Exploring the State of Gender-Centered Health Research in the Context of Refugee Resettlement in Canada: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
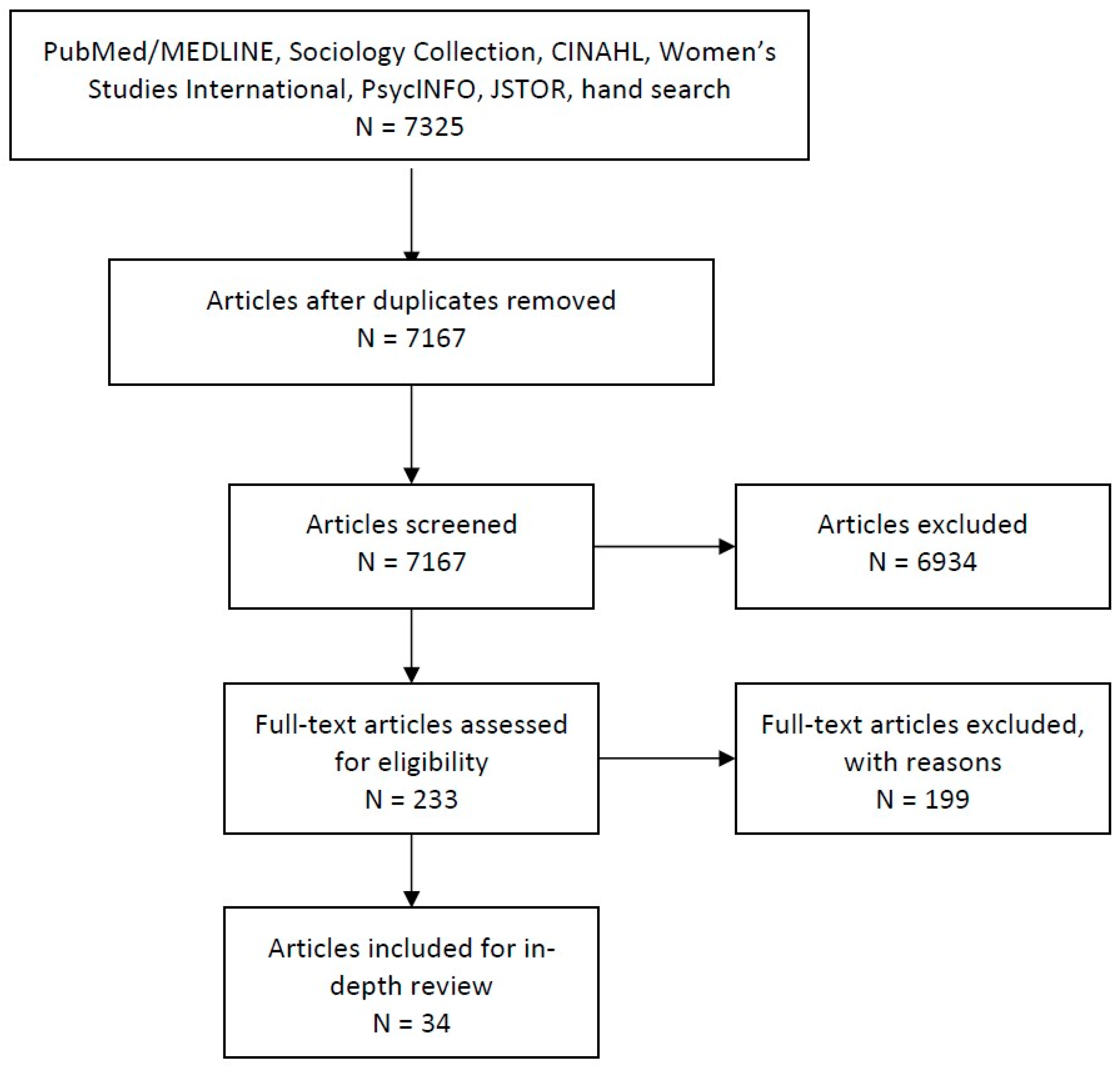
2.2. Study Selection
2.3. Data Management, Extraction, and Analysis
3. Results
3.1. Study Characteristics
3.1.1. Study Design
3.1.2. Study Populations
3.1.3. Article Focus
3.2. Results of Thematic Analysis
3.2.1. Micro Level: Gender, Health, and the Family
Challenges Fulfilling Gender Roles and Expectations within the Family
Changes in Gender Roles and Expectations and Family Dynamics
3.2.2. Meso Level: Gender, Social Support, and Community Building
Loss of Social Support Networks and Sense of Belonging
3.2.3. Macro Level: Gender and Health-Seeking Behavior, Access to Health and Health Services
Structural Barriers to Healthcare
Cultural Incongruity and Lack of Sensitivity
Confidentiality when Accessing Healthcare
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Government of Canada. Canada: A History of Refuge. Available online: https://www.canada.ca/en/immigration-refugees-citizenship/services/refugees/canada-role/timeline.html (accessed on 3 April 2020).
