Barriers and Facilitators of Adherence to Nicotine Replacement Therapy: A Systematic Review and Analysis Using the Capability, Opportunity, Motivation, and Behaviour (COM-B) Model
Abstract
:1. Backgrounds
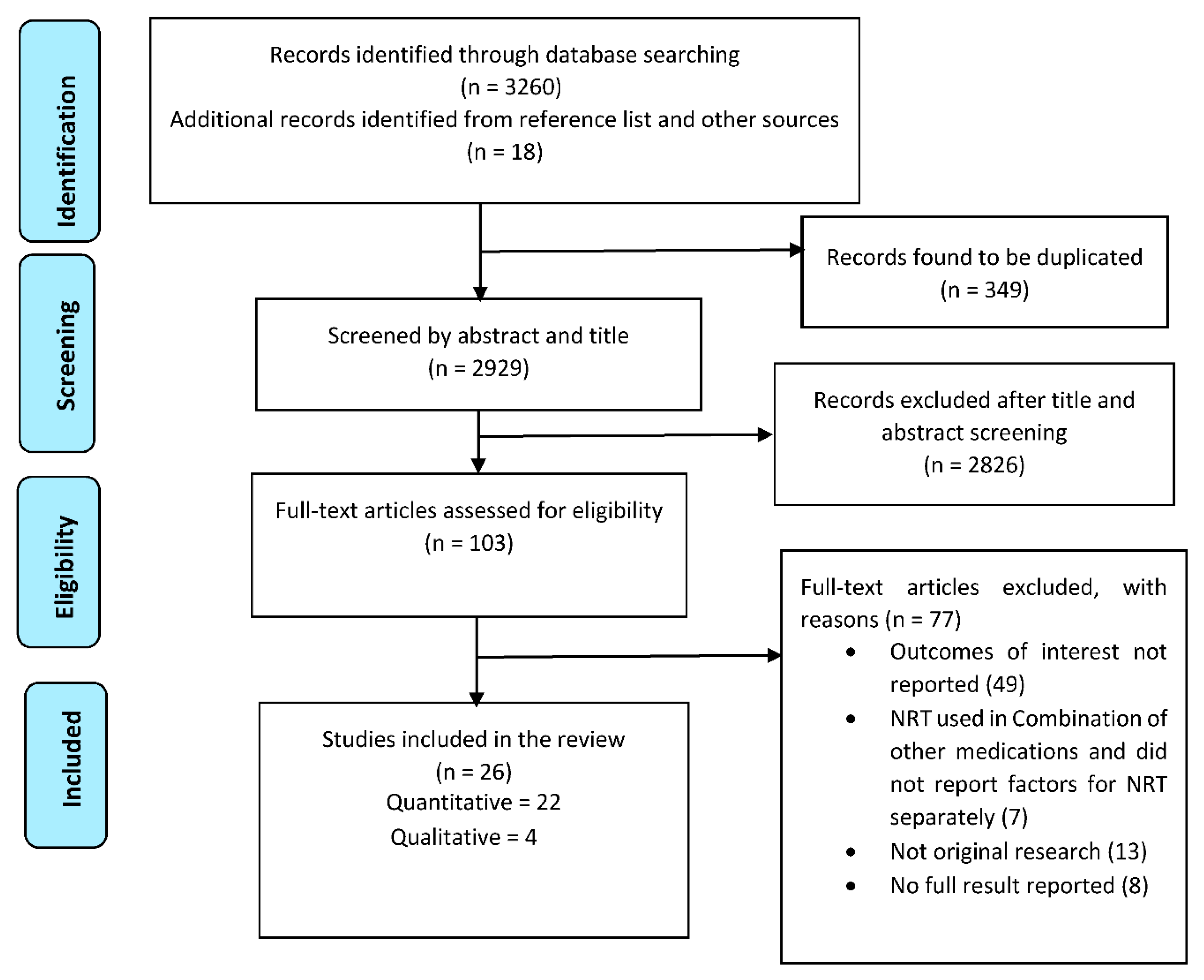
2. Methods
2.1. Selection Criteria
2.2. Literature Searching and Citation Screening
2.3. Keywords
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis
3. Results
3.1. Characteristics of Included Studies
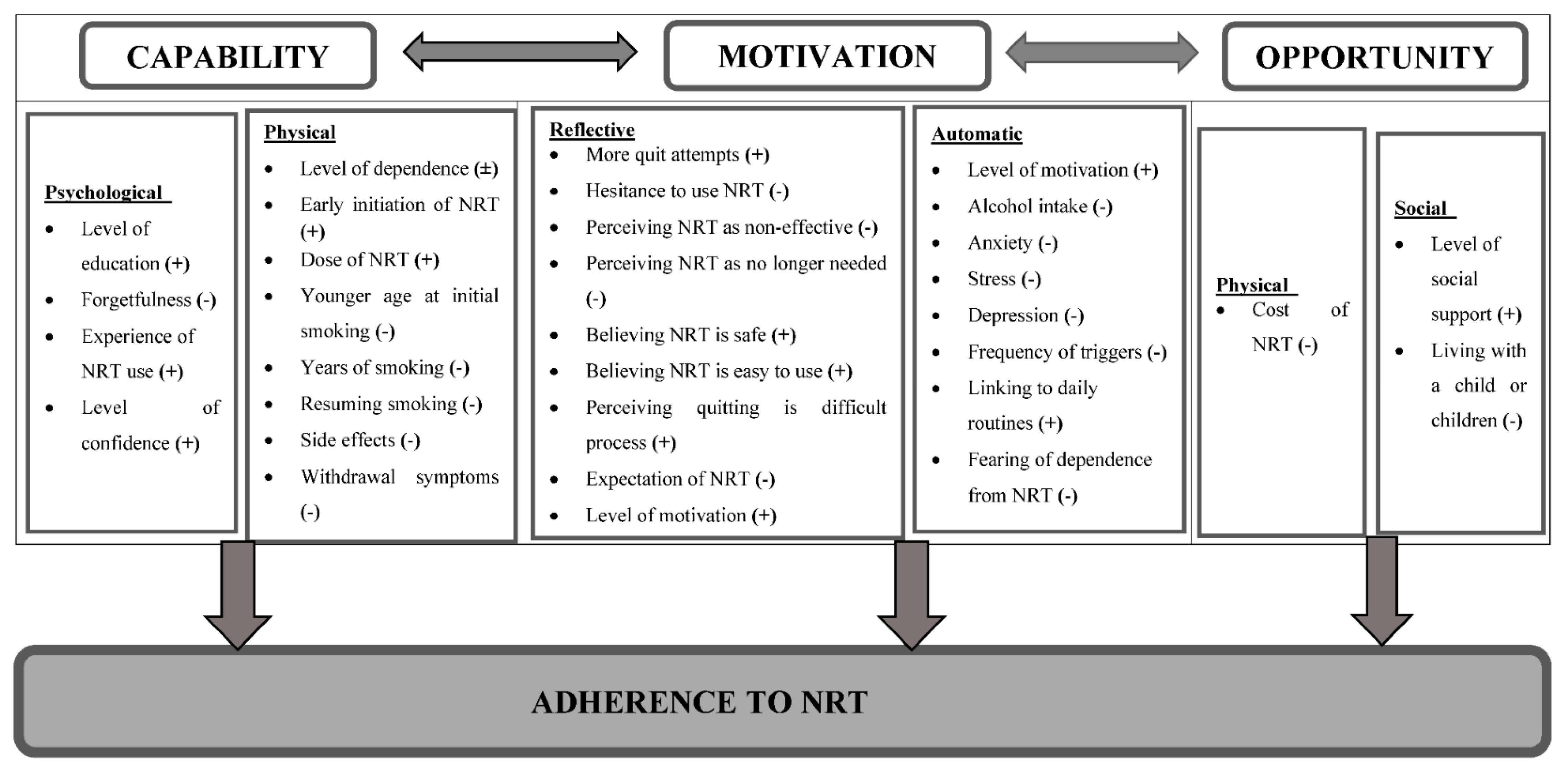
3.2. COM-B Analysis
3.3. Psychological Capability
One of the interviewees said, “I’m currently couch surfing…I try to keep the box of patches [nicotine patches] in my suitcase but sometimes I forget.”[43]
Another participant said, “I put it where, you know, like the deodorant and the perfumes and the colognes are, which is what I do in some of the medications that I take and they’re right here and I’m going to make sure that I put it on. But that’s how I remember things.”[43]
3.4. Physical Capability
One participant said, “Regardless of where I put it…my skin was still itching through the patch, so I’d scratch right on the patch.”[44]
One consumer using oral NRT said, “Yeah, totally delayed cos I keep saying ‘oh I don’t want to taste it yet, I’ll give it another ten minutes you know, or I’ll give it a bit longer’. It is delaying it cos you think I’m not looking forward to the taste of it so I’ll just wait a bit longer.”[45]
A pregnant woman said, “I was just more worried about the side effects obviously because I’m quite early on in pregnancy, and especially with morning sickness anyway, I didn’t know that it [NRT] would cause—obviously [it] made me feel more nauseous and [I] vomited quite a few times when I had the gum. So just would have been nice to have a heads up about it that it makes you feel sick”.[45]
3.5. Motivation
One participant said, “… I know it’s helping me out. I haven’t missed a dose because I’m motivated.”[43]
3.6. Reflective Motivation
One person stated that, “Well, all they keep saying is you know it gets rid of the toxins, you still get the nicotine but it gets rid of the toxins, this, that and the other and it’s just in that the nicotine you take it in. The nicotine itself is what makes it addictive, so to me the more nicotine that you’re taking in any way, the more you’re going to want to smoke or you know you’re going to need that nicotine.”[45]
3.7. Automatic Motivation
A participant said, “It’s a routine. I put it on after I shower in the morning and put the patches next to my medication.”[43]
Another interviewee stated, “I leave it [the patches] next to my medication and remember to take it at the same time each day.”[44]
3.8. Physical Opportunity
3.9. Social Opportunity
4. Discussion
4.1. Strength and Limitations of the Study
4.2. Implications for Policy, Research, and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BCW | Behaviour change wheel |
