Risk Factors Associated with Malnutrition among Children Under-Five Years in Sub-Saharan African Countries: A Scoping Review
Abstract
1. Introduction
The Aim of the Scoping Review
2. Methodology
2.1. Design
2.2. Protocol and Registration Declaration
2.3. Identification of the Research Questions
- What are the existing examples of evidence of individual and contextual risk factors associated with the malnutrition status of children under five years in Sub-Saharan Africa countries?
- What evidence exists in the use of classical regression analysis methods to determine the risk factors related to the malnutrition of children under five years in Sub-Saharan African countries?
2.4. Eligibility Criteria
2.5. Identify the Relevant Sources of Evidence
Information Sources
2.6. Selection of Sources for Evidence and Eligibility Criteria
Search Strategy
2.7. Selection Process
2.8. Data Charting Management
3. Results
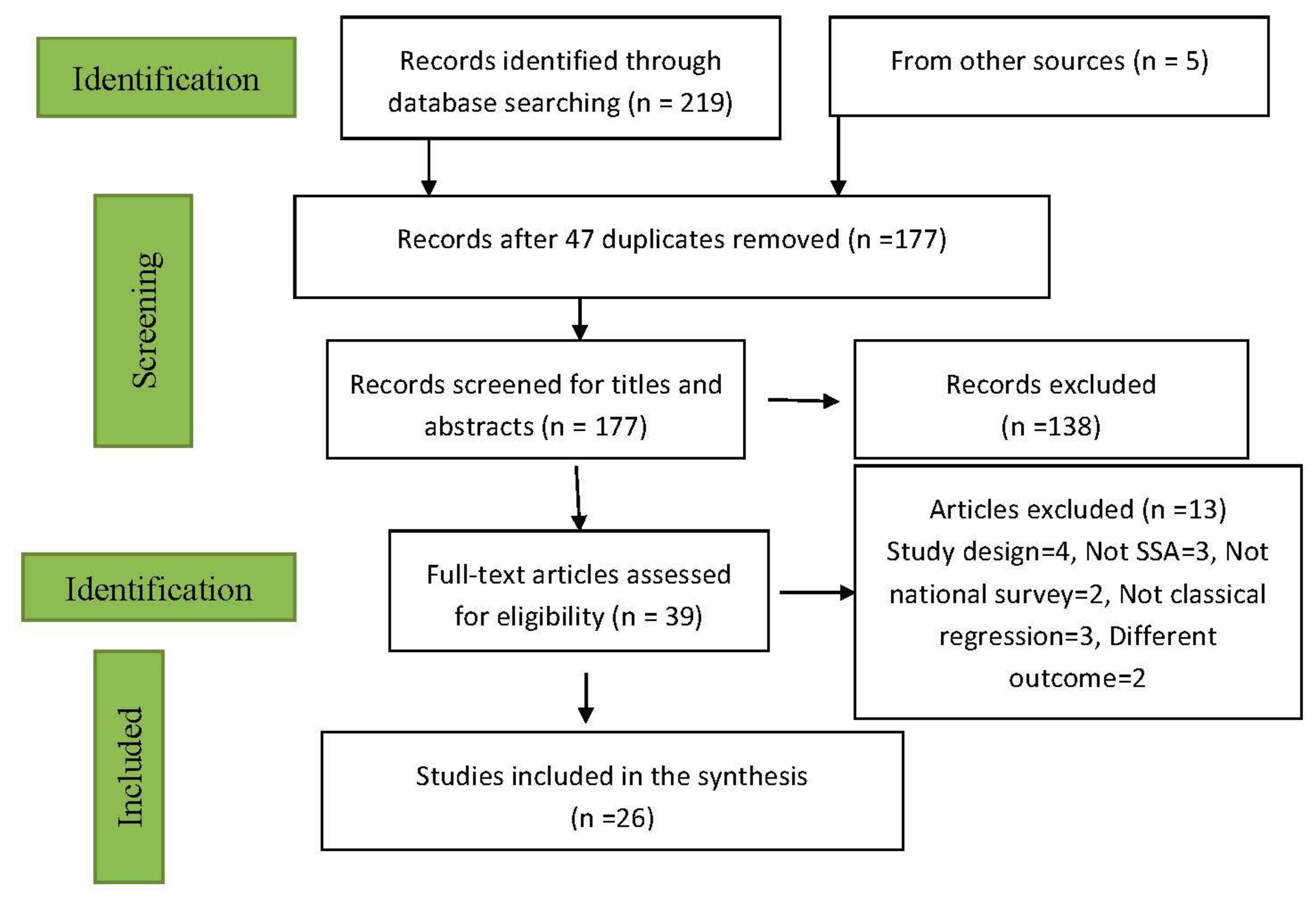
3.1. Selection of Sources of Evidence
3.2. Characteristics of Sources of Evidence
3.2.1. Characteristics of Study Setting
3.2.2. Characteristics of Study Analytical Methods
3.2.3. Characteristics of Study Outcomes
3.2.4. Characteristics of Significant Risk Factors
4. Discussion
5. Strengths and Limitations
6. Future Work
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organisation Fact Sheets—Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 31 May 2020).
- Simonyan, H.; Sargsyan, A.; Balalian, A.A.; Davtyan, K.; Gupte, H.A. Short-term nutrition and growth indicators in 6-month to 6-year-old children are improved following implementation of a multidisciplinary community-based programme in a chronic conflict setting. Public Health Nutr. 2020, 23, 134–145. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation WHO|Global Targets 2025. Available online: http://www.who.int/nutrition/global-target-2025/en/ (accessed on 11 August 2020).
- Martin Goal 2: Zero Hunger. Available online: https://www.un.org/sustainabledevelopment/hunger/ (accessed on 6 August 2020).
- Global Nutrition Report The Burden of Malnutrition. Available online: https://globalnutritionreport.org/reports/global-nutrition-report-2018/burden-malnutrition/ (accessed on 25 June 2020).
- UNICEF/WHO/World Bank Group Levels and Trends in Child Malnutrition: Key Findings of the 2019 Edition. Available online: https://www.who.int/nutgrowthdb/jme-2019-key-findings.pdf?ua=1 (accessed on 8 March 2020).
