Multimorbidity Patterns of Chronic Diseases among Indonesians: Insights from Indonesian National Health Insurance (INHI) Sample Data
Abstract
:1. Introduction
2. Materials and Methods
3. Results
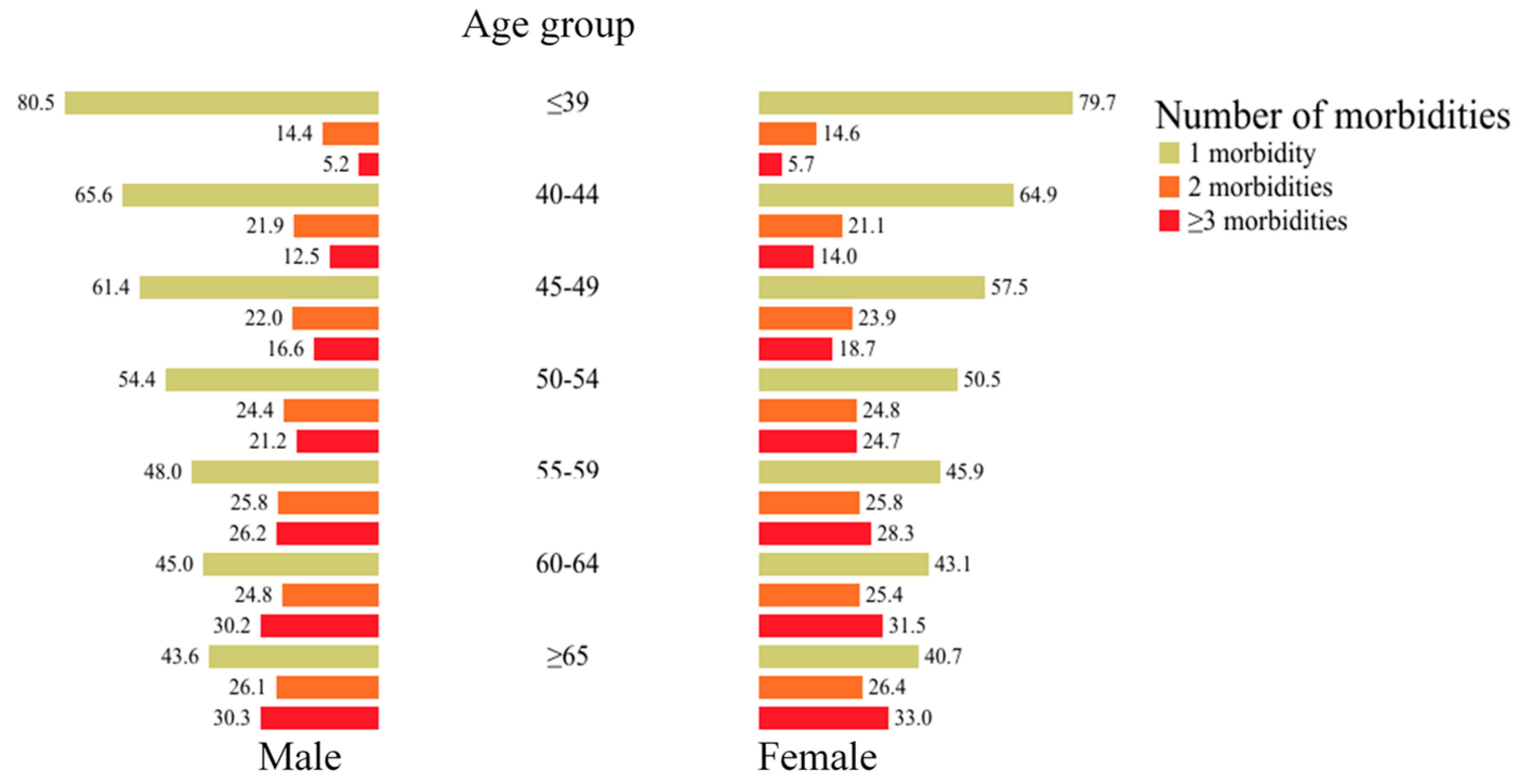
3.1. Proportions and Distributions of Chronic Multimorbidities among Indonesians
3.2. Risk of Having Chronic Multimorbidities among Indonesians
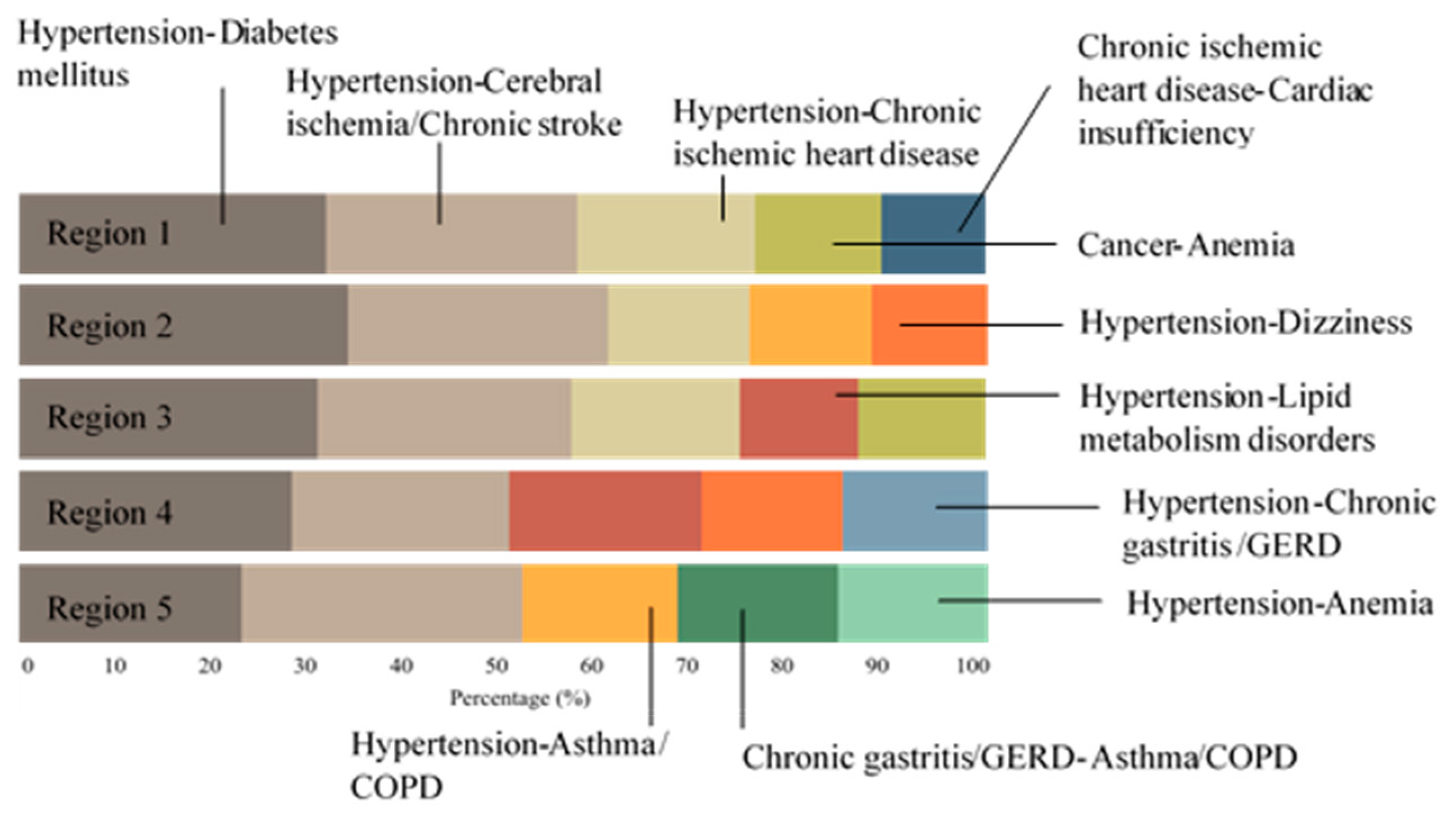
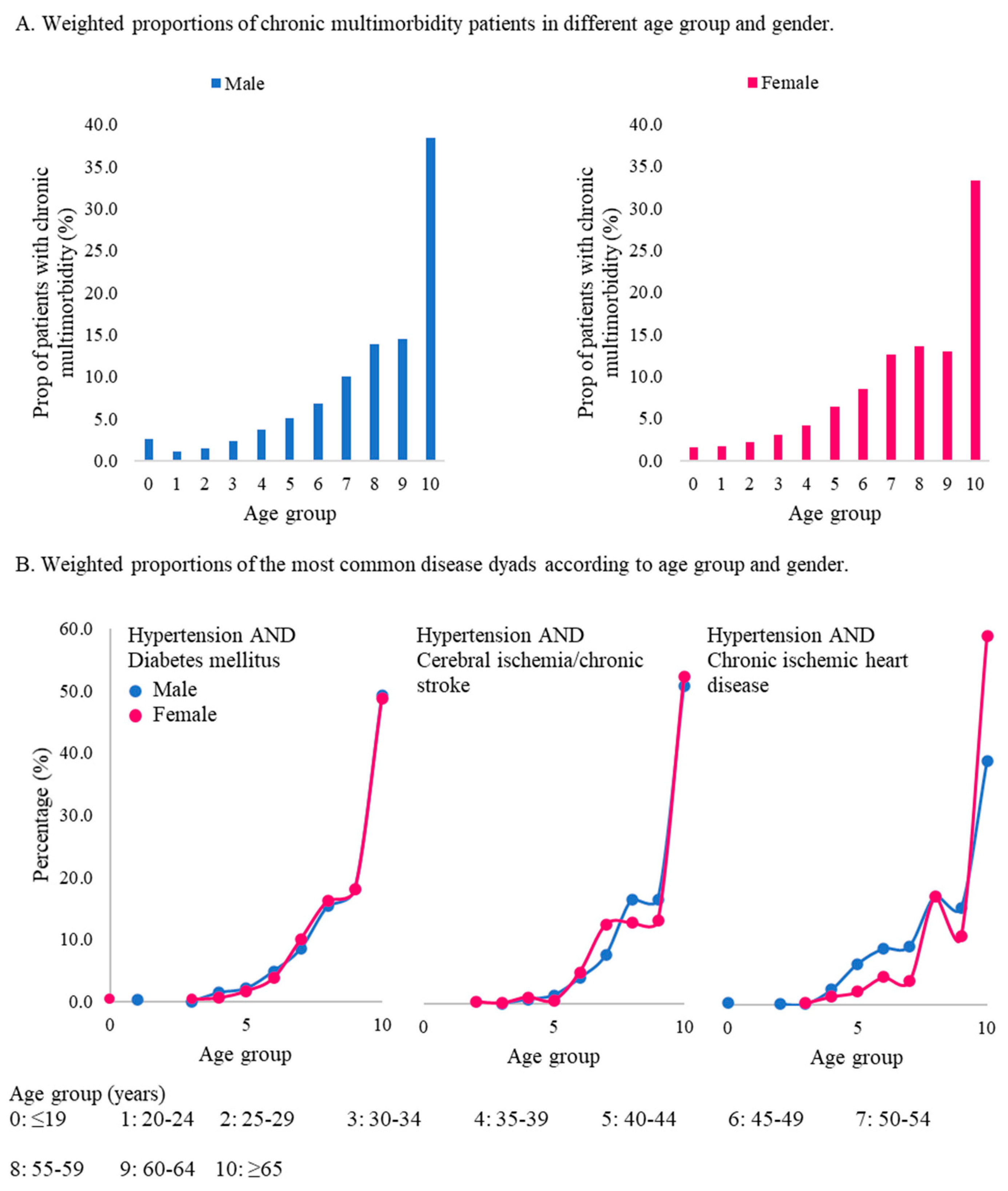
3.3. Common Disease Dyads and Disease Proportions in Different Age Groups and Genders
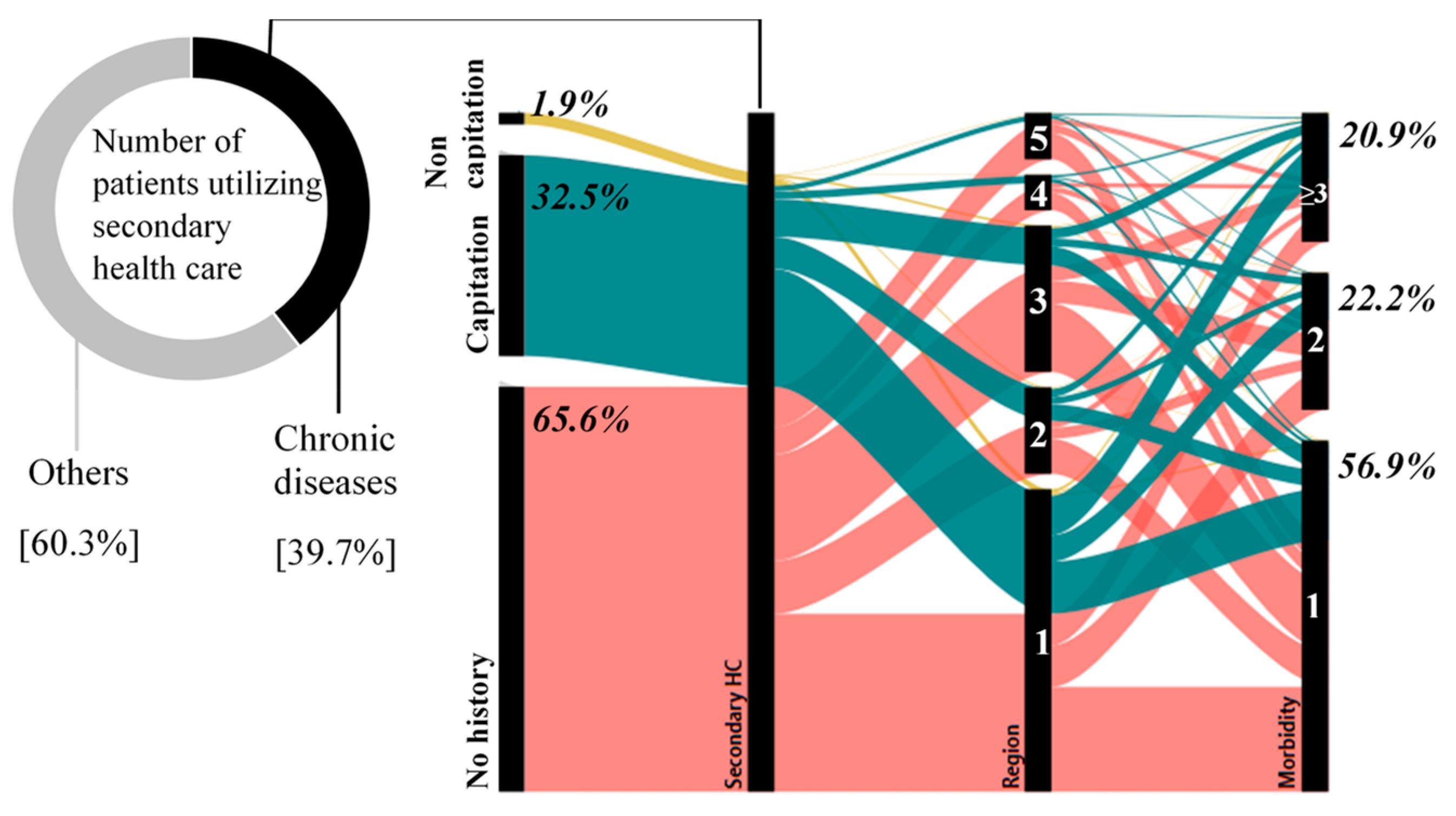
3.4. Patterns of Healthcare Utilization for Chronic Disease Patients
