Outcomes of Culturally Tailored Dietary Intervention in the North African and Bangladeshi Diabetic Patients in Italy
Abstract
1. Introduction
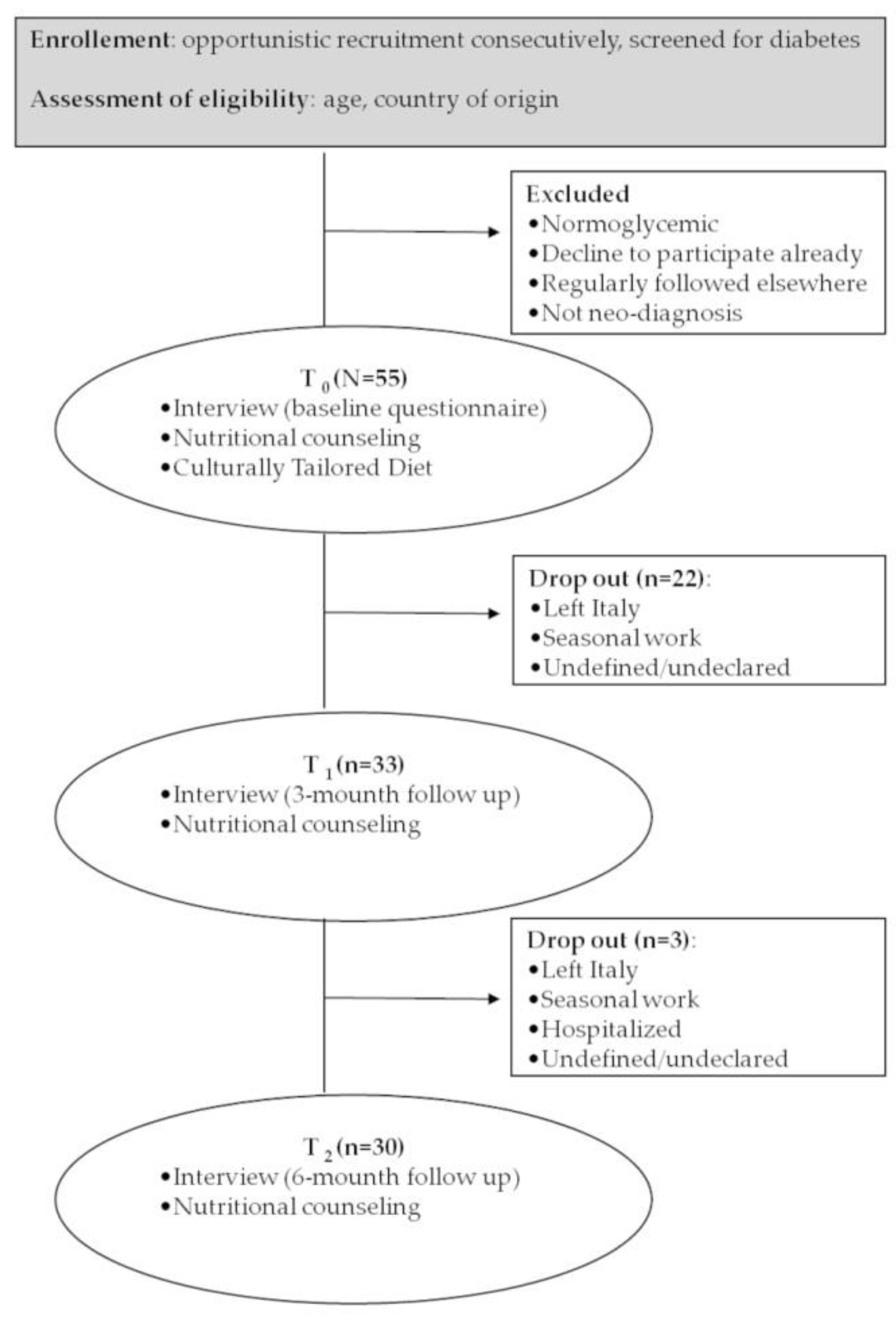
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McAuliffe, M.; Khadria, B. (Eds.) World Migration Report 2020; International Organization for Migration: Geneva, Switzerland, 2019; ISBN 978-92-9068-789-4. [Google Scholar]
- Lee, S.; O’Neill, A.H.; Ihara, E.S.; Chae, D.H. Change in self-reported health status among immigrants in the United States: Associations with measures of acculturation. PLoS ONE 2013, 8, e76494. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, A.; Di Napoli, A.; Demuru, E.; Ventura, M.; Gnavi, R.; Di Minco, L.; Tamburini, C.; Mirisola, C.; Sebastiani, G. Socioeconomic and citizenship inequalities in hospitalisation of the adult population in Italy. PLoS ONE 2020, 15, e0231564. [Google Scholar] [CrossRef]
- Rechel, B. (Ed.) Migration and Health in EUROPEAN Union; European Observatory on Health Systems and Policies Series; McGraw Hill/Open University Press: Maidenhead, UK, 2011; ISBN 978-0-335-24567-3. [Google Scholar]
- Gushulak, B.; Weekers, J.; MacPherson, D. Migrants and emerging public health issues in a globalized world: Threats, risks and challenges, an evidence-based framework. Emerg. Health Threat. J. 2010, 2. [Google Scholar] [CrossRef]
- Commodore-Mensah, Y.; Selvin, E.; Aboagye, J.; Turkson-Ocran, R.-A.; Li, X.; Himmelfarb, C.D.; Ahima, R.S.; Cooper, L.A. Hypertension, overweight/obesity, and diabetes among immigrants in the United States: An analysis of the 2010–2016 National Health Interview Survey. BMC Public Health 2018, 18, 773. [Google Scholar] [CrossRef]
- Petrelli, A.; Di Napoli, A.; Perez, M.; Gargiulo, L. The health status of the immigrant population in Italy: Evidence from multipurpose surveys of the Italian National Institute of Statistics (Istat). Epidemiol. Prev. 2017, 41, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Dalla Zuanna, T.; Cacciani, L.; Barbieri, G.; Ferracin, E.; Zengarini, N.; Di Girolamo, C.; Caranci, N.; Petrelli, A.; Marino, C.; Agabiti, N.; et al. Avoidable hospitalisation for diabetes mellitus among immigrants and natives: Results from the Italian Network for Longitudinal Metropolitan Studies. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1535–1543. [Google Scholar] [CrossRef] [PubMed]