- Doctor, H.V.; Nkhana-Salimu, S. Trends and Determinants of Child Growth Indicators in Malawi and Implications for the Sustainable Development Goals. AIMS Public Health 2017, 4, 590. [Google Scholar] [CrossRef] [PubMed]
- Global Nutrition Report Africa Nutrition Profile. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/ (accessed on 6 August 2020).
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Wali, N.; Renzaho, A.M.N.; Merom, D. Stunting, wasting and underweight in Sub-Saharan Africa: A systematic review. Int. J. Environ. Res. Public Health 2017, 14, 863. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Merom, D.; Astell-Burt, T.; Renzaho, A.M. Stunting and severe stunting among children under-5 years in Nigeria: A multilevel analysis. BMC Pediatrics 2017, 17, 15. [Google Scholar] [CrossRef]
- McKenna, C.G.; Bartels, S.A.; Pablo, L.A.; Walker, M. Women’s decision-making power and undernutrition in their children under age five in the Democratic Republic of the Congo: A cross-sectional study. PLoS ONE 2019, 14, e0226041. [Google Scholar] [CrossRef]
- UNICEF 1 in 5 Children under Five Are Not Growing Well Due to Malnutrition in Latin America and the Caribbean, Warns UNICEF. Available online: https://www.unicef.org/lac/en/press-releases/1-in-5-children-under-five-are-not-growing-well-due-to-malnutrition-in-LAC (accessed on 21 November 2020).
- Amalia, P. Malnutrition among Children in Latin America and the Caribbean. Available online: https://www.cepal.org/en/insights/malnutrition-among-children-latin-america-and-caribbean (accessed on 21 November 2020).
- Institute of Child Health Micronutrient Malnutrition—Detection, Measurement and Intervention: A Training Package for Field Staff. Available online: https://www.unhcr.org/uk/45fa6dad2.pdf (accessed on 21 November 2020).
- Akombi, B.J.; Agho, K.E.; Merom, D.; Hall, J.J.; Renzaho, A.M. Multilevel Analysis of Factors Associated with Wasting and Underweight among Children Under-Five Years in Nigeria. Nutrients 2017, 9, 44. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Updates on the Management of Severe Acute Malnutrition in infants and Chldren; World Health Organization: Geneva, Switzerland, 2013; ISBN 978-92-4-150203-0. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- FDA Media Using the PICOTS Framework to Strengthen Evidence Gathered in Clinical Trials—Guidance from the AHRQ’s Evidence-based Practice Centers Program. Available online: https://www.fda.gov/media/109448/download (accessed on 21 November 2020).
- Maphosa, T.P.; Mulqueeny, D.M.; Osei, E.; Kuupiel, D.; Mashamba-Thompson, T.P. Mapping evidence on malnutrition screening tools for children under 5 years in sub-Saharan Africa: A scoping review protocol. Syst. Rev. 2020, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Larissa Shamseer, D.M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Adekanmbi, V.T.; Kayode, G.A.; Uthman, O.A. Individual and contextual factors associated with childhood stunting in Nigeria: A multilevel analysis. Matern. Child Nutr. 2013, 9, 244–259. [Google Scholar] [CrossRef] [PubMed]
- Akombi, B.J.; Agho, K.E.; Renzaho, A.M.; Hall, J.J.; Merom, D.R. Trends in socioeconomic inequalities in child undernutrition: Evidence from Nigeria Demographic and Health Survey (2003–2013). PLoS ONE 2019, 14, e0211883. [Google Scholar] [CrossRef] [PubMed]
- Ntoimo, L.F.C.; Odimegwu, C.O. Health effects of single motherhood on children in sub-Saharan Africa: A cross-sectional study. BMC Public Health 2014, 14, 1145. [Google Scholar] [CrossRef] [PubMed]
- Ukwuani, F.A.; Suchindran, C.M. Implications of women’s work for child nutritional status in sub-Saharan Africa: A case study of Nigeria. Soc. Sci. Med. 2003, 56, 2109–2121. [Google Scholar] [CrossRef]
- Amare, Z.Y.; Ahmed, M.E.; Mehari, A.B. Determinants of nutritional status among children under age 5 in Ethiopia: Further analysis of the 2016 Ethiopia demographic and health survey. Glob. Health 2019, 15, 62. [Google Scholar] [CrossRef]
- Gebru, K.F.; Haileselassie, W.M.; Temesgen, A.H.; Seid, A.O.; Mulugeta, B.A. Determinants of stunting among under-five children in Ethiopia: A multilevel mixed-effects analysis of 2016 Ethiopian demographic and health survey data. BMC Pediatrics 2019, 19, 176. [Google Scholar]
- Kuche, D.; Moss, C.; Eshetu, S.; Ayana, G.; Salasibew, M.; Dangour, A.D.; Allen, E. Factors associated with dietary diversity and length-for-age z-score in rural Ethiopian children aged 6–23 months: A novel approach to the analysis of baseline data from the Sustainable Undernutrition Reduction in Ethiopia evaluation. Matern. Child Nutr. 2020, 16. [Google Scholar] [CrossRef]
- Takele, K.; Zewotir, T.; Ndanguza, D. Understanding correlates of child stunting in Ethiopia using generalized linear mixed models. BMC Public Health 2019, 19, 626. [Google Scholar] [CrossRef]
- Acharya, Y.; Naz, S.; Galway, L.P.; Jones, A.D. Deforestation and Household- and Individual-Level Double Burden of Malnutrition in Sub-saharan Africa. Front. Sustain. Food Syst. 2020, 4. [Google Scholar] [CrossRef]