- Government of Canada. Resettlement Assistance Program (RAP) Service Provider Handbook. Available online: https://www.canada.ca/en/immigration-refugees-citizenship/corporate/publications-manuals/resettlement-assistance-program-handbook.html#s1-1 (accessed on 21 July 2020).
- Guruge, S.; Sidani, S.; Illesinghe, V.; Younes, R.; Bukhari, H.; Altenberg, J.; Rashid, M.; Fredericks, S. Healthcare needs and health service utilization by Syrian refugee women in Toronto. Confl. Health 2018, 12, 46. [Google Scholar] [CrossRef] [PubMed]
- Gushulak, B.D.; Pottie, K.; Roberts, J.H.; Torres, S.; DesMeules, M. Migration and health in Canada: Health in the global village. CMAJ 2011, 183, 952–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simich, L.; Beiser, M.; Stewart, M.; Mwakarimba, E. Providing social support for immigrants and refugees in Canada: Challenges and directions. J. Immigr. Minor. Health 2005, 7, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.; Dennis, C.L.; Kariwo, M.; Eastlick Kushner, K.; Letourneau, N.L.; Makumbe, K.; Makwarimba, E.; Shizha, E. Challenges faced by refugee new parents from Africa in Canada. J. Immigr. Minor. Health 2015, 17, 1146–1156. [Google Scholar] [CrossRef] [PubMed]
- Lamba, N.K. The employment experiences of Canadian refugees: Measuring the impact of human and social capital on quality of employment. Can. Rev. Sociol. 2003, 40, 45–64. [Google Scholar] [CrossRef]
- Krahn, H.; Derwing, T.; Mulder, M.; Wilkinson, L. Educated and underemployed: Refugee integration into the Canadian labour market. JIMI 2000, 1, 59–84. [Google Scholar] [CrossRef]
- Wilson, R.M.; Murtaza, R.; Shakya, Y.B. Pre-migration and post-migration determinants of mental health for newly arrived refugees in Toronto. In Canadian Issues—Thèmes Canadiennes; Public Health Agency of Canada: Ottawa, ON, Canada, 2010; p. 45. [Google Scholar]
- Beiser, M.; Goodwill, A.M.; Albanese, P.; McShane, K.; Kanthasamy, P. Predictors of the integration of Sri Lankan Tamil refugees in Canada: Pre-migration adversity, mental health, personal attributes, and post-migration experience. Int. J. Migrat. Health Soc. Care 2015, 11, 29–44. [Google Scholar] [CrossRef]
- Hynie, M. The social determinants of refugee mental health in the post-migration context: A critical review. Can. J. Psych. 2018, 63, 297–303. [Google Scholar] [CrossRef]
- Houle, R. Results from the 2016 Census: Syrian Refugees Who Resettled in Canada in 2015 and 2016; Statistics Canada: Ottawa, ON, Canada, 2018. Available online: https://www150.statcan.gc.ca/n1/en/pub/75-006-x/2019001/article/00001-eng.pdf?st=bOccZKIE (accessed on 21 July 2020).
