Prevalence of Depression, Anxiety, and Stress among the General Population in Saudi Arabia during Covid-19 Pandemic
Abstract
1. Introduction
2. Methods
2.1. Data Analysis
2.2. Ethical Approval
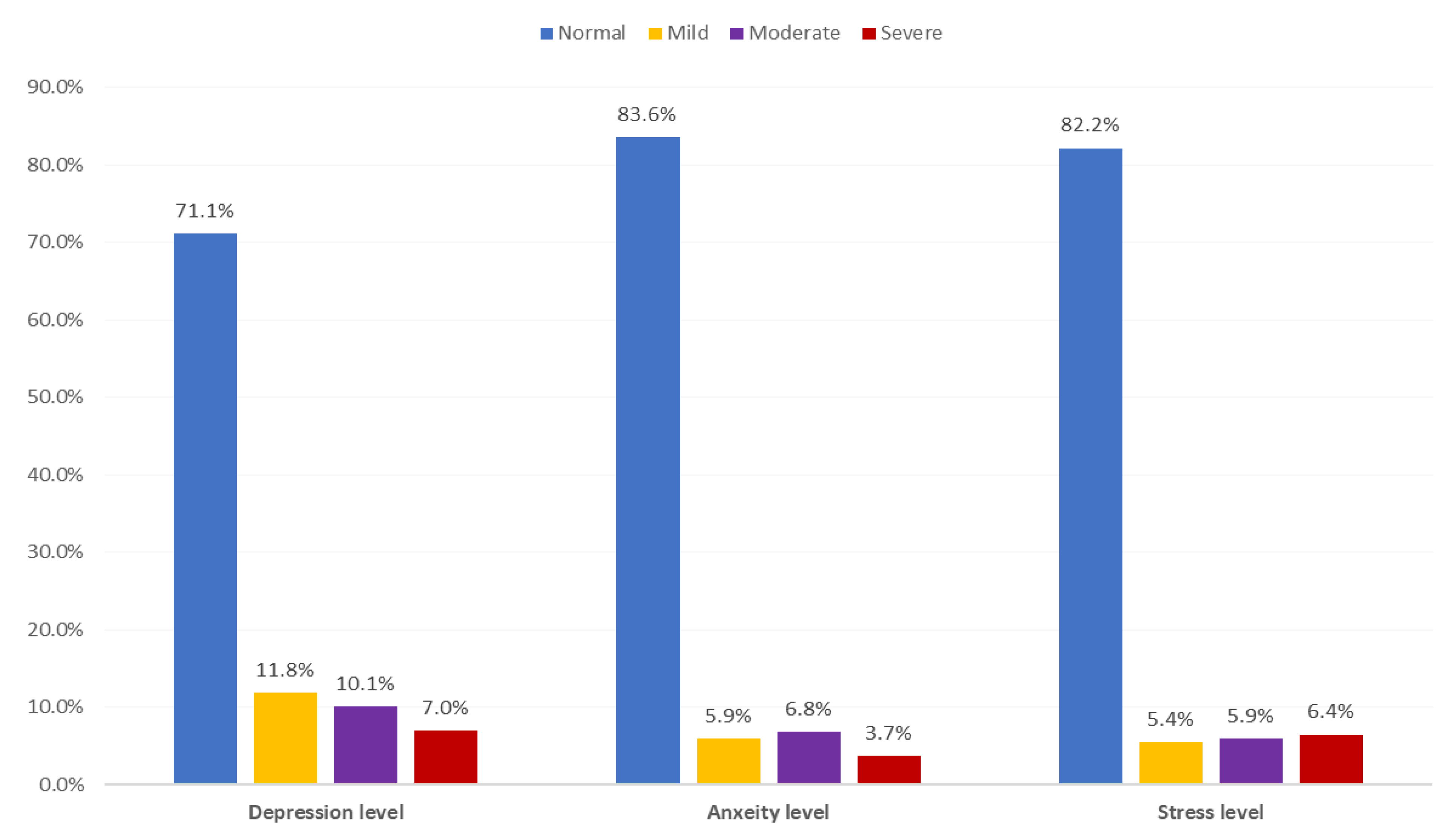
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Nishiura, H.; Jung, S.M.; Linton, N.M.; Kinoshita, R.; Yang, Y.; Hayashi, K.; Kobayashi, T.; Yuan, B.; Akhmetzhanov, A.R. The Extent of Transmission of Novel Coronavirus in Wuhan, China, 2020. J. Clin. Med. 2020, 9, 330. [Google Scholar] [CrossRef] [PubMed]
- WHO. Situation Reports. 2020. Available online: https://www.who.int/emergencies/diseases/novelcoronavirus-2019/situation-reports (accessed on 20 November 2020).
