Multimorbidity and Mental Health: The Role of Gender among Disease-Causing Poverty, Rural, Aged Households in China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data and Sample
2.2. Key Variables, Multimorbidity
2.3. Mental Health
2.4. Sociodemographic Variables
2.5. Statistical Analysis
3. Results
3.1. Respondents’ Characteristics
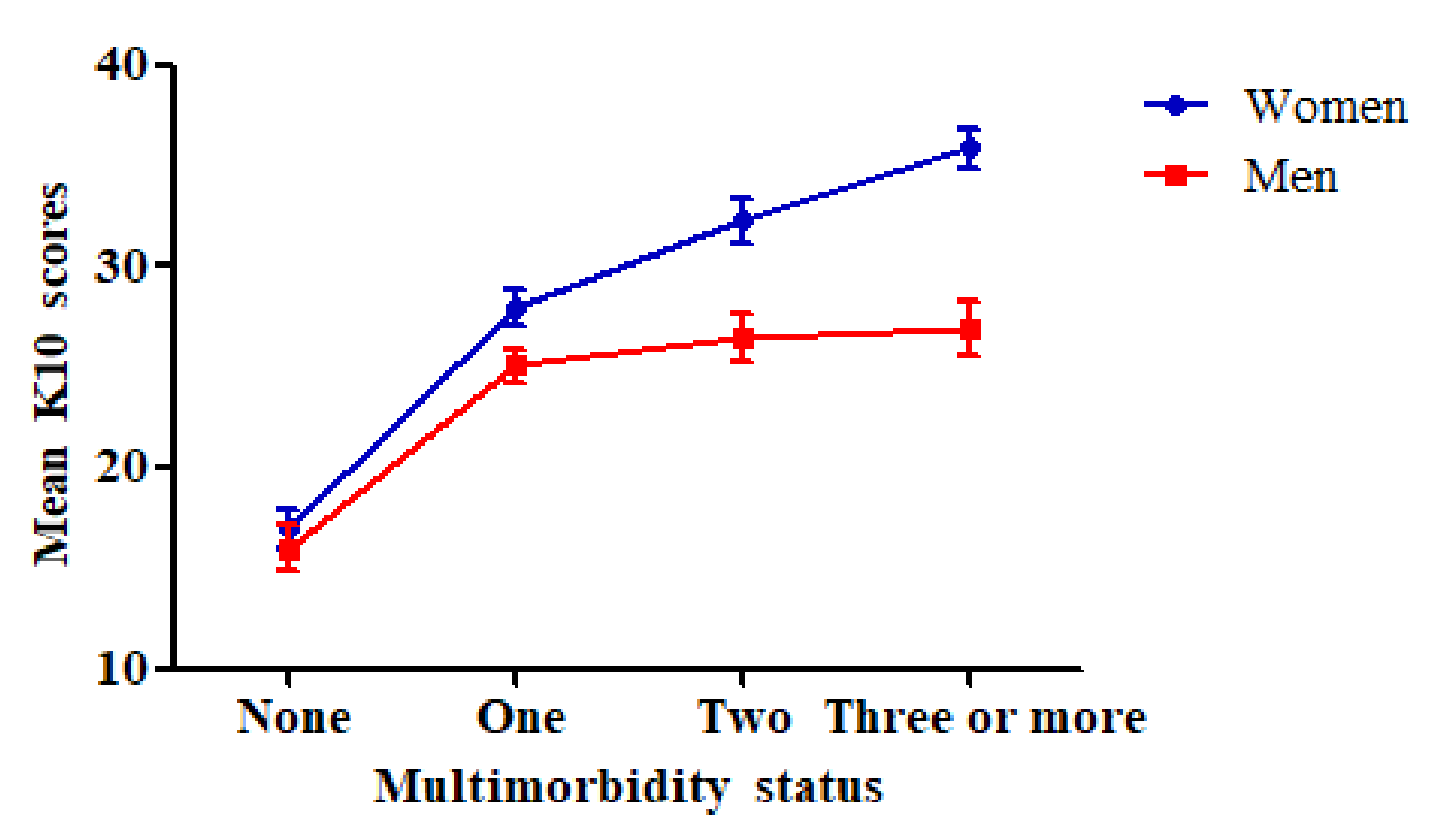
3.2. Comparison of Mental Health between Categories of Multimorbidity Status
3.3. Association between Multimorbidity and Mental Health and Its Gender Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Birk, J.L.; Kronish, I.M.; Moise, N.; Falzon, L.; Yoon, S.; Davidson, K.W. Depression and Multimorbidity: Considering Temporal Characteristics of the Associations Between Depression and Multiple Chronic Diseases. Health Psychol. 2019, 38, 802–811. [Google Scholar] [CrossRef] [PubMed]
- The World Health Report 2008: Primary Health Care Now More than Ever. Available online: https://www.who.int/whr/2008/en/ (accessed on 22 November 2020).
