The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea
Abstract
:1. Introduction
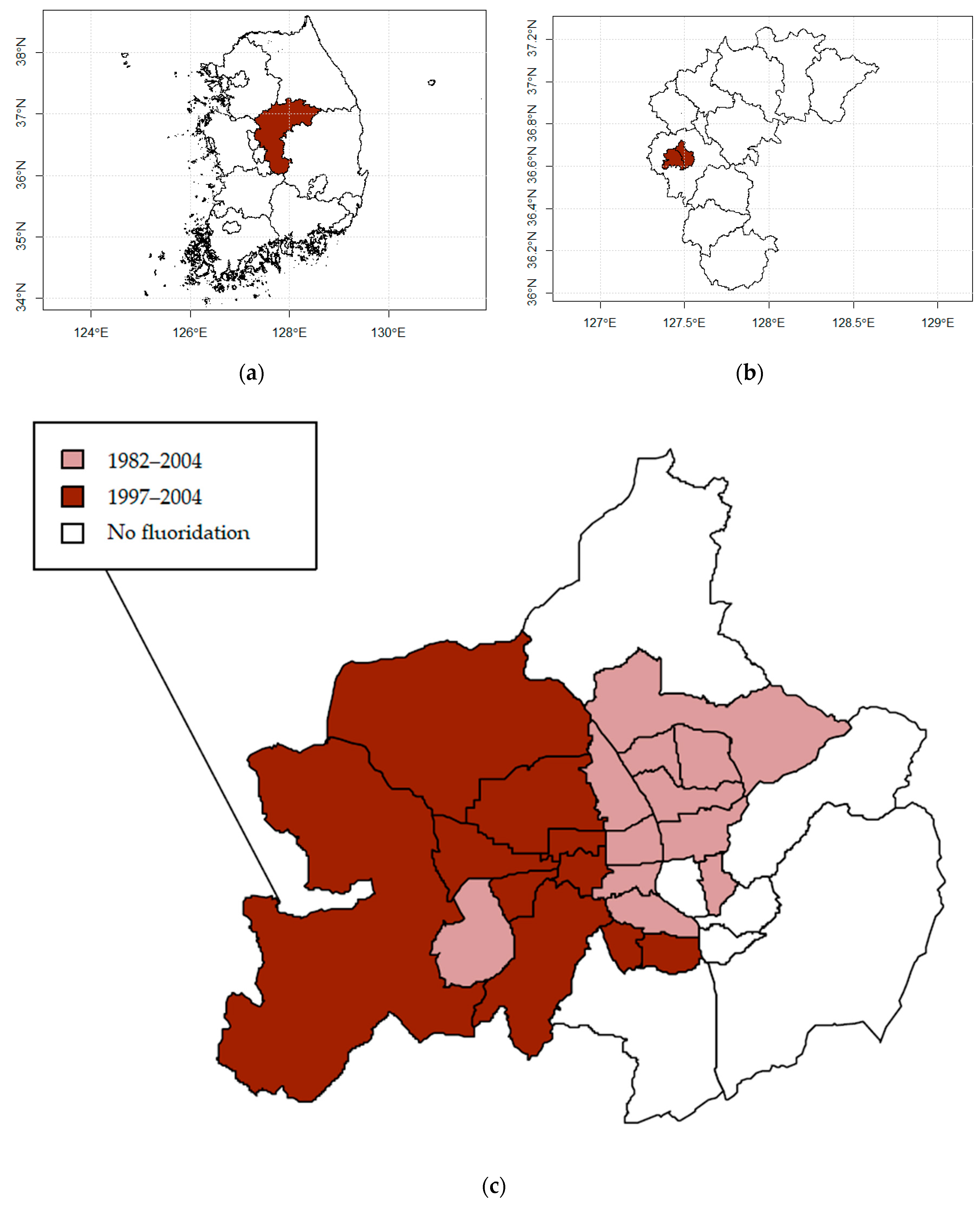
2. Study Area and Data
2.1. Study Design and Locations
2.2. Data Sources and Variables
3. Methodology
3.1. Modeling Health Risk
3.2. Spatio-Temporal Model
3.3. Sensitivity Analysis
3.4. Ethics Approval
4. Results
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Community Water Fluoridation. Available online: https://www.cdc.gov/fluoridation/index.html (accessed on 10 March 2020).