| COM-B | Capability, opportunity, and motivation model |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| NRT | Nicotine replacement therapy |
References
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef] [Green Version]
- Stoklosa, M.; Drope, J.; Chaloupka, F.J. Prices and e-cigarette demand: Evidence from the European Union. Nicotine Tob. Res. 2016, 18, 1973–1980. [Google Scholar] [CrossRef]
- Chaloupka, F.J.; Yurekli, A.; Fong, G.T. Tobacco taxes as a tobacco control strategy. Tob. Control 2012, 21, 172–180. [Google Scholar] [CrossRef] [Green Version]
- Hopkins, D.P.; Razi, S.; Leeks, K.D.; Kalra, G.P.; Chattopadhyay, S.K.; Soler, R.E.; Task Force on Community Preventive Services. Smokefree policies to reduce tobacco use. A systematic review. Am. J. Prev. Med. 2010, 38 (Suppl. S2), S275–S289. [Google Scholar] [CrossRef]
- Lancaster, T.; Stead, L.F. Individual behavioural counselling for smoking cessation. Cochrane Database Syst. Rev. 2017, 3, Cd001292. [Google Scholar] [CrossRef]
- Notley, C.; Gentry, S.; Livingstone-Banks, J.; Bauld, L.; Perera, R.; Hartmann-Boyce, J. Incentives for smoking cessation. Cochrane Database Syst. Rev. 2019, 7, Cd004307. [Google Scholar] [CrossRef] [PubMed]
- West, R. Tobacco smoking: Health impact, prevalence, correlates and interventions. Psychol. Health 2017, 32, 1018–1036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, T.H.; Abdullah, A.S.; Chan, S.S.C.; Hedley, A.J. Adherence to nicotine replacement therapy versus quitting smoking among Chinese smokers: A preliminary investigation. Psychopharmacology 2005, 177, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Mersha, A.G.; Eftekhari, P.; Bovill, M.; Tollosa, D.N.; Gould, G.S. Evaluating level of adherence to nicotine replacement therapy and its impact on smoking cessation: A systematic review and meta-analysis. BMJ Open 2020, 10, e039775. [Google Scholar] [CrossRef]
- Pacek, L.R.; McClernon, F.J.; Bosworth, H.B. Adherence to Pharmacological Smoking Cessation Interventions: A Literature Review and Synthesis of Correlates and Barriers. Nicotine Tob Res. 2018, 20, 1163–1172. [Google Scholar] [CrossRef] [Green Version]
- Solberg, L.I.; Parker, E.; Foldes, S.S. Disparities in tobacco cessation medication orders and fills among special populations. Nicotine Tob. Res. 2010, 12, 144–151. [Google Scholar] [CrossRef]
- Zeng, F.; Chen, C.-I.; Mastey, V.; Zou, K.H.; Harnett, J.; Patel, B.V. Effects of Copayment on Initiation of Smoking Cessation Pharmacotherapy: An Analysis of Varenicline Reversed Claims. Clin. Ther. 2011, 33, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Catz, S.L.; Jack, L.M.; McClure, J.B.; Javitz, H.S.; Deprey, M.; Zbikowski, S.M.; McAfee, T.; Richards, J.E.; Swan, G.E. Adherence to varenicline in the COMPASS smoking cessation intervention trial. Nicotine Tob. Res. 2011, 13, 361–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Browning, K.K.; Wewers, M.E.; Ferketich, A.K.; Diaz, P.; Koletar, S.L.; Reynolds, N.R. Adherence to Tobacco Dependence Treatment Among HIV-Infected Smokers. AIDS Behav. 2016, 20, 608–621. [Google Scholar] [CrossRef] [Green Version]