- Medicine JHU. Coronavirus Resource Center. 2020. Available online: https://coronavirus.jhu.edu/ (accessed on 20 November 2020).
- 1389 New COVID-19 Cases and 1626 Recoveries, MOH Says [Press Release]; Ministry of Health: Riyadh, Saudi Arabia, 5 August 2020.
- Abdallah, N. Saudi Arabia Imposes 24-Hour Curfew in Riyadh and Other Cities. Reuters, 6 April 2020. [Google Scholar]
- Ministry of transportation. Saudi Arabia Suspends International Flights Starting Sunday to Prevent Spread of Coronavirus. Arab News, 14 March 2020. [Google Scholar]
- Samar Ahmed, M.R. Saudi Arabia to Bar Arrivals from Abroad to Attend the Haj. Reuters, 22 June 2020. [Google Scholar]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [PubMed]
- Fagiolini, A.; Cuomo, A.; Frank, E. COVID-19 Diary from a Psychiatry Department in Italy. J. Clin. Psychiatry 2020, 81, 20com13357. [Google Scholar] [CrossRef] [PubMed]
- Porcheddu, R.; Serra, C.; Kelvin, D.; Kelvin, N.; Rubino, S. Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J. Infect. Dev. Ctries 2020, 14, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Rodriguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact of COVID-19 in Spain: Early data report. Psychol. Trauma 2020, 12, 550–552. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Ali, A.M.; Ahmed, A.; Sharaf, A.; Kawakami, N.; Abdeldayem, S.M.; Green, J. The Arabic Version of The Depression Anxiety Stress Scale-21: Cumulative scaling and discriminant-validation testing. Asian J. Psychiatry 2017, 30, 56–58. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F.; Psychology Foundation of Australia. Manual for the Depression Anxiety Stress Scales; Psychology Foundation of Australia: Sydney, NSW, Australia, 1995. [Google Scholar]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102076. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, Ó.; Sánchez-Sánchez, L.C.; García-Montes, J.M. Psychological impact of COVID-19 confinement and its relationship with meditation. Int. J. Environ. Res. Public Health 2020, 17, 6642. [Google Scholar] [CrossRef] [PubMed]
- Sareen, J.; Erickson, J.; Medved, M.I.; Asmundson, G.J.; Enns, M.W.; Stein, M.; Leslie, W.; Doupe, M.; Logsetty, S. Risk factors for post-injury mental health problems. Depress Anxiety 2013, 30, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.R.; Agho, K.E.; Stevens, G.J.; Raphael, B. Factors influencing psychological distress during a disease epidemic: Data from Australia’s first outbreak of equine influenza. BMC Public Health 2008, 8, 347. [Google Scholar] [CrossRef] [PubMed]
- Tian, F.; Li, H.; Tian, S.; Yang, J.; Shao, J.; Tian, C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020, 288, 112992. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychol. Health Med. 2020, 1–12. [Google Scholar] [CrossRef]
- Jia, Z.; Tian, W.; Liu, W.; Cao, Y.; Yan, J.; Shun, Z. Are the elderly more vulnerable to psychological impact of natural disaster? A population-based survey of adult survivors of the 2008 Sichuan earthquake. BMC Public Health 2010, 10, 172. [Google Scholar] [CrossRef]