- Magadi, M.A. Household and community HIV/AIDS status and child malnutrition in sub-Saharan Africa: Evidence from the demographic and health surveys. Soc. Sci. Med. 2011, 73, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Tusting, L.S.; Gething, P.W.; Gibson, H.S.; Greenwood, B.; Knudsen, J.; Lindsay, S.W.; Bhatt, S. Housing and child health in sub-Saharan Africa: A cross-sectional analysis. PLoS Med. 2020, 17, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Yaya, S.; Uthman, O.A.; Ekholuenetale, M.; Bishwajit, G.; Adjiwanou, V. Effects of birth spacing on adverse childhood health outcomes: Evidence from 34 countries in sub-Saharan Africa. J. Matern. Fetal. Neonatal. Med. 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Agadjanian, V.; Prata, N. Civil war and child health: Regional and ethnic dimensions of child immunization and malnutrition in Angola. Soc. Sci. Med. 2003, 56, 2515–2527. [Google Scholar] [CrossRef]
- Aheto, J.M.K. Simultaneous quantile regression and determinants of under-five severe chronic malnutrition in Ghana. BMC Public Health 2020, 20. [Google Scholar] [CrossRef]
- Amaral, M.M.; Herrin, W.E.; Gulere, G.B. Using the Uganda National Panel Survey to analyze the effect of staple food consumption on undernourishment in Ugandan children. BMC Public Health 2017, 18, 32. [Google Scholar] [CrossRef]
- Custodio, E.; Descalzo, M.A.; Roche, J.; Sánchez, I.; Molina, L.; Lwanga, M.; Bernis, C.; Villamor, E.; Baylin, A. Nutritional status and its correlates in Equatorial Guinean preschool children: Results from a nationally representative survey. Food Nutr. Bull. 2008, 29, 49–58. [Google Scholar] [CrossRef]
- Kennedy, G.; Nantel, G.; Brouwer, I.D.; Kok, F.J. Does living in an urban environment confer advantages for childhood nutritional status? Analysis of disparities in nutritional status by wealth and residence in Angola, Central African Republic and Senegal. Public Health Nutr. 2006, 9, 187–193. [Google Scholar] [CrossRef][Green Version]
- Machisa, M.; Wichmann, J.; Nyasulu, P.S. Biomass fuel use for household cooking in Swaziland: Is there an association with anaemia and stunting in children aged 6–36 months? Trans. R. Soc. Trop. Med. Hyg. 2013, 107, 535–544. [Google Scholar] [CrossRef]
- Miller, C.M.; Gruskin, S.; Subramanian, S.V.; Heymann, J. Emerging health disparities in Botswana: Examining the situation of orphans during the AIDS epidemic. Soc. Sci. Med. 2007, 64, 2476–2486. [Google Scholar] [CrossRef]
- Nankinga, O.; Kwagala, B.; Walakira, E. Maternal Employment and Child Nutritional Status in Uganda. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6922416/ (accessed on 11 August 2020).
- Nshimyiryo, A.; Hedt-Gauthier, B.; Mutaganzwa, C.; Kirk, C.M.; Beck, K.; Ndayisaba, A.; Mubiligi, J.; Kateera, F.; El-Khatib, Z. Risk factors for stunting among children under five years: A cross-sectional population-based study in Rwanda using the 2015 Demographic and Health Survey. BMC Public Health 2019, 19, 175. [Google Scholar] [CrossRef] [PubMed]
- Mishra, V.; Retherford, R.D. Does biofuel smoke contribute to anaemia and stunting in early childhood? Int. J. Epidemiol. 2007, 36, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Yaya, S.; Uthman, O.A.; Amouzou, A.; Bishwajit, G. Mass media exposure and its impact on malaria prevention behaviour among adult women in sub-Saharan Africa: Results from malaria indicator surveys. Glob. Health Res. Policy 2018, 3, 20. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Fund UNICEF’s Approach to Scaling up Nutrition for Mothers and their Children; Discussion Paper; Programme Division; UNICEF: New York, NY, USA, 2015.
- National Population Commission (NPC); ICF International. Nigeria Demographic and Health Survey 2018; NPC: Abuja, Nigeria; ICF International: Rockville, MD, USA, 2019.
- Hien, N.N.; Kam, S. Nutritional status and the characteristics related to malnutrition in children under five years of age in Nghean, Vietnam. J. Prev. Med. Public Health 2008, 41, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Seetharaman, N.; Chacko, T.V.; Shankar, S.L.R.; Mathew, A.C. Measuring malnutrition -The role of Z scores and the composite index of anthropometric failure (CIAF). Indian J. Community Med. 2007, 32, 35. [Google Scholar] [CrossRef]
- Lehman, S. The Different Types of Malnutrition and Your Health: Overnutrition and Undernutrition of Nutrient. Available online: https://www.verywellfit.com/understanding-malnutrition-2507055 (accessed on 19 August 2020).
- Nandy, S.; Jaime Miranda, J. Overlooking undernutrition? Using a composite index of anthropometric failure to assess how underweight misses and misleads the assessment of undernutrition in young children. Soc. Sci. Med. 2008, 66, 1963–1966. [Google Scholar] [CrossRef]
- Bamiwuye, S.O.; Wet, N.D.; Adedini, S.A. Linkages between autonomy, poverty and contraceptive use in two sub-Saharan African countries. Afr. Popul. Stud. 2013, 27, 164–173. [Google Scholar] [CrossRef]
- Sakwe, N.; Bigoga, J.; Ngondi, J.; Njeambosay, B.; Esemu, L.; Kouambeng, C.; Nyonglema, P.; Seumen, C.; Gouado, I.; Oben, J. Relationship between malaria, anaemia, nutritional and socio-economic status amongst under-ten children, in the North Region of Cameroon: A cross-sectional assessment. PLoS ONE 2019, 14, e0218442. [Google Scholar] [CrossRef]
- Nandy, S.; Daoud, A.; Gordon, D. Examining the changing profile of undernutrition in the context of food price rises and greater inequality. Soc. Sci. Med. 2016, 149, 153–163. [Google Scholar] [CrossRef]
- Gorstein, J.; Sullivan, K.M.; Parvanta, I.; Begin, F. Indicators and Methods for Cross-Sectional Surveys of Vitamin and Mineral Status of Populations; The Micronutrient Initiative: Ottawa, ON, Canada; The Centers for Disease Control and Prevention: Atlanta, GA, USA, 2007; p. 155.