- Burns, E.K.; Levinson, A.H. Discontinuation of Nicotine Replacement Therapy Among Smoking-Cessation Attempters. Am. J. Prev. Med. 2008, 34, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Okuyemi, K.S.; Zheng, H.; Guo, H.; Ahluwalia, J.S. Predictors of adherence to nicotine gum and counseling among African-American light smokers. J. Gen. Intern. Med. 2010, 25, 969–976. [Google Scholar] [CrossRef] [Green Version]
- Hood, N.E.; Ferketich, A.K.; Paskett, E.D.; Wewers, M.E. Treatment adherence in a lay health adviser intervention to treat tobacco dependence. Health Educ. Res. 2013, 28, 72–82. [Google Scholar] [CrossRef] [Green Version]
- Wiggers, L.C.W.; Smets, E.M.A.; Oort, F.J.; De Haes, H.C.J.M.; Storm-Versloot, M.N.; Vermeulen, H.; Legemate, D.; Van Loenen, L.B.M.; Peters, R.J.G. Adherence to nicotine replacement patch therapy in cardiovascular patients. International J. Behav. Med. 2006, 13, 79–88. [Google Scholar] [CrossRef]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [Green Version]
- Michie, S.A.L.; West, R. The Behaviour Change Wheel: A Guide to Developing Interventions; Silverback Publishing: London, UK, 2015; Available online: www.behaviourchangewheel.com (accessed on 1 August 2020).
- Posner, J.; Bye, A.; Dean, K.; Peck, A.W.; Whiteman, P.D. The disposition of bupropion and its metabolites in healthy male volunteers after single and multiple doses. Eur. J. Clin. Pharmacol. 1985, 29, 97–103. [Google Scholar] [CrossRef]
- Faessel, H.; Obach, R.S.; Rollema, H.; Ravva, P.; Williams, K.E.; Burstein, A.H.; Faessel, H.M. A review of the clinical pharmacokinetics and pharmacodynamics of varenicline for smoking cessation. Clin. Pharm. 2010, 49, 799–816. [Google Scholar] [CrossRef] [PubMed]
- Leischow, S.J.; Muramoto, M.L.; Matthews, E.; Floden, L.L.; Grana, R.A. Adolescent Smoking Cessation With Bupropion: The Role of Adherence. Nicotine Tob. Res. 2016, 18, 1202–1205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buchanan, T.S.; Berg, C.J.; Cox, L.S.; Nazir, N.; Benowitz, N.L.; Yu, L.; Yturralde, O.; Jacob, P.; Choi, W.S.; Ahluwalia, J.S.; et al. Adherence to varenicline among African American smokers: An exploratory analysis comparing plasma concentration, pill count, and self-report. Nicotine Tob. Res. 2012, 14, 1083–1091. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; A Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Mersha, A.G.; Gould, G.S.; Bovill, M.; Eftekhari, P. Barriers and Facilitators of Adherence to Nicotine Replacement Therapy: A Systematic Review. 2020. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020186621 (accessed on 29 November 2020).
