Towards Climate Resilient and Environmentally Sustainable Health Care Facilities
Abstract
:1. Introduction
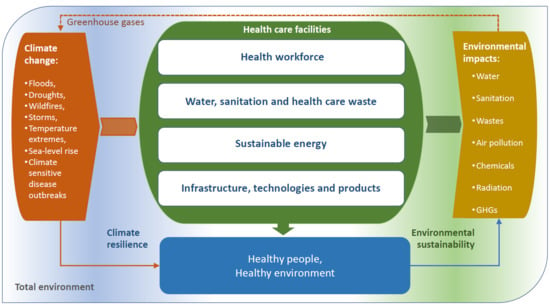
2. Understanding Climate Resilience and Environmental Sustainability of HCFs
2.1. What Do We Understand by Climate Resilience in HCFs?
2.2. What Do We Understand by Environmental Sustainability in HCFs?
3. Strengthening Climate Resilience and Environmental Sustainability
3.1. Risks to Health Care Facilities from Climate Change
3.2. Risks to Environmental Sustainability from Health Care Facility Operations
3.3. The Policy Context
4. A Framework for Action
4.1. Interventions to Strengthen Climate Resilience and Environmental Sustainability in Health Care Facilities
4.2. Area 1: Health Workforce
- Human resources—HCFs having a sufficient number of health workers with healthy and safe working conditions and capacity to deal with health risks from climate change, as well as the awareness and empowerment to ensure environmentally sustainable actions.
- Capacity development—training, information and knowledge management targeted at health care workers to respond to climate risks and minimize environmental threats resulting from the operation of the HCF.
- Communication and awareness raising—communicate, coordinate and increase awareness related to climate resilience and environmental sustainability among health workers, patients, visitors, target communities and with other sectors.
4.3. Interventions for Climate Resilience
4.4. Interventions for Environmental Sustainability
4.5. Area 2: Water, Sanitation and Health Care Waste
- Monitoring and assessment—information regarding water, sanitation, chemical use and health care waste management considers climate resilience and environmental sustainability for promoting action.
- Risk management—strengthened capacity of HCFs to manage water, sanitation, chemicals and health care waste risks to workers, patients and served communities, by including assessments of climate resilience and environmental sustainability in responding to hazards and identifying and reducing exposures and vulnerabilities.
- Health and safety regulation—water, sanitation, chemical safety and health care waste regulations are implemented, taking into consideration climate variability and change, and environmental sustainability.
4.6. Interventions for Climate Resilience
4.7. Interventions for Environmental Sustainability
4.8. Area 3: Energy
- Monitoring and assessment—information regarding energy services should consider climate resilience and environmental sustainability for promoting action.
- Risk management—strengthened capacity of HCFs to manage energy-related risks to workers, patients and served communities, by including assessments of climate resilience and environmental sustainability in responding to hazards and identifying and reducing exposures and vulnerabilities.
- Health and safety regulation—regulations on energy use and access are implemented, taking into consideration climate variability and change, and environmental sustainability.
4.9. Interventions for Climate Resilience
4.10. Interventions for Environmental Sustainability
- Building characteristics: the quality of the building and its features affect the energy demand through the quality of insulation of walls and windows, the use of passive cooling and shading options and its location and exposure to climate and weather.
- Energy efficiency: electric lighting fixtures can consume a large proportion of electrical energy and, depending upon the source, can contribute to internal heat loads. Efficient appliances and thermal insulation also contribute to energy efficiency.
- Transportation: transportation is a major source of both air pollution and GHG emissions, and the health sector—with its fleet of ambulances, hospital vehicles and delivery vehicles, as well as staff and patient travel—is a transportation-intensive industry.
- Food: purchased, prepared and provided in a variety of health care settings contributes to GHG emissions of the health care sector.
- Pharmaceuticals: produced in facilities that use a great deal of energy and emit significant GHGs. While selecting and prescribing medicines, it may be possible to consider those manufactured with the least environmental impact.
4.11. Area 4: Infrastructure, Technology and Products
- Adaptation of current systems and infrastructures—building regulations implemented in the construction and retrofitting of HCFs to ensure climate resilience and environmental sustainability.
- Promotion of new systems and technologies—adopt new technologies and processes that can provide climate resilience, environmental sustainability and enhanced health service delivery.
- Sustainability of health care facility operations—adopt and procure low environmental impact technologies, processes and products to enhance climate resilience and environmental sustainability.