| Criteria | Determinants | Inclusion Criteria | Exclusion Criteria |
|---|---|---|---|
| Population (P) | Children Under five years are those less than five years of age. | The studies included both male and female children less than five years of age and residing in any of the Sub-Saharan Africa (SSA) countries. We also include publications that involved both adults, children above five years and children under five years; the provided data for under five years were reported differently from others. | Studies involving older children, but no separate reporting for data involving under five years were taken |
| Intervention (I) | Risk factors associated with malnutrition classified as child-related variables, parental/care-givers-related variables, household-related socioeconomic status, demographic status and area characteristics. | Studies that focused on predictors or risk factors or determinants of malnutrition among under five or pre-school children in SSA that covered both individual and contextual exposures. | |
| Comparator (C) | These studies involved two mutually exclusive groups: those that are ‘nourished’ and ‘malnourished’ for which we compared the exposures. | However, we included studies which declassified malnutrition status into stunting, wasting, underweight, overweight and nutrition status. | |
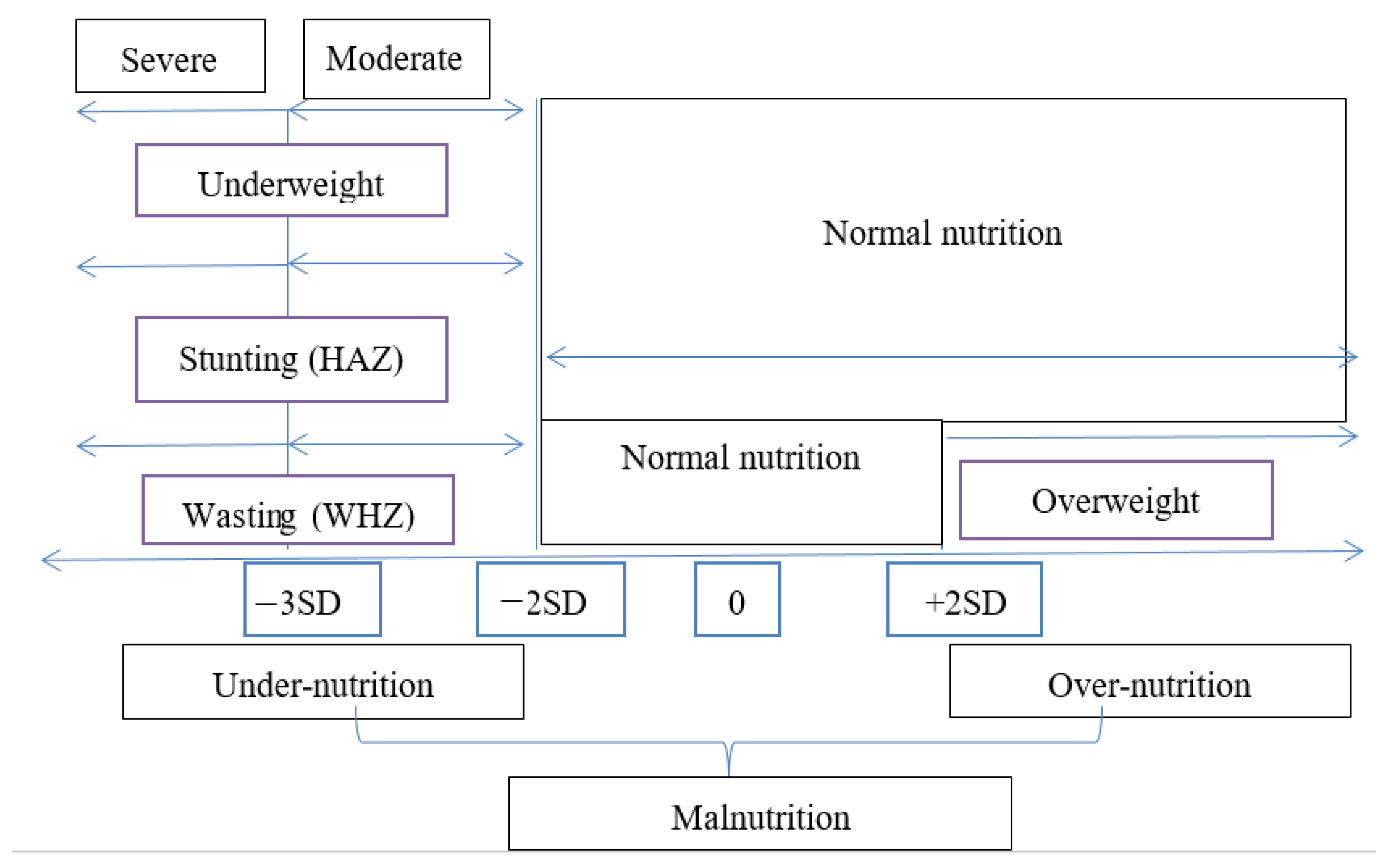
| Outcomes (O) | The main outcome is the malnutrition status (MNS) of children under five years. The MNS is determined through the measurement of anthropometric indices expressed as either stunting (assessed through height-for-age), wasting (assessed through weight-for-height) underweight (assessed through weight-for-age) each with Z-score ≤ −2SD from the median of the reference population, and overweight (estimated via weight-for-height) with Z-score > +2SD from the median of the reference population. | Studies that used any of the indicators or composite index of stunting, wasting, underweight and/or overweight, were onsidered for inclusion, as well as studies that used severity level (such as acute, mild etc.) for the indicators to classify malnutrition or nutrition status, and as such only one aspect was chosen (mild, severe or acute). | |
| Timing (T) | The time articles were published. | The publication period for the article is between 1st January 1990 and 30th July 2020 to capture recent publications on the topic from when UNICEF’s conceptual framework of causes of malnutrition was in effect, the MDG and SDGs | All papers published outside the period 1990–2020. |
| Settings/Design (S) | These studies must be a nationally representative health-related survey in one or more of the Sub-Saharan African countries. These include Demographic and Health Survey (DHS), Multiple Indicator and Cluster Survey (MICS), AIDS Indicator Survey (AIDSIS), and any other countries’ specific survey with a national spread. | Observational studies such as cross-sectional studies that focused on risk factors as predictors. The search also included those studies that applied classical regression for the analyses. | Studies that used other methods such as Bayesian or spatial analyses techniques. Papers on nationally representative health surveys not conducted for SSA countries. Community-based, facility-based and non-nationally representative surveys. Systematic review studies. |
| S/N | Terms and Keywords | Results |
|---|---|---|
| 1 | Demographic and health survey OR DHS OR AIDS indicator survey OR malaria Indicator survey OR multiple indicator cluster survey OR health survey OR Nutrition Survey OR MIS OR MICS | 258,604 |
| 2 | Sub-Saharan Africa OR SSA | 37,452 |
| 3 | 1 AND 2 | 1764 |
| 4 | Socioeconomic OR demographic OR contextual OR environmental OR community OR determinants OR risk factor OR predictor | 3,298,141 |
| 5 | Malnutrition OR stunting OR wasting OR underweight OR under-weight OR overweight OR over-weight OR Nutrition Status OR Nutritional | 451,419 |
| 6 | 4 AND 5 | 107,110 |
| 7 | 3 AND 6 | 134 |
| 8 | Limit 7 to human and English language and infant < to one year > OR preschool child < 1 to 6 years > | 40 |
| 9 | Logistic regression OR multilevel regression OR multinomial logistic OR random-effects OR hierarchical OR fixed effects | 55,708 |
| 10 | 8 AND 9 | 12 |
| 11 | Limit to last 30 years (1990 to 2020) | 12 |
| Author and Data | Country | Study Design | Participants (N) and Study Population | Analysis Methods | Software Used |
|---|---|---|---|---|---|
| Adekanmbi et al. (2013) [23] | Nigeria | 2008 Nigeria Demographic and Health Survey (NDHS) | 28,647 0–59 months | Multilevel logistic regression | Stata |
| Acharya et al. (2020) [31] | Multi-countries | Demographic and Health Survey and Global Forest Change dataset | Women 15–49 years (25,285) and 12–59 months (73,941) | Logistic regression methods | Stata |
| Agadjanian et al. (2003) [35] | Angola | 1996 Angola Multiple Indicator Cluster Survey (AMICS) | Number of participants not stated 6–59 months | Multivariate logistic regression | Stata |
| Aheto (2020) [36] | Ghana | 2014 Ghana Demographic and Health Survey (GDHS) | 2716 Under five years | Multivariate Simultaneous quantile regression | R-Package |
| Akombi et al. (2019) [24] | Nigeria | 2003–2013 NDHS | 22,217 0–59 months | Logistic regression | Stata |
| Akombi et al. (2017) [15] | Nigeria | 2013 NDHS | 24,529 0–59 months | Multilevel logistic regression | Stata |
| Amaral et al. (2017) [37] | Uganda | Uganda National Panel Survey (UNPS) | 3427 under-5 years | Binary logistic regression | Stata |
| Amare et al. (2019) [27] | Ethiopia | 2016 Ethiopia Demographic and Health Survey (EDHS) | 9419 under-5 years | Multiple logistic regression | Stata |
| Custodio et al. (2008) [38] | Equatorial Guinea | 2004 nationally survey | 552 Under five years | Multivariate logistic regression | PEPI |
| Doctor & Nkhana-Salimu (2017) [7] | Malawi | 1992–2016 Malawi Demographic and Health Survey (MDHS) | 31,630 Under five years | Logistic regression | Nil |