- Croot, L.; O’Cathain, A.; Sworn, K.; Yardley, L.; Turner, K.; Duncan, E.; Hoddinott, P. Developing interventions to improve health: A systematic mapping review of international practice between 2015 and 2016. Pilot Feasibility Stud. 2019, 5, 127. [Google Scholar] [CrossRef] [PubMed]
- Karampela, M.; Isomursu, M.; Porat, T.; Maramis, C.; Mountford, N.; Giunti, G.; Chouvarda, I.G.; Lehocki, F. The Extent and Coverage of Current Knowledge of Connected Health: Systematic Mapping Study. J. Med. Internet Res. 2019, 21, e14394. [Google Scholar] [CrossRef]
- de Klerk, N.H.; Musk, A.W.; Ambrosini, G.L.; Eccles, J.L.; Hansen, J.; Olsen, N.; Watts, V.L.; Lund, H.G.; Pang, S.C.; Beilby, J.; et al. Vitamin A and cancer prevention II: Comparison of the effects of retinol and beta-carotene. Int. J. Cancer 1998, 75, 362–367. [Google Scholar] [CrossRef]
- The Joanna Briggs Institute Critical Appraisal Tools. Available online: https://joannabriggs.org/ebp/critical_appraisal_tools (accessed on 7 May 2020).
- Alterman, A.I. Nicodermal patch adherence and its correlates. Drug Alcohol Depend. 1999, 53, 159–165. [Google Scholar] [CrossRef]
- Berg, C.J.; Ahluwalia, J.S.; Cropsey, K. Predictors of Adherence to Behavioral Counseling and Medication Among Female Prisoners Enrolled in a Smoking Cessation Trial. J. Correct. Health Care 2013, 19, 236–247. [Google Scholar] [CrossRef]
- Cooper, T.V.; DeBon, M.W.; Stockton, M.; Klesges, R.C.; Steenbergh, T.A. Correlates of adherence with transdermal nicotine. Addict. Behav. 2004, 29, 1565–1578. [Google Scholar] [CrossRef]
- Fish, L.J.; Peterson, B.L.; Brouwer, R.J.N.; Lyna, P.; Oncken, C.A.; Swamy, G.K.; Myers, E.R.; Pletsch, P.K.; Pollak, K.I. Adherence to nicotine replacement therapy among pregnant smokers. Nicotine Tob. Res. 2009, 11, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Handschin, J.; Hitsman, B.; Blazekovic, S.; Veluz-Wilkins, A.; Wileyto, E.P.; Leone, F.T.; Schnoll, R.A. Factors Associated with Adherence to Transdermal Nicotine Patches within a Smoking Cessation Effectiveness Trial. J. Smok. Cessat. 2018, 13, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Hollands, G.J.; Sutton, S.; McDermott, M.S.; Marteau, T.M.; Aveyard, P. Adherence to and consumption of nicotine replacement therapy and the relationship with abstinence within a smoking cessation trial in primary care. Nicotine Tob. Res. 2013, 15, 1537–1544. [Google Scholar] [CrossRef] [PubMed]
- Vaz, L.R.; Aveyard, P.; Cooper, S.; Leonardi-Bee, J.; Coleman, T. The association between treatment adherence to nicotine patches and smoking cessation in pregnancy: A secondary analysis of a randomized controlled trial. Nicotine Tob. Res. 2016, 18, 1952–1959. [Google Scholar] [CrossRef] [Green Version]
- Kushnir, V.; Sproule, B.A.; Cunningham, J.A. Mailed distribution of free nicotine patches without behavioral support: Predictors of use and cessation. Addict. Behav. 2017, 67, 73–78. [Google Scholar] [CrossRef]
- Scherphof, C.S.; Eijnden, R.J.J.M.V.D.; Lugtig, P.; Engels, R.C.M.E.; Vollebergh, W.A.M. Adolescents’ use of nicotine replacement therapy for smoking cessation: Predictors of compliance trajectories. Psychopharmacology 2014, 231, 1743–1752. [Google Scholar] [CrossRef]
- De Dios, M.A.; Stanton, C.A.; Cano, M.Á.; Lloyd-Richardson, E.; Niaura, R. The Influence of Social Support on Smoking Cessation Treatment Adherence Among HIV+ Smokers. Nicotine Tob. Res. 2016, 18, 1126–1133. [Google Scholar] [CrossRef] [Green Version]
- Kim, N.; McCarthy, D.E.; Loh, W.-Y.; Cook, J.W.; Piper, M.E.; Schlam, T.R.; Baker, T.B. Predictors of adherence to nicotine replacement therapy: Machine learning evidence that perceived need predicts medication use. Drug Alcohol Depend. 2019, 205, 107668. [Google Scholar] [CrossRef]
- Balmford, J.; Borland, R.; Hammond, D.; Cummings, K.M. Adherence to and reasons for premature discontinuation from stop-smoking medications: Data from the ITC four-country survey. Nicotine Tob. Res. 2011, 13, 94–102. [Google Scholar] [CrossRef] [Green Version]
- Shadel, W.G.; Galvan, F.H.; Tucker, J.S. Developing a nicotine patch adherence intervention for HIV-positive Latino smokers. Addict. Behav. 2016, 59, 52–57. [Google Scholar] [CrossRef] [Green Version]
- Wright, A.J.; Sutton, S.; Armstrong, D.; Aveyard, P.; Kinmonth, A.L.; Marteau, T.M. Factors influencing the impact of pharmacogenomic prescribing on adherence to nicotine replacement therapy: A qualitative study of participants from a randomized controlled trial. Transl. Behav. Med. 2018, 8, 18–28. [Google Scholar] [PubMed]
- Bowker, K.; Campbell, K.A.; Coleman, T.; Lewis, S.; Naughton, F.; Cooper, S. Understanding pregnant smokers’ adherence to nicotine replacement therapy during a quit attempt: A qualitative study. Nicotine Tob. Res. 2016, 18, 906–912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDaid, L.; Thomson, R.; Emery, J.; Coleman, T.; Cooper, S.; Phillips, L.; Bauld, L.; Naughton, F. Understanding pregnant women’s adherence-related beliefs about Nicotine Replacement Therapy for smoking cessation: A qualitative study. Br. J. Health Psychol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ben Taleb, Z.; Ward, K.D.; Asfar, T.; Bahelah, R.; Maziak, W. Predictors of adherence to pharmacological and behavioral treatment in a cessation trial among smokers in Aleppo, Syria. Drug Alcohol Depend. 2015, 153, 167–172. [Google Scholar] [CrossRef] [Green Version]