4.12. Interventions for Climate Resilience
4.13. Interventions for Environmental Sustainability
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Operational Framework for Building Climate Resilient Health Systems. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/189951/9789241565073_eng.pdf (accessed on 19 October 2020).
- WHO Regional Office for Europe. The Tallinn Charter: Health Systems for Health and Wealth. 2008. Available online: http://www.euro.who.int/__data/assets/pdf_file/0008/88613/E91438.pdf (accessed on 19 October 2020).
- Kruk, M.E.; Myers, M.; Varpilah, S.T.; Dahn, B.T. What is a resilient health system? Lessons from Ebola. Lancet 2015, 385, 1910–1912. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60755-3/fulltext (accessed on 19 October 2020). [CrossRef]
- Kutzin, J.; Sparkes, S.P. Health systems strengthening, universal health coverage, health security and resilience. Bull. World Health Organ. 2016, 94, 2. Available online: https://www.who.int/bulletin/volumes/94/1/15-165050/en/ (accessed on 19 October 2020). [CrossRef] [PubMed]
- World Health Organization Environmental Health in Emergencies. Health-Care Facilities. Available online: https://www.who.int/environmental_health_emergencies/services/en/ (accessed on 9 October 2020).
- Field, C.B.; Barros, V.R.; Dokken, D.J.; Mach, K.J.; Mastrandrea, M.D.; Bilir, T.E.; Pachauri, R.K.; Allen, M.R.; Broome, J.; Cramer, W. (Eds.) Summary for policymakers. In Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge and New York; Cambridge University Press: Cambridge, UK, 2014; Available online: https://www.ipcc.ch/site/assets/uploads/2018/02/ar5_wgII_spm_en.pdf (accessed on 19 October 2020).
- Field, C.B.; Barros, V.; Stocker, T.F.; Qin, D.; Dokken, D.J.; Ebi, K.L.; Mastrandrea, M.D.; Mach, K.J.; Plattner, G.-K.; Allen, S.K.; et al. (Eds.) Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change; Cambridge and New York; Cambridge University Press: Cambridge, UK, 2012; Available online: https://www.ipcc.ch/site/assets/uploads/2018/03/SREX_Full_Report-1.pdf (accessed on 19 October 2020).
- World Health Organization. Health Emergency and Disaster Risk Management Framework. 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/326106/9789241516181-eng.pdf (accessed on 19 October 2020).
- Cimellaroa, G.P.; Reinhornb, A.M.; Bruneauc, M. Framework for analytical quantification of disaster resilience. Eng. Struct. 2010, 32, 3639–3649. Available online: https://www.eng.buffalo.edu/~bruneau/Engineering%20Structures%202010%20Cimellaro%20Reinhorn%20Bruneau.pdf (accessed on 19 October 2020). [CrossRef]
- World Health Organization. Environmentally Sustainable Health Systems: A Strategic Document. 2017. Available online: https://www.euro.who.int/__data/assets/pdf_file/0004/341239/ESHS_Revised_WHO_web.pdf (accessed on 19 October 2020).
- World Health Organization. Water and Sanitation for Health Facility Improvement Tool (WASH FIT). A Practical Guide for Improving Quality of Care Through Water, Sanitation and Hygiene in Health Care Facilities. 2017. Available online: https://apps.who.int/iris/bitstream/handle/10665/254910/9789241511698-eng.pdf?sequence=1 (accessed on 19 October 2020).
- Harhay, M.O.; Halpern, S.D.; Harhay, J.S.; Olliaro, P.L. Health care waste management: A neglected and growing public health problem worldwide. Trop Med. Int. Health. 2009, 14, 1414–1417. Available online: https://pubmed.ncbi.nlm.nih.gov/19735368/ (accessed on 19 October 2020). [CrossRef] [PubMed]
- Chartier, Y.; Emmanuel, J.; Pieper, U.; Prüss, A.; Rushbrook, P.; Stringer, R. (Eds.) Safe Management of Wastes from Health-Care Activities, 2nd ed.; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/85349/9789241548564_eng.pdf (accessed on 9 October 2020).
- Guenther, R.; Vernon, W. Global lessons in healthcare. Healthc. Des. Mag. Available online: https://www.healthcaredesignmagazine.com/architecture/global-lessons-healthcare/ (accessed on 19 October 2020).