- Ngo, E.B. When Disasters and Age Collide: Reviewing Vulnerability of the Elderly. Nat. Hazards Rev. 2001, 2, 80–89. [Google Scholar] [CrossRef]
- Cheng, C.; Jun, H.; Liang, B. Psychological health diathesis assessment system: A nationwide survey of resilient trait scale for Chinese adults. Stud. Psychol. Behav. 2014, 12, 735–742. [Google Scholar]
- Gooding, P.A.; Hurst, A.; Johnson, J.; Tarrier, N. Psychological resilience in young and older adults. Int. J. Geriatr. Psychiatry 2012, 27, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological Impact and Associated Factors During the Initial Stage of the Coronavirus (COVID-19) Pandemic Among the General Population in Spain. Front. Psychol. 2020, 11, 1540. [Google Scholar] [CrossRef] [PubMed]
- Frech, A.; Williams, K. Depression and the psychological benefits of entering marriage. J. Health Soc. Behav. 2007, 48, 149–163. [Google Scholar] [CrossRef] [PubMed]
- Kalmijn, M. The Ambiguous Link between Marriage and Health: A Dynamic Reanalysis of Loss and Gain Effects. Soc. Forces 2017, 95, 1607–1636. [Google Scholar] [CrossRef]
- Radó, M.K. Tracking the Effects of Parenthood on Subjective Well-Being: Evidence from Hungary. J. Happiness Stud. 2020, 21, 2069–2094. [Google Scholar] [CrossRef]
- Nomaguchi, K.M. Parenthood and psychological well-being: Clarifying the role of child age and parent-child relationship quality. Soc. Sci. Res. 2012, 41, 489–498. [Google Scholar] [CrossRef]
- Cai, X.; Hu, X.; Ekumi, I.O.; Wang, J.; An, Y.; Li, Z.; Yuan, B. Psychological Distress and Its Correlates Among COVID-19 Survivors During Early Convalescence Across Age Groups. Am. J. Geriatr. Psychiatry 2020, 28, 1030–1039. [Google Scholar] [CrossRef]
- Ho, C.S.H.; Tan, E.L.Y.; Ho, R.C.M.; Chiu, M.Y.L. Relationship of Anxiety and Depression with Respiratory Symptoms: Comparison between Depressed and Non-Depressed Smokers in Singapore. Int. J. Environ. Res. Public Health 2019, 16, 163. [Google Scholar] [CrossRef]
- Hatch, R.; Young, D.; Barber, V.; Griffiths, J.; Harrison, D.A.; Watkinson, P. Anxiety, Depression and Post Traumatic Stress Disorder after critical illness: A UK-wide prospective cohort study. Crit Care 2018, 22, 310. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Alghamdi, S.M.; Almehmadi, M.; Alqahtani, A.S.; Quaderi, S.; Mandal, M.; Hurst, J.R. Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0233147. [Google Scholar] [CrossRef]
- Tan, B.Y.Q.; Chew, N.W.S.; Lee, G.K.H.; Jing, M.; Goh, Y.; Yeo, L.L.L.; Zhang, K.; Chin, H.-K.; Ahmad, A.; Khan, F.A.; et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Ann. Intern. Med. 2020, 173, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Khan, F.A.; Shanmugam, G.N.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Alsubaie, S.; Hani Temsah, M.; Al-Eyadhy, A.A.; Gossady, I.; Hasan, G.M.; Al-Rabiaah, A.; Jamal, A.A.; Alhaboob, A.A.; Alsohime, F.; Somily, A.M. Middle East Respiratory Syndrome Coronavirus epidemic impact on healthcare workers’ risk perceptions, work and personal lives. J. Infect. Dev. Ctries 2019, 13, 920–926. [Google Scholar] [CrossRef]