3.5. Potential Use of Claims Data for Chronic Disease Surveillance, Prevention, and Control Programs in Indonesia
4. Discussion
- Age is the most important variable that corresponds to the risk of having chronic multimorbidities. Numerous studies in Asian countries have also demonstrated an older age as the most common risk of having chronic multimorbidities [2,3,4,5,6,7], including a former study conducted in Indonesia [12]. A high proportion of multimorbidities in elderly groups shown in this study was also found in a previous study in a Chinese population [8]. Therefore, this fact could be a warning since Indonesia is currently undergoing development of demographic aging [9]. In addition, the highest odds occurred in regions 3 and 4 in the age class of 45–49 years, signifying the presence of chronic multimorbidity risks in that younger age group, which was also found in former studies [2,12]. These findings mean that in the next few years, a large burden of chronic multimorbidities will potentially result in massive healthcare needs with heavy cost burdens.
- Without controlling for age, persons who are female, currently married, and non-subsidy recipients were also identified as having higher odds of multimorbidities compared to those in the reference group. This finding differs from previous research in Cambodia, Myanmar, Thailand, Vietnam [4], and Japan [5] that showed higher risks in male groups but resembled former studies in India [3,6], Indonesia [12], and Taiwan [2] that pointed out females as a vulnerable group for chronic multimorbidities. In addition, a higher chance of multimorbidities for married persons was also found in research of an Iranian population [18]. The correlation between the marital status and risk of multimorbidities is not completely understood; however, a previous study explained that this phenomenon might be associated with the presence of social support [3]. The risk might be biased by the large proportion of non-subsidy recipients in datasets, which accounted for more than 70% of records.