- Gagnon, A.J.; Dougherty, G.; Wahoush, O.; Saucier, J.F.; Dennis, C.L.; Stanger, E.; Palmer, B.; Merry, L.; Stewart, D.E. International migration to Canada: The post-birth health of mothers and infants by immigration class. Soc. Sci. Med. 2013, 76, 197–207. [Google Scholar] [CrossRef] [Green Version]
- O’Mahony, J.; Donnelly, T. Immigrant and refugee women’s post-partum depression help-seeking experiences and access to care: A review and analysis of the literature. J. Psychiatr. Ment. Health Nurs. 2010, 17, 917–928. [Google Scholar] [CrossRef]
- Merry, L.A.; Gagnon, A.J.; Kalim, N.; Bouris, S.S. Refugee claimant women and barriers to health and social services post-birth. Can. J. Public Health 2011, 102, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Hynes, M.; Cardozo, B.L. Observations from the CDC: Sexual violence against refugee women. J Wom Health Gend. Base Med. 2000, 9, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Januwalla, A.; Pulver, A.; Wanigaratne, S.; O’Campo, P.; Urquia, M.L. Interventions to reduce adverse health outcomes resulting from manifestations of gender bias amongst immigrant populations: A scoping review. BMC Womens Health 2018, 18, 104. [Google Scholar] [CrossRef] [Green Version]
- Shishehgar, S.; Gholizadeh, L.; DiGiacomo, M.; Green, A.; Davidson, P.M. Health and socio-cultural experiences of refugee women: An integrative review. J. Immigr. Minor. Health 2017, 19, 959–973. [Google Scholar] [CrossRef] [PubMed]
- Patil, C.L.; Maripuu, T.; Hadley, C.; Sellen, D.W. Identifying gaps in health research among refugees resettled in Canada. Int. Migr. 2015, 53, 204–225. [Google Scholar] [CrossRef]
- Gabriel, P.S.; Morgan-Jonker, C.; Phung, C.M.W.; Barrios, R.; Kaczorowski, J. Refugees and health care–the need for data: Understanding the health of government-assisted refugees in Canada through a prospective longitudinal cohort. Can. J. Public Health 2011, 102, 269–272. [Google Scholar] [CrossRef]
- Oda, A.; Tuck, A.; Agic, B.; Hynie, M.; Roche, B.; McKenzie, K. Health care needs and use of health care services among newly arrived Syrian refugees: A cross-sectional study. CMAJ Open 2017, 5, 354. [Google Scholar] [CrossRef] [Green Version]
- Guruge, S.; Khanlou, N. Intersectionalities of influence: Researching the health of immigrant and refugee women. CJNR 2004, 36, 32–47. [Google Scholar]
- Kabeer, N. Reversed Realities: Gender Hierarchies in Development Thought; Verso: London, UK, 1994; p. 346. [Google Scholar]
- Srinivasan, S. Growing up unwanted: Girls’ experiences of gender discrimination and violence in Tamil Nadu, India. In Generationing Development; Palgrave Macmillan: London, UK, 2016; pp. 267–289. [Google Scholar]
- Rousseau, C.; Kirmayer, L.J. From complicity to advocacy: The necessity of refugee research. Am. J. Bioeth. 2010, 10, 65–67. [Google Scholar] [CrossRef]
- Hugman, R.; Pittaway, E.; Bartolomei, L. When ‘do no harm’ is not enough: The ethics of research with refugees and other vulnerable groups. Br. J. Soc. 2011, 41, 1271–1287. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Marie-Pierre, G.; Frances, G.; Belinda, N.; et al. Mixed methods appraisal tool (MMAT), version 2018. Educ. Inform. 2018, 34, 285–291. [Google Scholar] [CrossRef] [Green Version]
- Chulach, T.; Gagnon, M.; Holmes, D. The Lived Experience of Pregnancy among HIV-Positive Refugee Women. Adv. Nurs. Sci. 2016, 39, 130–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yohani, S.; Okeke-Ihejirika, P. Pathways to help-seeking and mental health service provision for African female survivors of conflict-related sexualized gender-based violence. Women Ther. 2018, 41, 380–405. [Google Scholar] [CrossRef]
- Mannion, C.A.; Raffin-Bouchal, S.; Henshaw, C.J. Navigating a strange and complex environment: Experiences of Sudanese refugee women using a new nutrition resource. Int. J. Womens Health 2014, 6, 411. [Google Scholar] [CrossRef] [Green Version]