- Marzona, I.; Avanzini, F.; Tettamanti, M.; Vannini, T.; Fortino, I.; Bortolotti, A.; Merlino, L.; Genovese, S.; Roncaglioni, M.C. Prevalence and management of diabetes in immigrants resident in the Lombardy Region: The importance of ethnicity and duration of stay. Acta Diabetol. 2018, 55, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Fedeli, U.; Casotto, V.; Ferroni, E.; Saugo, M.; Targher, G.; Zoppini, G. Prevalence of diabetes across different immigrant groups in North-eastern Italy. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 924–930. [Google Scholar] [CrossRef]
- Jabbar, A.; Abdallah, K.; Hassoun, A.; Malek, R.; Senyucel, C.; Spaepen, E.; Treuer, T.; Bhattacharya, I. Patterns and trends in insulin initiation and intensification among patients with Type 2 diabetes mellitus in the Middle East and North Africa region. Diabetes Res. Clin. Pract. 2019, 149, 18–26. [Google Scholar] [CrossRef]
- Abdulah, D.M.; Hassan, A.B.; Saadi, F.S.; Mohammed, A.H. Impacts of self-management education on glycaemic control in patients with type 2 diabetes mellitus. Diabetes Metab. Syndr. Clin. Res. Rev. 2018, 12, 969–975. [Google Scholar] [CrossRef]
- Ley, S.H.; Hamdy, O.; Mohan, V.; Hu, F.B. Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet 2014, 383, 1999–2007. [Google Scholar] [CrossRef]
- Pan, B.; Wu, Y.; Yang, Q.; Ge, L.; Gao, C.; Xun, Y.; Tian, J.; Ding, G. The impact of major dietary patterns on glycemic control, cardiovascular risk factors, and weight loss in patients with type 2 diabetes: A network meta-analysis. J. Evid. Based Med. 2019, 12, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Mora, N.; Golden, S.H. Understanding Cultural Influences on Dietary Habits in Asian, Middle Eastern, and Latino Patients with Type 2 Diabetes: A Review of Current Literature and Future Directions. Curr. Diab Rep. 2017, 17, 126. [Google Scholar] [CrossRef] [PubMed]
- Vanstone, M.; Giacomini, M.; Smith, A.; Brundisini, F.; DeJean, D.; Winsor, S. How diet modification challenges are magnified in vulnerable or marginalized people with diabetes and heart disease: A systematic review and qualitative meta-synthesis. Ont. Health Technol. Assess. Ser. 2013, 13, 1–40. [Google Scholar]
- Chambre, C.; Gbedo, C.; Kouacou, N.; Fysekidis, M.; Reach, G.; Le Clesiau, H.; Bihan, H. Migrant adults with diabetes in France: Influence of family migration. J. Clin. Transl. Endocrinol. 2017, 7, 28–32. [Google Scholar] [CrossRef]
- Smith-Miller, C.A.; Berry, D.C.; Miller, C.T. Diabetes affects everything: Type 2 diabetes self-management among Spanish-speaking hispanic immigrants. Res. Nurs. Health 2017, 40, 541–554. [Google Scholar] [CrossRef]