- Hu, X.; Huang, J.; Lv, Y.; Li, G.; Peng, X. Status of prevalence study on multimorbidity of chronic disease in China: Systematic review. Geriatr. Gerontol. Int. 2015, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lancet, T. Making more of multimorbidity: An emerging priority. Lancet 2018, 391, 1637. [Google Scholar] [CrossRef]
- Cui, J.; Mao, F.; Wang, Z.H. Comorbidity of common chronic diseases among the elderly in China. Chin. Public Health 2016, 32, 66–69. [Google Scholar] [CrossRef]
- Nilsen, W.J.; Olster, D.H. News from NIH: Effective behavioral treatments for patients with multiple chronic conditions. Transl. Behav. Med. 2013, 3, 1–2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fortin, M.; Lapointe, L.; Hudon, C.; Vanasse, A. Multimorbidity is common to family practice: Is it commonly researched? Can. Fam. Physician 2005, 51, 244–245. [Google Scholar] [PubMed]
- Romain, A.J.; Marleau, J.; Baillot, A. Association between physical multimorbidity, body mass index and mental health/disorders in a representative sample of people with obesity. J. Epidemiol. Community Health 2019, 73, 874–880. [Google Scholar] [CrossRef]
- Sandison, B. Australian Institute of Health and Welfareÿ. Impact 2017, 10, 78–79. [Google Scholar] [CrossRef]
- Yu, Z.-H. Comparative Study on Mental Health Status of Elderly Hypertensive Patients in Urban and Rural Areas in Shandong Province. Master’s Thesis, Shandong University, Jinan, China, 2019. [Google Scholar]
- Wang, H.X.; Wang, J.J.; Wong, Y.S.; Wong, C.S.; Li, F.J.; Wang, P.X.; Zhou, Z.H.; Zhu, C.Y.; Griffiths, S.M.; Mercer, S.W. Epidemiology of multimorbidity in China and implications for the healthcare system: Cross-sectional survey among 162,464 community household residents in southern China. BMC Med. 2014, 12, 188. [Google Scholar] [CrossRef]
- Ahmadi, B.; Alimohammadian, M.; Yaseri, M.; Majidi, A.; Boreiri, M.; Islami, F.; Poustchi, H.; Derakhshan, M.H.; Feizesani, A.; Pourshams, A. Multimorbidity: Epidemiology and Risk Factors in the Golestan Cohort Study, Iran: A Cross-Sectional Analysis. Medicine 2016, 95, e2756. [Google Scholar] [CrossRef]
- Wells, J.C.K.; Nesse, R.M.; Sear, R.; Johnstone, R.A.; Stearns, S.C. Evolutionary public health: Introducing the concept. Lancet 2017, 309, 500–509. [Google Scholar] [CrossRef]
- Scott, K.M.; Browne, M.A.O.; Mcgee, M.A.; Elisabeth Wells, J. Mental-physical comorbidity in Te Rau Hinengaro: The New Zealand mental health survey. Aust. N. Z. J. Psychiatry 2009, 40, 882–888. [Google Scholar] [CrossRef]
- Moise, N.; Khodneva, Y.; Jannat-Khah, D.P.; Richman, J.; Davidson, K.W.; Kronish, I.M.; Shaffer, J.; Safford, M.M. Observational study of the differential impact of time-varying depressive symptoms on all-cause and cause-specific mortality by health status in community-dwelling adults: The REGARDS study. BMJ Open 2018, 8, e17385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gratzer, D.; Levitan, R.D.; Sheldon, T.; Toneatto, T.; Rector, N.A.; Goering, P. Lifetime rates of alcoholism in adults with anxiety, depression, or co-morbid depression/anxiety: A community survey of Ontario. J. Affect. Disord. 2004, 79, 209–215. [Google Scholar] [CrossRef]