| Gebru et al. (2019) [28] | Ethiopia | 2016 Ethiopia Demographic and Health Survey (EDHS) | 8855 Under five years | Multilevel logistic regression | Stata |
| Kennedy et al. (2006) [39] Multi-countries | Angola | 2001 Angola Multiple Indicator Cluster Survey (AMICS) | 5116 Under five years | Logistic regression | SPSS |
| Central African Republic | 2000 Multiple Indicator Cluster Survey (CARMICS) | 12,499 Under five years | Logistic regression | SPSS | |
| Senegal | 2000 Multiple Indicator Cluster Survey (SMICS) | 8319 Under five years | Logistic regression | SPSS | |
| Kuche et al. (2020) [29] | Ethiopia | 2016 Sustainable Undernutrition Reduction in Ethiopia (SURE) | 1848 6–23 months | Ordinal logistic/linear regression model | Nil |
| Machisa et al. (2013) [40] | Swaziland | 2008–2007 Swaziland Demographic and Health Survey (SDHS) | 1155 6–36 months | Multinomial logistic regression | Stata |
| Magadi (2011) [32] | multi-countries | 2003–2008 Demographic and Health Survey (DHS) | 55,749 Under five years | Multilevel logistic regression | MlwiN |
| McKenna et al. (2019) [11] | Democratic Republic of Congo | 2013–2014 Democratic Republic of Congo Demographic and Health Survey (CDHS) | 3722 6–59 months | Logistic regression | SPSS |
| Miller et al. (2007) [41] | Botswana | 2000 Botswana Multiple Indicator Cluster Survey (BMICS) | 2723 Under five years | Multilevel logistic regression | MlwiN |
| Nankinga et al. (2019) [42] | Uganda | 2016 Uganda Demographic and Health Survey (UDHS) | 3531 under-5 years | Multivariate logistic regression | Stata |
| Nshimyiryo et al. (2019) [43] | Rwanda | 2014–2015 Rwanda Demographic and Health Survey (RDHS) | 3594 Under five years | Logistic regression | Stata |
| Ntoimo et al. (2014) [25] multi-countries | Cameroon | 2011 Cameroon Demographic and Health Survey (CDHS) | 5053 Under five years | Logistic regression | Nil |
| Nigeria | 2008 Nigeria Demographic and Health Survey (NDHS) | 18,823 Under five years | Logistic regression | Nil | |
| Democratic Republic of Congo (DRC) | 2007 Congo Demographic and Health Survey (CDHS) | 3777 Under five years | Logistic regression | Nil | |
| Ssentongo et al. (2019) | Uganda | 2015–2016 Uganda Demographic and Health Survey (UDHS) | 4765 0–5 years | Logistic regression | Nil |
| Takele et al. (2019) [30] | Ethiopia | 2016 Ethiopia Demographic and Health Survey (EDHS) | 8743 Under five years | Generalized Linear Mixed Model | Nil |
| Tusting et al. (2020) [33] | SSA countries | Demographic and Health Survey (DHS), Malaria Indicator Survey (MIS) and AIDS Indicator Survey (AIDSIS) | 824,694 0–5 years | Conditional logistic regression | Nil |
| Mishra et al. (2007) [44] | Kenya | 2003 Kenya Demographic and Health Survey (KDHS) | 2756 0–4 years | Logistic regression | Nil |
| Ukwuani & Suchindran (2003) [26] | Nigeria | 1990 NDHS | 5331 0–59 months | Ordinal logistic analysis | |
| Yaya et al. (2019) [34] | SSA countries | Demographic and Health Survey (DHS) | 299,065 Under five years | Multinomial and logistic regression | Stata |
| Author and Date | Aim of the Study | Outcome Variables Studied | Prevalence | Predictors Considered in the Study | Significant Risk Factors Identified (Stunting) | Significant Risk Factors Identified (Wasting) | Significant Risk Factors Identified (Underweight) | Significant Risk Factors Identified (Overweight) | Conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Adekambi et al. (2013) [23] | To determine the predictor of childhood stunting | Stunting | 25.6% | Child’s age sex, birth weight, type of birth; mother’s age, education, breastfeeding, immunization, BMI work status, birth interval, household under five size, ethnicity, mother health-seeking, type of family, wealth status; community place of residence, region, poverty rate, illiteracy rate proper sanitation and safe water | (CR): Child’s age, sex, birth weight, type of birth; (PHR): mother’s, education, breastfeeding, BMI, birth interval, mother health-seeking, wealth status; (AR): community region, illiteracy rate. | Nil | Nil | Nil | The study shows the importance of both individual and community-related risk factors in determining childhood stunting in Nigeria |
| Acharya et al. (2020) [31] | To establish the effect of deforestation on the individual- and household-level double burden of malnutrition in 15 SSA countries | Stunting and overweight | 2.7% | Forest cover loss, child’s age, sex, mother’s education level, age, anaemia status, overweight status, household wealth, size, improve water, sanitation, own agriculture, own livestock, place of residence, a distance of cluster to the nearest road (Km) | (CR): child’s age in months, and child’s age square, (PHR): mother’s education, age wealth status, improved sanitation, (AR): forest cover lost | Forest cover lost, mother’s education, age wealth status, improved sanitation, child’s age in months, and child’s age square | |||
| Agadjanian et al. (2003) [35] | To determine if regional or ethnic differences exist in malnutrition levels | Wasting and stunting | Nil | Place of residence, degree of war, region of residence, language spoken at home, age, full immunization for age | (CR): age, sex, immunization status, (PHR): sex of household head, mean of education of adults, ownership of radio, drinking water, language spoken | (PHR): age, mean years of schooling of adults, and language spoken | Nil | Nil | Malnutrition rates are higher than most SSA countries |
| Aheto (2020) [36] | To identify risk factors of under five severe stunting | Wevere stunting | 5.30% | Type of birth, sex, age, had diarrhoea, had a fever, place of delivery, size at birth, number of children, health insurance, currently breastfeeding, wealth status, maternal education | (CR): birth type, age, sex, diarrhoeal, place delivered, birth size, (PHR): maternal age, and education. Numbers of children <5 years in the household, maternal health insurance, wealth status | Nil | Nil | Nil | Use of Simultaneous Quartile Regression (SQR) can benefit in addressing under 5 stunting |