- World Health Organization. Public Health Impact of Chemicals: Knowns and Unknowns; and Data Addendum for 2016. Available online: https://www.who.int/ipcs/publications/chemicals-public-health-impact/en/ (accessed on 19 October 2020).
- World Health Organization. WHO Chemicals Road Map. Road Map to Enhance Health Sector Engagement in the Strategic Approach to International Chemicals Management towards the 2020 Goal and Beyond. 2017. Available online: https://apps.who.int/iris/bitstream/handle/10665/273137/WHO-FWC-PHE-EPE-17.03-eng.pdf (accessed on 19 October 2020).
- World Health Organization. Ionizing Radiation, Health Effects and Protective Measures. 2016. Available online: https://www.who.int/news-room/fact-sheets/detail/ionizing-radiation-health-effects-and-protective-measures (accessed on 19 October 2020).
- World Health Organization. Ambient Air Pollution: Health Impacts. Available online: https://www.who.int/airpollution/ambient/health-impacts/en/ (accessed on 19 October 2020).
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Capsrick, S.; Chambers, J.; et al. The 2019 report of The Lancet Countdown on health and climate change: Ensuring that the health of a child born today is not defined by a changing climate. Lancet 2019, 394, P1836–P1878. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)32596-6/fulltext (accessed on 19 October 2020). [CrossRef] [Green Version]
- Health Care Without Harm. Healthy Food in Health Care. Available online: https://noharm-uscanada.org/healthyfoodinhealthcare (accessed on 19 October 2020).
- World Health Organization. Chemical Releases Caused by Natural Hazard Events and Disasters: Information for Public Health Authorities. 2018. Available online: https://www.who.int/ipcs/publications/natech/en/ (accessed on 19 October 2020).
- Without Harm and Arup Health Care. Health Care’s Climate Footprint: How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action. Available online: https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (accessed on 19 October 2020).
- Greenhouse Gas Protocol. We Set the Standards to Measure and Manage Emissions. Available online: https://ghgprotocol.org (accessed on 19 October 2020).
- Intergovernmental Panel on Climate Change. 2019 Refinement to the 2006 IPCC Guidelines for National Greenhouse Gas Inventories. Available online: https://www.ipcc-nggip.iges.or.jp/public/2019rf/index.html (accessed on 19 October 2020).
- World Health Organization. WHO Global Strategy on Health, Environment and Climate Change: The Transformation Needed to Improve Lives and Well-Being Sustainably through Healthy Environments. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331959/9789240000377-eng.pdf (accessed on 24 June 2020).
- United Nations. Department of Economic and Social Affairs. Sustainable Development Goals. Available online: https://sustainabledevelopment.un.org/?menu=1300 (accessed on 19 October 2020).
- International Labour Office. Health WISE Action Manual. Work Improvement in Health Services. 2014. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_dialogue/---sector/documents/instructionalmaterial/wcms_237276.pdf (accessed on 19 October 2020).
- World Health Organization. Water, Sanitation and Hygiene in Health Care Facilities: Practical Steps to Achieve Universal Access to Quality Care. 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/311618/9789241515511-eng.pdf (accessed on 19 October 2020).
- World Health Organization. Health Care Waste. Key Facts. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 19 October 2020).
- World Health Organization. Access to Modern Energy Services for Health Facilities in Resource-Constrained Settings A Review of Status, Significance, Challenges and Measurement. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/156847/9789241507646_eng.pdf (accessed on 19 October 2020).
- UN Foundation and SEforALL. Lasting Impact–Sustainable Off-Grid Solar Delivery Models to Power Health and Education. 2019. Available online: https://www.seforall.org/system/files/2019-04/Powering-Health_042019.pdf (accessed on 19 October 2020).
- Burgess, C.; Goodman, J.; Rocky Mountain Institute. Solar Under Storm: Select Best Practices for Resilient Ground-Mount PV Systems with Hurricane Exposure. Boulder. Available online: https://rmi.org/wp-content/uploads/2018/06/Islands_SolarUnderStorm_Report_digitalJune122018.pdf (accessed on 19 October 2020).
- Stout, S.; Lee, N.; Cox, S.; Elsworth, J.; Leish, J. Power Sector Resilience Planning Guidebook. A Self-Guided Reference for Practitioners; Department of Energy’s National Renewable Energy Laboratory and United States Agency for International Development: Washington, DC, USA, 2019. Available online: https://www.nrel.gov/docs/fy19osti/73489.pdf (accessed on 19 October 2020).