- Floyd, A.; Sakellariou, D. Healthcare access for refugee women with limited literacy: Layers of disadvantage. Int. J. Equity Health 2017, 16, 195. [Google Scholar] [CrossRef] [Green Version]
- Dyck, I.; Dossa, P. Place, health and home: Gender and migration in the constitution of healthy space. Health Place 2007, 13, 691–701. [Google Scholar] [CrossRef]
- Donnelly, T.; Hwang, J.J.; Este, D.; Ewashen, C.; Adair, C.; Clinton, M. If I was going to kill myself, I wouldn’t be calling you. I am asking for help: Challenges influencing immigrant and refugee women’s mental health. Issues Ment. Health Nurs. 2011, 32, 279–290. [Google Scholar] [CrossRef]
- Clark, N. Exploring community capacity: Karen refugee women’s mental health. IJHRH 2018, 11, 244–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hurly, J. ‘I feel something is still missing’: Leisure meanings of African refugee women in Canada. Leis. Stud. 2019, 38, 1–14. [Google Scholar] [CrossRef]
- Simich, L.; Este, D.; Hamilton, H. Meanings of home and mental well-being among Sudanese refugees in Canada. Ethn. Health 2010, 15, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Racine, L.; Lu, Y. Refugees’ resettlement in a Canadian mid-sized prairie city: Examining experiences of multiple forced migrations. IJHRH 2015, 8, 173–186. [Google Scholar] [CrossRef]
- Affleck, W.; Thamotharampillai, U.; Jeyakumar, J.; Whitley, R. “If One Does Not Fulfil His Duties, He Must Not Be a Man”: Masculinity, Mental Health and Resilience Amongst Sri Lankan Tamil Refugee Men in Canada. Cult. Med. Psychiatry 2018, 42, 840–861. [Google Scholar] [CrossRef]
- Redwood-Campbell, L.; Thind, H.; Howard, M.; Koteles, J.; Fowler, N.; Kaczorowski, J. Understanding the health of refugee women in host countries: Lessons from the Kosovar re-settlement in Canada. Prehosp. Disaster. Med. 2008, 23, 322–327. [Google Scholar] [CrossRef] [Green Version]
- Kulig, J.C. Conception and birth control use: Cambodian refugee women’s beliefs and practices. J. Community Health Nurs. 1988, 5, 235–246. [Google Scholar] [CrossRef]
- Kowal, S.P.; Jardine, C.G.; Bubela, T.M. “If they tell me to get it, I’ll get it. If they don’t....”: Immunization decision-making processes of immigrant mothers. Can. J. Public Health 2015, 106, 230–235. [Google Scholar] [CrossRef]
- Higginbottom, G.M.A.; Safipour, J.; Mumtaz, Z.; Chiu, Y.; Paton, P.; Pillay, J. “I have to do what I believe”: Sudanese women’s beliefs and resistance to hegemonic practices at home and during experiences of maternity care in Canada. BMC Pregnancy Childbirth 2013, 13, 51. [Google Scholar] [CrossRef] [Green Version]
- Berman, H.; Girón, E.R.I.; Marroquín, A.P. A narrative study of refugee women who have experienced violence in the context of war. CJNR 2009, 41, 144–165. [Google Scholar]
- Moussa, H. Violence against refugee women: Gender oppression, Canadian policy and the international struggle for human rights. Resour. Fem. Res. 1998, 26, 79. [Google Scholar]
- Rousseau, C.; Drapeau, A.; Platt, R. Family environment and emotional and behavioural symptoms in adolescent Cambodian refugees: Influence of time, gender, and acculturation. Med. Confl. Surviv. 2004, 20, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Bokore, N. Suffering in silence: A Canadian-Somali case study. J. Soc. Work. Pract. 2013, 27, 95–113. [Google Scholar] [CrossRef]
- Rousseau, C.; Drapeau, A.; Platt, R. Family trauma and its association with emotional and behavioral problems and social adjustment in adolescent Cambodian refugees. Child. Abus. Negl. 1999, 23, 1263–1273. [Google Scholar] [CrossRef]
- Chung, K.; Hong, E.; Newbold, B. Resilience among single adult female refugees in Hamilton, Ontario. Refuge 2013, 29, 65–74. [Google Scholar]