- Ran, T.; Chattopadhyay, S.K. Community Preventive Services Task Force. Economic evaluation of community water fluoridation: A community guide systematic review. Am. J. Prev. Med. 2016, 50, 790–796. [Google Scholar] [CrossRef]
- Griffin, S.O.; Regnier, E.; Griffin, P.M.; Huntley, V. Effectiveness of fluoride in preventing caries in adults. J. Dent. Res. 2007, 86, 410–415. [Google Scholar] [CrossRef]
- Armfield, J.M. When public action undermines public health: A critical examination of antifluoridationist literature. Aust. N. Z. Health Policy 2007, 4. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.N.; Kim, J.H.; Kim, S.Y.; Kim, J.B. Associations of Community Water Fluoridation with Caries Prevalence and Oral Health Inequality in Children. Int. J. Environ. Res. Public Health 2017, 14, 631. [Google Scholar] [CrossRef] [Green Version]
- Aoun, A.; Darwiche, F.; Al Hayek, S.; Doumit, J. The Fluoride Debate: The Pros and Cons of Fluoridation. Prev. Nutr. Food Sci. 2018, 23, 171–180. [Google Scholar] [CrossRef]
- Thornton-Evans, G.; Junger, M.L.; Lin, M.; Wei, L.; Espinoza, L.; Beltran-Aguilar, E. Use of toothpaste and toothbrushing patterns among children and adolescents—The United States, 2013–2016. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 87–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osterman, J.W. Evaluating the impact of municipal water fluoridation on the aquatic environment. Am. J. Public Health 1990, 80, 1230–1235. [Google Scholar] [CrossRef]
- McDonagh, M.S.; Whiting, P.F.; Wilson, P.M.; Sutton, A.J.; Chestnutt, I.; Cooper, J.; Misso, K.; Bradley, M.; Treasure, E.; Kleijnen, J. Systematic review of water fluoridation. BMJ 2000, 321, 855–859. [Google Scholar] [CrossRef] [Green Version]
- Morabia, A. Community water fluoridation: Open discussions strengthen public health. Am. J. Public Health 2016, 106, 209–210. [Google Scholar] [CrossRef]
- Korea Health Promotion Institution. A Community Health Promotion Programme Report Dental Health. 2003. Available online: https://www.khealth.or.kr/kps (accessed on 7 December 2019).
- Cho, H.J.; Jin, B.H.; Park, D.Y.; Jung, S.H.; Lee, H.S.; Paik, D.I.; Bae, K.H. Systemic effect of water fluoridation on dental caries prevalence. Commun. Dent. Oral Epidemiol. 2014, 42, 341–348. [Google Scholar] [CrossRef]
- Kim, M.J.; Kim, H.N.; Jun, E.J.; Ha, J.E.; Han, D.H.; Kim, J.B. Association between estimated fluoride intake and dental caries prevalence among 5-year-old children in Korea. BMC Oral Health 2015, 15, 169. [Google Scholar] [CrossRef] [Green Version]
- Han, S.J.; Kwon, Y.B.; Kim, S.Y.; Kim, J.S.; Lee, J.H.; Kim, J.B. Factors related to the difference in the incidence of caries between children in fluoridated and non-fluoridated areas. J. Korean Acad. Oral Health 2018, 42, 136–144. [Google Scholar] [CrossRef]
- Ok, T.Y.; Kwon, Y.B.; Kim, J.S.; Kim, S.Y.; Lee, J.H.; Kim, H.N.; Kim, J.B. Caries reduction effect of permanent teeth from community water fluoridation program for 17 years in Jinju city. J. Korean Acad. Oral Health 2019, 43, 63–71. [Google Scholar] [CrossRef] [Green Version]
