Effects of Trunk Exercise on Unstable Surfaces in Persons with Stroke: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
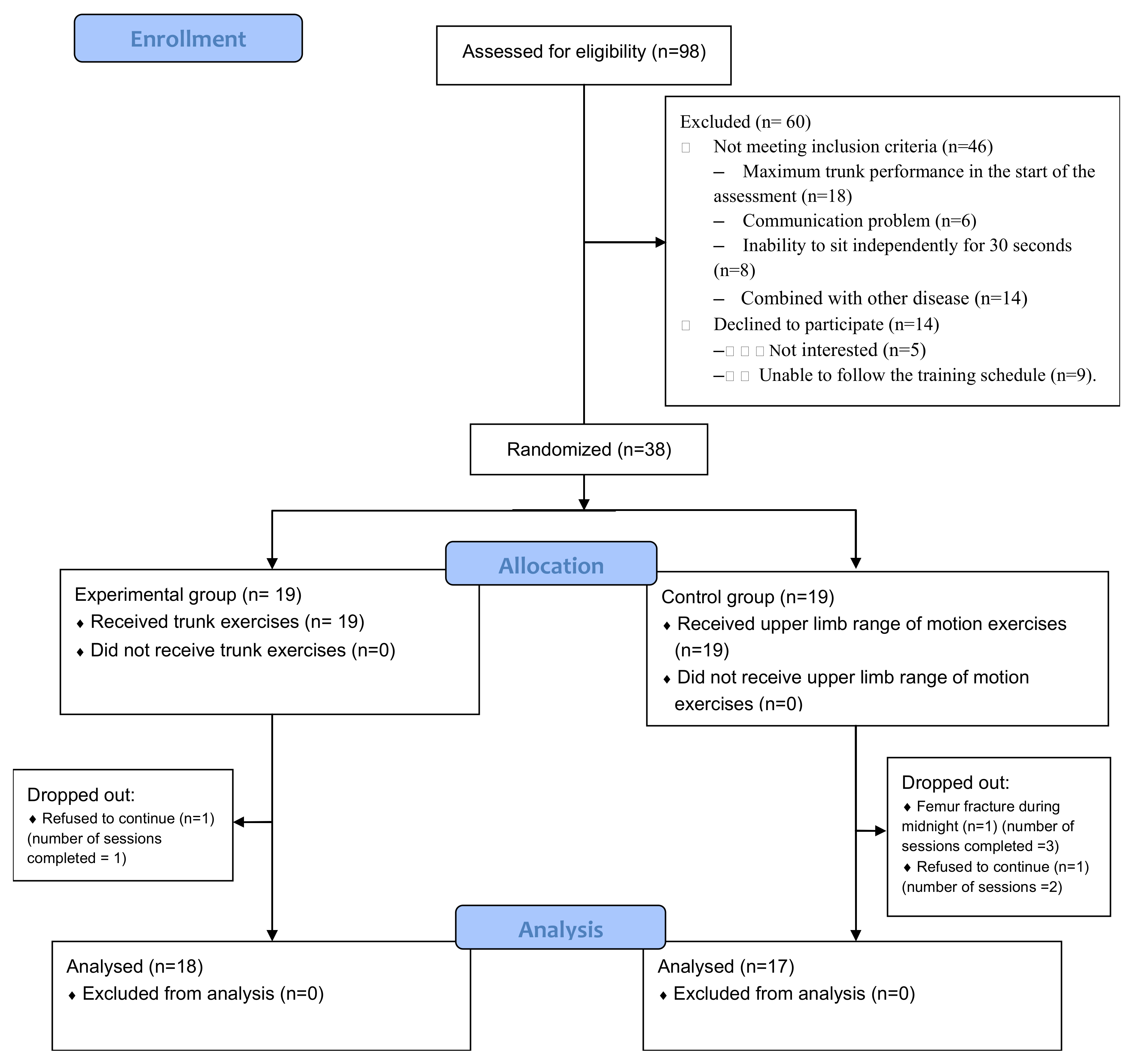
2.1. Study Design and Setting
2.2. Participants
2.3. Sensorimotor Function and Walking Assessment
2.4. Balance Assessment
2.5. Intervention
2.6. Outcome Measures
2.7. Statistical Analysis
2.8. Data Availability
3. Results
3.1. Sensorimotor Function and Walking
3.2. Sitting Performance
3.3. Standing Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Norrving, B.; Mensah, G.A. Global burden of stroke. Circ. Res. 2017, 120, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Scuffham, P.; Chaplin, S.; Legood, R. Incidence and costs of unintentional falls in older people in the United Kingdom. J. Epidemiol. Community Health 2003, 57, 740–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lamb, S.E.; Ferrucci, L.; Volapto, S.; Fried, L.P.; Guralnik, J.M. Risk factors for falling in home-dwelling older women with stroke: The Women’s Health and Aging Study. Stroke 2003, 34, 494–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwakkel, G.; Wagenaar, R.C.; Kollen, B.J.; Lankhorst, G.J. Predicting disability in stroke—A critical review of the literature. Age Ageing 1996, 25, 479–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tyson, S.F.; Hanley, M.; Chillala, J.; Selley, A.; Tallis, R.C. Balance disability after stroke. Phys. Ther. Sport 2006, 86, 30–38. [Google Scholar] [CrossRef] [Green Version]
- Vincent-Onabajo, G.; Musa, H.Y.; Joseph, E. Prevalence of balance impairment among stroke survivors undergoing neurorehabilitation in Nigeria. J. Stroke Cerebrovasc. Dis. 2018, 27, 3487–3492. [Google Scholar] [CrossRef] [PubMed]
- De Haart, M.; Geurts, A.C.; Huidekoper, S.C.; Fasotti, L.; van Limbeek, J. Recovery of standing balance in postacute stroke patients: A rehabilitation cohort study. Arch. Phys. Med. Rehabil. 2004, 85, 886–895. [Google Scholar] [CrossRef]
- van Dijk, M.M.; Meyer, S.; Sandstad, S.; Wiskerke, E.; Thuwis, R.; Vandekerckhove, C. A cross-sectional study comparing lateral and diagonal maximum weight shift in people with stroke and healthy controls and the correlation with balance, gait and fear of falling. PLoS ONE 2017, 12, e0183020. [Google Scholar] [CrossRef] [Green Version]
- McCombe Waller, S.; Yang, C.L.; Magder, L.; Yungher, D.; Creath, R.; Gray, V.; Roger, M.W. Impaired motor preparation and execution during standing reach in people with chronic stroke. Neurosci. Lett. 2016, 630, 38–44. [Google Scholar] [CrossRef]
- Dickstein, R.; Shefi, S.; Marcovitz, E.; Villa, Y. Anticipatory postural adjustment in selected trunk muscles in post stroke hemiparetic patients. Arch. Phys. Med. Rehabil. 2004, 85, 261–267. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Cassidy, D.; Walsh, S. Trunk muscle strength is impaired multidirectionally after stroke. Clin. Rehabil. 1995, 9, 47–51. [Google Scholar] [CrossRef]