| Akombi et al. (2019) [24] | To examine the trend and determinants of child undernutrition | Undernutrition (Stunting, wasting and underweight) | Child’s age, mother’s age sex of child, mother’s education, father’s education, wealth index, place of residence, region. | (CR): child’s age, Sex of child; (AR): maternal, place of residence, zone. | (CR): child’s age, sex of the child, | (CR): child’s age, sex of the child; (PHR): father’s education, wealth index, | |||
| Akombi et al. (2017) [15] | To determine the associated risk factors of wasting and undernutrition | Wasting and underweight | 18% and 29% | Place of residence, region, wealth index, mother work status, education, father’s education, occupation, marital status, mother’s literacy, source of drinking water, media factors newspaper, radio, television, Mother’s age, age at birth, type, mode and place of delivery, ANC, the timing of postnatal check, breastfeeding, child’s birth order, birth interval, sex, birth size, age, had diarrhoea, had a fever | (CR): child’s birth interval, sex, had a fever (PHR): place of residence, region, education, father’s education, television | (CR): duration breastfeeding, child’s sex, birth size, had diarrhoea, had a fever (PHR): the region, mother’s education, father’s education, current | |||
| Amaral et al. (2017) [37] | to establish that greater staple food concentrations affect stunting and wasting | Stunting and wasting | Stunting (22.2%), wasting (3.1%) | Staple Budget Share, spending, place of residence, mother present, sex household head educated | (PHR): Staple Budget Share, spending, place of residence, mother present; (CR): sex of the child | (PHR): Staple Budget Share, household head educated; (CR): sex of the child | Nil | Nil | Nutritious staple food are strongly associated with higher odds of stunting and wasting |
| Amare et al. (2019) [27] | To establish the determinants of malnutrition among children under age 5 in Ethiopia | Stunting and wasting | Nil | Child’s age, sex. Birth order, birth weight. Mother’s marital status, age at child’s birth, educational status, BMI, working status, maternal stature. Place of residence, region, wealth status, improve drinking water, toilet type, cooking fuel type | (CR): age, sex, birth weight; (PHR): mother above primary education, BMI, stature, household wealth above poorer, type of toilet facilities and cooking fuel | (CR): Child’s age is 2years+, sex, birth weight > average; (PHR): mother’s BMI, wealth status >middle quintile | Nil | Nil | A multi-sectoral and multidimensional approach is needed to curtail malnutrition in Ethiopia |
| Custodio et al. (2008) [38] | To determine the underlying factors affecting the malnutrition status of children in Equatorial Guinea | Stunting | 35.20% | Socioeconomic status or wealth status, household social index, and community endowment index | (CR): child’s age, (PHR): fishing by household, hospital as close at the health facility | Nil | Nil | Nil | An integrated strategy of combating poverty and improving maternal education to solve stunting problem in Equatorial Guinea |
| Doctor and Nkhana-Salimu (2017) [7] | To understand the trend and effect of determinants of child nutrition among Malawian children under five | Stunting and underweight | 32.60% | Place and region of residence, wealth index, source of drinking water, toilet facilities, mother’s education status, age, number of under 5, child’s sex, age, birth-order, size at birth, had diarrhoea, had a fever, had a cough | (PHR): region of residence, wealth index, mother’s education status; (CR): child’s sex, age, size at birth, had diarrhoea; (Others): survey rounds | Nil | (PHR): region of residence, wealth index, mother’s education status (is Secondary+), age (is 20–30 years); (CR): child’s sex, age, size at birth, had diarrhoea, had a fever, (Others) survey round | Nil | Decline experienced in underweight and stunting among children under 5, but remain a serious public health burden in Malawi |
| Gebru et al. (2019) [28] | to identify individual and community-related variables associated with stunting among children in Ethiopia under 5 | Stunting | 38.39% | Child’s age, sex, mother’s BMI, age, education, occupation, marital status, perceived child’s birth size, the child had diarrhoea and/or fever in the last weeks, father’s education, occupation, wealth index, place of delivery, number of children under 5 in the household, antenatal care visits, mother’s age at 1st birth, birth type, birth interval and mass-media exposure. | (CR): Child’s age, sex, perceived child’s birth size, the child had diarrhoea and/or fever in the last weeks, birth type, and birth interval; (PHR): mother’s BMI, education, occupation, marital status, father’s occupation, wealth index, number of children under 5 in the household | Nil | Nil | Nil | That individual and community factors are important determinants of stunting in Ethiopia |
| Kennedy et al. (2006) [39] Multi-countries | To examine the relationship between wealth status and childhood undernutrition | Stunting and underweight | 45.2% and 20.5% | Place of residence, women with formal education household with adequate sanitation, with access to safe water, had diarrhoea, had acute respiratory infection and wealth status | (PHR): wealth status (poorest poor and middle) | Nil | (PHR): wealth status | Nil | Prevalence of undernutrition is similar for the same socio-economic status across the place of residence in developing countries. |
| To examine the relationship between wealth status and childhood undernutrition | Stunting and underweight | 38.9% and 24.3% | Place of residence, women with formal education, household with adequate sanitation, with access to safe water, had diarrhoea, had acute respiratory infection and wealth status | (PHR): wealth status (poorest, and middle) | Nil | (PHR): wealth status (poor and middle) | Nil | Prevalence of undernutrition is similar for the same socio-economic status across the place of residence. | |