- De Graaf, R.; Bijl, R.V.; Smit, F.; Vollebergh, W.A.M.; Spijker, J. Risk factors for 12-month comorbidity of mood, anxiety, and substance use dirorders: Findings from the Netherlands Mental Health Survey and Incidence Study. Am. J. Psychiatry 2002, 159, 620–629. [Google Scholar] [CrossRef] [PubMed]
- John, U.; Meyer, C.; Rumpf, H.; Hapke, U. Smoking, nicotine dependence and psychiatric comorbidity—A population-based study including smoking cessation after three years. Drug Alcohol Depend. 2004, 76, 287–295. [Google Scholar] [CrossRef]
- Wells, J.E.; Browne, M.A.O.; Scott, K.M. Te Rau Hinengaro: The New Zealand mental health survey: Overview of methods and findings. Aust. N. Z. J. Psychiatry 2006, 40. [Google Scholar] [CrossRef]
- Teesson, M.; Hall, W.; Lynskey, M.; Degenhardt, L. Alcohol- and drug-use disorders in Australia: Implications of the national survey of mental health and wellbeing. Aust. N. Z. J. Psychiatry 2015, 34, 206–213. [Google Scholar] [CrossRef]
- Kessler, R.C.; Chiyu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [Green Version]
- Hasin, D.S.; Stinson, F.S.; Ogburn, E.; Grant, B.F. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Alcohol Abuse and Dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry 2007, 64, 830–842. [Google Scholar] [CrossRef] [Green Version]
- Rijken, M.; Kerkhof, M.V.; Dekker, J.; Schellevis, F.O.G. Comorbidity of chronic diseases. Qual. Life Res. 2005, 14, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-M.; Lee, I.-C.; Su, Y.Y.; Mullan, J.; Chiu, H.-C. The longitudinal relationship between mental health disorders and chronic disease for older adults: A population-based study. Int. J. Geriatr. Psychiatry 2017. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wei, L.; Shan-Ju, H. Research on mental health status of different types of elderly in urban communities based on correspondence analysis. China Health Stat. 2018, 35, 209–211. [Google Scholar]
- Wu, Y. A Study on the Relationship between Socioeconomic Status and the Equity of the Elderly Health Status: An Evidence-Based Study in Suzhou. Master’s Thesis, Suzhou University, Suzhou, China, 2012. [Google Scholar]
- Sheng, L.; Li, L.; Jin, Z. Meta-analysis of the influencing factors of mental health of the Chinese elderly. Chin. J. Gerontol. 2017, 24, 6194–6196. [Google Scholar]
- Niu, T.-H.; Meng, Q.-Y.; Song, T. Cumulative logistic regression analysis of factors affecting the mental health of the elderly in rural areas. Chin. J. Health Psychol. 2009, 11, 1324–1326. [Google Scholar]
- Fitch, C.; Hamilton, S.; Bassett, P.; Davey, R. The relationship between personal debt and mental health: A systematic review. Ment. Health Rev. 2011, 16, 153–166. [Google Scholar] [CrossRef]
- Xu, K.; Evans, D.B.; Kawabata, K.; Zeramdini, R.; Klavus, J.; Murray, C.J.L. Household catastrophic health expenditure: A multicountry analysis. Lancet 2003, 362, 111–117. [Google Scholar] [CrossRef]