- Tanaka, S.; Hachisuka, K.; Ogata, H. Trunk rotatory muscle performance in post-stroke hemiplegic patients. Am. J. Phys. Med. Rehabil. 1997, 76, 366–369. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Hachisuka, K.; Ogata, H. Muscle strength of trunk flexion-extension in post-stroke hemiplegic patients. Am. J. Phys. Med. Rehabil. 1998, 77, 288–290. [Google Scholar] [CrossRef] [PubMed]
- Ryerson, S.; Byl, N.N.; Brown, D.A.; Wong, R.A.; Hidler, J.M. Altered trunk position sense and its relation to balance functions in people post-stroke. J. Neurol. Phys. Ther. 2008, 32, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karatas, M.; Çetin, N.; Bayramoglu, M.; Dilek, A. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. Am. J. Phys. Med. Rehabil. 2004, 83, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Van Criekinge, T.; Truijen, S.; Schroder, J.; Maebe, Z.; Blanckaert, K.; van der Waal, C.; Vink, M.; Saeys, W. The effectiveness of trunk training on trunk control, sitting and standing balance and mobility post-stroke: A systematic review and meta-analysis. Clin. Rehabil. 2019, 33, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Haruyama, K.; Kawakami, M.; Otsuka, T. Effect of core stability training on trunk function, standing balance, and mobility in stroke patients. Neurorehabil. Neural Repair 2017, 31, 240–249. [Google Scholar] [CrossRef] [Green Version]
- Cabanas-Valdes, R.; Cuchi, G.U.; Bagur-Calafat, C. Trunk training exercises approaches for improving trunk performance and functional sitting balance in patients with stroke: A systematic review. NeuroRehabilitation 2013, 33, 575–592. [Google Scholar] [CrossRef]
- Yoon, H.S.; Cha, Y.J.; You, J.S.H. Effects of dynamic core-postural chain stabilization on diaphragm movement, abdominal muscle thickness, and postural control in patients with subacute stroke: A randomized control trial. NeuroRehabilitation 2020, 46, 381–389. [Google Scholar] [CrossRef]
- Czaprowski, D.; Afeltowicz, A.; Gebicka, A.; Pawlowska, P.; Kedra, A.; Barrios, C.; Hadala, M. Abdominal muscle EMG-activity during bridge exercises on stable and unstable surfaces. Phys. Ther. Sport. 2014, 15, 162–168. [Google Scholar] [CrossRef]
- Vera-Garcia, F.J.; Grenier, S.G.; McGill, S.M. Abdominal muscle response during curl-ups on both stable and labile surfaces. Phys. Ther. 2000, 80, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Marshall, P.W.; Desai, I. Electromyographic analysis of upper body, lower body, and abdominal muscles during advanced Swiss ball exercises. J. Strength Cond. Res. 2010, 24, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Behm, D.G.; Anderson, K.; Curnew, R.S. Muscle force and activation under stable and unstable conditions. J. Strength. Cond. Res. 2002, 16, 416–422. [Google Scholar]
- Lam, H.S.; Lau, F.W.; Chan, G.K.; Sykes, K. The validity and reliability of a 6-Metre Timed Walk for the functional assessment of patients with stroke. Physiother. Theory Pract. 2010, 26, 251–255. [Google Scholar] [CrossRef]