- Zeh, P.; Sandhu, H.K.; Cannaby, A.M.; Sturt, J.A. Cultural barriers impeding ethnic minority groups from accessing effective diabetes care services: A systematic review of observational studies. Divers. Equal. Health Care 2014, 11. [Google Scholar] [CrossRef]
- Association, A.D. 4. Lifestyle Management: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018, 41, S38–S50. [Google Scholar] [CrossRef]
- Islam, N.S.; Wyatt, L.C.; Taher, M.D.; Riley, L.; Tandon, S.D.; Tanner, M.; Mukherji, B.R.; Trinh-Shevrin, C. A Culturally Tailored Community Health Worker Intervention Leads to Improvement in Patient-Centered Outcomes for Immigrant Patients With Type 2 Diabetes. Clin. Diabetes 2018, 36, 100–111. [Google Scholar] [CrossRef]
- Lagisetty, P.A.; Priyadarshini, S.; Terrell, S.; Hamati, M.; Landgraf, J.; Chopra, V.; Heisler, M. Culturally Targeted Strategies for Diabetes Prevention in Minority Population: A Systematic Review and Framework. Diabetes Educ. 2017, 43, 54–77. [Google Scholar] [CrossRef]
- Nam, S.; Janson, S.L.; Stotts, N.A.; Chesla, C.; Kroon, L. Effect of Culturally Tailored Diabetes Education in Ethnic Minorities With Type 2 Diabetes: A Meta-analysis. J. Cardiovasc. Nurs. 2012, 27, 505–518. [Google Scholar] [CrossRef]
- Jaworski, M.; Panczyk, M.; Cedro, M.; Kucharska, A. Adherence to dietary recommendations in diabetes mellitus: Disease acceptance as a potential mediator. Patient Prefer. Adherence 2018, 12, 163–174. [Google Scholar] [CrossRef]
- Franz, M.J.; MacLeod, J.; Evert, A.; Brown, C.; Gradwell, E.; Handu, D.; Reppert, A.; Robinson, M. Academy of Nutrition and Dietetics Nutrition Practice Guideline for Type 1 and Type 2 Diabetes in Adults: Systematic Review of Evidence for Medical Nutrition Therapy Effectiveness and Recommendations for Integration into the Nutrition Care Process. J. Acad. Nutr. Diet. 2017, 117, 1659–1679. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; van Halen, C.; van Baaren, R.B.; Müller, B.C.N. Self-Persuasion Increases Healthy Eating Intention Depending on Cultural Background. Int. J. Environ. Res. Public Health 2020, 17, 3405. [Google Scholar] [CrossRef]
- Cunha, L.M.; Cabral, D.; Moura, A.P.; de Almeida, M.D.V. Application of the Food Choice Questionnaire across cultures: Systematic review of cross-cultural and single country studies. Food Qual. Prefer. 2018, 64, 21–36. [Google Scholar] [CrossRef]
- Gibson, R.S. Principles of Nutritional Assessment; Oxford University Press: New York, NY, USA, 2005; ISBN 978-0-19-517169-3. [Google Scholar]
- FAOSTAT. Available online: http://www.fao.org/faostat/en/#data/FBS/report (accessed on 21 January 2017).