- Ahmed, A.; Bowen, A.; Feng, C.X. Maternal depression in Syrian refugee women recently moved to Canada: A preliminary study. BMC Pregnancy Childbirth 2017, 17, 240. [Google Scholar] [CrossRef]
- Brown-Bowers, A.; McShane, K.; Wilson-Mitchell, K.; Gurevich, M. Postpartum depression in refugee and asylum-seeking women in Canada: A critical health psychology perspective. Health 2015, 19, 318–335. [Google Scholar] [CrossRef]
- Dennis, C.L.; Merry, L.; Gagnon, A.J. Postpartum depression risk factors among recent refugee, asylum-seeking, non-refugee immigrant, and Canadian-born women: Results from a prospective cohort study. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 411–422. [Google Scholar] [CrossRef]
- Beiser, M.; Hou, F. Predictors of positive mental health among refugees: Results from Canada’s General Social Survey. Transcult. Psychiatry 2017, 54, 675–695. [Google Scholar] [CrossRef]
- Kulig, J.C. Childbearing Beliefs among Cambodian Refugee Women. West J. Nurs. Res. 1990, 12, 108–118. [Google Scholar] [CrossRef]
- Wahoush, E.O. Equitable health-care access: The experiences of refugee and refugee claimant mothers with an ill preschooler. CJNR 2009, 41, 186–206. [Google Scholar] [PubMed]
- Yohani, S.C.; Hagen, K.T. Refugee women survivors of war related sexualised violence: A multicultural framework for service provision in resettlement countries. Intervention 2010, 8, 207–222. [Google Scholar] [CrossRef] [Green Version]
- Khanlou, N.; Haque, N.; Skinner, A.; Mantini, A.; Landy, C.K. Scoping review on maternal health among immigrant and refugee women in Canada: Prenatal, Intrapartum, and postnatal care. J. Pregnancy 2017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winn, A.; Hetherington, E.; Tough, S. Caring for pregnant refugee women in a turbulent policy landscape: Perspectives of health care professionals in Calgary, Alberta. Int. J. Equity Health 2018, 17, 91. [Google Scholar] [CrossRef] [Green Version]
- Edge, S.; Newbold, B. Discrimination and the health of immigrants and refugees: ExploringCanada’s evidence base and directions for future research in newcomer receiving countries. J. Immigr. Minor. Health 2013, 15, 141–148. [Google Scholar] [CrossRef]
- Kahn, S.; Alessi, E.J.; Kim, H.; Woolner, L.; Olivieri, C.J. Facilitating mental health support for LGBT forced migrants: A qualitative inquiry. J. Couns. Dev. 2018, 96, 316–326. [Google Scholar] [CrossRef]
- Fornazzari, X.; Freire, M. Women as victims of torture. Acta Psychiatr. Scand. 1990, 82, 257–260. [Google Scholar] [CrossRef]
- Okigbo, C.; Reierson, J.; Stowman, S. Leveraging acculturation through action research: A case study of refugee and immigrant women in the United States. Action Res. 2009, 7, 127–142. [Google Scholar] [CrossRef]
- Minkler, M. Using participatory action research to build healthy communities. Public Health Rep. 2000, 115, 191. [Google Scholar] [CrossRef]
- Baird, M.B.; Domian, E.W.; Mulcahy, E.R.; Mabior, R.; Jemutai-Tanui, G.; Filippi, M.K. Creating a Bridge of Understanding between Two Worlds: Community-Based Collaborative-Action Research with Sudanese Refugee Women. Public Health Nurs. 2015, 32, 388–396. [Google Scholar] [CrossRef]
| Refugee | refugee* OR forced migrant* OR forced migration |
| Health | health OR healthy OR wellbeing OR well-being OR well being OR wellness OR illness OR disease OR chronic OR disorder OR healthcare OR health services OR access to health OR quality of life |
| Gender | gender* OR woman OR women OR female OR mother* OR wife OR man OR men OR male OR father OR husband OR maternal OR paternal OR family OR families OR sex OR gender relations OR girl* OR boy* OR partner OR marriage OR married OR sex roles OR gender roles OR gender identity OR transgender OR spouse OR interpersonal relations |
| Canada | Canada OR Canadian OR Ontario OR Quebec OR British Columbia OR Nova Scotia OR Saskatchewan OR Alberta OR Manitoba OR Newfoundland and Labrador OR Newfoundland OR Prince Edward Island OR New Brunswick OR Yukon OR Northwest Territories OR Nunavut OR Toronto OR Vancouver OR Montreal |