- Java island is the densest island for chronic multimorbidities. This finding might be due to the highest coverage of health care being concentrated on Java. Differing from other regions, Java and Bali have lower ratios of primary and secondary healthcare facilities per 10,000 population which indicate a better availability of healthcare facilities [19]. This condition results in extensive case findings only in those five provinces and remaining low proportions in the 29 other provinces. Indeed, healthcare access directly affects healthcare utilization. Therefore, in this analysis, around 49% of chronic patients came from Java island or region 1. In terms of healthcare utilization at the primary level and number of patients with chronic multimorbidities, Java had higher respective proportions at 41.8% and 47.4% compared to non-Java areas (28.8% and 39.0%). This finding resembles a study in India which demonstrated that the highest proportion of multimorbid patients came from states with better access and utilization of healthcare services [6]. Hence, a lower proportion of multimorbidities might not represent the true condition in the population but could be caused by limited access and utilization of healthcare services. This result indicates that in the next few years, as health care coverage increases, the number of chronic patients will potentially increase in all provinces of Indonesia.
- Hypertension was the leading disease that was present in 70% of the most common disease dyads in the five regions. The same hypertension pattern also occurred in other Asian countries, including Cambodia, Myanmar, Thailand, Vietnam [4], India [6], Japan [5], and an earlier study in Indonesia [12]. Similar patterns of comorbidities with hypertension (diabetes mellitus (DM), cerebral ischemia/chronic stroke, and chronic ischemic heart disease) were also present in Bangladesh [7] and Cambodia [4]. However, a previous study in Indonesia [12] illustrated different disease comorbidities including cardiac diseases, hypercholesterolemia, and arthritis. That study mentioned high proportions of hypertension in the female group in both adult (45.8%) and elderly groups (69.8%). That study also showed the proportions of cardiac disease of around 11.1% to 17.8% and low occurrences of DM (3.8%–5.2%) and stroke (0.3%–2.1%) [12]. Percentages of hypertension and cardiac diseases were higher in the elderly female group, while those of stroke and DM were greater in the elderly male group. Although patterns were only presented by disease proportions, it might be difficult to compare to the current analysis, which presents the pattern according to disease dyads.
- Over one-third (34.4%) of chronic disease patients were also recorded utilizing health care at the primary level, both for capitation and non-capitation groups. As a consequence, in order to provide better healthcare services, primary health care should facilitate increasing awareness of multimorbidities [1].
- Access to healthcare services. Better access and utilization of healthcare services might be dominant aspects of multimorbidity studies [6]. In addition, the health system may also affect health-seeking behaviors. Therefore, multimorbidities could be higher in countries that implement universal health coverage (UHC) systems with high levels of healthcare coverage, access, and utilization.
- The number of diseases used for the analysis. Various lists of diseases selected to assess multimorbidities may cause different magnitudes of multimorbidities [2]. Previous studies in Asian countries used five to 22 types of chronic diseases [2,3,4,5,6,7,12]. To obtain better representativeness of multimorbidities, this research used 46 chronic diseases. However, a larger scope of diseases might have expanded the analysis.
- Rate of demographic aging. According to research in Taiwan [2], the rate of demographic aging may also affect the magnitude of multimorbidities. Therefore, multimorbidity rates might be higher in countries with high rates of demographic aging.