- Wang, H.-P.; Wang, Z.-T.; Ma, P.-C. Analysis and Thinking of Poverty Caused by Disease in Rural Areas—Based on Survey Data of 1214 Poor Households Caused by Disease in 9 Provinces and Cities in Western China. Economist 2016, 10, 71–81. [Google Scholar]
- Leng, A.; Jing, J.; Nicholas, S.; Wang, J. Catastrophic health expenditure of cancer patients at the end-of-life: A retrospective observational study in China. BMC Palliat. Care 2019, 18. [Google Scholar] [CrossRef]
- Wang, S.; Ungvari, G.S.; Forester, B.P.; Chiu, H.F.K.; Wu, Y.; Kou, C.; Fu, Y.; Qi, Y.; Liu, Y.; Tao, Y. Gender differences in general mental health, smoking, drinking and chronic diseases in older adults in Jilin province, China. Psychiatry Res. 2017, 251, 58. [Google Scholar] [CrossRef]
- Sunderland, M.; Hobbs, M.J.; Anderson, T.M.; Andrews, G. Psychological distress across the lifespan: Examining age-related item bias in the Kessler 6 Psychological Distress Scale. Int. Psychogeriatr. 2012, 24, 231–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fassaert, T.; Wit, M.A.S.D.; Tuinebreijer, W.C.; Wouters, H.; Verhoeff, A.P.; Beekman, A.T.F.; Dekker, J. Psychometric properties of an interviewer-administered version of the Kessler Psychological Distress scale (K10) among Dutch, Moroccan and Turkish respondents. Int. J. Methods Psychiatr. Res. 2010, 18, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Anderson, T.M.; Sunderland, M.; Andrews, G.; Titov, N.; Dear, B.F.; Sachdev, P.S. The 10-item Kessler psychological distress scale (K10) as a screening instrument in older individuals. Am. J. Geriatr. Psychiatry 2013, 21, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Mcnamara, B.J.; Banks, E.; Gubhaju, L.; Williamson, A.; Joshy, G.; Raphael, B.; Eades, S.J. Measuring psychological distress in older Aboriginal and Torres Strait Islanders Australians: A comparison of the K-10 and K-5. Aust. N. Z. J. Public Health 2014, 38, 567–573. [Google Scholar] [CrossRef] [Green Version]
- Barry, L.C.; Soulos, P.R.; Murphy, T.E.; Kasl, S.V.; Gill, T.M. Association between indicators of disability burden and subsequent depression among older persons. J. Gerontol. 2013, 68, 286–292. [Google Scholar] [CrossRef] [Green Version]
- Dixon-Ibarra, A.; Horner-Johnson, W. Disability status as an antecedent to chronic conditions: National health interview survey, 2006–2012. Prev. Chronic Dis. 2014, 11, 130251. [Google Scholar] [CrossRef] [Green Version]
- Jean, A.; Elaine, S.; Daniel, N.; Milne, E.M.G.; Carol, J. Anticipated survival and health behaviours in older English adults: Cross sectional and longitudinal analysis of the English Longitudinal Study of Ageing. PLoS ONE 2015, 10, e118782. [Google Scholar] [CrossRef]
- Teesson, M.; Mitchell, P.B.; Deady, M.; Memedovic, S.; Slade, T.; Baillie, A. Affective and anxiety disorders and their relationship with chronic physical conditions in Australia: Findings of the 2007 National Survey of Mental Health and Wellbeing. Aust. N. Z. J. Psychiatry 2011. [Google Scholar] [CrossRef]
- Husky, M.M.; Mazure, C.M.; Paliwal, P.; Mckee, S.A. Gender differences in the comorbidity of smoking behavior and major depression. Drug Alcohol Depend. 2008, 93, 176–179. [Google Scholar] [CrossRef] [Green Version]
