |
| Infant’s age in months | ||
| Mean (SD); Interquartile Range | 12.15 (9.11); 5–17.50 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neter, E.; Bagants, L. Compensatory Health Beliefs on Breastfeeding Varying by Breastfeeding Status; A Scale Development. Int. J. Environ. Res. Public Health 2020, 17, 5759. https://doi.org/10.3390/ijerph17165759
Neter E, Bagants L. Compensatory Health Beliefs on Breastfeeding Varying by Breastfeeding Status; A Scale Development. International Journal of Environmental Research and Public Health. 2020; 17(16):5759. https://doi.org/10.3390/ijerph17165759
Chicago/Turabian StyleNeter, Efrat, and Levana Bagants. 2020. "Compensatory Health Beliefs on Breastfeeding Varying by Breastfeeding Status; A Scale Development" International Journal of Environmental Research and Public Health 17, no. 16: 5759. https://doi.org/10.3390/ijerph17165759