- Behm, D.G.; Drinkwater, E.J.; Willardson, J.M.; Cowley, P.M. The use of instability to train the core musculature. Appl. Physiol. Nutr. Metab. 2010, 35, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Teasell, R.; Hussein, N. Background Concepts in Stroke Rehabilitation. In Evidence Based Review of Stroke Rehabilitation [Internet]; EBTSR: London, ON, Canada, 2019; Available online: http://www.ebrsr.com/sites/default/files/v18-SREBR-CH3-NET.pdf (accessed on 11 April 2020).
- Van Criekinge, T.; Saeys, W.; Vereeck, L.; De Hertogh, W.; Truijen, S. Are unstable support surfaces superior to stable support surfaces during trunk rehabilitation after stroke? A systematic review. Disabil. Rehabil. 2018, 17, 1981–1988. [Google Scholar] [CrossRef]
- Horak, F.B.; Esselman, P.; Anderson, M.E.; Lynch, M.K. The effects of movement velocity, mass displaced, and task certainty on associated postural adjustments made by normal and hemiplegic individuals. J. Neurol. Neurosurg. Psychiatry 1984, 47, 1020–1028. [Google Scholar] [CrossRef] [Green Version]
- Garland, S.J.; Stevenson, T.J.; Ivanova, T. Postural responses to unilateral arm perturbation in young, elderly, and hemiplegic subjects. Arch. Phys. Med. Rehabil. 1997, 78, 1072–1077. [Google Scholar] [CrossRef]
- Milosevic, M.; Masani, K.; Kuipers, M.J.; Rahouni, H.; Verrier, M.C.; McConville, K.M.; Popovic, M.R. Trunk control impairment is responsible for postural instability during quiet sitting in individuals with cervical spinal cord injury. Clin. Biomech. 2015, 30, 507–512. [Google Scholar] [CrossRef]
- Verheyden, G.; Vereeck, L.; Truijen, S.; Troch, M.; Lafosse, C.; Saeys, W.; Leenaerts, E.; Palinckx, A.; De Weerdt, W. Additional exercises improve trunk performance after stroke: A pilot randomized controlled trial. Neurorehabil. Neural Repair 2009, 23, 281–286. [Google Scholar] [CrossRef]
- Saeys, W.; Vereeck, L.; Truijen, S.; Lafosse, C.; Wuyts, F.P.; Heyning, P.V. Randomized controlled trial of truncal exercises early after stroke to improve balance and mobility. Neurorehabil. Neural Repair 2012, 26, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Dean, C.; Shepherd, R.; Adams, R. Sitting balance I: Trunk-arm coordination and the contribution of the lower limbs during self-paced reaching in sitting. Gait Posture 1999, 10, 135–146. [Google Scholar] [CrossRef]
- Yoo, S.D.; Jeong, Y.S.; Kim, D.H.; Lee, M.A.; Noh, S.G.; Shin, Y.W.; Kim, S.H.; Kim, H.S. The Efficacy of Core Strengthening on the Trunk Balance in Patients with Subacute Stroke. Ann. Rehabil. Med. 2010, 34, 677–682. [Google Scholar]
- Cabanas-Valdes, R.; Bagur-Calafat, C.; Girabent-Farres, M.; Caballero-Gomez, F.M.; Hernandez-Valino, M.; Urrutia Cuchi, G. The effect of additional core stability exercises on improving dynamic sitting balance and trunk control for subacute stroke patients: A randomized controlled trial. Clin. Rehabil. 2016, 30, 1024–1033. [Google Scholar] [CrossRef] [PubMed]