- Green, R.; Lanphear, B.; Hornung, R.; Flora, D.; Martinez-Mier, E.A.; Neufeld, R.; Ayotte, P.; Muckle, G.; Till, C. Association between maternal fluoride exposure during pregnancy and IQ scores in offspring in Canada. JAMA Pediatr. 2019, 173, 940–948. [Google Scholar] [CrossRef]
- Till, C.; Green, R.; Flora, D.; Hornung, R.; Martinez-Mier, E.A.; Blazer, M.; Farmus, L.; Ayotte, P.; Muckle, G.; Lanphear, B. Fluoride exposure from infant formula and child IQ in a Canadian birth cohort. Environ. Int. 2020, 134, 105315. [Google Scholar] [CrossRef]
- Riddell, J.K.; Malin, A.J.; Flora, D.; McCague, H.; Till, C. Association of water fluoride and urinary fluoride concentrations with attention deficit hyperactivity disorder in Canadian youth. Environ. Int. 2019, 133, 105190. [Google Scholar] [CrossRef]
- Park, E.Y.; Hwang, S.S.; Kim, J.Y.; Cho, S.H. Effects of Long-term Fluoride in Drinking Water on Risks of Hip Fracture of the Elderly: An Ecologic Study Based on Database of Hospitalization Episodes. J. Prev. Med. Public Health 2008, 41, 147–152. [Google Scholar] [CrossRef]
- Han, Y.J.; Min, J.Y.; Han, D.H.; Kim, H.D.; Paek, D.M. The Effect of Adjusted Water Fluoridation on Bone Mineral Density. Korean J. Environ. Health Sci. 2008, 34, 261–270. [Google Scholar] [CrossRef]
- Ryu, D.R. Introduction to the medical research using national health insurance claims database. Ewha Med. J. 2017, 40, 66–70. [Google Scholar] [CrossRef] [Green Version]
- Kim, L.; Sakong, J.; Kim, Y.; Kim, S.; Kim, S.; Tchoe, B.; Jeong, H.; Lee, T. Developing the inpatient sample for the National Health Insurance claims data. Health Policy Manag. 2013, 23, 152–161. [Google Scholar] [CrossRef]
- Knorr-Held, L. Bayesian modelling of inseparable space-time variation in disease risk. Stat. Med. 2000, 19, 2555–2567. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.; Rushworth, A.; Napier, G. Spatio-temporal areal unit modelling in R with conditional autoregressive priors using the CARBayesST package. J. Stat. Softw. 2018, 84. [Google Scholar] [CrossRef] [Green Version]
- Anderson, C.; Ryan, L. A comparison of Spatio-temporal disease mapping approaches including an application to ischaemic heart disease in New South Wales, Australia. Int. J. Environ. Res. Public Health 2017, 14, 146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, X.H.; Huang, G.L.; Lin, D.R.; Wan, C.C.; Wang, Y.D.; Song, J.K.; Xu, P. Exposure to fluoride in drinking water and hip fracture risk: A meta-analysis of observational studies. PLoS ONE 2015, 10, e0126488. [Google Scholar] [CrossRef]
- Phipps, K.R.; Orwoll, E.S.; Mason, J.D.; Cauley, J.A. Community water fluoridation, bone mineral density, and fractures: Prospective study of effects in older women. BMJ 2000, 321, 860–864. [Google Scholar] [CrossRef] [Green Version]
- O’Sullivan, V.; O’Connell, B.C. Water fluoridation, dentition status and bone health of older people in Ireland. Commun. Dent. Oral Epidemiol. 2015, 43, 58–67. [Google Scholar] [CrossRef]
- Public Health. Water Fluoridation: Health Monitoring Report for England. 2018. Available online: https://www.gov.uk/government/publications/water-fluoridation-health-monitoring-report-for-england22 (accessed on 18 February 2020).