- Data source utilized for the analysis. Survey data obtained through a self-reported method [3,4,6,7,12] are the most common data source for chronic multimorbidity studies. Besides that, there are a few studies that utilized claims data [2,5] and surveillance data [17]. Accordingly, different data sources with diverse data collection methods could affect rates of multimorbidities at a certain level.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Vetrano, D.L.; Calderon-Larranaga, A.; Marengoni, A.; Onder, G.; Bauer, J.M.; Cesari, M.; Ferrucci, L.; Fratiglioni, L. An International Perspective on Chronic Multimorbidity: Approaching the Elephant in the Room. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 1350–1356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, R.H.; Hsiao, F.Y.; Chen, L.J.; Huang, P.T.; Hsu, W.W. Increasing Age- and Gender-Specific Burden and Complexity of Multimorbidity in Taiwan, 2003–2013: A Cross-Sectional Study Based on Nationwide Claims Data. BMJ Open 2019, 9, e028333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, P.K.; Singh, L.; Dubey, R.; Singh, S.; Mehrotra, R. Socioeconomic Determinants of Chronic Health Diseases Among Older Indian Adults: A Nationally Representative Cross-Sectional Multilevel Study. BMJ Open 2019, 9, e028426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pengpid, S.; Peltzer, K. Multimorbidity in Chronic Conditions: Public Primary Care Patients in Four Greater Mekong Countries. Int. J. Environ. Res. Public Health 2017, 14, 1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitsutake, S.; Ishizaki, T.; Teramoto, C.; Shimizu, S.; Ito, H. Pattern of Co-occurance of Chronic Disease Among Older Adults in Tokyo, Japan. Prev. Chronic Dis. 2019, 16. [Google Scholar] [CrossRef]
- Mini, G.K.; Thankappan, K.R. Pattern, Correlates and Implications of Non-Communicable Disease Multimorbidity Among Older Adults in Selected Indian States: A Cross-Sectional Study. BMJ Open 2017, 7, e013529. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Jehan, I.; de Silva, H.A.; Naheed, A.; Farazdaq, H.; Hirani, S.; Kasturiratne, A.; Ranasinha, C.D.; Islam, M.T.; Siddiquee, A.T.; et al. Prevalence and Correlates of Cardiometabolic Multimorbidity Among Hypertensive Individuals: A Cross-Sectional Study in Rural South Asia-Bangladesh, Pakistan and Sri Lanka. BMJ Open 2019, 9, e030584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, S.-S.; Meng, X.; Cao, G.-Y.; Huang, Z.-T.; Chen, Z.-S.; Wang, K.; Su, H.-X.; Luo, Y.; Hu, Y.; Xu, B. Associations between Multimorbidity and Physical Performance in Older Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 4546. [Google Scholar] [CrossRef] [PubMed]
- Syakriah, A. Indonesia Enters Early Stages of Aging Population. The Jkt. Post. 2019. Available online: https://www.thejakartapost.com/news/2019/10/11/indonesia-enters-early-stages-aging-population.html#:~:text=As%20Indonesia%20enters%20the%20early,citizens%20aged%2060%20and%20above (accessed on 28 August 2020).
- Sitohang, M.Y. The Death of Indonesian National Commission for the Elderly. Available online: http://kependudukan.lipi.go.id/en/population-study/publich-health/625-matinya-komnas-lansia-dan-jalan-lain-meningkatkan-kesejahteraan-lansia-indonesia (accessed on 10 September 2020).
- Schroders, J.; Wall, S.; Hakimi, M.; Dewi, F.S.T.; Weinehall, L.; Nichter, M.; Nilsson, M.; Kusnanto, H.; Rahajeng, E.; Ng, N. How is Indonesia Coping with Its Epidemic of Chronic Noncommunicable Diseases? A Systematic Review with Meta-Analysis. PLoS ONE 2017, 12, e0179186. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.A.; Huxley, R.R.; Al Mamun, A. Multimorbidity Prevalence and Pattern in Indonesian Adults: An Exploratory Study Using National Survey Data. BMJ Open 2015, 5, e009810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larkin, J.; Foley, L.; Susan, M.; Harrington, P.; Clyne, B. The experience of financial burden for patients with multimorbidity: A protocol for a systematic review of qualitative research. Hrb. Open Res. 2020, 2. [Google Scholar] [CrossRef]
- Ariawan, I.; Sartono, B.; Jaya, C.; Mawardi, J.; Sodiq, J.; Baros, W.A.; Hidayat, R.; Panggabean, P.D.; Wahyuningsih, W. Code Book of Indonesian Health Claim Sample Data Set, 2nd ed.; Indonesian Health Insurance Agency: Jakarta, Indonesia, 2019; pp. 1–36. [Google Scholar]
- Koller, D.; Schön, G.; Schäfer, I.; Glaeske, G.; Bussche, H.v.d.; Hansen, H. Multimorbidity and Long-term Care Dependency—A Five-year Follow-up. BMC Geriatr. 2014, 14, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Indonesian Central Bureau of Statistics. Profil Penduduk Indonesia Hasil SUPAS 2015; Indonesian Central Bureau of Statistics: Jakarta, Indonesia, 2015.