- Ojo-Fati, O.; Thomas, J.L.; I Vogel, R.; Ogedegbe, O.; Jean-Louis, G.; Okuyemi, K.S. Predictors of Adherence to Nicotine Replacement Therapy (Nicotine Patch) Among Homeless Persons Enrolled in a Randomized Controlled Trial Targeting Smoking Cessation. J. Fam. Med. 2016, 3, 1079. [Google Scholar]
- Rojewski, A.M.; Fucito, L.M.; Baldassarri, S.; Hyland, A.; Cummings, K.M.; Toll, B.A. Nicotine Replacement Therapy Use Predicts Smoking and Drinking Outcomes among Heavy-Drinking Smokers Calling a Tobacco Quitline. J. Smok. Cessat. 2017, 12, 99–104. [Google Scholar] [CrossRef] [Green Version]
- Shiffman, S.; Ferguson, S.G.; Rohay, J.; Gitchell, J.G. Perceived safety and efficacy of nicotine replacement therapies among US smokers and ex-smokers: Relationship with use and compliance. Addiction 2008, 103, 1371–1378. [Google Scholar] [CrossRef]
- Yingst, J.M.; Veldheer, S.; Hrabovsky, S.; Sciamanna, C.; Foulds, J. Reasons for non-adherence to nicotine patch therapy during the first month of a quit attempt. International J. Clin. Pract. 2015, 69, 883–888. [Google Scholar] [CrossRef]
- Benowitz, N.L.; Hukkanen, J.; Jacob, P., 3rd. Nicotine chemistry, metabolism, kinetics and biomarkers. Handb. Exp. Pharmacol 2009, 29–60. [Google Scholar] [CrossRef] [Green Version]
- Johnson, K.C.; Klesges, L.M.; Somes, G.W.; Coday, M.C.; DeBon, M. Access of Over-the-counter Nicotine Replacement Therapy Products to Minors. Arch. Pediatrics Adolesc. Med. 2004, 158, 212–216. [Google Scholar] [CrossRef] [Green Version]
- Behaviour Change Technique Taxonomy v1 (BCTTv1) Online Training 2014. Available online: https://www.bct-taxonomy.com/ (accessed on 29 July 2020).
- Cropsey, K.L.; Clark, C.B.; Zhang, X.; Hendricks, P.S.; Jardin, B.F.; Lahti, A.C. Race and Medication Adherence Moderate Cessation Outcomes in Criminal Justice Smokers. Am. J. Prev. Med. 2015, 49, 335–344. [Google Scholar] [CrossRef] [Green Version]
- Herbec, A.; Brown, J.; Shahab, L.; West, R.; Raupach, T. Pragmatic randomised trial of a smartphone app (NRT2Quit) to improve effectiveness of nicotine replacement therapy in a quit attempt by improving medication adherence: Results of a prematurely terminated study. Trials 2019, 20, 547. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, C.G.; Madrid, J.; Leventhal, A.M. Tobacco withdrawal symptoms mediate motivation to reinstate smoking during abstinence. J. Abnorm. Psychol. 2015, 124, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Lindson, N.; Chepkin, S.C.; Ye, W.; Fanshawe, T.R.; Bullen, C.; Hartmann-Boyce, J. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 2019, 4, CD013308. [Google Scholar] [CrossRef] [PubMed]
- Cahill, K.; Lindson-Hawley, N.; Thomas, K.H.; Fanshawe, T.R.; Lancaster, T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst. Rev. 2016, 2016, CD006103. [Google Scholar] [CrossRef] [Green Version]
- Schlam, T.R.; Cook, J.W.; Baker, T.B.; Hayes-Birchler, T.; Bolt, D.M.; Smith, S.S.; Fiore, M.C.; Piper, M.E. Can we increase smokers’ adherence to nicotine replacement therapy and does this help them quit? Psychopharmacology 2018, 235, 2065–2075. [Google Scholar] [CrossRef]
- Tucker, J.S.; Shadel, W.G.; Galvan, F.H.; Naranjo, D.; Lopez, C.; Setodji, C.M. Pilot evaluation of a brief intervention to improve nicotine patch adherence among smokers living with HIV/AIDS. Psychol. Addict. Behav. 2017, 31, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Zvolensky, M.J.; Bakhshaie, J.; Sheffer, C.; Perez, A.; Goodwin, R.D. Major depressive disorder and smoking relapse among adults in the United States: A 10-year, prospective investigation. Psychiatry Res. 2015, 226, 73–77. [Google Scholar] [CrossRef] [Green Version]
- Lembke, A.; Johnson, K.; DeBattista, C. Depression and smoking cessation: Does the evidence support psychiatric practice? Neuropsychiatr. Dis. Treat. 2007, 3, 487–493. [Google Scholar]
- Crocq, M.-A. Alcohol, nicotine, caffeine, and mental disorders. Dialogues Clin. Neurosci. 2003, 5, 175–185. [Google Scholar]
- Mitchell, S.H.; de Wit, H.; Zacny, J.P. Effects of varying ethanol dose on cigarette consumption in healthy normal volunteers. Behav. Pharmacol. 1995, 6, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Krall, E.A.; Garvey, A.J.; Garcia, R.I. Smoking relapse after 2 years of abstinence: Findings from the VA Normative Aging Study. Nicotine Tob. Res. 2002, 4, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Fiore, M.C.; Jaén, C.R.; Baker, T.B.; Bailey, W.C.; Benowitz, N.L.; Curry, S.J.; Dorfman, S.F.; Froelicher, E.S.; Goldstein, M. A Clinical Practice Guideline for Treating Tobacco Use and Dependence: 2008 Update; U.S. Department of Health and Human Services, Public Health Service: Rockville, MD, USA, 2008. [Google Scholar]
- Hughes, J.R.; Kalman, D. Do smokers with alcohol problems have more difficulty quitting? Drug Alcohol Depend. 2006, 82, 91–102. [Google Scholar] [CrossRef]
- Mooney, M.E.; Sayre, S.L.; Hokanson, P.S.; Stotts, A.L.; Schmitz, J.M. Adding MEMS feedback to behavioral smoking cessation therapy increases compliance with bupropion: A replication and extension study. Addict. Behav. 2007, 32, 875–880. [Google Scholar] [CrossRef]
- Ong, M.K.; Glantz, S.A. Free nicotine replacement therapy programs vs implementing smoke-free workplaces: A cost-effectiveness comparison. Am. J. Public Health 2005, 95, 969–975. [Google Scholar] [CrossRef]