- Kelsey, J.L. Risk factors for osteoporosis and associated fractures. Public Health Rep. 1989, 104, 14. [Google Scholar]
- Tuck, S.P.; Datta, H.K. Osteoporosis in the aging male: Treatment options. Clin. Interv. Aging 2007, 2, 521. [Google Scholar] [CrossRef] [Green Version]
- Khosla, S.; Melton, L.J., III; Atkinson, E.J.; O’fallon, W.M.; Klee, G.G.; Riggs, B.L. Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: A key role for bioavailable estrogen. J. Clin. Endocrinol. Metab. 1998, 83, 2266–2274. [Google Scholar]
- Peres, M.A.; Peres, K.G.; Barbato, P.R.; Höfelmann, D.A. Access to fluoridated water and adult dental caries: A natural experiment. J. Dent. Res. 2016, 95, 868–874. [Google Scholar] [CrossRef]
- Berry, S.D.; Zullo, A.R.; McConeghy, K.; Lee, Y.; Daiello, L.; Kiel, D.P. Defining hip fracture with claims data: Outpatient and provider claims matter. Osteoporos. Int. 2017, 28, 2233–2237. [Google Scholar] [CrossRef] [PubMed]



| Variables | CWF | Non-CWF | ||
|---|---|---|---|---|
| No. of Residents | % | No. of Residents | % | |
| Total | 4,406,021 | 2,270,959 | ||
| Gender | ||||
| Male | 2,200,104 | 49.9 | 1,126,495 | 49.6 |
| Female | 2,205,917 | 50.1 | 1,144,464 | 50.4 |
| Age (years) | ||||
| <20 | 1,135,966 | 25.8 | 603,984 | 26.6 |
| 20–39 | 1,473,753 | 33.4 | 650,749 | 28.7 |
| 40–59 | 1,292,255 | 29.3 | 813,074 | 35.8 |
| 60–79 | 445,321 | 10.1 | 177,593 | 7.8 |
| ≥80 | 58,726 | 1.33 | 25,559 | 1.13 |
| Population density (people per km2) | 5.1 | 3.4 | ||
| Number of towns (N) | 21 | 9 | ||
| Education level * | ||||
| Middle school or lower | 1689 | 36.8 | 2541 | 34.9 |
| High school | 1433 | 31.2 | 2140 | 29.4 |
| College or higher | 1469 | 32.0 | 2607 | 35.8 |
| Period of residence * | ||||
| >1 year | 324 | 23.5 | 691 | 34.1 |
| 1–5 years | 493 | 35.8 | 1002 | 49.4 |
| 5–10 years | 397 | 28.9 | 462 | 22.8 |
| 10–25 years | 362 | 26.3 | 461 | 22.7 |
| ≥25 years | 124 | 9.01 | 104 | 5.13 |
| Source of water * | ||||
| Community water system | 4363 | 98.8 | 2681 | 98.6 |
| Village water (temporal) | 6 | 0.14 | 0 | 0.00 |
| None | 49 | 1.11 | 39 | 1.43 |
| Types of drinking water | ||||
| Drinking tap water | 812 | 47.8 | 1237 | 45.5 |
| Purified tap water | 524 | 30.9 | 860 | 31.6 |
| Bottled water | 238 | 14.0 | 427 | 15.7 |
| Others | 124,691 | 7.30 | 196 | 7.21 |
| Total | Male | Female | |
|---|---|---|---|
| RR * (95% CrI **) | |||
| Hip Fracture | 0.95 (0.87–1.05) | 0.88 (0.75–1.01) | 0.99 (0.89–1.09) |
| Osteoporosis | 0.94 (0.87–1.02) | 0.86 (0.76–0.97) | 0.95 (0.87–1.03) |
| Bone Cancer | 1.20 (0.89–1.61) | 1.26 (0.84–1.88) | 1.03 (0.87–1.22) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, N.; Kang, S.; Lee, W.; Hwang, S.-s. The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea. Int. J. Environ. Res. Public Health 2020, 17, 9170. https://doi.org/10.3390/ijerph17249170
Lee N, Kang S, Lee W, Hwang S-s. The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea. International Journal of Environmental Research and Public Health. 2020; 17(24):9170. https://doi.org/10.3390/ijerph17249170
Chicago/Turabian StyleLee, Naae, Sungchan Kang, Woojoo Lee, and Seung-sik Hwang. 2020. "The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea" International Journal of Environmental Research and Public Health 17, no. 24: 9170. https://doi.org/10.3390/ijerph17249170
APA StyleLee, N., Kang, S., Lee, W., & Hwang, S.-s. (2020). The Association between Community Water Fluoridation and Bone Diseases: A Natural Experiment in Cheongju, Korea. International Journal of Environmental Research and Public Health, 17(24), 9170. https://doi.org/10.3390/ijerph17249170