- Feely, A.; Lix, L.M.; Reimer, K. Estimating Multimorbidity Prevalence with The Canadian Chronic Disease Surveillance System. Health Promot. Chronic. Dis. Prev. Can. 2017, 37, 215–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alimohammadian, M.; Majidi, A.; Yaseri, M.; Ahmadi, B.; Islami, F.; Derakhshan, M.; Delavari, A.; Amani, M.; Feyz-Sani, A.; Poustchi, H.; et al. Multimorbidity as an important issue among women: Results of a gender difference investigation in a large population-based cross-sectional study in West Asia. BMJ Open 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Misnaniarti, M.; Junadi, P.; Hidayat, B.; Pujiyanto, P.; Purwoko, B.; Nadjib, M.; Thabrany, H.; Yulaswati, V. Ketersediaan Fasilitas dan Tenaga Kesehatan Dalam Mendukung Cakupan Semesta Jaminan Kesehatan Nasional. J. Penelit. Dan Pengemb. Pelayanan Kesehat. 2017, 1. [Google Scholar] [CrossRef]
- Word Health Organization. NCDs STEPwise Approach to Chronic Disease Risk Factor Surveillance. Available online: https://www.who.int/ncds/surveillance/steps/indonesia/en/ (accessed on 10 September 2020).
- RAND Corporation. Indonesian Family Life Survey (IFLS). Available online: https://www.rand.org/well-being/social-and-behavioral-policy/data/FLS/IFLS.html (accessed on 10 September 2020).
- Putri, S.T.; Andriyani, S. Needs and Problems of Posbindu Program: Community Health Volunteers Perspective. In Proceedings of the 2nd Annual Applied Science and Engineering Conference, Bandung, Indonesia, 24 August 2017. [Google Scholar]
- Indonesian Ministry of Health. Distribution of Posbindu. Available online: www.p2ptm.kemkes.go.id/profil-p2ptm/daftar-informasi-publik/peta-jumlah-posbindu-ptm (accessed on 10 September 2020).
- Indonesian Ministry of Health. Prolanis’ Guideline; Indonesian Ministry of Health: Jakarta, Indonesia, 2015.
- Rachmawati, S.; Prihhastuti-Puspitasari, H.; Zairina, E. The Implementation of A Chronic Disease Management Program (Prolanis) in Indonesia: A Literature Review. J. Basic Clin. Physiol. Pharmacol. 2019, 3, 1–6. [Google Scholar] [CrossRef] [PubMed]
- National Health Research Institutes. National Health Insurance Research Databases. Available online: https://nhird.nhri.org.tw/en/Data_Files.html (accessed on 12 October 2020).
| No. | Island | Province | No. of Patients with Chronic Conditions | No. of Patients with Chronic Multimorbidities | Total Population |
|---|---|---|---|---|---|
| 1 | Sumatera | Aceh | 3208 | 1187 | 4,993,385 |
| 2 | North Sumatera | 4538 | 1695 | 13,923,262 | |
| 3 | Riau | 1675 | 706 | 6,330,941 | |
| 4 | West Sumatera | 2708 | 1251 | 5,190,577 | |
| 5 | Jambi | 1265 | 473 | 3,397,164 | |
| 6 | Bengkulu | 751 | 254 | 1,872,136 | |
| 7 | South Sumatera | 2064 | 760 | 8,043,042 | |
| 8 | Lampung | 1954 | 669 | 8,109,601 | |
| 9 | Island of Riau | 735 | 270 | 1,968,313 | |
| 10 | Island of Bangka Belitung | 535 | 217 | 1,370,331 | |
| 11 | Java | Banten | 3483 | 1443 | 11,934,373 |
| 12 | West Java | 17,273 | 7791 | 46,668,214 | |
| 13 | Central Java | 15,149 | 7277 | 33,753,023 | |
| 14 | Special Region of Jakarta | 6256 | 2825 | 10,154,134 | |
| 15 | Special Region of Yogyakarta | 2478 | 1300 | 3,675,768 | |
| 16 | East Java | 12,636 | 5623 | 38,828,061 | |
| 17 | Kalimantan | West Kalimantan | 1208 | 501 | 4,783,209 |
| 18 | Central Kalimantan | 727 | 333 | 2,490,178 | |
| 19 | South Kalimantan | 1043 | 440 | 3,984,315 | |
| 20 | East Kalimantan | 1639 | 621 | 3,422,676 | |