- Association, A.D. Standards of Medical Care in Diabetes—2016: Summary of Revisions. Diabetes Care 2016, 39, S4–S5. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, M.; Mente, A.; Zhang, X.; Swaminathan, S.; Li, W.; Mohan, V.; Iqbal, R.; Kumar, R.; Wentzel-Viljoen, E.; Rosengren, A.; et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): A prospective cohort study. Lancet 2017, 390, 2050–2062. [Google Scholar] [CrossRef]
- Gilbert, P.A.; Khokhar, S. Changing dietary habits of ethnic groups in Europe and implications for health Affiliations. Nutr. Rev. 2008, 66, 203–215. [Google Scholar] [CrossRef]
- Abaza, H.; Marschollek, M. SMS education for the promotion of diabetes self-management in low & middle income countries: A pilot randomized controlled trial in Egypt. BMC Public Health 2017, 17, 962. [Google Scholar] [CrossRef]
- Stewart-Knox, B.; Rankin, A.; Kuznesof, S.; Poínhos, R.; de Almeida, M.D.V.; Fischer, A.; Frewer, L.J. Promoting healthy dietary behaviour through personalised nutrition: Technology push or technology pull? Proc. Nutr. Soc. 2015, 74, 171–176. [Google Scholar] [CrossRef]
- Alzubaidi, H.; Namara, K.M.; Browning, C. Time to question diabetes self-management support for Arabic-speaking migrants: Exploring a new model of care. Diabet. Med. 2017, 34, 348–355. [Google Scholar] [CrossRef]
- Abuelmagd, W.; Håkonsen, H.; Mahmood, K.Q.-A.; Taghizadeh, N.; Toverud, E.-L. Living with Diabetes: Personal Interviews with Pakistani Women in Norway. J. Immigr. Minority Health 2018, 20, 848–853. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.; Garg, V.; Kapoor, D.; Wasser, H.; Prabhakaran, D.; Jaacks, L.M. Food Choice Drivers in the Context of the Nutrition Transition in Delhi, India. J. Nutr. Educ. Behav. 2018, 50, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Kohinor, M.J.E.; Stronks, K.; Nicolaou, M.; Haafkens, J.A. Considerations affecting dietary behaviour of immigrants with type 2 diabetes: A qualitative study among Surinamese in the Netherlands. Ethn. Health 2011, 16, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Reinders, M.J.; Bouwman, E.P.; van den Puttelaar, J.; Verain, M.C.D. Consumer acceptance of personalised nutrition: The role of ambivalent feelings and eating context. PLoS ONE 2020, 15, e0231342. [Google Scholar] [CrossRef] [PubMed]
- Celis-Morales, C.; Livingstone, K.M.; Marsaux, C.F.; Macready, A.L.; Fallaize, R.; O’Donovan, C.B.; Woolhead, C.; Forster, H.; Walsh, M.C.; Navas-Carretero, S.; et al. Effect of personalized nutrition on health-related behaviour change: Evidence from the Food4Me European randomized controlled trial. Int. J. Epidemiol. 2017, 46, 578–588. [Google Scholar] [CrossRef]
- Bush, C.L.; Blumberg, J.B.; El-Sohemy, A.; Minich, D.M.; Ordovás, J.M.; Reed, D.G.; Behm, V.A.Y. Toward the Definition of Personalized Nutrition: A Proposal by The American Nutrition Association. J. Am. Coll. Nutr. 2020, 39, 5–15. [Google Scholar] [CrossRef]
- Malmusi, D.; Borrella, C.; Benach, J. Migration-related health inequalities: Showing the complex interactions between gender, social class and place of origin. Soc. Sci. Med. 2010, 71, 1610–1619. [Google Scholar] [CrossRef]
- de Waure, C.; Bruno, S.; Furia, G.; Di Sciullo, L.; Carovillano, S.; Specchia, M.L.; Geraci, S.; Ricciardi, W. Health inequalities: An analysis of hospitalizations with respect to migrant status, gender and geographical area. BMC Int. Health Hum. Rights 2015, 15, 2. [Google Scholar] [CrossRef]