- Vezzoli, C.; Ceschin, F.; Osanjo, L.; M’Rithaa, M.K.; Moalosi, R.; Nakazibwe, V.; Diehl, J.C. Distributed/decentralized renewable energy systems. In Designing Sustainable Energy for All. Green Energy and Technology; Springer: Berlin/Heidelberg, Germany, 2018; Available online: https://doi.org/10.1007/978-3-319-70223-0_2 (accessed on 18 November 2020).
- World Health Organization and Pan American Health Organization. Hospital Safety Index: Guide for Evaluators. Second ed. Safe Hospitals Initiative. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/258966/9789241548984-eng.pdf (accessed on 19 October 2020).
- United Nations Office for Disaster Risk Reduction. Structural and Non-Structural Measures. Available online: https://www.undrr.org/terminology/structural-and-non-structural-measures (accessed on 19 October 2020).
- World Health Organization. Guidance for Climate Resilient and Environmentally Sustainable Health Care Facilities. 2020. Available online: https://www.who.int/publications/i/item/climate-resilient-and-environmentally-sustainable-health-care-facilities (accessed on 19 October 2020).


| SDGs | Targets | HCF Action Areas |
|---|---|---|
| 13. Take urgent action to combat climate change and its impacts | 13.1 Strengthen resilience and adaptive capacity to climate-related hazards and natural disasters in all countries | Health workforce; Infrastructure, technologies and products |
| 13.2 Integrate climate change measures into national policies, strategies and planning | Health workforce; Infrastructure, technologies and products | |
| 13.3 Improve education, awareness-raising and human and institutional capacity on climate change mitigation, adaptation, impact reduction and early warning | Health workforce | |
| 12. Ensure sustainable consumption and production patterns | 12.4 By 2020, achieve the environmentally sound management of chemicals and all wastes throughout their life cycle, in accordance with agreed international frameworks, and significantly reduce their release to air, water and soil in order to minimize their adverse impacts on human health and the environment | Water, sanitation and health care waste |
| 12.5 By 2030, substantially reduce waste generation through prevention, reduction, recycling and reuse | Water, sanitation and health care waste | |
| 12.7 Promote public procurement practices that are sustainable, in accordance with national policies and priorities | Infrastructure, technologies and products | |
| 6. Ensure availability and sustainable management of water and sanitation for all | 6.1 By 2030, achieve universal and equitable access to safe and affordable drinking water for all | Water, sanitation and health care waste |
| 6.3 By 2030, improve water quality by reducing pollution, eliminating dumping and minimizing release of hazardous chemicals and materials, halving the proportion of untreated wastewater and substantially increasing recycling and safe reuse globally | Water, sanitation and health care waste | |
| 6.4 By 2030, substantially increase water-use efficiency across all sectors and ensure sustainable withdrawals and supply of freshwater to address water scarcity and substantially reduce the number of people suffering from water scarcity | Water, sanitation and health care waste | |
| 7. Ensure access to affordable, reliable, sustainable and modern energy for all | 7.1 By 2030, ensure universal access to affordable, reliable and modern energy services | Energy |
| 7.2 By 2030, increase substantially the share of renewable energy in the global energy mix | Energy | |
| 7.3 By 2030, double the global rate of improvement in energy efficiency | Energy | |
| 8. Promote sustained, inclusive and sustainable economic growth, full and productive employment and decent work for all | 8.8 Protect labour rights and promote safe and secure working environments for all workers, including migrant workers, in particular women migrants, and those in precarious employment | Health workforce |
| 9. Build resilient infrastructure, promote inclusive and sustainable industrialization and foster innovation | 9.4 By 2030, upgrade infrastructure and retrofit industries to make them sustainable, with increased resource-use efficiency and greater adoption of clean and environmentally sound technologies and industrial processes, with all countries taking action in accordance with their respective capabilities | Infrastructure, technologies and products |
| 3. Ensure healthy lives and promote well-being for all at all ages | 3.8 Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all | Access to health care facilities |
| 3.9 By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination | Water, sanitation and health care waste |
| Objectives | Climate Resilience | Environmental Sustainability | |
|---|---|---|---|