- Temsah, M.H.; Al-Sohime, F.; Alamro, N.; Al-Eyadhy, A.; Al-Hasan, K.; Jamal, A.; Al-Maglouth, I.; Aljamaan, F.; Al Amri, M.; Barry, M.; et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J. Infect. Public Health 2020, 13, 877–882. [Google Scholar] [CrossRef] [PubMed]
| Severity | Depression | Anxiety | Stress |
|---|---|---|---|
| Normal | 0–9 | 0–7 | 0–14 |
| Mild | 10–13 | 8–9 | 15–18 |
| Moderate | 14–20 | 10–14 | 19–25 |
| Severe | 21–27 | 15–19 | 26–33 |
| Extremely severe | 28+ | 20+ | 34+ |
| Personal Data | No | % | |
|---|---|---|---|
| Gender | Male | 871 | 54.5% |
| Female | 726 | 45.5% | |
| Age in years | <18 years | 29 | 1.8% |
| 18–25 | 270 | 16.9% | |
| 26–35 | 501 | 31.4% | |
| 36–45 | 488 | 30.6% | |
| 46–55 | 223 | 14.0% | |
| 56–65 | 77 | 4.8% | |
| >65 years | 9 | 0.6% | |
| Nationality | Non-Saudi | 62 | 3.9% |
| Saudi | 1535 | 96.1% | |
| Educational level | Below secondary | 27 | 1.7% |
| Secondary | 263 | 16.5% | |
| University/more | 1307 | 81.8% | |
| Work | Not working | 496 | 31.1% |
| Governmental sector | 783 | 49.0% | |
| Private sector | 188 | 11.8% | |
| Military sector | 130 | 8.1% | |
| Health care practitioner | Yes | 542 | 33.9% |
| No | 1055 | 66.1% | |
| Monthly income | <5000 SR | 435 | 27.2% |
| 50,00–10,000 SR | 293 | 18.3% | |
| 10,000–20,000 SR | 587 | 36.8% | |
| >20,000 SR | 282 | 17.7% | |
| Marital status | Single | 424 | 26.5% |
| Married | 1104 | 69.1% | |
| Divorced/widow | 69 | 4.3% | |
| Number of children | None | 113 | 9.6% |
| 1–2 | 373 | 31.8% | |
| 3–5 | 547 | 46.6% | |
| 6+ | 140 | 11.9% | |
| If female, pregnant? | Yes | 34 | 6.7% |
| No | 476 | 93.3% | |
| Smoking | Never smoker | 1114 | 69.8% |
| Current smoker | 283 | 17.7% | |
| Ex-smoker | 200 | 12.5% | |
| Risk of Exposure to COVID-19 | No | % | |
|---|---|---|---|
| Was abroad during last three months | Yes | 118 | 7.4% |
| No | 1479 | 92.6% | |
| Contact with COVID-19 case during last month | Yes | 35 | 2.2% |
| No | 1562 | 97.8% | |
| Previously quarantined | Yes | 38 | 2.4% |
| No | 1559 | 97.6% | |
| Chronic health problems | None | 1172 | 73.4% |
| Autoimmune diseases including asthma | 119 | 7.5% | |
| Hypertension under treatment | 93 | 5.8% | |
| Chronic heart diseases | 22 | 1.4% | |
| Diabetes Mellitus | 113 | 7.1% | |
| Immunosuppressive disorders | 34 | 2.1% | |
| Hypothyroidism | 32 | 2.0% | |
| Renal disorders | 5 | 0.3% | |
| Others | 91 | 5.7% | |
| Domain | Items | Did Not Apply to Me at All | Applied to Me to Some Degree, or Some of the Time | Applied to Me to a Considerable Degree or a Good Part of Time | Applied to Me Very Much or Most of the Time | ||||
|---|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | No | % | ||
| Depression | I could not seem to experience any positive feeling at all | 935 | 58.5% | 467 | 29.2% | 141 | 8.8% | 54 | 3.4% |
| I found it difficult to work up the initiative to do things | 1036 | 64.9% | 396 | 24.8% | 101 | 6.3% | 64 | 4.0% | |
| I felt that I had nothing to look forward to | 1042 | 65.2% | 376 | 23.5% | 102 | 6.4% | 77 | 4.8% | |
| I felt down hearted and blue | 797 | 49.9% | 556 | 34.8% | 133 | 8.3% | 111 | 7.0% | |
| I was unable to become enthusiastic about anything | 1174 | 73.5% | 302 | 18.9% | 72 | 4.5% | 49 | 3.1% | |