| Level | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| 1. Title and abstract screening | Mentions refugees or migrants (unspecified) | Asylum-seekers (refugee claimant), immigrants, or other non-refugee migrant classes |
| Mentions one of the search terms for gender (exception of “sex”) | ||
| Any aspect of physical, mental, or emotional health | Sociocultural aspects or social determinants of health not clearly linked to health outcomes or access | |
| Study population in Canada | ||
| Academic journal article | ||
| 2. Full text screening | Article including or pertaining to those with refugee status | Articles that included individuals/ households with refugee status but aggregated data or did not specify status |
| Articles that examine (relational) aspects of gender: roles, expectations, beliefs, relations | Articles that used gender as a variable, focus on one gender but do not explore relations | |
| Focus of article is any aspect of physical, mental, or emotional health or a social determinant of health | ||
| Study Population is in Canada | Articles that included but were not limited to a study population from Canada, but did not specify resettlement country of participants in analysis | |
| Peer-reviewed academic journal article available in English |
| Author(s) Year | Study Population: Migrant Status and Gender | Study Design/Methodology | Objective of Article |
|---|---|---|---|
| Maternal Health | |||
| Ahmed, Bowen, Xin Feng 2017 | Refugees from Syria (status unspecified) Women | Mixed methods: focus groups, questionnaires | Understand and characterize maternal depression among Syrian refugee women |
| Brown-Bowers et al., 2015 | Refugees (status unspecified) Women | Theoretical | Describe experiences of postpartum depression in women from a critical psychology perspective/socioecological framework |
| Chulach, Gagnon, Holmes 2016 | Refugees who were HIV-positive (status unspecified) Women | Qualitative: semi-structured interviews | Describe and explore meaning and experience of pregnancy from the perspective of HIV-positive refugee women |
| Dennis, Merry, Gagnon 2017 | Refugees and other migrant classes with separated data Women | Quantitative: questionnaires | Identify risk factors for postpartum depression across migrant classes |
| Higginbottom 2013 | Refugees (status unspecified) Women | Qualitative: focus groups | Investigate beliefs around pregnancy and childbirth and discuss relationship between cultural/personal beliefs and maternity services |
| Khanlou et al., 2017 | Refugees and other migrant classes with separated data Women | Scoping review | Review on maternal health among immigrant and refugee women in Canada |
| Kulig 1989 | Refugees (status unspecified) Women | Qualitative: in-depth interviews, participant observation | Describe women’s cultural knowledge of conception and fetal development and the impact on birth control and prenatal care |
| Winn, Hetherington, Tough 2018 | Healthcare providers Women | Qualitative: in-depth and semi-structured interviews | Understand the experiences of healthcare providers of pregnant refugee women |
| Social and Emotional Health | |||
| Chung, Hong, Newbold 2013 | Refugees (status unspecified) Women | Qualitative: in-depth and semi-structured interviews | Examine how resilience is promoted, reinforced, or grown among low-income single refugee women |
| Dyck, Dossa 2007 | Refugees and other migrant classes with separated data Women | Qualitative: focus groups, semi-structured interviews | Describe practices and means through which women facilitate and create “healthy space”, as they pursue individual and family health in Canada |