- Xiang, Y.-T.; Wang, G.; Guo, T.; Hu, C.; Ungvari, G.S.; Kilbourne, A.M.; Lai, Y.C.; Wong, Y.S.; Si, T.-M.; Zheng, Q.-W.; et al. Gender differences in demographic and clinical features and prescribing patterns of psychotropic medications in patients with major depressive disorder in China. Compr. Psychiatry 2013, 54, 1198–1202. [Google Scholar] [CrossRef]
- National Bureau of Statistics. China Statistical Yearbook; China Statistics: Beijing, China, 2013; Volume 32. [Google Scholar]
- Feng-Rong, Z.; Xue, J. Multivariate analysis of factors affecting women’s mental health. J. Fujian Jiangxia Univ. 2013, 4, 74–80. [Google Scholar]
- Molarius, A.; Berglund, K.; Eriksson, C.; Lambe, M.; Nordstrom, E.; Eriksson, H.G.; Feldman, I. Socioeconomic conditions, lifestyle factors, and self-rated health among men and women in Sweden. Eur. J. Public Health 2007, 17, 125–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyd, C.M.; Fortin, M. Future of multimorbidity research: How should understanding of multimorbidity inform health system design? Public Health Rev. 2010, 32, 451–474. [Google Scholar] [CrossRef] [Green Version]
- Xu, Q.-Q. Study on the Relationship between Mental Health and Quality of Life of Female Diabetic Patients in Shandong Province. Master’s Thesis, Shandong University, Jinan, China, 2019. [Google Scholar]
- Xu, A.-Q. Women’s physical and mental health and its influencing factors: A report from Shanghai. Collect. Women’s Stud. 2004, 17–22. [Google Scholar] [CrossRef]
- Wei, C.-Y.; Xu, L.-Z.; Wang, J. Health poverty alleviation policies from the perspective of multidimensional poverty theory: Taking Shandong Province as an example. Shandong Soc. Sci. 2019, 9, 118–127. [Google Scholar]

| Variable | Total (n = 936) | Women (n = 495) | Men (n = 441) | p-Value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age | 0.034 b | |||
| 60–69 | 214 (22.9) | 121 (24.4) | 93 (21.1) | |
| 70–79 | 619 (66.1) | 318 (64.2) | 301 (68.2) | |
| ≥80 | 103 (11.0) | 56 (11.4) | 47 (10.7) | |
| Education attainment | <0.001 b | |||
| None | 334 (35.7) | 221 (44.6) | 116 (26.3) | |
| Primary school | 336 (35.9) | 158 (31.9) | 181 (41.0) | |
| Middle school or above | 266 (28.4) | 116 (23.5) | 144 (32.7) | |
| Marital status | <0.001 b | |||
| Yes | 504 (53.8) | 257 (51.9) | 247 (56) | |
| No | 432 (46.2) | 238 (48.1) | 194 (44) | |
| Work status | <0.001 b | |||
| Yes | 263 (28.1) | 21 (4.2) | 242 (54.9) | |
| No | 673 (71.9) | 474 (95.8) | 199 (45.1) | |
| Medical insurance | 0.042 b | |||
| Yes | 630 (67.3) | 292 (66.2) | 338 (68.3) | |
| No | 306 (32.7) | 149 (33.8) | 157 (31.7) | |
| Multimorbidity | <0.001 b | |||
| None | 48 (5.1) | 23 (4.6) | 25 (5.7) | |
| 1 | 534 (57.1) | 274 (55.4) | 260 (58.9) | |
| 2 | 287 (30.7) | 151 (30.5) | 136 (30.8) | |
| ≥3 | 67 (7.1) | 47 (9.5) | 20 (4.6) | |
| K10, mean ± SD | 25.68 ± 3.24 | 28.13 ± 2.35 | 23.72 ± 2.96 | <0.001 a |
| Variable | None | One Disease | Two Diseases | Three or More Diseases | p-Value a |
|---|---|---|---|---|---|
| Women | |||||
| K10, mean ± SD | 16.92 ± 2.16 | 27.93 ± 1.98 | 32.28 ± 2.56 | 35.85 ± 2.21 | <0.05 |