| Health workforce | Human resources | Identify minimum needs in terms of health care workers to ensure the operational sufficiency of every HCF department, in case of climate-related disaster or emergency | Increase human resources available to reduce or eliminate disease burden among vulnerable populations resulting from environmental hazards in HCFs |
| Capacity development | Health workforce receives training and exercises for preparing for, responding to and recovering from extreme weather-related emergencies | Education and training provided to HCF staff and the community on environmental factors that contribute to the burden of disease | |
| Communication and awareness raising | Key messages for target audiences (such as patients, staff, public) drafted in preparation for the most likely extreme weather disaster scenarios | Increase knowledge and communication about the environmental impact of pharmaceuticals and their disposal | |
| Water, sanitation and health care wastes | Monitoring and assessment | Develop climate resilient water safety plans | Implement and monitor a waste reduction program including waste management training for all staff |
| Risk management | WASH climate risk management plan implemented | Wastewater is safely managed through use of on-site treatment or sent to a functioning sewer system | |
| Health and safety regulation | Sanitation technologies designed to be more resistant to climate hazards and able to operate under a range of climate conditions | Harvested rainwater or gray water is safely used to flush toilets, clean outdoor pavement areas and water plants when possible | |
| Energy | Monitoring and assessment | Assess that location of energy backup or renewable energy infrastructure can withstand extreme weather events (such as strong winds, hail, floods) | Assess the HCF to determine how and where energy use can be reduced (or increased in energy poor areas) |
| Risk management | Plan developed for managing intermittent energy supplies or system failure | HCF fossil fuel consumption reduced by use of renewable energy sources, including solar (photovoltaic) power, wind power, hydro power and biofuels | |
| Health and safety regulation | Adequate lighting, communications, refrigeration and sterilization equipment are available during climate-related disasters or emergencies | Developed an energy management plan to measure energy consumption | |
| Infrastructure, technology. Products | Adaptation of current systems and infrastructures | HCFs built or retrofitted to cope with extreme weather events, ensuring their resilience, safety and continuous operation | New (or retrofitted) HCFs designed and constructed based on low-carbon approaches |
| Promotion of new systems and technologies | HCF uses proven smart materials and applications, sensors, low-power electronics, telemedicine and similar health care-appropriate technology | Substitute mercury-containing thermometers and blood pressure-measuring devices for affordable, validated device alternatives | |
| Sustainability of HCF operations | Anticipate the impact of the most likely disaster events on the supply of water, food and energy | Implement a clear environmentally sustainable procurement policy statement or protocol for all types of products, equipment and medical devices used in the HCF |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corvalan, C.; Villalobos Prats, E.; Sena, A.; Campbell-Lendrum, D.; Karliner, J.; Risso, A.; Wilburn, S.; Slotterback, S.; Rathi, M.; Stringer, R.; et al. Towards Climate Resilient and Environmentally Sustainable Health Care Facilities. Int. J. Environ. Res. Public Health 2020, 17, 8849. https://doi.org/10.3390/ijerph17238849
Corvalan C, Villalobos Prats E, Sena A, Campbell-Lendrum D, Karliner J, Risso A, Wilburn S, Slotterback S, Rathi M, Stringer R, et al. Towards Climate Resilient and Environmentally Sustainable Health Care Facilities. International Journal of Environmental Research and Public Health. 2020; 17(23):8849. https://doi.org/10.3390/ijerph17238849
Chicago/Turabian StyleCorvalan, Carlos, Elena Villalobos Prats, Aderita Sena, Diarmid Campbell-Lendrum, Josh Karliner, Antonella Risso, Susan Wilburn, Scott Slotterback, Megha Rathi, Ruth Stringer, and et al. 2020. "Towards Climate Resilient and Environmentally Sustainable Health Care Facilities" International Journal of Environmental Research and Public Health 17, no. 23: 8849. https://doi.org/10.3390/ijerph17238849
APA StyleCorvalan, C., Villalobos Prats, E., Sena, A., Campbell-Lendrum, D., Karliner, J., Risso, A., Wilburn, S., Slotterback, S., Rathi, M., Stringer, R., Berry, P., Edwards, S., Enright, P., Hayter, A., Howard, G., Lapitan, J., Montgomery, M., Prüss-Ustün, A., Varangu, L., & Vinci, S. (2020). Towards Climate Resilient and Environmentally Sustainable Health Care Facilities. International Journal of Environmental Research and Public Health, 17(23), 8849. https://doi.org/10.3390/ijerph17238849