| Edge, Newbold 2013 | Refugees and other migrant classes with separated data All genders | Scoping review | Describe existing knowledge on experiences of discrimination by newcomers and impact/relation with health and access to health services |
| Hurly 2019 | Refugees (status unspecified) Women | Qualitative: semi-structured interviews | Explore definitions of leisure and sources or practices of leisure of three resettled African refugee women |
| Racine, Lu 2015 | Refugees (status unspecified) All genders | Qualitative: in-depth interviews | Describe experiences of multiple forced displacements and resettlement in a mid-sized city |
| Rousseau, Drapeau, Platt 2004 | Refugees or refugee backgrounds from Cambodia (status unspecified) Youth All genders | Quantitative: in-depth interviews | Examine family environment and acculturation over adolescence and their emotional impacts on young Cambodian boys and girls |
| Rousseau, Drapeau, Platt 1999 | Refugees or refugee backgrounds from Cambodia (status unspecified) Youth All genders | Quantitative: questionnaires | Investigate the effect of war-related trauma on subsequent social adjustment and functioning of adolescent Cambodians with refugee background |
| Health Impacts of Sexual and Gender-Based Violence and Torture | |||
| Berman, Giron, Marroquin 2009 | Refugees (status unspecified) Women | Qualitative: in-depth interviews, focus groups | Describe experiences of refugee women who have experienced violence in context of war |
| Bokore 2013 | Government Assisted Refugees from Somalia Women | Qualitative: case studies | Describe pre- and post-migration experiences of Somali refugee women, particularly in relation to impacts of sexual and gender-based violence and trauma on health and wellbeing during resettlement |
| Fornazzari, Freire 1990 | Refugees (status unspecified) Women | Quantitative: case reports | Compare demographic information, psychological effects of torture and recovery rates of women who have experienced direct versus indirect psychological or physical torture |
| Moussa 1998 | Refugees (status unspecified) Women | Theoretical | Describe violence against women and gender oppression more broadly in the context of refugee crisis as well as in Canadian resettlement |
| Yohani, Hagen 2010 | Healthcare providers (Women) | Qualitative: case study | Institutional case study describing the author’s (healthcare provider) experience with facilitating a healing program for refugee women survivors of war-related sexual violence during resettlement, both challenges and impacts. |
| Access to Health and Social Services | |||
| Clark 2018 | Government Assisted Refugees Women Healthcare and social service providers | Qualitative: in-depth and semi-structured interviews, focus groups, participant observation | Describe Karen refugees’ experience with community support and factors impacting mental health during resettlement |
| Floyd, Sakellariou 2017 | Government Assisted Refugees from SSA Women | Qualitative: semi-structured interviews | Describe experiences of accessing healthcare of non-literate, non-English speaking women from sub-Saharan Africa (SSA) |
| Guruge et al., 2018 | Government Assisted Refugees from Syria Women | Qualitative: focus groups | Describe healthcare needs and experiences of recently resettled Syrian women |
| Kahn et al., 2018 | Refugees Healthcare and social service providers All genders | Qualitative: in-depth and semi-structured interviews | Describe pathways and barriers to mental health care for LGBTQ+ forced migrants |
| Redwood-Campbell et al., 2008 | Refugees from Kosovo Women Sponsors of Kosovar Refugees All genders | Mixed methods: questionnaires, focus groups | Describe Kosovar women’s unmet healthcare needs and barriers to accessing healthcare according to sponsors |
| Decision-Making and Health-Seeking Behavior | |||