- Vyavaharkar, M.; Moneyham, L.; Tavakoli, A.; Phillips, K.D.; Murdaugh, C.; Jackson, K.; Meding, G. Social support, coping, and medication adherence among HIV-positive women with depression living in rural areas of the southeastern United States. AIDS Patient Care STDS 2007, 21, 667–680. [Google Scholar] [CrossRef]
- Dalmida, S.G.; Koenig, H.G.; Holstad, M.M.; Wirani, M.M. The Psychological Well-Being of People Living with HIV/AIDS and the Role of Religious Coping and Social Support. Int. J. Psychiatry Med. 2013, 46, 57–83. [Google Scholar] [CrossRef]
| Author, Year of Publication, References | Country of Study | Study Design and Sample Size | Participants | Definition of Adherence | Main Outcomes on Factors Associated with Adherence | Quality |
|---|---|---|---|---|---|---|
| Alterman, 1999 [31] | USA | Cross-sectional, 101 | Males or non-pregnant females between the ages of 18 and 65, who met DSM-IV criteria for nicotine dependence and reported at least one previous failed quit attempt. | Patch adherence was obtained by counting dispensed and used patches by the research technician. | Greater dependence was associated with less patch use, indicating that subjects smoking more cigarettes were less patch adherent. A positive relationship between greater motivation and more patch use was demonstrated. | 62% |
| Balmford, 2010 [42] | Australia, USA, UK, Canada | Cross-sectional, 981 | Adult smokers or recent ex-smokers who reported having made a quit attempt in the previous year and reported using NRT to help them quit. | Completion of a course of treatment was defined as use for 8 weeks, with those who terminated before this cut point considered to have stopped prematurely. | Relapse back to smoking was the most common reason for discontinuation of medication reported by 41.6% of respondents. Side effects (18.3%) and believing that the medication was no longer needed (17.1%) were also commonly reported. | 87% |
| Ben Taleb, 2015 [47] | Syria | RCT, 269 | Adult smokers in the age group of 18 to 65 years old. | Participants were asked whether they had followed treatment instructions to use one patch every day over the past week. Adherence to patch use as responding “yes” to this question during at least 5 of the 6 weeks (>80%). | Participants who smoked a greater number of cigarettes per day at baseline (OR = 0.97; 95% CI = 0.94–0.99) and had higher withdrawal symptoms (OR = 0.97; 95% CI= 0.95–0.98) were less likely to adhere to patch usage. | 92% |
| Berg, 2013 [32] | USA | RCT, 202 | Adult smokers of 18 years of age or above. | Calculated adherence level as the number of patches used (80% adherence as adherent; <80% adherence was considered nonadherent). | Predictors of patch adherence included greater prior smoking levels and more quit attempts in the past. | 69% |
| Bowker, 2016 [45] | UK | Qualitative study, 14 | Pregnant smokers are prescribed with NRT. | Pregnant women not using NRT as it was recommended by the health care provider. | Four main themes were identified: expectations of NRT, the experience of using NRT, safety concerns, and experience of using e-cigarettes. Low NRT adherence is associated with believing the risk of smoking and NRT as comparable. | 80% |
| Burns, 2008 [15] | USA | Cross-sectional, 366 | Currently smoked every day or some days or had quit within 365 days of the interview date, tried to quit within 365 days of the interview, and used NRT in the most recent quit attempt. | NRT usage as prescribed by a health care provider instruction. | Discontinuing NRT factors were resuming smoking (34%), side effects (17%), NRT not helping with quitting (14%), quitting smoking (10%), and cost (5%). | 75% |
| Cooper, 2004 [33] | USA | RCT, 619 | Adults who smoked at least 10 cigarettes per day, had been smoking for at least a year. | Based on patch use during the 6 week treatment period, participants were categorized as fully adherent (used ‘‘all of the patches’’), partially adherent (used ‘‘most or some of the patches’’), or nonadherent (used ‘‘a bit or none of the patches’’). | Not dropping out of the study and intensive treatment (compared to the standard care). | 69% |
| de Dios, 2016 [40] | USA | RCT, 444 | Participants were eligible if they were: (1) seropositive for HIV, (2) 18+ years of age, (3) currently smoking (≥5 cigarettes/d for the past 3 months). | Adherence was measured using retrospective self-reports of NRT patch collected at each follow-up visit. | Greater social support network contact was associated with higher levels of nicotine patch adherence. | 85% |
| Fish, 2009 [34] | USA | RCT, 104 | Pregnant women, GA 13–25 weeks, smoked at least 100 cigarettes in their lifetime, currently smoking five cigarettes per day. | Total days of nicotine patch use per week for the follow-up period. | Using NRT as directed in the first 48 h (OR = 5.4, 95% CI = 2.2–12.9, p = 0.0002) and having made a previous quit attempt (OR = 2.9, 95% CI = 1.1–7.6, p = 0.04) were the strongest predictors of longer NRT use. | 85% |
| Handschin, 2018 [35] | USA | RCT, 440 | 18 years of age or older, report smoking at least 10 cigarettes per day and had to express an interest in quitting smoking. | Adherent (≥80% of daily patch use) and non-adherent participants (<80% of daily patch use. | In a logistic regression model, being female, living with a child or children, and higher self-reported anxiety symptoms were predictive of lower patch adherence. | 85% |