| To examine the relationship between wealth status and childhood undernutrition | stunting and underweight | 25.4% and 22.7% | Place of residence, women with formal education, household with adequate sanitation, with access to safe water, had diarrhoea, had acute respiratory infection and wealth status | (PHR): wealth status (poorest and middle) | Nil | (PHR): wealth status (poorest) | Nil | Prevalence of undernutrition is similar for the same socio-economic status across the place of residence. | |
| Kuche et al. (2020) [29] | To examine the impact of sociodemographic, agricultural diversity and women’s employment variables on child’s length-for-age z-score in children 6–23 months in Ethiopia | Length-for-age (Stunting) | Nil | Child’s dietary diversity, age, sex, household wealth, maternal education, women decision-making power, paternal domestic chores, food insecurity, minimum women dietary diversity, animal source food types, fruit and vegetable types, land owned | (CR): child’s dietary diversity, age (months), age squared, sex; (PHR): household wealth, maternal education, fruit and vegetable types, land owned | Nil | Nil | Nil | Household production of fruit and vegetables can improve a child’s length-for-age |
| Machisa et al. (2013) [40] | To establish the association between the use of biomass fuels for household cooking and stunting in children | Stunting | 27.60% | Child’s age, sex, anaemia, birth order, preceding birth interval. Birthweight, recent episode of an acute respiratory infection, diarrhoea and fever; mother’s age, BMI, highest education, iron supplement, anaemia status; household use of biomass fuel, place of residence, region, number of people in the household, wealth index | (CR): child’s age, preceding birth interval, birthweight; (PHR): household wealth index and use of biomass fuel | Nil | Nil | Nil | The study shows that stunting in children needs to be given priority in health intervention |
| Magadi (2011) [32] | To determine the effect of HIV/AIDS-affected household health outcomes on children under five years in SSA | Undernutrition (stunting, wasting underweight) | Nil | Household HIV status, paternal orphan, child’s age sex, multiple births, birth order, birth interval, breastfed, birth size, place of residence, mother’s age, education, single parenting, wealth status, community HIV prevalence, country HIV prevalence, GDP per capital | (CR): child’s age sex, multiple births, birth order, birth interval, breastfed, birth size; (PHR): The place of residence, mother’s age, education, single parenting, wealth status, household HIV status, paternal orphan; (AR): community HIV prevalence, GDP per capital | (CR): breastfed, birth size; (PHR): place of residence, mother’s education, wealth status, country, household HIV status; (AR): community HIV prevalence | (CR): child’s age sex, multiple births, birth order, birth interval, breastfed, birth size; (PHR): place of residence, mother’s age, education, single parenting, wealth status, household HIV status, paternal orphan, GDP per capital | Nil | The study reveals the need for integration of HIV/AIDS improvement toward the management of child nutrition services in vulnerable communities |
| McKenna et al. (2019) [11] | To determine the relationship between women’s decision-making power and stunting/wasting in children under five in DRC | Stunting/wasting | 35.2%/9.2% | Decide over their own income. Husband’s income, own health, large household purchases, visits to family, child’s sex, age, mother’s education, age, birth interval, number of under-5 in HHs, Number people in HHs, province (region), place of residence, wealth status | (CR): child’s sex, age; (PHR): mother’s education, age, wealth status (richest), province (region), place of residence | (CR): child’s, age; (PHR): mother’s education (primary), place of residence, wealth status (richest) | Nil | Nil | Detailed studies with more relevant and contextual variables are needed to accurately determine the effects of women’s decision-making power and undernutrition in children |
| Miller et al. (2007) [41] | To determine if orphan-based health inequalities measured with anthropometric data exist. | Underweight | Nil | Nil | Nil | Nil | (CR): the child being orphan, child’s age; (PHR): number of dependent children, household head education, wealth index | More data and studies are needed to fully understand the processes that the orphan-based health disparities work on | |
| Nankinga et al. (2019) [42] | To determine the association between maternal employment and the nutritional status of children under 5 in Uganda | Nutritional status (stunting, wasting, underweight) | Nil | Residence, region, wealth status, toilet type, source of drinking water, sex of household head, marital status, maternal occupation, mother’s employer, decision-making power, the distance a problem to health services, child’s sex, age, birth weight | (PHR): maternal age is 35–49 years, education level, maternal occupation; (CR): child’s birth weight, dewormed, | (PHR): region, maternal employer, (CR); child’s sex, age, birth weight | (PHR): mother’s education, employer; (CR): child’s birthweight | Nil | Flexible labor participation for women to enable them time to care for the child |
| Nshimyiryo et al. (2019) [43] | To identify risk factors in stunting in Rwanda | Stunting | 38% | Child’s sex, age group, parity, birth weight, had diarrhoea in last two weeks; mother’s height, educational level, took parasite-controlling drugs during pregnancy, number of days of daily intake of iron tablets, breastfed in the first hour after birth and household’s wealth index, size, access to improved water, improved toilet facility, and household place of residence, region altitude | (CR): child’s sex, age group, birth weight; (PHR): mother’s height, educational level, took parasite-controlling drugs during pregnancy, and household’s wealth | Nil | Nil | Nil | Family-related factors are the major determinants of stunting in Rwanda |