- Gkiouleka, A.; Huijts, T. Intersectional migration-related health inequalities in Europe: Exploring the role of migrant generation, occupational status & gender. Soc. Sci. Med. 2020, 17, 113218. [Google Scholar] [CrossRef]
- Sugerman, S.; Backman, D.; Foerster, S.B.; Ghirardelli, A.; Linares, A.; Fong, A. Using an Opinion Poll to Build an Obesity-Prevention Social Marketing Campaign for Low-Income Asian and Hispanic Immigrants: Report of Findings. J. Nutr. Educ. Behav. 2011, 43, S53–S66. [Google Scholar] [CrossRef] [PubMed]
- Metwally, A.M.; Soliman, M.; Abdelmohsen, A.M.; Kandeel, W.A.; Saber, M.; Elmosalami, D.M.; Asem, N.; Fathy, A.M. Effect of Counteracting Lifestyle Barriers through Health Education in Egyptian Type 2 Diabetic Patients. Open Access. Maced J. Med. Sci. 2019, 7, 2886–2894. [Google Scholar] [CrossRef] [PubMed]
| Main Meal | Bangladesh | Egypt |
|---|---|---|
| Breakfast | Salty Tea/coffee (sugar free) with ruti and boiled shak vegetable (no peas or potatoes) | Sweety Light yogurt and sugar free tea with biscuits |
| Lunch | A meal of parboiled/brown rice and salad as aperitif Rice with dhal or Rice with meat/fish curry or Rice with shobji and eggs or Rice with shak | A meal of parboiled/brown rice Koshari and vegetables or Sayydaiah and rice with vegetables or Melokhia with meat and rice |
| Dinner | Ruti with shobji (no potatoes) and light yogurt or Fish rui/tengra/rupchada with turmeric and ruti or ½ ruti with aloo or Ruti with dhal | Couscous with chickpeas/fish/meat and vegetables or Pasta with vegetables/meat/fish sauce and salad |
| Characteristic | M (Range) | n | % |
|---|---|---|---|
| Sex (n, %) | |||
| Male | 49 | 89 | |
| Female | 6 | 11 | |
| Age, y (M, range) | 44.3 (22–65) | ||
| ≤29 | 3 | 5 | |
| 30-39 | 14 | 25 | |
| 40–49 | 20 | 36 | |
| ≥50 | 18 | 34 | |
| Origin (n, %) | |||
| Bangladesh | 37 | 67 | |
| Morocco | 10 | 18 | |
| Algeria | 2 | 4 | |
| Tunisia | 1 | 2 | |
| Egypt | 5 | 9 | |
| Religion (n, %) | |||
| Muslim | 53 | 96 | |
| Hinduism | 2 | 4 | |
| Qualification (n, %) | |||
| Not schooled | 7 | 13 | |
| Junior high school diploma | 28 | 51 | |
| High school diploma | 11 | 20 | |
| Degree and beyond | 9 | 16 | |
| Area of origin (n, %) | |||
| Rural area | 21 | 56 | |
| Urban area | 24 | 44 | |
| Living in Italy, y (M, range) | 11.4 (0–41) | ||
| Accommodation (n, %) | |||
| House rent with family or compatriots | 36 | 66 | |
| As guest | 9 | 16 | |
| Migrants helter | 5 | 9 | |
| Homeless | 4 | 7 | |
| Own house | 1 | 2 | |
| Juridical status (n, %) | |||
| Irregular | 26 | 47 | |
| Regular | 29 | 53 | |
| Work (n, %) | |||
| Unemployed | 16 | 29 | |
| Employed | 39 | 71 |
| Items | Categories | n | % |
|---|---|---|---|
| Degree of satisfaction with the diet 1 | 1 | 6 | 11 |
| 2 | 4 | 7 | |
| 3 | 17 | 31 | |
| 4 | 12 | 22 | |
| 5 | 16 | 29 | |
| How much diet have changed after arriving in Italy 2 | 1 | 9 | 16 |
| 2 | 9 | 16 | |
| 3 | 14 | 26 | |
| 4 | 10 | 18 | |
| 5 | 13 | 24 | |
| Kind of diet followed in Italy | Only or mainly typical of own country | 40 | 73 |
| Only or mainly Italian | 15 | 27 | |
| Principal reasons | «I prefer it» | 31 | 56 |
| «I have no choice» | 20 | 36 | |
| «People who cook for me prefer it» | 2 | 4 | |
| «It’s cheaper» | 1 | 2 | |