| Hollands, 2013 [36] | UK | RCT, 633 | All participants were prescribed a nicotine patch and oral NRT dose. | The proportion of all NRT prescribed consumed each day, averaged over the 4 week treatment period. | Prescribing higher doses of patch and oral NRT was associated with higher mean daily consumption of NRT. | 77% |
| Hood, 2013 [17] | USA | RCT, 147 | Participants were adult women living in Ohio on NRT for smoking cessation. | Patch adherence was dichotomised into 7 weeks or less versus >7 weeks to distinguish between participants who received close to the recommended 8 weeks of patches from those who did not. | Depressive symptoms and low nicotine dependence were associated with lower patch adherence, while the high poverty-to-income ratio was associated with high responsiveness. | 85% |
| Kim, 2019 [41] | USA | RCT, 623 | Participants needed to be willing to quit smoking in the next 30 days, at least 18 years old, smoking at least 5 cigarettes per day for the previous 6 months. | Daily patch use was coded as binary (0 = used patches 6 or fewer days in the past week and 1 = used patches every day for the past week) and mean daily mini-lozenge use was coded as an ordered categorical variable. | Greater baseline dependence predicting greater medication use. Greater quitting motivation and confidence and believing that smoking cessation medication was safe and easy to use were associated with greater adherence. | 77% |
| Kushnir, 2017 [38] | Canada | RCT, 421 | Adult current daily smokers who had smoked at least 10 cigarettes per day. | The number of nicotine patches used was assessed at an 8 week follow-up (end-of-treatment) survey by asking respondents “how much of the nicotine patches did you use?”, with the response options of “none”, “some”, “all”. | The most common reasons for using only some of the 5 weeks of nicotine patches were delayed initiation, side effects, and discontinuation of use due to stress. Among individuals who have not used any of the nicotine patches, the most common reasons were not being ready to quit, stress, and hesitance to use because of the misperception of nicotine patch effects or side-effects. | 85% |
| Lam, 2004 [8] | China | Cross-sectional, 1051 | Adult current smokers using NRT for smoking cessation. | Self-reported use of NRT daily for at least 4 weeks during the first 3 months. | Higher education, the experience of NRT use, perceiving quitting as more difficult, and willingness to pay were significant predictors of adherence. | 87% |
| McDaid, 2020 [46] | UK | Qualitative study, 18 | Pregnant or recently pregnant women in England and Wales who gave birth within 6 months. | NRT usage as prescribed by a health care provider’s instruction during pregnancy. | NRT adherence was found to be associated with pregnant women’s preference for quitting unassisted, unrealistic expectations, overconfidence, safety concerns, side effects, and capability to use. | 80% |
| Ojo-Fati, 2016 [48] | USA | RCT, 430 | Being currently homeless, smoked at least 5 cigarettes per day, smoked at least 100 cigarettes in a lifetime, and smoked at least one cigarette every day. | Adherence was defined as a total score of zero in a modified Morisky adherence scale at the end of NRT treatment (8 weeks). | After adjusting for confounders, smokers who were depressed at baseline (OR = 0.58, 95% CI, 0.38–0.87, p = 0.01), had lower confidence to quit (OR = 1.10, 95% CI, 1.01–1.19, p = 0.04), were less motivated to adhere (OR = 1.04, 95% CI, 1.00–1.07, p = 0.04), and were less likely to be adherent to NRT. Further, the age of initial smoking was positively associated with adherence status (OR = 0.83, 95% CI, 0.69–0.99, p = 0.04). | 92% |
| Okuyemi,2010 [16] | USA | RCT, 755 | African American light smokers (defined as smoking ≤10 cigarettes/day). | Adherence to gum was defined as using greater than or equal 75% of the total prescribed gum usage during the 8 weeks of treatment with gum. | Having more quit attempts in the past year (OR= 1.04, 95% CI = 1.01 to 1.07), higher baseline exhaled carbon monoxide (OR = 1.22, 95% CI = 1.01 to 1.48), and higher perceived stress (OR = 1.12, 95% CI = 1.03 to 1.22) increased the likelihood of adherence to nicotine gum. | 92% |
| Rojewski, 2016 [49] | USA | Cross-sectional, 843 | 18 years of age and meet hazardous drinking criteria as defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA). | NRT use was assessed by self-report at the 7 month follow-up. Participants were asked to select which category best described their level of medication use: (1) all of it, (2) about half of it, (3) less than half of it, or (4) none of it. NRT use was coded as follows: used all NRT = 1, used some NRT = 2 (collapsed half and less than half together), used none = 3. | Those who used all of the NRT had been smoking for a fewer number of years (22.8 ± 12.8), reported a lower percentage of heavy drinking days at baseline (11.6%), and were more likely to complete the second counselling session (38.4%). | 87% |
| Scherphof, 2014 [39] | The Netherlands | RCT, 265 | Participants were allowed to participate if they were 12 years up to and including 18 years old, they smoked at least seven cigarettes a day, they were motivated to quit smoking. | The number of days participants had used the patches. | Reasons for non-adherence were having the feeling that the patches had no effect (38.0%), forgetfulness (37.4%), experiencing side effects (19.3%), and quitting smoking (10.2%). | 77% |