| Ntoimo et al. (2014) [25] multi-countries | To determine the relationship between single motherhood and stunting | Stunting | 32.0% | The child died, marital status, maternal education, place of residence, occupation, wealth status, sibling size, prenatal care, breastfeeding, birth interval, BMI, widowhood, other single mothers | Nil | Nil | Nil | Nil | Single motherhood is a challenge to stunting in SSA countries which can be reduced considerably when the families of the single mother are economically empowered |
| To determine the relationship between single motherhood and stunting | Stunting | 41% | The child died, marital status, maternal education, place of residence, occupation, wealth status, sibling size, prenatal care, breastfeeding, birth interval, BMI, widowhood, other single mothers | Nil | Nil | Nil | Nil | ||
| To determine the relationship between single motherhood and stunting | Stunting | 44.50% | The child died, marital status, maternal education, place of residence, occupation, wealth status, sibling size, prenatal care, breastfeeding, birth interval, BMI, widowhood, other single mothers | Nil | Nil | Nil | Nil | ||
| Ssentongo et al. (2019) | To establish the relationship between vitamin A deficiency and deficit in linear and ponderal growth | Stunting, wasting and underweight | 27%, 4% and 7% | Child age, sex, birth order, vitamin A supplementation, deworming, had diarrhea, anaemia level, wealth status, mother educated, father educated, mother working, father working, iodized salt, owns the land for agriculture, owns livestock, place of residence, region | (CR): vitamin A deficiency | Nil | Nil | Nil | VAD is associated with stunting and not with wasting and underweight |
| Takele et al. (2019) [30] | To determine the risk factors associated with child stunting | Stunting | Nil | Child’s sex, age, birth interval, mother’s BMI, household wealth index, source of drinking water, type of toilet facility, breastfed, mother’s education level and region | (CR): child’s sex, age, age and birthweight; (PHR): mother’s BMI, household wealth index, use of internet facility, type of toilet facility, breastfed, mother’s education level and interaction terms, source of drinking water and mother’s BMI | Nil | Nil | Nil | Children whose mothers are uneducated are at higher risk of being stunted |
| Tusting et al. (2020) [33] | To establish that improved housing is associated with improved child health in SSA | stunting, wasting and underweight | 30%, 8% and 22% | improved drinking water, improved sanitation, house built with finished materials, improved house, the household head had secondary education+; children mean age, child sex | Finished building materials, improved housing | (PHR): improved housing | (PHR): finished building materials, improved housing | Nil | Poor housing is a predictor of health outcomes related to child survival in SSA |
| Mishra et al. (2007) [44] | To determine the effect of the child being orphaned or fostered, and of HIV-infected parents, on nutrition status | Stunting, wasting and underweight | Nil | The child is orphaned, fostered, HIV+ parents, the mother is HIV– but no spouse, HIV status is unknown, HIV– parents | (PHR): child’s parent HIV status is unknown | (PHR): child whose parent is HIV+ | (CR): child is fostered | Nil | Welfare programs should include children that are orphans, fosters, single mothers, HIV-infected parents |
| Ukwuani and Suchindran (2003) [26] | To establish the relationship between women’s work and child nutritional status (stunting and wasting) | Stunting and wasting | 42.6% and 8.9% | Women economic activity, maternal education, paternal education, occupation, wealth index, type of marriage, religion, duration of breastfeeding, sex of the child, birth order, prenatal care, place of delivery, birth size, food supplement, immunization, had fever, had cough, had diarrhoea, source of drinking water, types of toilet, place of residence, region | (PHR): maternal education, wealth index, religion, age at 1st birth; (CR): duration of breastfeeding, sex of the child, birth order, birth size, immunization, had diarrhoea, place of residence, age | (CR): birth size, vaccination, had a fever, toilet, age of child; (PHR): religion | Nil | Nil | |
| Yaya et al. (2019) [34] | To establish the effect of birth spacing interval on child health outcomes | Stunting, wasting, underweight and overweight | Nil | Inter-pregnancy interval (<24 months, 24–36 months, 37–59 months and ≥60 months) | (PHR): inter-pregnancy interval (<24 months, 24–36 months (ref), 37–59 months and ≥60 months) | (PHR): inter-pregnancy interval (24–36 months (ref), ≥60 months) | (PHR): inter-pregnancy interval (<24 months, 24–36 months (ref), 37–59 months and ≥60 months) | (PHR): inter-pregnancy interval (24–36 months (ref), ≥60 months) | The study stressed the importance of promoting an inter-pregnancy interval of between 24 and 36 months to enhance child health outcomes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Obasohan, P.E.; Walters, S.J.; Jacques, R.; Khatab, K. Risk Factors Associated with Malnutrition among Children Under-Five Years in Sub-Saharan African Countries: A Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 8782. https://doi.org/10.3390/ijerph17238782
Obasohan PE, Walters SJ, Jacques R, Khatab K. Risk Factors Associated with Malnutrition among Children Under-Five Years in Sub-Saharan African Countries: A Scoping Review. International Journal of Environmental Research and Public Health. 2020; 17(23):8782. https://doi.org/10.3390/ijerph17238782
Chicago/Turabian StyleObasohan, Phillips Edomwonyi, Stephen J. Walters, Richard Jacques, and Khaled Khatab. 2020. "Risk Factors Associated with Malnutrition among Children Under-Five Years in Sub-Saharan African Countries: A Scoping Review" International Journal of Environmental Research and Public Health 17, no. 23: 8782. https://doi.org/10.3390/ijerph17238782
APA StyleObasohan, P. E., Walters, S. J., Jacques, R., & Khatab, K. (2020). Risk Factors Associated with Malnutrition among Children Under-Five Years in Sub-Saharan African Countries: A Scoping Review. International Journal of Environmental Research and Public Health, 17(23), 8782. https://doi.org/10.3390/ijerph17238782