| Men | |||||
| K10, mean ± SD | 15.98 ± 2.44 | 25.05 ± 1.86 | 26.44 ± 2.82 | 26.96 ± 2.99 | <0.05 |
| Variable | Model I Women | Model II Men | Model III | |||
|---|---|---|---|---|---|---|
| Interaction: Gender × Multimorbidity | ||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age (Reference: ≥80) | ||||||
| 60–69 | 1.853 * | (1.009, 3.403) | 1.379 * | (1.059, 1.795) | 1.541 * | (1.082, 2.191) |
| 70–79 | 1.790 * | (1.299, 2.466) | 1.167 | (0.734, 1.792) | 1.513 * | (1.092, 1.931) |
| Education (Reference: None) | ||||||
| Primary school | 0.772 | (0.581, 1.027) | 0.629 | (0.270, 1.465) | 0.636 | (0.401, 1.009) |
| Middle school or above | 0.687 * | (0.490, 0.962) | 0.419 * | (0.295, 0.596) | 0.577 * | (0.403, 0.828) |
| Marital status (Reference: Single) | ||||||
| Married | 0.562 * | (0.384, 0.823) | 0.421 * | (0.287, 0.598) | 0.504 * | (0.385, 0.660) |
| Work (Reference: None) | ||||||
| Yes | 0.445 | (0.292, 1.067) | 0.293 * | (0.185, 0.463) | 0.304 * | (0.189, 0.489) |
| Medical insurance (Reference: None) | ||||||
| Yes | 0.680 * | (0.478, 0.965) | 0.504 * | (0.385, 0.660) | 0.566 * | (0.381, 0.841) |
| Multimorbidity (Reference: 1) | ||||||
| None | 0.506 * | (0.361, 0.667) | 0.144 * | (0.092, 0.223) | 0.307 * | (0.172, 0.493) |
| 2 | 1.372 * | (1.049, 1.682) | 1.009 | (0.756, 1.787) | 1.242 * | (1.063, 1.782) |
| ≥3 | 1.517 * | (1.196, 1.937) | 1.063 | (0.986, 1.242) | 1.397 * | (1.165, 1.667) |
| Women (Reference: Men) | 1.342 * | (1.034, 1.761) | ||||
| Gender × Multimorbidity | ||||||
| Women × None | 0.771 | (0.356, 1.672) | ||||
| Women × Two diseases | 1.463 * | (1.176, 1.832) | ||||
| Women × Three or more diseases | 1.681 * | (1.402, 2.011) | ||||
| Respondents | 495 | 441 | 936 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiao, C.; Leng, A.; Nicholas, S.; Maitland, E.; Wang, J.; Zhao, Q.; Xu, L.; Gong, C. Multimorbidity and Mental Health: The Role of Gender among Disease-Causing Poverty, Rural, Aged Households in China. Int. J. Environ. Res. Public Health 2020, 17, 8855. https://doi.org/10.3390/ijerph17238855
Jiao C, Leng A, Nicholas S, Maitland E, Wang J, Zhao Q, Xu L, Gong C. Multimorbidity and Mental Health: The Role of Gender among Disease-Causing Poverty, Rural, Aged Households in China. International Journal of Environmental Research and Public Health. 2020; 17(23):8855. https://doi.org/10.3390/ijerph17238855
Chicago/Turabian StyleJiao, Chen, Anli Leng, Stephen Nicholas, Elizabeth Maitland, Jian Wang, Qinfeng Zhao, Lizheng Xu, and Chaofan Gong. 2020. "Multimorbidity and Mental Health: The Role of Gender among Disease-Causing Poverty, Rural, Aged Households in China" International Journal of Environmental Research and Public Health 17, no. 23: 8855. https://doi.org/10.3390/ijerph17238855
APA StyleJiao, C., Leng, A., Nicholas, S., Maitland, E., Wang, J., Zhao, Q., Xu, L., & Gong, C. (2020). Multimorbidity and Mental Health: The Role of Gender among Disease-Causing Poverty, Rural, Aged Households in China. International Journal of Environmental Research and Public Health, 17(23), 8855. https://doi.org/10.3390/ijerph17238855