| I felt I wasn’t worth much as a person | 1224 | 76.6% | 242 | 15.2% | 84 | 5.3% | 47 | 2.9% | |
| I felt that life was meaningless | 1170 | 73.3% | 276 | 17.3% | 72 | 4.5% | 79 | 4.9% | |
| Anxiety | I was aware of dryness of my mouth | 1158 | 72.5% | 351 | 22.0% | 63 | 3.9% | 25 | 1.6% |
| I experienced breathing difficulty | 1372 | 85.9% | 176 | 11.0% | 36 | 2.3% | 13 | 0.8% | |
| I experienced trembling | 1437 | 90.0% | 133 | 8.3% | 13 | .8% | 14 | 0.9% | |
| I was worried about situations in which I might panic and make a fool of myself | 902 | 56.5% | 482 | 30.2% | 136 | 8.5% | 77 | 4.8% | |
| I felt I was close to panic | 1480 | 92.7% | 96 | 6.0% | 16 | 1.0% | 5 | 0.3% | |
| I was aware of the action of my heart in the absence of physical exertion | 1445 | 90.5% | 108 | 6.8% | 24 | 1.5% | 20 | 1.3% | |
| I felt scared without any good reason | 1238 | 77.5% | 277 | 17.3% | 54 | 3.4% | 28 | 1.8% | |
| Stress | I found it hard to wind down | 597 | 37.4% | 715 | 44.8% | 199 | 12.5% | 86 | 5.4% |
| I tended to over-react to situations | 962 | 60.2% | 458 | 28.7% | 129 | 8.1% | 48 | 3.0% | |
| I felt that I was using a lot of nervous energy | 957 | 59.9% | 481 | 30.1% | 104 | 6.5% | 55 | 3.4% | |
| I found myself getting agitated | 812 | 50.8% | 563 | 35.3% | 142 | 8.9% | 80 | 5.0% | |
| I found it difficult to relax | 895 | 56.0% | 468 | 29.3% | 142 | 8.9% | 92 | 5.8% | |
| I was intolerant of anything that kept me from getting on with what I was doing | 1066 | 66.8% | 392 | 24.5% | 86 | 5.4% | 53 | 3.3% | |
| I felt that I was rather touchy | 972 | 60.9% | 470 | 29.4% | 102 | 6.4% | 53 | 3.3% | |
| Bio-Demographic Data | Depression | Anxiety | Stress | ||||
|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | ||
| Gender | Male | 218 | 25.0% | 118 | 13.5% | 124 | 14.2% |
| Female | 244 | 33.6% | 144 | 19.8% | 161 | 22.2% | |
| p-Value | 0.001 * | 0.001 * | 0.001 * | ||||
| Age in years | <35 years | 285 | 35.6% | 163 | 20.4% | 184 | 23.0% |
| >35 years | 177 | 22.2% | 99 | 12.4% | 101 | 12.7% | |
| p-Value | 0.001 * | 0.001 * | 0.001 * | ||||
| Nationality | Non-Saudi | 23 | 37.1% | 15 | 24.2% | 14 | 22.6% |
| Saudi | 439 | 28.6% | 247 | 16.1% | 271 | 17.7% | |
| p-Value | 0.148 | 0.091 | 0.321 | ||||
| Educational level | Below secondary | 6 | 22.2% | 5 | 18.5% | 2 | 7.4% |
| Secondary | 71 | 27.0% | 37 | 14.1% | 39 | 14.8% | |
| University/ more | 385 | 29.5% | 220 | 16.8% | 244 | 18.7% | |
| p-Value | 0.536 | 0.520 | 0.120 | ||||
| Work | Not working | 171 | 34.5% | 87 | 17.5% | 97 | 19.6% |
| Governmental sector | 203 | 25.9% | 126 | 16.1% | 132 | 16.9% | |
| Private sector | 51 | 27.1% | 26 | 13.8% | 37 | 19.7% | |
| Military sector | 37 | 28.5% | 23 | 17.7% | 19 | 14.6% | |
| p-Value | 0.011 * | 0.662 | 0.412 | ||||
| Health care practitioner | Yes | 177 | 32.7% | 109 | 20.1% | 120 | 22.1% |
| No | 285 | 27.0% | 153 | 14.5% | 165 | 15.6% | |
| p-Value | 0.019 * | 0.004 * | 0.001 * | ||||
| Marital status | Single | 176 | 41.5% | 89 | 21.0% | 106 | 25.0% |
| Married | 266 | 24.1% | 155 | 14.0% | 165 | 14.9% | |