| Donnelly et al., 2011 | Refugees and other migrant classes with separated data Women | Qualitative: in-depth interviews | Describe supports and barriers refugee and immigrant women face to accessing mental healthcare experiences services of refugee and immigrant women |
| Kowal, Jardine, Bubela 2015 | Refugees and other migrant classes with separated data Women | Qualitative: semi-structured interviews | Describe information-gathering and decision-making about self and child vaccine acceptance and uptake by migrant mothers |
| Mannion, Raffin-Bouchal, Henshaw 2014 | Government Assisted Refugees Women Healthcare providers | Qualitative: in-depth interviews, focus groups, participant observation | Evaluate acceptability of the “Market Guide” created by authors to assist refugees in grocery shopping during resettlement. Describe barriers to buying nutritional foods during resettlement |
| Wahoush 2009 | Refugees and refugee claimants with data separated Women | Mixed methods: focus groups, semi-structured interviews | Describe health-seeking behaviors of refugee mothers responding to an ill preschooler |
| Yohani, Okeke-Ihejirika 2018 | Healthcare providers | Qualitative: semi-structured interviews | Describe experiences and help-seeking behaviors of African refugee survivors of sexual and gender-based violence, from perspective of mental healthcare providers |
| Mental Health | |||
| Affleck et al., 2018 | Refugees (status unspecified) Men | Qualitative: in-depth interviews | Describe impacts of war, migration, and resettlement on mental health, specifically in relation to conceptions of masculinity |
| Beiser, Hou 2017 | Refugees and other migrant classes with separated data All genders | Quantitative: computer-assisted telephone interviews | Determine whether refugees have lower levels of positive mental health than economic and family class immigrants from the same source country, and if so what experiences contribute to this disadvantage and to what extent does gender modify the relationships between mental health and post-migration experience |
| Simich, Este, Hamilton 2010 | Refugees (unspecified)-Predominantly Government Assisted Refugees All genders | Mixed methods: in-depth interviews, surveys | Describe family and social factors that impact mental health during resettlement through conceptions of the meaning of “home” |
| Sexual and Reproductive Health | |||
| Kulig 1988 | Refugees (unspecified) Women | Qualitative: in-depth interviews, participant observation | Describe relationship between traditional knowledge around conception and the use of birth control Study population included one male traditional healer |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zivot, C.; Dewey, C.; Heasley, C.; Srinivasan, S.; Little, M. Exploring the State of Gender-Centered Health Research in the Context of Refugee Resettlement in Canada: A Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 7511. https://doi.org/10.3390/ijerph17207511
Zivot C, Dewey C, Heasley C, Srinivasan S, Little M. Exploring the State of Gender-Centered Health Research in the Context of Refugee Resettlement in Canada: A Scoping Review. International Journal of Environmental Research and Public Health. 2020; 17(20):7511. https://doi.org/10.3390/ijerph17207511
Chicago/Turabian StyleZivot, Chloe, Cate Dewey, Cole Heasley, Sharada Srinivasan, and Matthew Little. 2020. "Exploring the State of Gender-Centered Health Research in the Context of Refugee Resettlement in Canada: A Scoping Review" International Journal of Environmental Research and Public Health 17, no. 20: 7511. https://doi.org/10.3390/ijerph17207511
APA StyleZivot, C., Dewey, C., Heasley, C., Srinivasan, S., & Little, M. (2020). Exploring the State of Gender-Centered Health Research in the Context of Refugee Resettlement in Canada: A Scoping Review. International Journal of Environmental Research and Public Health, 17(20), 7511. https://doi.org/10.3390/ijerph17207511