| Shadel, 2016 [43] | USA | Qualitative study, 35 | At least 18 years of age, Latino, HIV-positive, smoked at least 5 cigarettes per day for at least the last 20 days, and had used the nicotine patch during any past quit attempt. | Consumption of NRT as prescribed by the health care provider. | Consistent use of the nicotine patch was associated with maintaining high motivation for use (i.e., not necessarily motivation to quit, but motivation to continue patch use); linking its use with established daily routines (e.g., with taking other medications, with brushing teeth); and maintaining realistic expectations for patch efficacy (e.g., that users may still experience some level of craving and/or withdrawal). | 80% |
| Shiffman, 2008 [50] | USA | Cross-sectional, 3203 | Adult smokers or ex-smokers who had quit within the last year. | Participants asked about the length of time they used the product and the average number of pieces/patches that they used per day when they were using the product/s. | Adherence was associated with believing stop-smoking products with nicotine are just as harmful as cigarettes, having concerns about the safety of NRT, not believing NRT to be efficacious. | 87% |
| Vaz, 2016 [37] | UK | RCT, 1050 | Pregnant women between 12 to 24 weeks of gestation from 1050 pregnant trial SNAP participants. | At 1 month, participants could report using patches for a maximum of 28 days and at delivery for a maximum of 56 days; adherence was measured with respect to these values. | Adherence during the first month was associated with lower baseline cotinine concentrations. | 92% |
| Wiggers, 2006 [18] | The Netherlands | Cross-sectional, 174 | Adults smoked > 5 cigarettes a day, received free patches, and intensive instructions from nurses. | Using the prescribed patches for 7–8 weeks as prescribed. | Low adherence was associated with not wanting to use the patches at the same time (13%), being allergic to NRT (11%), having doubts about the effectiveness of NRT (9%), fearing becoming dependent to the patches (7%), or the patches falling off (6%). | 75% |
| Wright, 2018 [44] | UK | Qualitative study, 40 | Individuals had to smoke at least 10 cigarettes a day. | Participants were requested to take their NRT as prescribed for 4 weeks after their quit date. | Adherence to NRT is associated with the presence of side effects, forgetfulness, or practical difficulties. | 70% |
| Yingst, 2015 [51] | USA | Follow-up cross-sectional study, 201 | Current daily smokers recruited from the Penn State Hershey Medical Centre and surrounding family medicine outpatient centres. | Adherence to the directed use of the nicotine patch was measured by the number of self-reported days, of 28 days, the patch was worn during the quit attempt in treatment. Participants were considered adherent if the patch was worn all 28 days and non-adherent if the nicotine patch was worn less than 28 days. | Reasons for non-adherence were forgetting to put the patch on (30%), not liking the experienced side effects (15%), resuming smoking (10%), and difficulty affording the cost of the patches (7%). | 87% |
| Study | Psychological Capability | Physical Capability | Reflective Motivation | Automatic Motivation | Physical Opportunity | Social Opportunity |
|---|---|---|---|---|---|---|
| Alterman [31] | ✓ | ✓ | ||||
| Balmford [42] | ✓ | ✓ | ||||
| Ben Taleb [47] | ✓ | |||||
| Berg [32] | ✓ | ✓ | ||||
| Burns [15] | ✓ | ✓ | ✓ | |||
| Cooper [33] | ✓ | |||||
| de Dios [40] | ✓ | |||||
| Fish [34] | ✓ | ✓ | ||||
| Handschin [35] | ✓ | ✓ | ||||
| Hollands [36] | ✓ | |||||
| Hood [17] | ✓ | ✓ | ||||
| Kim [41] | ✓ | ✓ | ✓ | ✓ | ||
| Kushnir [38] | ✓ | ✓ | ✓ | |||
| Lam [8] | ✓ | ✓ | ||||
| McDaid [46] | ✓ | ✓ | ✓ | ✓ | ||
| Ojo-Fati [48] | ✓ | ✓ | ✓ | ✓ | ||
| Okuyemi [16] | ✓ | ✓ | ✓ | |||
| Rojewski [49] | ✓ | |||||
| Scherphof [39] | ✓ | ✓ | ✓ | |||
| Shiffman [50] | ✓ | |||||
| Vaz [37] | ✓ | |||||
| Wiggers [18] | ✓ | ✓ | ✓ | |||
| Yingst et al. [51] | ✓ | ✓ | ✓ | ✓ | ||
| Bowker [45] | ✓ | ✓ | ✓ | |||
| Shadel [43] | ✓ | ✓ | ||||
| Wright [44] | ✓ | ✓ | ✓ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mersha, A.G.; Gould, G.S.; Bovill, M.; Eftekhari, P. Barriers and Facilitators of Adherence to Nicotine Replacement Therapy: A Systematic Review and Analysis Using the Capability, Opportunity, Motivation, and Behaviour (COM-B) Model. Int. J. Environ. Res. Public Health 2020, 17, 8895. https://doi.org/10.3390/ijerph17238895
Mersha AG, Gould GS, Bovill M, Eftekhari P. Barriers and Facilitators of Adherence to Nicotine Replacement Therapy: A Systematic Review and Analysis Using the Capability, Opportunity, Motivation, and Behaviour (COM-B) Model. International Journal of Environmental Research and Public Health. 2020; 17(23):8895. https://doi.org/10.3390/ijerph17238895
Chicago/Turabian StyleMersha, Amanual Getnet, Gillian Sandra Gould, Michelle Bovill, and Parivash Eftekhari. 2020. "Barriers and Facilitators of Adherence to Nicotine Replacement Therapy: A Systematic Review and Analysis Using the Capability, Opportunity, Motivation, and Behaviour (COM-B) Model" International Journal of Environmental Research and Public Health 17, no. 23: 8895. https://doi.org/10.3390/ijerph17238895