| Divorced/ widow | 20 | 29.0% | 18 | 26.1% | 14 | 20.3% | |
| p-Value | 0.001 * | 0.001 * | 0.001 * | ||||
| Number of children | None | 30 | 26.5% | 21 | 18.6% | 15 | 13.3% |
| 1–2 | 117 | 31.4% | 73 | 19.6% | 83 | 22.3% | |
| 3–5 | 124 | 22.7% | 70 | 12.8% | 75 | 13.7% | |
| 6+ | 15 | 10.7% | 9 | 6.4% | 6 | 4.3% | |
| p-Value | 0.001 * | 0.001 * | 0.001 * | ||||
| If female, pregnant? | Yes | 14 | 41.2% | 7 | 20.6% | 10 | 29.4% |
| No | 138 | 29.0% | 88 | 18.5% | 90 | 18.9% | |
| p-Value | 0.133 | 0.761 | 0.136 | ||||
| Smoking | Never smoker | 311 | 27.9% | 181 | 16.2% | 190 | 17.1% |
| Current smoker | 101 | 35.7% | 52 | 18.4% | 65 | 23.0% | |
| Ex-smoker | 50 | 25.0% | 29 | 14.5% | 30 | 15.0% | |
| p-Value | 0.015 * | 0.509 | 0.036 * | ||||
| Was abroad during last three months | Yes | 41 | 34.7% | 26 | 22.0% | 29 | 24.6% |
| No | 421 | 28.5% | 236 | 16.0% | 256 | 17.3% | |
| p-Value | 0.148 | 0.086 | 0.047 * | ||||
| Contact with COVID-19 case during last month | Yes | 15 | 42.9% | 15 | 42.9% | 9 | 25.7% |
| No | 447 | 28.6% | 247 | 15.8% | 276 | 17.7% | |
| p-Value | 0.066 | 0.001 * | 0.219 | ||||
| Previously quarantined | Yes | 11 | 28.9% | 12 | 31.6% | 5 | 13.2% |
| No | 451 | 28.9% | 250 | 16.0% | 280 | 18.0% | |
| p-Value | 0.998 | 0.011 * | 0.445 | ||||
| Chronic health problems | None | 326 | 27.8% | 170 | 14.5% | 194 | 16.6% |
| High risk health condition | 136 | 32.0% | 92 | 21.6% | 91 | 21.4% | |
| p-Value | 0.103 | 0.001 * | 0.025 * | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alamri, H.S.; Algarni, A.; Shehata, S.F.; Al Bshabshe, A.; Alshehri, N.N.; ALAsiri, A.M.; Hussain, A.H.; Alalmay, A.Y.; Alshehri, E.A.; Alqarni, Y.; et al. Prevalence of Depression, Anxiety, and Stress among the General Population in Saudi Arabia during Covid-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9183. https://doi.org/10.3390/ijerph17249183
Alamri HS, Algarni A, Shehata SF, Al Bshabshe A, Alshehri NN, ALAsiri AM, Hussain AH, Alalmay AY, Alshehri EA, Alqarni Y, et al. Prevalence of Depression, Anxiety, and Stress among the General Population in Saudi Arabia during Covid-19 Pandemic. International Journal of Environmental Research and Public Health. 2020; 17(24):9183. https://doi.org/10.3390/ijerph17249183
Chicago/Turabian StyleAlamri, Hasan Saeed, Abdullah Algarni, Shehata F. Shehata, Ali Al Bshabshe, Nada N. Alshehri, Abdalla M. ALAsiri, Amjad H. Hussain, Abdulrahman Y. Alalmay, Eman A. Alshehri, Yahya Alqarni, and et al. 2020. "Prevalence of Depression, Anxiety, and Stress among the General Population in Saudi Arabia during Covid-19 Pandemic" International Journal of Environmental Research and Public Health 17, no. 24: 9183. https://doi.org/10.3390/ijerph17249183
APA StyleAlamri, H. S., Algarni, A., Shehata, S. F., Al Bshabshe, A., Alshehri, N. N., ALAsiri, A. M., Hussain, A. H., Alalmay, A. Y., Alshehri, E. A., Alqarni, Y., & Saleh, N. F. (2020). Prevalence of Depression, Anxiety, and Stress among the General Population in Saudi Arabia during Covid-19 Pandemic. International Journal of Environmental Research and Public Health, 17(24), 9183. https://doi.org/10.3390/ijerph17249183