| 21 | North Kalimantan | 341 | 131 | 639,639 | |
| 22 | West Sulawesi | 352 | 151 | 1,279,994 | |
| 23 | Central Sulawesi | 986 | 428 | 2,872,857 | |
| 24 | Sulawesi | Gorontalo | 531 | 225 | 1,131,670 |
| 25 | North Sulawesi | 1319 | 551 | 2,409,921 | |
| 26 | South Sulawesi | 3580 | 1355 | 8,512,608 | |
| 27 | Southeast Sulawesi | 650 | 243 | 2,495,248 | |
| 28 | Maluku | North Maluku | 265 | 112 | 1,160,275 |
| 29 | Maluku | 483 | 194 | 1,683,856 | |
| 30 | Nusa | Bali | 1607 | 569 | 4,148,588 |
| 31 | Tenggara | West Nusa Tenggara | 1282 | 517 | 4,830,118 |
| 32 | East Nusa Tenggara | 1394 | 571 | 5,112,760 | |
| 33 | Papua | West Papua | 978 | 351 | 868,819 |
| 34 | Papua | 411 | 156 | 3,143,088 | |
| Total | 95,504 | 41,190 | 255,182,144 |
| Characteristics | Overall | POR by Region | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||
| Gender | Male | Reference | |||||
| Female | 1.0 | 1.0 | 1.0 ns | 1.0 ns | 1.0 ns | 1.0 ns | |
| Age group (years) | ≤39 | Reference | |||||
| 40−44 | 2.2 | 2.2 | 2.5 | 2.0 | 2.5 | 2.0 | |
| 45−49 | 2.9 | 2.9 | 2.7 | 3.1 | 3.0 | 2.7 | |
| 50−54 | 4.0 | 4.1 | 3.6 | 3.8 | 3.7 | 4.1 | |
| 55−59 | 4.8 | 4.9 | 4.5 | 4.6 | 4.7 | 3.6 | |
| 60−64 | 5.4 | 5.7 | 5.4 | 4.3 | 5.8 | 5.5 | |
| ≥65 | 6.1 | 6.2 | 6.1 | 5.4 | 5.6 | 6.5 | |
| Marital status | Currently not married | Reference | |||||
| Currently married | 1.6 | 1.6 | 1.6 | 1.6 | 1.5 | 1.6 | |
| Type of membership | Subsidies’ recipients | Reference | |||||
| Non subsidies’ recipients | 1.3 | 1.2 | 1.3 | 1.3 | 1.0 ns | 1.2 | |
| Legend: | |||||||
| Prevalence odds ratio (POR) | 0–2 | 2.1–3.1 | 3.2–4.1 | 4.2–5.4 | 5.5–6.5 | ||
| No. | Opportunities | Challenges |
|---|---|---|
| 1. | Presents patterns across various aspects including demographic characteristics, time, spatial distinctions, disease dyads, and claim-related variables | Contains no disease severity data or information on laboratory results |
| 2. | More economical than primary data collection through a survey | Does not record out of pocket expenditures |
| 3. | Not influenced by recall bias | May be affected by misclassification errors of diagnoses |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Husnayain, A.; Ekadinata, N.; Sulistiawan, D.; Chia-Yu Su, E. Multimorbidity Patterns of Chronic Diseases among Indonesians: Insights from Indonesian National Health Insurance (INHI) Sample Data. Int. J. Environ. Res. Public Health 2020, 17, 8900. https://doi.org/10.3390/ijerph17238900
Husnayain A, Ekadinata N, Sulistiawan D, Chia-Yu Su E. Multimorbidity Patterns of Chronic Diseases among Indonesians: Insights from Indonesian National Health Insurance (INHI) Sample Data. International Journal of Environmental Research and Public Health. 2020; 17(23):8900. https://doi.org/10.3390/ijerph17238900
Chicago/Turabian StyleHusnayain, Atina, Nopryan Ekadinata, Dedik Sulistiawan, and Emily Chia-Yu Su. 2020. "Multimorbidity Patterns of Chronic Diseases among Indonesians: Insights from Indonesian National Health Insurance (INHI) Sample Data" International Journal of Environmental Research and Public Health 17, no. 23: 8900. https://doi.org/10.3390/ijerph17238900
APA StyleHusnayain, A., Ekadinata, N., Sulistiawan, D., & Chia-Yu Su, E. (2020). Multimorbidity Patterns of Chronic Diseases among Indonesians: Insights from Indonesian National Health Insurance (INHI) Sample Data. International Journal of Environmental Research and Public Health, 17(23), 8900. https://doi.org/10.3390/ijerph17238900