- Patla, A.E.; Ishac, M.G.; Winter, D.A. Anticipatory control of center of mass and joint stability during voluntary arm movement from a standing posture: Interplay between active and passive control. Exp. Brain Res. 2002, 143, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.A. Anticipatory control of postural and task muscles during rapid arm flexion. J. Mot. Behav. 1980, 12, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Cordo, P.J.; Nashner, L.M. Properties of postural adjustments associated with rapid arm movements. J. Neurophysiol. 1982, 47, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Bazalgette, D.; Zattara, M.; Bathien, N.; Bouisset, S.; Rondot, P. Postural adjustments associated with rapid voluntary arm movements in patients with Parkinson’s disease. Adv. Neurol. 1986, 45, 371–374. [Google Scholar]
- Babu, K.; Nayak, A. Additional trunk training improves sitting balance following acute stroke: A pilot randomized controlled trial. Int. J. Curr. Res. Rev. 2011, 2, 26–43. [Google Scholar]
| Progression | Unstable Surface | ||
|---|---|---|---|
| Buttocks | Feet | ||
| Hook-lying | |||
| 1. Abdominal draw-in maneuver | None |  | |
| 2. Abdominal muscles isometric contraction | 1st |  | |
| 3. Lower trunk rotation | 2nd |  | |
| 4. Bridging with abdominal draw-in maneuver | 3rd |  |  |
| Sitting Level 1—sitting without foot support | |||
| 1. Pelvic anterior and posterior tilt | |||
| 2. Pelvic lateral tilt | 1st |  | |
| 3. Trunk flexion, extension, rotation | |||
| 4. Affected arm lateral reach with Swiss ball under the arm | 2nd |  | |
| 5. Pelvic rotation | |||
| Sitting Level 2—sitting on Swiss ball with feet on the ground | |||
| 1. Quiet sitting with chest expansion exercise |  | ||
| 2. Pelvic anterior and posterior tilt | |||
| 3. Pelvic lateral tilt | None | ||
| 4. Stepping | |||
| 5. Stepping with arm swing | |||
| Note. | |||
 | Balance pad | ||
 | BOSU ball | ||
 | Swiss ball | ||
| Control Group (n = 17) | Experimental Group (n = 18) | p | |
|---|---|---|---|
| Age (year) | 62.4 ± 13.3 | 60.2 ± 11.7 | 0.444 |
| Gender (male/female) | 9/8 | 10/8 | 0.122 |
| Height (cm) | 164.1 ± 6.7 | 166.1 ± 6.7 | 0.352 |
| Weight (kg) | 64.2 ± 10.2 | 74.6 ± 17.8 | 0.501 |
| Stroke onset time (weeks) | 6.9 ± 2.2 | 7.0 ± 2.7 | 0.695 |
| Affected side (left/right) | 7 /10 | 6/12 | 0.631 |
| Stroke type (infarction/hemorrhage) | 6/11 | 6/12 | 0.833 |
| Stroke location (number of participants) | |||
| Corona radiate | 3 | 2 | |
| Putamen | 5 | 7 | |
| Pons | 2 | 2 | |
| Thalamus | 1 | 1 | |
| Basal ganglion | 4 | 2 | |
| Frontal–temporal lobe | 1 | 0 | |
| Parieto-occipital lobe | 0 | 1 | |
| Corona radiate, basal ganglion, putamen | 1 | 2 | |
| Basal ganglion, thalamus | 1 | 0 | |
| Modified Ashworth scale (mean/median/mode) | |||
| Hip adductor | 0.1/0/0 | 0.2/0/0 | 0.581 |
| Hip flexor | 0.0/0/0 | 0.1/0/0 | 0.157 |
| Hip extensor | 0.1/0/0 | 0.2/0/0 | 0.316 |
| Knee extensor | 0.1/0/0 | 0.3/0/0 | 0.615 |
| Ankle dorsiflexor | 0.0/0/0 | 0.4/0/0 | 0.212 |
| Ankle plantarflexor | 0.3/0/0 | 0.5/0/0 | 0.549 |
| Control Group | Experimental Group | Pre-Training between-Group Comparisons | Post-Training between-Group Comparisons | |||||
|---|---|---|---|---|---|---|---|---|