| «Other» | 1 | 2 | |
| Most common bad dietary habits | «I don’t know» | 32 | 57 |
| «I eat badly (qualitatively)» | 11 | 20 | |
| «I eat too many sweets» | 7 | 13 | |
| «I often eat out of meals» | 2 | 4 | |
| «I eat too much» | 1 | 2 | |
| «Other» | 2 | 4 | |
| What the patient eats depends on... | «My personal taste» | 27 | 49 |
| «What I find ready to eat» | 13 | 24 | |
| «Taste of people I live with» | 11 | 20 | |
| «How much money I can spend» | 3 | 5 | |
| «What is given to me (food parcels, gifts)» | 1 | 2 | |
| Principal difficulties in management of food behaviors | «Eating well is expensive» | 11 | 20 |
| «I don’t have any difficulties» | 21 | 38 | |
| «I have no choice» | 7 | 13 | |
| «Laziness or lack of time» | 4 | 7 | |
| «I always have stomachache» | 2 | 4 | |
| «Respect for religious prescriptions» | 1 | 2 | |
| «Fear of forgetting the origins» | 1 | 2 | |
| «Other» | 8 | 14 |
| Food Categories | Patients with Adequate Consumption n (%) | ||
|---|---|---|---|
| Before | After | Δ | |
| Daily | |||
| Meals (4–5) | 7 (23.3) | 13 (43.3) | +6 (+20.0) |
| Fruit and vegetable (3–5) | 5 (16.7) | 10 (33.3) | +5 (+16.6) |
| Cereals and derivatives (3) | 7 (23.3) | 14 (46.7) | +7 (+23.4) 1 |
| Milk and yogurt (1–2) | 15 (50.0) | 18 (60.0) | +3 (+10.0) |
| Weekly | |||
| Meat (2–3) | 3 (10.0) | 12 (40.0) | +9 (+30.0) 1 |
| Legumes (≥ 2) | 24 (80.0) | 26 (86.7) | +2 (+6.7) |
| Fish (≥ 2) | 26 (86.7) | 27 (90.0) | +1 (+3.3) |
| Potatoes (≤ 2) | 19 (63.3) | 27 (90.0) | +8 (+26.7) 1 |
| Cheese (≤ 2) | 24 (80.0) | 27 (90.0) | +3 (+10.0) |
| Monthly (rare) | |||
| Snack | 22 (73.3) | 21 (70.0) | −1 (−3.3) |
| Alcohol drinks | 30 (100) | 29 (96.7) | −1 (−3.3) |
| Soft drinks | 16 (53.3) | 18 (60.0) | +2 (+6.7) |
| Nr of adequate dietary habits per patient (median) | 7 | 8 | +1 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piombo, L.; Nicolella, G.; Barbarossa, G.; Tubili, C.; Pandolfo, M.M.; Castaldo, M.; Costanzo, G.; Mirisola, C.; Cavani, A. Outcomes of Culturally Tailored Dietary Intervention in the North African and Bangladeshi Diabetic Patients in Italy. Int. J. Environ. Res. Public Health 2020, 17, 8932. https://doi.org/10.3390/ijerph17238932
Piombo L, Nicolella G, Barbarossa G, Tubili C, Pandolfo MM, Castaldo M, Costanzo G, Mirisola C, Cavani A. Outcomes of Culturally Tailored Dietary Intervention in the North African and Bangladeshi Diabetic Patients in Italy. International Journal of Environmental Research and Public Health. 2020; 17(23):8932. https://doi.org/10.3390/ijerph17238932
Chicago/Turabian StylePiombo, Laura, Gianluca Nicolella, Giulia Barbarossa, Claudio Tubili, Mayme Mary Pandolfo, Miriam Castaldo, Gianfranco Costanzo, Concetta Mirisola, and Andrea Cavani. 2020. "Outcomes of Culturally Tailored Dietary Intervention in the North African and Bangladeshi Diabetic Patients in Italy" International Journal of Environmental Research and Public Health 17, no. 23: 8932. https://doi.org/10.3390/ijerph17238932
APA StylePiombo, L., Nicolella, G., Barbarossa, G., Tubili, C., Pandolfo, M. M., Castaldo, M., Costanzo, G., Mirisola, C., & Cavani, A. (2020). Outcomes of Culturally Tailored Dietary Intervention in the North African and Bangladeshi Diabetic Patients in Italy. International Journal of Environmental Research and Public Health, 17(23), 8932. https://doi.org/10.3390/ijerph17238932