| Pre-Training | Post-Training | Pre-Training | Post-Training | Mean Difference (95%CI) | p | Mean Difference (95%CI) | p | |
| Sensorimotor function | ||||||||
| Unaffected hand grip (kg) $ | 21.5 ± 12.0 | 23.5 ± 11.8 | 21.9 ± 7.9 | 23.8 ± 8.2 | 0.386 | 0.357 | ||
| Affected plantar sensitivity (log) $ | 4.8 ± 0.8 | 4.6 ± 0.8 | 4.9 ± 1.1 | 4.9 ± 1.0 | 0.708 | 0.708 | ||
| FMLE motor $ | 17.4 ± 5.5 | 18.7 ± 5.3 | 18.3 ± 6.3 | 18.6 ± 5.8 | 0.682 | 0.97 | ||
| STREAM $ | 36.6 ± 16.8 | 43.2 ± 14.0 | 40.2 ± 14.5 | 49.1 ± 13.9 | 0.369 | 0.218 | ||
| TIS total # | 14.9 ± 2.7 | 16.6 ± 1.7 | 14.6 ± 3.1 | 17.9 ± 2.3 | 0.804 (−1.006–2.613) | 0.373 | −1.458 (−2.814–−0.101) | 0.035 |
| 6 m walk (s) *$ | 34.4 ± 21.1 (n = 12) | 36.4 ± 22.5 (n = 17) | 29.7 ± 14.5 (n = 17) | 17.3 ± 8.0 (n = 18) | 0.434 | 0.012 | ||
| Sitting with foot support | ||||||||
| Static sway area (mm2) $ | 9.7 ± 8.7 | 11.3 ± 6.9 | 15.1 ± 18.5 | 9.5 ± 6.0 | 0.195 | 0.195 | ||
| Forward leaning (mm2) # | 39.1 ± 17.3 | 46.1 ± 20.2 | 55.8 ± 22.5 | 57.7 ± 18.0 | −16.690 (−30.547–−2.832) | 0.02 | −11.685 (−24.876–1.505) | 0.078 |
| Arm raising (degree/sec) $ | 124.8 ± 54.4 | 124.4 ± 42.5 | 132.5 ± 39.6 | 158.7 ± 41.6 | 0.732 | 0.564 | ||
| Sitting without foot support | ||||||||
| Static sway area (mm2) $ | 21.1 ± 18.6 | 17.4 ± 9.6 | 15.0 ± 10.5 | 11.9 ± 5.5 | 0.684 | 0.045 | ||
| Forward leaning (mm) ^# | 39.7 ± 16.6 | 41.1 ± 15.7 | 39.7 ± 13.0 | 53.4 ± 20.3 | 0.024 (−10.314–10.362) | 0.095 | −12.208 (−24.659–−0.242) | 0.001 |
| Arm raising (degree/sec) # | 132.1 ± 49.7 | 134.3 ± 41.5 | 135.8 ± 42.4 | 157.5 ± 33.3 | −3.665 (−35.581–28.252) | 0.816 | −35.187 (−61.016–−9.359) | 0.009 |
| Standing balance | ||||||||
| Static sway area (mm2) $ | 675.0 ± 499.2 | 486.0 ± 413.6 | 539.8 ± 319.3 | 385.5 ± 245.8 | 0.721 | 0.483 | ||
| Forward leaning (mm2) ^# | 44.2 ± 17.5 | 40.4 ± 14.0 | 50.4 ± 13.1 | 60.9 ± 17.2 | −5.640 (−17.098–5.818) | 0.296 | −16.076 (−27.338–−4.813) | 0.007 |
| Arm raising (degree/sec) $ | 129.6 ± 58.0 | 127.7 ± 44.4 | 130.2 ± 36.3 | 162.2 ± 42.9 | 0.935 | 0.219 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, P.-Y.; Huang, J.-C.; Tseng, H.-Y.; Yang, Y.-C.; Lin, S.-I. Effects of Trunk Exercise on Unstable Surfaces in Persons with Stroke: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 9135. https://doi.org/10.3390/ijerph17239135
Lee P-Y, Huang J-C, Tseng H-Y, Yang Y-C, Lin S-I. Effects of Trunk Exercise on Unstable Surfaces in Persons with Stroke: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(23):9135. https://doi.org/10.3390/ijerph17239135
Chicago/Turabian StyleLee, Pei-Yun, Jhen-Cih Huang, Hui-Yu Tseng, Yi-Ching Yang, and Sang-I Lin. 2020. "Effects of Trunk Exercise on Unstable Surfaces in Persons with Stroke: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 23: 9135. https://doi.org/10.3390/ijerph17239135
APA StyleLee, P.-Y., Huang, J.-C., Tseng, H.-Y., Yang, Y.-C., & Lin, S.-I. (2020). Effects of Trunk Exercise on Unstable Surfaces in Persons with Stroke: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(23), 9135. https://doi.org/10.3390/ijerph17239135




